Abstract
Objective
In this study, our aim was to investigate the efficacy and sufficiency of bispectral indeks (BIS) guided remifentanil-desflurane anaesthesia on intraoperative haemodynamic stability in both normotensive and hypertensive patients undergoing off-pump coronary artery bypass surgery.
Methods
Thirty adult, ASA I–III patients undergoing elective off-pump coronary surgery were included in the study. According to the presence of essential hypertension preoperatively, patients were divided into two groups. Haemodynamic parameters were recorded at 11 time points during the operation.
Results
There were no differences in the demographic data, heart rate and intraoperative and postoperative parameters between the groups. Arterial blood pressure and additional requirement of remifentanil were found to be significantly higher in the hypertensive group intraoperatively.
Conclusion
In patients undergoing off-pump coronary revascularisation surgery, intraoperative haemodynamic stabilisation with remifentanil–desflurane anaesthesia under BIS guidance was safely provided, but higher remifentanil doses were required in hypertensive patients.
Keywords: Desflurane, remifentanil, fast-track anaesthesia, off-pumpcardiac surgery, off-pump coronary revascularisation, hypertension, haemodynamic stabilisation, anaesthesia
Introduction
In patients undergoing off-pump coronary artery bypass surgery (OPCAB), the primary goal of anaesthesiologists is to provide maximal myocardial protection while ensuring a safe anaesthesia induction and administration without benefiting from the protective effects of hypothermia and without the pump support (1, 2). Especially in hypertensive patients, providing a haemodynamic stability sufficient enough to protect coronary perfusion is one of the goals. The use of short-acting and easily titratable agents in fast-track anaesthesia is more suitable for early extubation. For this purpose, low-dose fentanyl or short-acting opioids such as remifentanil and sufentanil are used in various combinations (3). Remifentanil is the first ultra-short acting opioid that can be titrated rapidly at various surgical stimulations. It provides deep intraoperative analgesia and haemodynamic stability, as well as early extubation and recovery (4). Desflurane, which is an inhalation anaesthetic, with a low blood–gas solubility provides a fast response time and a fast wake-up time. This low solubility allows an easy adjustment of the depth of anaesthesia and a better haemodynamic stability during operation. Desflurane–remifentanil anaesthesia is now the fastest anaesthetic combination that provides the fastest recovery (5, 6).
The bispectral index (BIS) monitoring allows to titrate the hypnotic component of anaesthesia, reduce unnecessary drug consumption, improve recovery and reduce unwanted side effects such as haemodynamic instability (7).
In this study, the primary goal was to investigate the effects of desflurane–remifentanil anaesthesia under the guidance of BIS on the intraoperative haemodynamics among two groups of normotensive and hypertensive patients who underwent OPCAB surgery. Patients’ extubation time, intensive care and hospital stay duration, and postoperative complications were evaluated as secondary goals.
Methods
Selection of patients
This study included 30 adult patients classified as Groups II and III according to the American Society of Anesthesiologists, who would undergo elective OPCAB surgeries, having obtained an approval from the Yuksek Ihtisas Training and Research Hospital Ethics Committee (222 no., 14 May 2009) and the written consents of the patients. Patients with an active neurological disease, active or previous cerebrovascular disease, with ejection fraction (EF) <40% and arrhythmia, patients in whom a preoperative inotropic agent and intra-aortic balloon pump were used, those who underwent a valve replacement or other surgical procedures, and those susceptible to opioids were excluded. Patients were divided into two groups of 15 patients according whether they were diagnosed with primary essential hypertension and whether they were receiving treatment: Group N (normotensive patients) and Group H (hypertensive patients). Patients who met the conditions were included in the study. All the patients were evaluated the day before the operation, and they were informed about the study and the anaesthetic techniques to be applied, and their approval was obtained. The age, gender, body mass index (BMI), EF, Euroscore value, chronic diseases and medications were recorded preoperatively. As premedication, 5–10 mg oral diazepam was given the night before surgery and 0.1 mg intramuscular morphine HCl was applied 30 minutes before induction.
