Abstract
Introduction
Childhood trauma is a risk factor for the development of psychosis. Furthermore, a number of theories propose specific mechanisms by which childhood trauma may contribute to more severe positive and negative psychotic symptoms, some of which are supported empirically. The robustness of this empirical evidence is unclear due to mixed results and methodological limitations of individual studies. A systematic review and meta-analysis of the evidence for associations between childhood trauma and severity of hallucinations, delusions, and negative psychotic symptoms in clinical populations with a diagnosed psychotic disorder is needed.
Method
A systematic search was conducted. Reference lists of relevant review articles were hand-searched, and authors contacted for data and additional unpublished studies. Study reporting bias and quality was assessed.
Results
In total, 6667 studies were identified and of these 41 studies met inclusion criteria. Of these, 29 studies (4680 participants) were meta-analyzed. Among individuals with psychosis, childhood trauma was significantly correlated with severity of hallucinations (r = .199, P < .001) and delusions (r = .172, P < .001) but contrary to our hypothesis, not correlated with severity of negative symptoms (r = .049, P = .095). Severity of childhood neglect was correlated with negative symptoms (r = .142, P = .005).
Conclusion
The results lend support for cognitive and biological theories that traumas in childhood may lead to hallucinations and delusions within psychotic disorders and have important implications for clinical practice.
Keywords: schizophrenia, psychotic, trauma, childhood, abuse, sexual, physical, emotional, neglect
There is now considerable evidence that childhood trauma, including exposures such as sexual, physical, and emotional abuse, and neglect is a risk factor for psychotic disorder,1,2 with emerging evidence supporting childhood trauma as a causal risk factor for psychotic symptoms and disorder.3–5 Researchers are moving away from psychosis diagnosis to specific symptoms (such as hallucinations) as an area of focus.5,6 A multitude of theories conceptualize how childhood trauma impacts affect, memory, and cognition to explain the development of specific psychotic symptoms.7,8
Both theoretical and empirical investigations have favored the exploration of childhood trauma in relation to hallucinations. Proposed mechanisms include hallucinations as variations of post-traumatic intrusions.9–12 Bentall’s theory proposes a specific relationship between childhood sexual abuse and hallucinations and that dissociation plays a role in the mechanism.8 This model has received empirical support.13–16
Delusions have been conceptualized as developing as a result of childhood trauma via biased threat beliefs, stemming from trauma-related negative beliefs about self and others.9,17,18 A more specific version of this theory posits that persecutory delusions develop as a consequence of early parental neglect, which impacts attachment, and leads to mistrust of others.8,19 These models have some empirical support.20
Theorists have also posited a route between childhood trauma and negative symptoms.21 The traumagenic neurodevelopmental model proposes a neurobiological pathway from childhood trauma through hyperarousal and the biological stress system to negative symptoms.21 Another model suggests that childhood neglect plays a role in the development of negative symptoms through poor attachment,22,23 and has received some empirical support.24
To date, the theorizing about causal pathways from specific childhood trauma types to specific psychotic symptoms has been supported by single or small numbers of empirical studies of varying methodological quality. If certain psychotic symptoms do arise from childhood trauma, it follows that these symptoms would be more severe among people with a psychotic disorder who have experienced childhood trauma. We intend to test this conjecture via systematic review and meta-analysis. We hypothesize that childhood trauma will be associated with more severe hallucinations, delusions, and negative symptoms in those with a psychotic disorder. There is an urgent need for this relationship to be clarified, particularly in light of calls for interventions for the treatment of trauma-related psychotic symptoms,25 which should take into account the specificity of relationships between childhood trauma and certain symptoms if indeed they do exist.
Method
Literature Search
This study was conducted in accordance with quality guidelines provided by the Meta-analysis of Observational Studies in Epidemiology (MOOSE) Group26 and PRISMA.27 A systematic database search covering the years 1980 to December 2014 was conducted on PubMed, SCOPUS, Medline, Embase, Clinahl, Web of Science, PsycINFO, Cochrane. Medical Subject Headings (MeSH), and database thesaurus tools were used to maximize search results. Our search used keywords: “psychosis,” “schizophrenia,” “schizoaffective,”, “psychotic,” “hallucination,” “delusion,” “paranoia” (category 1); “child abuse,” “child trauma,” “physical abuse,” “sexual abuse,” “rape,” “witness,” “psychological abuse,” “emotional abuse,” “neglect,” “maltreatment,” “bully,” “bullied,” “victim,” “sexual trauma,” “psychological trauma,” “physical assault,” “sexual assault,” “molest,” “child molest,” “sexual molest,” or “victim of crime” (category 2). Category 1 or 2 were combined with OR, and then category 1 and 2 were combined with AND. Reference lists of published studies were also reviewed for additional studies.
Three raters extracted data (TB, AGS, EB). Independent trial runs with random samples of 14–17 studies were completed until the 3 raters achieved 100% inter-rater reliability. Inconsistencies were discussed and resolved in consultation with co-author SB until 100% inter-rater reliability was reached. Of 473 studies that reached full-text screening, 148 (31%) were doubly data extracted by at least 2 raters.
Inclusion Criteria
Articles must have been published in English and meet the following inclusion criteria:
1. Studies including clinical samples with a diagnosis of schizophrenia, schizoaffective disorder, schizophreniform, psychosis not otherwise specified, first episode psychosis, delusional disorder, depression with psychotic features, and bipolar disorder with psychotic features based on DSM-III, DSM-III-R, DSM-IV, DSM-IV-TR, DSM-5, ICD-9, ICD-10, determined by semi-structured interview or psychiatrist or psychologist evaluation.
2. Studies measuring childhood trauma, defined as: (1) must have occurred before age 18 or be described as in “childhood” or “adolescence” (2) must be differentiated from adulthood trauma (3). The types of childhood trauma included in the review were: childhood sexual abuse (eg, intercourse, sexual touching), childhood physical abuse (physical harm and punishment), childhood emotional abuse (also called psychological abuse; eg, harsh treatment or teasing by parents), childhood physical neglect (eg, failure to provide food, hydration, or clothing), childhood emotional neglect (eg, unresponsive to a child’s emotional needs), bullying (eg, repeated assault, intimation, or name-calling). Parental death and parental separation were not included. Studies were included if childhood trauma was measured in at least 90% of participants.