Monitoring
Routine monitoring of the patients (electrocardiography, pulse oximeter, noninvasive arterial blood pressure) was performed before the induction of anaesthesia in the operation theatre. Two peripheral venous accesses were established (18 and 16 gauge), and invasive arterial blood pressure monitoring was initiated by performing radial artery cannulation. Following endotracheal intubation, a nasopharyngeal probe was inserted to monitor the body temperature, and internal jugular venous cannulation was applied to monitor the central venous pressure. Each patient was monitored with BIS, as well as routine cardiac surgery anaesthesia monitoring. For bispectral index monitoring, a BIS module (BIS, Inc. S/5 monitor module, Datex-Ohmeda Madison, WI, USA) and a BIS sensor (BIStm Quatro, Aspect Medical Systems, Inc., Newton, MA USA) were used. For BIS monitoring, the forehead and temple skin were cleaned with an alcohol buffer and dabbed. The electrode no. 1 was placed on the patient’s forehead approximately 5 cm above the nose bridge, the electrode no. 3 was placed on the left temporal region in the middle of the eye corner and the hair line, the electrode no. 4 was placed right above the eyebrow, and the electrode no. 2 was placed between the electrodes no. 1 and no. 4. By applying pressure to the electrodes for 5–10 seconds, it was observed on the monitor that the impedance of all the electrodes was below 5000 Ohm in the impedance test.
Anaesthesia application
Patients were hydrated with isotonic saline solution (5 mL kg−1) prior to the anaesthesia induction. Following 3 minutes of preoxygenation and induction of anaesthesia, a 4-minute infusion of remifentanil (2.5 μg kg−1) with midazolam (0.1 mg kg−1) was administered. Muscle relaxation was achieved with rocuronium (0.6 mg kg−1). When BIS was lower than 60, the mechanical ventilation was initiated following the endotracheal intubation.
All the patients were mechanically ventilated with a tidal volume of 7 mL kg−1 and a respiratory frequency set to keep EtCO2 levels between 35–40 mmHg. In both groups, anaesthesia administration was achieved with desflurane and remifentanil infusion (0.125 μg kg−1 min−1) in a mixture of oxygen/air (1 L/1 L) with a BIS value ranging between 30 and 60. The concentration of the anaesthetic gases was monitored with a Draeger Primus anaesthesia device (Draeger, Medizintechnik, Germany). As CO2 absorbent, soda lime (Sorbo-Lime, Berkum, Turkey) was used. As the anaesthetic gas concentration changed, the Primus device was used to recalculate the minimum alveolar concentration (MAC) taking the age adjustment, height verification and the calculation of the mixture of other gases into account. However, it could not calculate a condition that reduces the MAC, such as opioid use. Since it is not possible to monitor all these variables instantaneously, the MAC values were monitored and evaluated to give general information about the groups in this study. It was planned to increase the inspired concentration of desflurane by 1% during the operation when the BIS value approached 60 and the mean arterial pressure and heart rate increased. It was also planned that the inspired concentration of desflurane would be reduced by 1% when the BIS value approached 30 and the mean arterial pressure and heart rate decreased. To establish the targeted haemodynamic conditions, desflurane inhalation and remifentanil infusion and bolus applications were performed by increasing and/or decreasing the desflurane percentage, while the flow rate was 2 L min−1 based on the BIS value. Muscle relaxation was maintained with rocuronium (0.3 mg kg−1) applied at 30–45 min intervals. Compared to the values in the beginning, when the mean arterial pressure (MAP) and heart rate (HR) increased by 20% while BIS ranged between 30 and 60, without changing the infusion dose, 0.1 μg kg−1 of remifentanil intravenously was applied, and after 2 minutes, the values were checked, and if the blood pressure kept increasing, a dose of 0.1 μg kg−1 remifentanil intravenously was repeated. In case of high blood pressure values despite the increased desflurane concentration and remifentanil additions, administration of nitroglycerin was planned. When the BIS ranged between 30 and 60, and the MAP and CAD decreased by 20% compared to the beginning, without changing the remifentanil infusion dose, the infusion of fluid was increased, and the values were checked after 2 minutes. If the decrease continued, they were tried to be elevated by intravenous ephedrine (5 mg) application.
Measurement periods and parameters
The mean systolic–diastolic arterial pressure, HR and BIS values were recorded before the induction of anaesthesia (T1); 4 minutes after the induction of anaesthesia (T2); 3 minutes after the endotracheal intubation (T3); 3 minutes after skin incision (T4); 3 min after sternotomy (T5); during the left internal mammary artery dissection (T6); after systemic heparinisation (T7); during coronary vascular anastomoses (T8); during haemostasis (T9); during the sternum closure (T10); and at the end of the operation (T11).