3. Studies with sufficient information to determine the presence of a statistically positive, negative, or nonsignificant association between childhood trauma and any characteristic of hallucinations, delusions, positive symptoms, or negative symptoms.
Studies were included in the meta-analyses when they provided sufficient data to estimate relevant effect size. Authors were contacted for the provision of missing data if necessary for the meta-analysis (including relevant additional data collected but not reported) and to determine the eligibility of several studies. Additional data were provided for 11 studies, and 2 new published articles were provided.
Data Analysis
Childhood trauma types were recorded according to the most frequently reported categories found across the studies: childhood sexual abuse, childhood physical abuse, childhood emotional abuse, childhood physical neglect, childhood emotional neglect, and total childhood trauma. Total childhood trauma represented studies that reported a global measure of childhood trauma or a combination of abuse and neglect trauma types. One study reported a group with a history of physical and sexual abuse, and was categorized as childhood sexual abuse as this trauma type was clearly predominant.28 Three studies reported overall abuse or overall neglect (or both) and this is represented in supplementary tables 2, 4 and 5.14,29,30 No studies reported separately on bullying.
Associations with trauma types were tabulated according to the following psychotic symptoms: hallucinations, delusions, positive symptoms, negative symptoms (Supplementary tables 2–5). To assess selective reporting, outcomes were marked “Outcome not reported” (shown by ^) where childhood trauma types were known to be measured but not reported. The Downs and Black checklist was used to assess the methodological quality and risk of bias of included studies.31
The meta-analysis was conducted using Comprehensive Meta-Analysis version 2.2 (CMA).32 Random effects models were used as we expected that the true effect may vary from study to study due to differences in measures, clinical features, and demographics of each sample. This model assumes that the true effects of the studies that have been performed are a random sample of all the possible studies that could be performed, and the summary effect is the mean of these true effects.33 Summary effect sizes were transformed to correlations for ease of interpretation, and α = 0.05 was used unless a more conservative α was applied by the authors. Where studies reported multiple psychosis outcomes that were similar (eg severity of auditory and visual hallucinations34) or outcomes at multiple time points, eg, Yun and colleagues35 data were combined by calculating the mean of the effect sizes using standard CMA procedures. Studies that measured several types of delusional content without reporting an overall severity measure were excluded from the meta-analysis.36,37 Childhood physical neglect and childhood emotional neglect were collapsed into one category called “neglect” to test our hypotheses. We examined heterogeneity between studies using the Q statistic and the I2 index.38 We assessed for publication bias by inspecting funnel plots, and calculating Egger’s test (2-tailed) and fail-safe N.39 The fail-safe N test calculates a combined P value for all studies in each meta-analysis, and estimates how many additional studies with no effect would be necessary to produce a nonsignificant P value.
Results
The systematic review yielded 41 studies (total participants = 7007; supplementary figure 1) that had outcomes pertaining to the relationship between childhood trauma and psychotic symptom severity among individuals with a diagnosis of psychosis. Of these, 29 studies had sufficient data available to be included in the meta-analyses (total n = 4680). Characteristics of the 41 included studies are described in supplementary table 1.
Quality and Selective Reporting
Thirty-six of 41 studies were cross-sectional in design. The remaining 5 were longitudinal.35,40–43 Quality scores on the Downs and Black checklist ranged from 9 to 18 (out of a possible 19 for cross-sectional studies), with a mean of 13.41 (SD = 2.30). Scores are shown in supplementary tables 1 and 6 for each included study. The most poorly met quality criteria were use of representative samples, reporting how many participants approached actually accepted, blinding interviewers, reporting the time period of recruitment, adjusting for confounds in analyses, and reporting power analyses (supplementary table 6). Selective reporting bias was rarely present for childhood trauma (over 95% of childhood trauma outcomes were reported), but was commonplace with the neglect outcomes, which were reported only half of the time (childhood physical neglect: 52% and childhood emotional neglect: 56%; supplementary tables 2–5).
Hallucinations
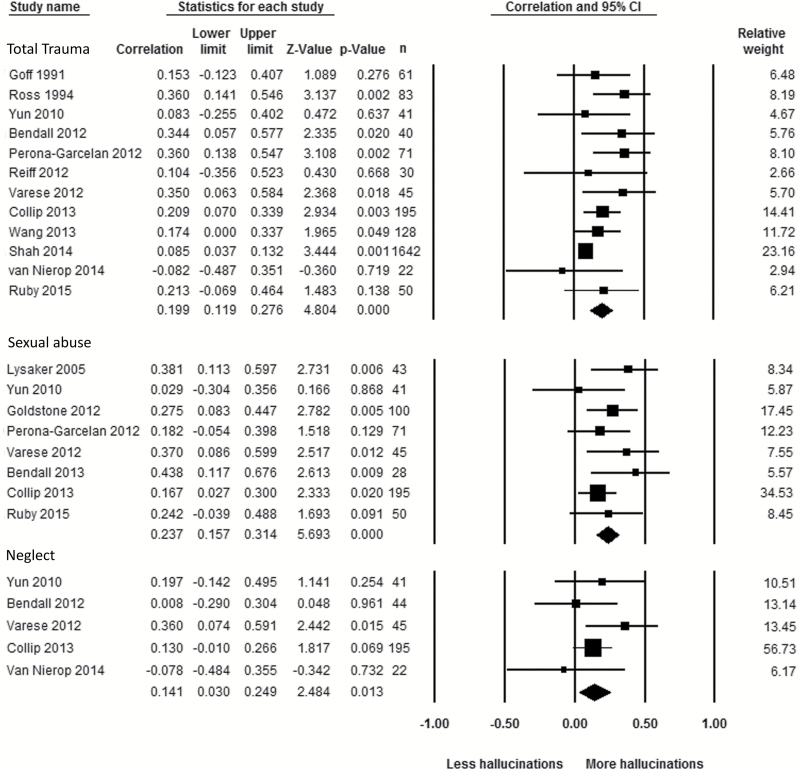
Twenty-one studies measured relationships between hallucination severity and childhood trauma (supplementary table 2). Of these, 7 studies collected relevant data that were not reported (supplementary table 2). Childhood sexual abuse data were omitted in 3 studies; childhood physical abuse, childhood emotional abuse, childhood physical neglect, and childhood emotional neglect data were omitted in between 4 and 7 studies. No studies omitted total childhood trauma data. Meta-analyses conducted using data from 14 of the studies revealed that hallucination severity was associated with the 3 childhood trauma types of interest (total childhood trauma, childhood sexual abuse, and neglect, figure 1). Total childhood trauma was associated with hallucination severity (12 studies; r = .199, 95% CI = [0.119, 0.276], P < .001), however, there was some evidence of publication bias (fail safe N = 119, Egger’s t = 2.505, P = .031). Hallucination severity was also associated with childhood sexual abuse (8 studies, r = .237, 95% CI = [0.157, 0.314], P < .001) and childhood neglect (5 studies, r = .141, 95% CI = [0.030, 0.249], P = .013). There was no evidence of publication bias in these 2 meta-analyses. Heterogeneity of studies was nonsignificant for all 3 of the analyses (table 1).
Fig. 1.
Forest plot showing relationships between hallucinations and total childhood trauma, childhood sexual abuse and childhood neglect.
Table 1.
Summary of Meta-Analyses Showing Pooled Estimates of Relationships Between Childhood Trauma and Psychotic Symptoms
| Symptom | Childhood Trauma Type | k | n | r (P) | I 2 | Q (P) |
|---|---|---|---|---|---|---|
| Hallucinations | Total trauma | 12 | 2408 | .199 (< .001)*** | 42.518 | 19.136 (.059) |
| Sexual abuse | 8 | 573 | .237 (<.001)*** | 0 | 6.588 (.473) | |
| Neglect | 5 | 347 | .141 (.013)* | 2.779 | 4.114 (.391) | |
| Delusions | Total trauma | 10 | 2288 | .172 (< .001)*** | 48.835 | 17.590 (.040)* |
| Sexual abuse | 7 | 544 | .139 (.025)* | 41.999 | 10.345 (.111) | |
| Neglect | 5 | 361 | .061 (0.272) | 0 | 3.083 (.544) | |
| Positive symptoms | Total trauma | 18 | 3857 | .142 (<.001)*** | 40.426 | 28.536 (.039)* |
| Sexual abuse | 10 | 829 | .201 (<.001)*** | 40.132 | 15.033 (.090) | |
| Neglect | 5 | 628 | .127 (.086) | 63.120 | 10.846 (.028)* | |
| Negative symptoms | Trauma | 15 | 3712 | .049 (.095) | 52.107 | 29.232 (.010)* |
| Sexual abuse | 9 | 746 | .092 (.133) | 57.013 | 18.610 (.017)* | |
| Neglect | 8 | 1274 | .142 (.005)** | 61.600 | 18.229 (.011)* |
Note: k, number of studies; n, combined sample size; r, meta-analytic estimate; I2, heterogeneity, Q, heterogeneity chi-square.
P < .05
P < .01
P < .001.
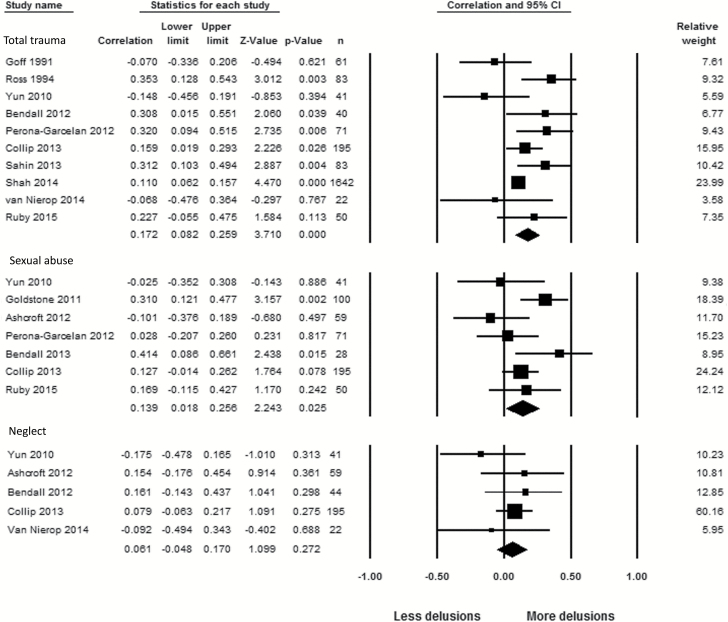
Delusions
Twenty studies measured relationships between delusion severity and childhood trauma (supplementary table 3). Of these, 9 studies collected relevant data that were not reported (supplementary table 3). Childhood sexual abuse data were omitted in 4 studies; childhood physical abuse, childhood emotional abuse, childhood physical neglect, and childhood emotional neglect data were omitted in between 5 and 9 studies. Meta-analyses revealed that delusion severity was associated with total childhood trauma and childhood sexual abuse, but not with childhood neglect (figure 2). Total childhood trauma was associated with delusion severity (10 studies; r = .172, 95% CI = [0.082, 0.259], P < .001). This analysis demonstrated significant heterogeneity between studies (table 1). Removal of Yun and colleagues35 reduced heterogeneity to nonsignificance (P = .060), and increased the pooled effect size slightly (r = .189, 95% CI = [0.100, 0.274], P = .000). Yun and colleagues’ study measured delusions at entry to an early psychosis service so participants were in the acute stage of their first psychotic episode. This may have introduced a ceiling effect whereby all participants had very severe positive symptoms. Childhood sexual abuse was also associated with delusion severity (7 studies, r = .139, 95% CI = [0.018, 0.256], P = .025). Childhood neglect (physical and emotional) was not significantly associated with delusion severity (5 studies, r = .061, 95% CI = [−0.048, 0.170], P = .272). None of these analyses showed evidence of publication bias.
Fig. 2.
Forest plot showing relationships between delusions and total childhood trauma, childhood sexual abuse and childhood neglect.