Surgical method
All patients were subjected to the standard OPCAB cardiopulmonary bypass (CPB) technique. Anticoagulation was provided with 100 IU kg−1 heparin with an activated clotting time of over 250 seconds before the onset of coronary vascular anastomoses. The number of coronary vascular anastomoses, duration and duration of surgery were recorded. At the end of the surgery, the patients were transferred to the intensive care unit.
Postoperative care process
During the first hour of intensive care, remifentanil dose was cut in half and the infusion continued. In addition, 20 mg intravenous+1 mg kg−1 intramuscular tramadol was administered when the skin was closed. Tramadol was continued to be administered when required. Patients in vigilant and communicable status, whose muscle strength maintained, with the fraction of inspired oxygen of 40%, arterial partial pressure oxygen over 80 mmHg, arterial partial carbon dioxide pressure below 45 mmHg, stable haemodynamic and metabolic parameters, hourly drainage less than 50 mL per hour, and no tremor were extubated. The duration of postoperative extubation, intensive care unit stay, chest tube drainages and hospital stay were recorded.
Statistical analysis
The Statistical Package for Social Science 15-packet programme (SPSS Inc., Chicago, IL, USA) was used for data analysis. The compliance of distribution of the data with the normal distribution was examined with the Shapiro–Wilk test. The data obtained with descriptive statistical measurements were shown as the mean±standard deviation, and for the nominal variables, the number of observations and percentage (%) were used. Student’s t test was used to determine whether the mean difference of the variables between the groups was statistically significant, and the significance of the difference of non-normally distributed continuous variables was investigated with the Mann–Whitney U test. Whether there was a statistically significant difference between recurrent measurements within the groups was assessed with the Friedman test if the number of repeated measurements was greater than two. When the Friedman test statistics outcome was significant, with the Wilcoxon Sign test, multiple comparisons were performed to determine the measurement times that caused the difference. The significance of the difference between the two measures was assessed by the dependent t test or the Wilcoxon Sign test when the number of recurrent measurements was two within the groups. Nominal variables were compared using the Pearson Chi-square or Fisher’s Full Result Probability test. For p<0.05, the results were considered to be statistically significant. In all possible intra-group and multiple comparisons, the Bonferroni correction was applied to control the Type I error.
Results
One patient was excluded due to hypotension and bradycardia requiring an interruption of remifentanil infusion following the induction of anaesthesia. A total of 30 patients were included in the study, 15 patients in each group. There were no statistically significant differences between the groups in terms of gender, age, additional disease, Euroscore values and the EF percentages. When the two groups were compared, the BMI measurements were significantly lower in the normotensive group (p<0.001) (Table 1).
Table 1.
Demographic characteristics of patients
| Group N (n=15) Normotensive |
Group H (n=15) Hypertensivesif |
p | |
|---|---|---|---|
| Age (year) (Mean±SD) | 55.46±13.21 | 59.60±9.88 | 0.340 |
| Gender (F/M) | 3/12 | 5/10 | 0.682 |
| Body mass index (Mean±SD) | 24.98±2.62* | 31.80±5.18 | 0.000 |
| Ejection fraction (%)(Mean±SD) | 50.53±7.41 | 53±6.51 | 0.341 |
| Euroscore | 3.53±2.16 | 4.53±1.30 | 0.116 |
| Diabetes mellitus (%) | 46.7 (n=7) | 53.3 (n=8) | 0.715 |
| Chronic obstructive pulmonary disease (%) | 0 (n=0) | 20 (n=3) | 0.224 |
| Goitre (%) | 6.7 (n=1) | 6.7 (n=1) | 1 |
p<0.001: When the two groups were compared.