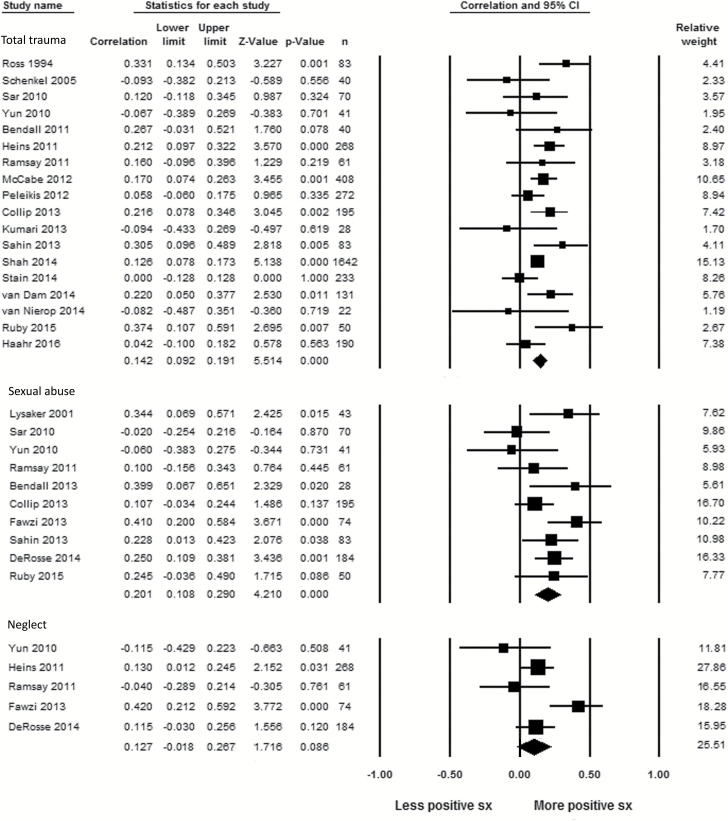
Positive Symptoms
Studies that reported a global measure of positive symptoms were also meta-analyzed. Thirty studies were found (supplementary table 4). Of these, 10 studies collected relevant data that were not reported (supplementary table 4). Childhood sexual abuse, childhood physical abuse, childhood emotional abuse, childhood physical neglect, and childhood emotional neglect data were omitted in between 8 and 9 studies. No studies omitted total childhood trauma data. Meta-analyses revealed that positive symptom severity was associated with total childhood trauma and childhood sexual abuse, but not with childhood neglect (figure 3). Positive symptom severity was associated with total childhood trauma (18 studies, r = .142, 95% CI = [0.092, 0.191], P < .001). There was significant heterogeneity between studies (table 1). Heterogeneity could not be explained by Yun and colleagues35 study as it had with hallucinations as removal of this study did not reduce heterogeneity to nonsignificance. (P = .040). Positive symptoms were also associated with childhood sexual abuse (10 studies, r = .201, 95% CI = [0.108, 0.290], P < .001) without any evidence of heterogeneity. Positive symptoms were not significantly associated with childhood neglect (5 studies, r = .127, 95% CI = [−0.018, 0.267], P = .086) and there was evidence of heterogeneity (table 1). Removing the study of Fawzi and colleagues28 and Yun and colleagues35 from the analysis reduced the point estimate to .106, 95% CI = [0.019, 0.191], P = .017) and removed heterogeneity (P = .491). Fawzi and colleagues’28 measure of “personal identity trauma” was closest to our childhood sexual abuse category but also included physical abuse and mugging and thus may have reflected a slightly different construct to childhood sexual abuse.
Fig. 3.
Forest plot showing relationships between positive symptoms and total childhood trauma, childhood sexual abuse and childhood neglect.
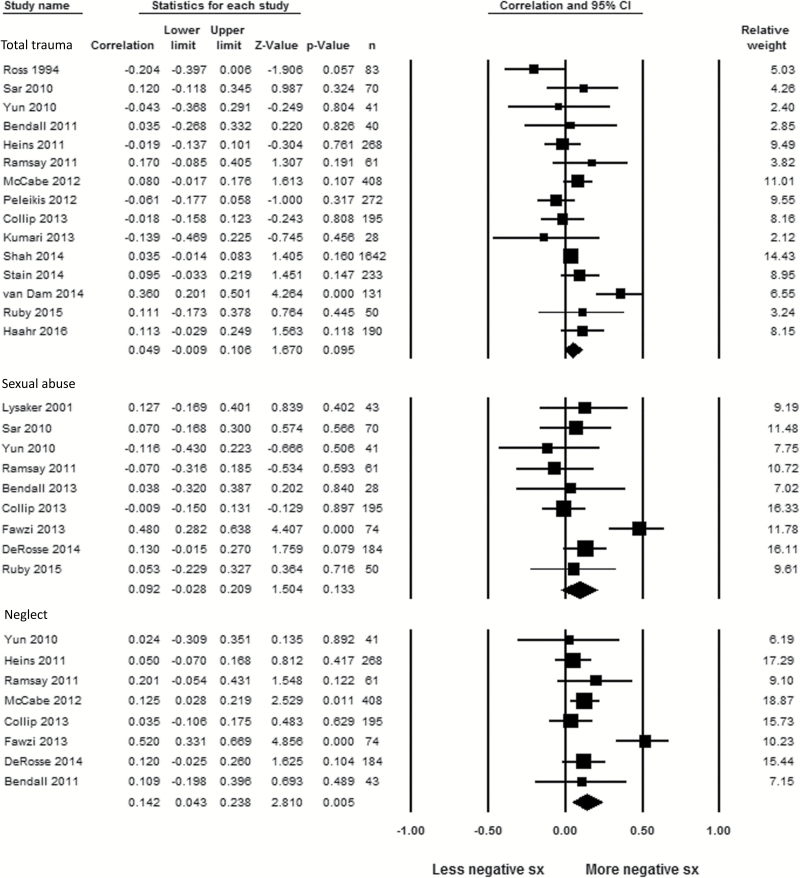
Negative Symptoms
Twenty-eight studies measured relationships between negative symptom severity and childhood trauma (supplementary table 5). Of these, 10 studies collected relevant data that were not reported (supplementary table 5). Childhood sexual abuse, childhood physical abuse, childhood emotional abuse, childhood physical neglect, and childhood emotional neglect data were omitted in between 5 and 8 studies. One study omitted total childhood trauma data. Meta-analyses revealed that negative symptom severity was not associated with total childhood trauma (15 studies; r = .049, 95% CI = [−0.009, 0.106], P = .095) nor with childhood sexual abuse (9 studies; r = .092, 95% CI = [−0.028, 0.209], P = .133), and both of these analyses evinced significant heterogeneity (figure 4). No studies were identified that could have contributed to heterogeneity in the negative symptoms and total childhood trauma meta-analysis. Removing the Fawzi and colleagues’ study28 (see explanation in Positive Symptoms results above) from the childhood sexual abuse analysis removed heterogeneity and the meta-analysis remained nonsignificant.
Fig. 4.
Forest plot showing relationships between negative symptoms and total childhood trauma, childhood sexual abuse and childhood neglect.
Negative symptom severity was significantly associated with childhood neglect (8 studies; r = .142, 95% CI = [0.043, 0.238], P = .005) with evidence of heterogeneity between studies (table 1). Removal of one outlying study, Fawzi and colleagues,28 reduced heterogeneity to nonsignificance, and reduced the meta-analytic estimate (r = .093, 95% CI = [0.036, 0.149], Z = 3.198, P = .001), which remained statistically significant. Fawzi and colleagues’ measure of “attachment trauma” may have reflected a slightly different construct to childhood neglect. There was no evidence of publication bias in any of the meta-analyses.
Summary of Meta-Analysis Results
A summary of the meta-analytic results is presented in table 1.
Discussion
This is the first meta-analysis to confirm that childhood trauma is related to more severe hallucinations and delusions among people with a diagnosed psychotic disorder. Contrary to our hypothesis, a relationship between total childhood trauma and negative symptom severity was not found. This suggests that for those with psychotic disorder, childhood trauma is associated with a symptom picture characterized by more positive symptoms rather than with greater symptom severity in all domains. Conversely, a specific relationship between childhood neglect and more severe negative symptoms, albeit of small magnitude, was found.
Hallucinations
Hallucinations in those with psychotic disorder were found to be related to total childhood trauma, childhood sexual abuse, and neglect. All 3 of the meta-analyses were able to utilize data from the majority of studies that reported on outcomes, with the total childhood trauma and hallucinations analysis able to use the highest proportion (80%). Despite some methodological problems with the available data (with one analysis showing selective reporting and another showing publication bias), the overall pattern of results is consistent and suggests all forms of childhood trauma are associated with more severe hallucinations in those with psychotic disorder.
Delusions
Meta-analytic results supported the hypothesis that childhood trauma would be associated with more severe delusions in those with psychotic disorder. We were able to use 83% of the reviewed studies in this meta-analysis. Childhood sexual abuse was associated with more severe delusions, however, the lower 95% confidence limit for this meta-analysis was 0.018, suggesting a less robust finding. There was no relationship between delusions and childhood neglect. Overall, while the data showed that delusions were associated with childhood trauma, there was a less consistent picture compared to the hallucination result.
Positive Psychotic Symptoms
We repeated the methodology we used to investigate hallucinations and delusions on studies with positive psychotic symptoms as an outcome to further test of our hypotheses with a greater number of studies. While our meta-analysis of the relationship between total childhood trauma and positive psychotic symptoms revealed a significant association, and did include the most studies and participants, it also showed significant heterogeneity, which we cannot explain in terms of specific study characteristics. Positive symptoms were more robustly associated with childhood sexual abuse than neglect, broadly reflecting the hallucinations and delusions results.
Overall, we see robust meta-analytic results for childhood trauma and hallucinations but less robust associations between childhood trauma and delusions and positive symptoms in those with psychotic disorder. This suggests that there may be differences in the relationship of childhood trauma to hallucinations versus delusions, which require further investigation. For example, many theories conceptualizing the relationship between childhood trauma and delusions refer to persecutory delusions, in particular,8 whereas many of the studies in the current review measured delusions a whole. Conversely, theoretical mechanisms linking childhood trauma to hallucinations generalize across all hallucination subtypes (eg, auditory, visual). Childhood trauma is conceptualized to cause more severe hallucinations through source monitoring errors,9,10 whereby intrusive memories12,44 involving low cognitive effort make an individual vulnerable to hallucinations, particularly if they have previously compromised source monitoring.45 Similarly, weak contextual integration during the encoding of highly stressful, traumatic memories may lead to involuntary triggering in those with biological vulnerability.11,46,47 While there is empirical support for some of these theories16,46 but not others,48 a strength of such models is that they provide clearly articulated constructs for testing. The current results support the continuation of rigorous testing, particularly as cognitive models of the development of specific symptoms as a result of trauma form the basis of the most effective treatments for PTSD.49
Negative Symptoms
Negative symptoms of psychosis were not associated with total childhood trauma or childhood sexual abuse in our meta-analyses with relatively large numbers of studies, and little selective reporting bias. While negative symptoms were found to be associated with childhood neglect, it must be noted that 7 studies in the systematic review collected but did not report this data, somewhat undermining the robustness of this finding. The results provide some support for theories that conceptualize a specific relationship between negative symptoms and neglect23,24 and suggest that more general theories regarding the biology of childhood trauma and negative symptoms could be refined.21 The data also provides a springboard for further research investigating specific mechanisms such as genotype, attachments difficulties, and motor retardation, all of which have been found to be important in single studies.22,50,51
Limitations
One limitation of this meta-analysis is the low proportion of included studies that reported all outcomes that were measured, which would have facilitated pooling results in the meta-analyses. This is not a criticism of these studies per se as many were testing specific hypotheses, which did not require the reporting of all data. This underlines the utility of open publication of data sets upon publication of specific studies to make the most use of meta-analytic technologies. Childhood physical abuse and childhood emotional abuse were the traumas least consistently reported (supplementary tables 2–4). If future studies supply open data sets, meta-analytic testing based on raw data of the relationship between childhood physical abuse or childhood emotional abuse and psychotic symptoms will be able to be undertaken.