SD: standard deviation
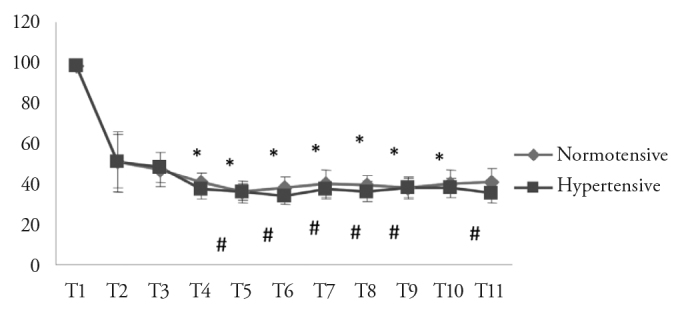
The HR during the patients’ intraoperative measurement periods did not differ between the groups (Figure 1). The MAP values in normotensive patients were found to be significantly lower 3 minutes after the skin incision, 3 minutes after sternotomy, during the anastomosis and sternum closure periods (p<0.05; Figure 2). There was a statistically significant decrease during. The systolic arterial pressure values in normotensive patients were found to be significantly lower 4 minutes after the basal induction of anaesthesia, 3 minutes after the skin incision, 3 minutes after sternotomy, during the anastomosis and sternum closure periods (p<0.05; Figure 3). Diastolic arterial pressure values were significantly lower in normotensive patients 3 minutes after the skin incision and 3 minutes after sternotomy (p<0.05; Figure 4).
Figure 1.
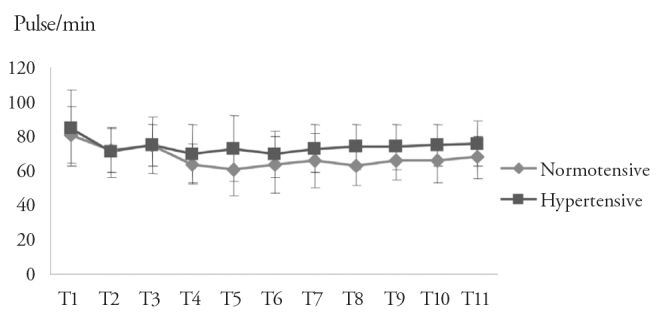
Changes in the heart rate during the measurement periods in both groups
Measurement times: T1: before induction; T2: 4 minutes after induction; T3: 3 minutes after intubation; T4: 3 minutes after the skin incision; T5: 3 minutes after sternotomy; T6: the removal stage of the left internal mammary artery; T7: after heparinisation; T8: during anastomosis; T9: during haemostasis; T10: the chest closure period; T11: the end of operation
Figure 2.
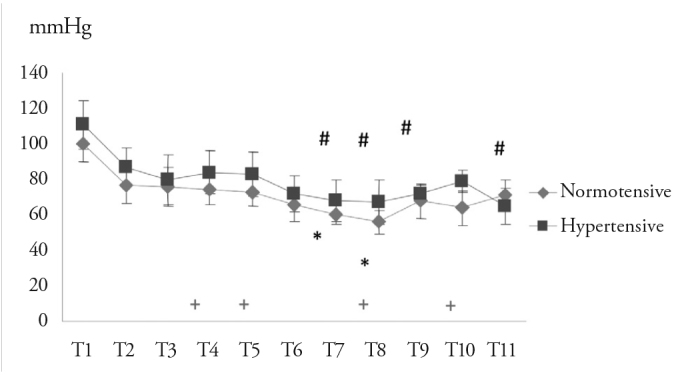
Changes in the mean arterial pressure during the measurement periods in both groups
Measurement times: T1: before induction, T2: 4 minutes after induction, T3: 3 minutes after intubation, T4: 3 minutes after the skin incision, T5: 3 minutes after sternotomy, T6: the removal stage of the left internal mammary artery, T7: after heparinisation, T8: during anastomosis, T9: during haemostasis, T10: the chest closure period, T11: the end of operation
+p<0.05: When the two groups were compared (according to the Bonferroni correction, p<0.004 was considered statistically significant).
Intra-group significance compared to second measurement period
Figure 3.
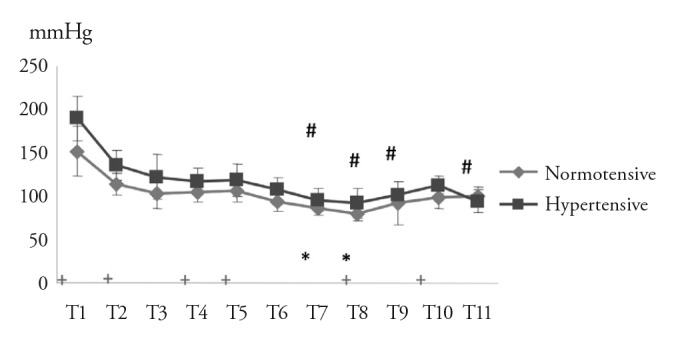
Changes in the systolic arterial pressure during the measurement periods in both groups
Measurement times: T1: before induction, T2: 4 minutes after induction, T3: 3 minutes after intubation, T4: 3 minutes after the skin incision, T5: 3 minutes after sternotomy, T6: the removal stage of the left internal mammary artery, T7: after heparinisation, T8: during anastomosis, T9: during haemostasis, T10: the chest closure period, T11: the end of operation
+p<0.05: When the two groups were compared (according to the Bonferroni correction, p<0.004 was considered statistically significant)
Intra-group significance compared to second measurement period
Figure 4.