The quality assessment showed that the included studies often used nonrepresentative samples and failed to report how many participants who were approached actually accepted. These may be particularly problematic in childhood trauma research where participants may be biased towards or biased against participating in research on trauma due to emotional reactions to their trauma experiences.
In all studies meta-analyzed, participants were assessed for the presence of trauma retrospectively, and after the onset of psychosis. Thus, reporting of trauma may be compromised by recall error or bias, which could overestimate the relationship between childhood trauma and symptoms.52 While prospective data collection reduces these problems, it has its own limitations.1 Importantly also, trauma reporting of those with psychosis is known to be reliable,40 and associations between trauma and psychosis have been found consistently in a variety of study designs, including in prospective studies.20
Few studies in the review adjusted for potential confounders, studies used different childhood trauma and psychopathology measures, and most studies measured symptom severity at only one time-point, all of which limit the conclusions that can be drawn from the results.
There was a time lag between the systematic literature search and submission for publication, which means newer studies were not included in the analysis. This was due to the large number of articles identified by the literature search and the extensive search for data collected but not reported in identified studies. However, the methodological rigor of the search methodology was essential in reducing bias within the reviewed studies and outweighs problems of lack of timeliness of the analysis.
Directions for Future Research
Investigation of the possible distinct roles of childhood abuse (sexual, physical, and emotional) and neglect in relation to hallucinations, delusions, and negative symptoms is a valuable area for future research. Many theories of the relationship between child trauma and hallucinations and delusions conceptualize the abusive traumas rather than the neglectful ones.9,11,12,44,46 Broad theories of the impact of trauma on the brain do not conceptualize differential impacts within the abusive traumas but some do conceptualize the abusive and the neglectful traumas as having differential psychobiological impacts.53 Our study methodology was not able to clearly define differential effects between the abusive and neglectful traumas. That said, our results for delusions and positive symptoms, which show significant association with both childhood trauma and childhood sexual abuse but no association with neglect lend tentative support for the notion that it is the abusive traumas that are driving the association seen in the childhood trauma outcome. This is not the case for hallucinations where an association was also found for neglect. However, abusive and neglectful experiences have been found to be highly correlated in psychosis so it may be that abuse is confounding the relationship found with neglect.4 Conversely, there is contention as to whether abuse and neglect constructs can be differentiated statistically in psychosis and so this should be established before further hypothesis testing in this area.4 One such analysis found physical and emotional abuse factored together but not parental sexual abuse.30 If separate childhood abuse and neglect constructs are valid, studies may need to use statistical procedures such as hierarchical regression to partial out the effect of abuse from neglect and vice versa. This suggestion is in contrast to some current research methodologies that are conceptualizing specific traumas (such as physical abuse or sexual abuse) as impacting specific symptoms.13 Future meta-analytic research should also focus on measuring any differences in strength of association between childhood trauma and hallucinations and delusions across the psychosis continuum from hallucinations and delusions in nonclinical samples through first-episode psychosis to chronic disorder.
Clinical Implications
To date clinical interventions to treat trauma in psychotic disorders have mainly focused on the treatment of post-traumatic stress disorder (PTSD).54 The current study shows that childhood trauma is associated with psychotic symptoms themselves, suggesting that trauma-focused interventions for the symptoms of psychosis should be developed and trialed. In terms of positive symptoms, this will involve the development and testing of further theories in order to build an empirically supported theoretical model of the relationship between trauma exposure and symptomology as exists in PTSD.49 The finding that childhood neglect was associated with negative symptoms has important implications for treatment. Negative symptoms have been resistant to both medication and psychotherapeutic interventions, and there is a need to isolate mechanisms to progress intervention research.55 This meta-analysis suggests that further exploration of the mechanisms (such as attachment) that mediate the relationship between neglect and negative symptoms and trialing treatments that address those mechanisms may be important. Finally, these results have implications for a trauma-informed approach to psychosis service-delivery, as those with more severe psychotic symptoms are more likely to have experienced childhood trauma. Clinical guidelines require sensitive assessment of trauma and its effects for those with psychosis.56,57 However, clinicians lack confidence assessing and treating trauma in psychosis, and psychotic symptom exacerbation can occur in trauma interventions despite the efficacy of evidence-based treatment for PTSD in groups with psychosis.54,58,59 More research and training in how to assess and treat the effects of trauma sensitively and effectively is essential to the delivery of trauma-informed services for psychosis.
Conclusion
In conclusion, our findings show that childhood trauma is associated with specific symptomatology within psychotic disorders. Establishing this meta-analytic evidence is a crucial step toward refining the mechanisms by which these effects are theorized to occur. It also brings into sharp relief the need to develop tailored clinical interventions to sensitively and effectively treat those with psychosis who have experienced childhood trauma.
Supplementary Material
Supplementary data are available at Schizophrenia Bulletin online.
Funding
S.B. and M.A.-J. were supported by fellowships from the National Health and Medical Research Council. A.M.G.-S was supported by a fellowship from Alicia Koplowitz Foundation (Spain). Funding for the study was received from Australian Rotary Health.
Supplementary Material
Acknowledgments
The authors wish to thank investigators who provided additional information including A/Prof. Green, Asst/Prof. Heins, Prof. Kelly, Dr McCabe, A/Prof. Perona-Garcelán, Dr Phassouliotis, A/Prof. Phillips, Dr Ruby, Prof. Sar, Dr Sporle, Dr van Nierop, and Asst/Prof. Waterreus. Thanks to Dr Kelly Allott for reviewing drafts of the manuscript. The authors identified no conflicts of interest.