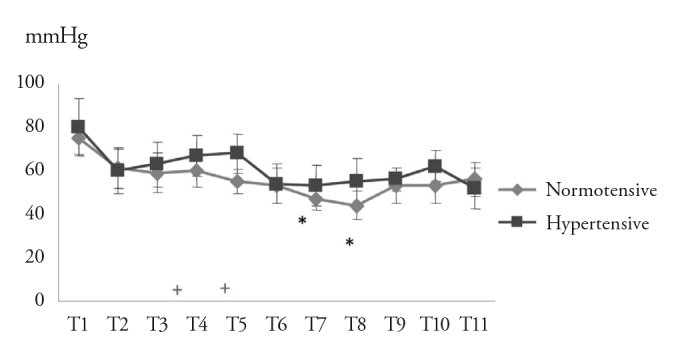
Change of the diastolic arterial pressure during the measurement periods in both groups
Measurement times: T1: before induction, T2: 4 minutes after induction, T3: 3 minutes after intubation, T4: 3 minutes after the skin incision, T5: 3 minutes after sternotomy, T6: the removal stage of the left internal mammary artery, T7: after heparinisation, T8: during anastomosis, T9: during haemostasis, T10: the chest closure period, T11: the end of operation
+p<0.05: When the two groups were compared (according to the Bonferroni correction, p<0.004 was considered statistically significant)
*(Group N), p<0.01: Intra-group significance compared to second measurement period
There was no statistically significant difference between the two groups in terms of the BIS and MAC values (Figures. 5, 6). Attempts to manually change the desflurane concentration were not recorded, but the MAC values that indirectly reflected this were recorded. Although there was no significant difference, to provide the BIS value ranging between 30 and 60 in Group H, higher concentrations of desflurane were needed throughout the operation, and the corresponding MAC value to this concentration was higher compared to Group N. Additional drug requirements were recorded from the beginning of induction of anaesthesia until the completion of the operation. There was a significant difference between groups in terms of an additional drug required during anastomosis. The amount of additional remifentanil applied in Group H was significantly higher than in Group N (Table 2). However, the nitroglycerin administration was not necessary in any patient. Ephedrine was administered to 1 patient due to remifentanil-associated hypotension in the hypertensive group.
Figure 5.
The change of the bispectral index values during the measurement periods in both groups
Measurement times: T1: before induction, T2: 4 minutes after induction, T3: 3 minutes after intubation, T4: 3 minutes after the skin incision, T5: 3 minutes after sternotomy, T6: the removal stage of the left internal mammary artery, T7: after heparinisation, T8: during anastomosis, T9: during haemostasis, T10: the chest closure period, T11: the end of operation
+p<0.05: When the two groups were compared (according to the Bonferroni correction, p<0.004 was considered significant)
Intra-group significance compared to second measurement period
Figure 6.
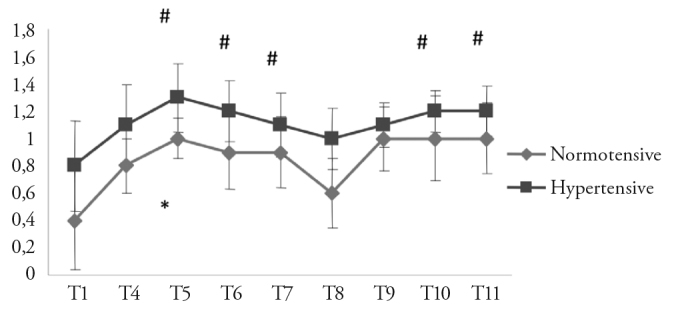
Changes in the minimum alveolar concentration values during the measurement periods in both groups
Measurement times: T1: before induction, T2: 4 minutes after induction, T3: 3 minutes after intubation, T4: 3 minutes after the skin incision, T5: 3 minutes after sternotomy, T6: the removal stage of the left internal mammary artery, T7: after heparinisation, T8: during anastomosis, T9: during haemostasis, T10: the chest closure period, T11: the end of operation
+p<0.05: When the two groups were compared (according to the Bonferroni correction, p<0.004 was considered statistically significant)
Intra-group significance compared to second measurement period
Table 2.