References
- 1. Bendall S, Jackson HJ, Hulbert CA, McGorry PD. Childhood trauma and psychotic disorders: a systematic, critical review of the evidence. Schizophr Bull. 2008;34:568–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Varese F, Smeets F, Drukker M, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012;38:661–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kelleher I, Keeley H, Corcoran P, et al. Childhood trauma and psychosis in a prospective cohort study: cause, effect, and directionality. Am J Psychiatry. 2013;170:734–741. [DOI] [PubMed] [Google Scholar]
- 4. Trauelsen AM, Bendall S, Jansen JE, et al. Childhood adversity specificity and dose-response effect in non-affective first-episode psychosis. Schizophr Res. 2015;165:52–59. [DOI] [PubMed] [Google Scholar]
- 5. Murray RM. Mistakes I have made in my research career. Schizophr Bull. 2017;43:253–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Carpenter WT. Shifting paradigms and the term schizophrenia. Schizophr Bull. 2016;42:863–864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hardy A. Pathways from trauma to psychotic experiences: a theoretically informed model of posttraumatic stress in psychosis. Front Psychol. 2017;8:697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bentall RP, de Sousa P, Varese F, et al. From adversity to psychosis: pathways and mechanisms from specific adversities to specific symptoms. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1011–1022. [DOI] [PubMed] [Google Scholar]
- 9. Garety PA, Kuipers E, Fowler D, Freeman D, Bebbington PE. A cognitive model of the positive symptoms of psychosis. Psychol Med. 2001;31:189–195. [DOI] [PubMed] [Google Scholar]
- 10. Bentall RP. The illusion of reality: a review and integration of psychological research on hallucinations. Psychol Bull. 1990;107:82–95. [DOI] [PubMed] [Google Scholar]
- 11. Steel C, Fowler D, Holmes EA. Trauma-related intrusions and psychosis: an information processing account. Behav Cogn Psychother. 2005;33:139–152. [Google Scholar]
- 12. Morrison AP. The interpretation of intrusions in psychosis: an integrative cognitive approach to hallucinations and delusions. 2001;29:257–276. [Google Scholar]
- 13. Hardy A, Emsley R, Freeman D, et al. Psychological mechanisms mediating effects between trauma and psychotic symptoms: the role of affect regulation, intrusive trauma memory, beliefs, and depression. Schizophr Bull. 2016;42(suppl 1):S34–S43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Varese F, Barkus E, Bentall RP. Dissociation mediates the relationship between childhood trauma and hallucination-proneness. Psychol Med. 2012;42:1025–1036. [DOI] [PubMed] [Google Scholar]
- 15. Perona-Garcelán S, Carrascoso-López F, García-Montes JM, et al. Dissociative experiences as mediators between childhood trauma and auditory hallucinations. J Trauma Stress. 2012;25:323–329. [DOI] [PubMed] [Google Scholar]
- 16. Bendall S, Hulbert CA, Alvarez-Jimenez M, Allott K, McGorry PD, Jackson HJ. Testing a model of the relationship between childhood sexual abuse and psychosis in a first-episode psychosis group: the role of hallucinations and delusions, posttraumatic intrusions, and selective attention. J Nerv Ment Dis. 2013;201:941–947. [DOI] [PubMed] [Google Scholar]
- 17. Freeman D, Garety PA, Kuipers E, Fowler D, Bebbington PE. A cognitive model of persecutory delusions. Br J Clin Psychol. 2002;41:331–347. [DOI] [PubMed] [Google Scholar]
- 18. Bentall RP, Corcoran R, Howard R, Blackwood N, Kinderman P. Persecutory delusions: a review and theoretical integration. Clin Psychol Rev. 2001;21:1143–1192. [DOI] [PubMed] [Google Scholar]
- 19. Baer JC, Martinez CD. Child maltreatment and insecure attachment: a meta-analysis. J Reprod Infant Psychol. 2006;24:187–197. [Google Scholar]
- 20. Bentall RP, Wickham S, Shevlin M, Varese F. Do specific early-life adversities lead to specific symptoms of psychosis? A study from the 2007 the Adult Psychiatric Morbidity Survey. Schizophr Bull. 2012;38:734–740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Read J, Perry BD, Moskowitz A, Connolly J. The contribution of early traumatic events to schizophrenia in some patients: a traumagenic neurodevelopmental model. Psychiatry. 2001;64:319–345. [DOI] [PubMed] [Google Scholar]
- 22. van Dam DS, Korver-Nieberg N, Velthorst E, Meijer CJ, de Haan L; For Genetic Risk and Outcome in Psychosis (GROUP). Childhood maltreatment, adult attachment and psychotic symptomatology: a study in patients, siblings and controls. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1759–1767. [DOI] [PubMed] [Google Scholar]
- 23. Liotti G, Gumley A. An attachment perspective on schizophrenia: the role of disorganized attachment, dissociation and mentalization. Psychosis, trauma and dissociation: emerging perspectives on severe psychopathology. In: Moskowitz A, Dorahy M, Schaefer I, eds. Psychosis, Trauma and Dissociation. New York, NY: Wiley; 2008:117–133. [Google Scholar]
- 24. Gallagher BJ III, Jones BJ. Childhood stressors and symptoms of schizophrenia. Clin Schizophr Relat Psychoses. 2013;7:124–130. [DOI] [PubMed] [Google Scholar]
- 25. Bendall S, Alvarez-Jimenez M, Nelson B, McGorry P. Childhood trauma and psychosis: new perspectives on aetiology and treatment. Early Interv Psychiatry. 2013;7:1–4. [DOI] [PubMed] [Google Scholar]
- 26. Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. [DOI] [PubMed] [Google Scholar]
- 27. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Fawzi MH, Kira IA, Fawzi MM Jr, Mohamed HE, Fawzi MM. Trauma profile in Egyptian adolescents with first-episode schizophrenia: relation to psychopathology and plasma brain-derived neurotrophic factor. J Nerv Ment Dis. 2013;201:23–29. [DOI] [PubMed] [Google Scholar]
- 29. Heins M, Simons C, Lataster T, et al. Childhood trauma and psychosis: a case–control and case-sibling comparison across different levels of genetic liability, psychopathology, and type of trauma. Am J Psychiatry. 2011;168:1286–1294. [DOI] [PubMed] [Google Scholar]
- 30. McCabe KL, Maloney EA, Stain HJ, Loughland CM, Carr VJ. Relationship between childhood adversity and clinical and cognitive features in schizophrenia. J Psychiatr Res. 2012;46:600–607. [DOI] [PubMed] [Google Scholar]
- 31. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Borenstein M, Hedges LV, Higgins JPT, Rothstein H.. Comprehensive meta-analysis. Englewood, NJ: Biostat, Inc; 2005. [Google Scholar]
- 33. Borenstein M, Hedges LV, Higgins JPT.. Introduction to Meta-Analysis. Hoboken, NJ: John Wiley & Sons; 2009. [Google Scholar]
- 34. Goff DC, Brotman AW, Kindlon D, Waites M, Amico E. Self-reports of childhood abuse in chronically psychotic patients. Psychiatry Res. 1991;37:73–80. [DOI] [PubMed] [Google Scholar]
- 35. Yun Y, Parslow R, Garner B, et al. Childhood trauma and psychosis in the first episode psychotic population: results from the SHARP study. Early Interv Psychiatry. 2010;4(suppl 1):80. [Google Scholar]
- 36. Mason OJ, Brett E, Collinge M, Curr H, Rhodes J. Childhood abuse and the content of delusions. Child Abuse Negl. 2009;33:205–208. [DOI] [PubMed] [Google Scholar]
- 37. Reiff M, Castille DM, Muenzenmaier K, Link B. Childhood abuse and the content of adult psychotic symptoms. Psychol Trauma. 2012;4:356–369. [Google Scholar]
- 38. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Rosenthal R. The file drawer problem and tolerance for null results. Psychol Bull. 1979;86:638–641. [Google Scholar]
- 40. Fisher HL, McGuffin P, Boydell J, et al. Interplay between childhood physical abuse and familial risk in the onset of psychotic disorders. Schizophr Bull. 2014;40:1443–1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Haahr UH, Larsen T, Simonsen E, et al. Relation between premorbid adjustment, duration of untreated psychosis and close interpersonal trauma in first-episode psychosis. Early Interv Psychiatry. 2016; doi:10.1111/eip.12315. [DOI] [PubMed] [Google Scholar]
- 42. Hoy K, Barrett S, Shannon C, et al. Childhood trauma and hippocampal and amygdalar volumes in first-episode psychosis. Schizophr Bull. 2012;38:1162–1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Lysaker PH, Beattie NL, Strasburger AM, Davis LW. Reported history of child sexual abuse in schizophrenia: associations with heightened symptom levels and poorer participation over four months in vocational rehabilitation. J Nerv Ment Dis. 2005;193:790–795. [DOI] [PubMed] [Google Scholar]
- 44. Hammersley P, Dias A, Todd G, Bowen-Jones K, Reilly B, Bentall RP. Childhood trauma and hallucinations in bipolar affective disorder: preliminary investigation. Br J Psychiatry. 2003;182:543–547. [DOI] [PubMed] [Google Scholar]
- 45. Bentall RP, Swarbrick R. The best laid schemas of paranoid patients: autonomy, sociotropy and need for closure. Psychol Psychother. 2003;76:163–171. [DOI] [PubMed] [Google Scholar]
- 46. Holmes EA, Steel C. Schizotypy: a vulnerability factor for traumatic intrusions. J Nerv Ment Dis. 2004;192:28–34. [DOI] [PubMed] [Google Scholar]
- 47. Steel C, Hemsley DR, Pickering AD. Distractor cueing effects on choice reaction time and their relationship with schizotypal personality. Br J Clin Psychol. 2002;41:143–156. [DOI] [PubMed] [Google Scholar]
- 48. Bendall S, Jackson HJ, Hulbert CA. What self-generated speech is externally misattributed in psychosis? Testing three cognitive models in a first-episode sample. Schizophr Res. 2011;129:36–41. [DOI] [PubMed] [Google Scholar]
- 49. Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behav Res Ther. 2000;38:319–345. [DOI] [PubMed] [Google Scholar]
- 50. Green MJ, Chia TY, Cairns MJ, et al. ; Australian Schizophrenia Research Bank Catechol-O-methyltransferase (COMT) genotype moderates the effects of childhood trauma on cognition and symptoms in schizophrenia. J Psychiatr Res. 2014;49:43–50. [DOI] [PubMed] [Google Scholar]
- 51. Isvoranu A-M, van Borkulo CD, Boyette L-L, Wigman JTW, Vinkers CH, Borsboom D; Group Investigators A network approach to psychosis: pathways between childhood trauma and psychotic symptoms. Schizophr Bull. 2016;43:187–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Reuben AM, Moffitt TE, Caspi A, Belsky DW, et al. Lest we forget: comparing retrospective and prospective assessments of adverse childhood experiences in the prediction of adult health. J Child Psychol Psychiatry. 2016;57:1103–1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Perry B. Child maltreatment: a neurodevelopmental perspective on the role of trauma and neglect in psychopathology. In: Beauchaine TP, Hinshaw SP, ed. Child and Adolescent Psychopathology. Somerset, NJ: John Wiley & Sons; 2008:93–128. [Google Scholar]
- 54. van den Berg DPG, de Bont PAJM, van der Vleugel BM, et al. Prolonged exposure vs eye movement desensitization and reprocessing vs waiting list for posttraumatic stress disorder in patients with a psychotic disorder: a randomized clinical trial. JAMA Psychiatry. 2015;72:259–267. [DOI] [PubMed] [Google Scholar]
- 55. Fusar-Poli P, Papanastasiou E, Stahl D, et al. Treatments of negative symptoms in schizophrenia: meta-analysis of 168 randomized placebo-controlled trials. Schizophr Bull. 2015;41:892–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. NICE. Psychosis and Schizophrenia in Children and Young People: Baseline Assessment Tool. London: National Institute for Clinical Excellence; 2013. [Google Scholar]
- 57. Galletly C, Castle D, Dark F, et al. Clinical practice guideline for the management of schizophrenia and related disorders. Aust N Z J Psychiatry. 2016;50:1–117. [DOI] [PubMed] [Google Scholar]
- 58. Tong J, Simpson K, Alvarez-Jimenez M, Bendall S. Distress, psychotic symptom exacerbation, and relief in reaction to talking about trauma in the context of beneficial trauma therapy: perspectives from young people with posttraumatic stress disorder and first episode psychosis. Behav Cogn Psychother. 2017;1–16. doi:10.1017/S1352465817000236. [DOI] [PubMed] [Google Scholar]
- 59. Gairns S, Alvarez-Jimenez M, Hulbert C, McGorry P, Bendall S. Perceptions of clinicians treating young people with first-episode psychosis for post-traumatic stress disorder. Early Interv Psychiatry. 2015;9:12–20. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.