Number of patients requiring additional medication
| Group N (n=15) | Group H (n=15) | p | |
|---|---|---|---|
| 4 minutes after induction | 0 | 4 | 0.100 |
| 3 minutes after intubation | 1 | 3 | 0.598 |
| 3 minutes after skin incision | 0 | 1 | 1 |
| 3 minutes after sternotomy | 0 | 3 | 0.224 |
| LIMA period | 0 | 1 | 1 |
| After heparinisation | 0 | 0 | |
| During anastomosis | 0 + | 11 | 0.000 |
| During haemostasis | 0 | 0 | |
| During sternum closure | 0 | 0 | |
| At the end of the operation | 0 | 0 |
p<0.001: When the two groups were compared (according to the Bonferroni correction, p<0.004 was considered as statistically significant).
In Group N, the ephedrine application in 1 patient at T3 was required due to hypotension; the ephedrine application in 1 patient in Group H during anastomosis was required due to hypotension induced by surgical manipulation. Other additionally required drugs were remifentanil (0.1 μg kg−1 IV push) due to hypertension. LIMA: Left internal mammary artery
The left internal mammary artery and saphenous vein were used as vascular grafts. The number and duration of anastomoses were similar between the groups. Patients’ extubation times, the duration of intensive care and hospital stay, and postoperative drainage amount did not differ significantly (Table 3). No blood or blood product transfusions were performed in any patient. The duration of extubation in Group H was longer than in Group N (192.7±195.1 min and 276±158.2 min), but this result was not statistically significant (p=0.116).
Table 3.
Surgery, anastomosis, extubation, the length of the intensive care and hospital stay, and drainage amount
| Group N (n=15) (Mean±SD) |
Group H (n=15) (Mean±SD) |
p | |
|---|---|---|---|
| Anastomosis duration (min) | 22.93±17.03 | 19.80±14.77 | 0.436 |
| Surgical time (min) | 134.00±22.29 | 121.66±23.57 | 0.152 |
| Extubation time (min) | 192.66±195.12 | 276.00±158.18 | 0.116 |
| Length of intensive care stay (hour) | 18.24±5.80 | 20.63±5.49 | 0.233 |
| Length of hospital stay (day) | 3.33±0.61 | 3.53±0.91 | 0.713 |
| Postoperative drainage (mL) | 875±290.16 | 800±267.26 | 0.486 |
SD: standard deviation
No difference was observed between the two groups in terms of complications in our study. The recorded side-effect profiles were typical for potent μ opioid receptor agonists. Nausea was observed in 7 patients in Group N and 5 patients in Group H. An improvement in nausea symptoms was observed in patients after the antiemetic treatment. Short-term ventricular ectopic pulses were observed in 1 patient in Group N and 2 patients in Group H in the first 6 hours postoperatively, and amiodarone was successfully administered. There was no difference in the amount of drainage between the groups.
Discussion
In this study, we found that in fast-track OPCAB surgical procedures, hypertensive patients with similar BIS values needed higher remifentanil and desflurane doses compared to normotensive patients, and those selected anaesthetics were sufficient to provide an intraoperative stable haemodynamic so that no patients needed nitroglycerin and/or beta-blockers. Because of the potential tachycardia caused by nitroglycerin and hypotension caused by beta-blockers, we had decided to use these agents as a secondary plan, but we observed that the ideal haemodynamic targets were achieved with the titration of the short-acting anaesthetic agents applied under the guidance of BIS. Under the BIS guidance, the use of anaesthesia with desflurane–remifentanil, which was carefully adjusted to the arterial blood pressure and HR, provided the desired intraoperative stable haemodynamic even in hypertensive patients, and the patients’ early extubation in the postoperative period without any problems highlighted the importance of anaesthesia techniques and titration. Although the MAC value corresponding to desflurane concentration, which provides the appropriate intraoperative BIS value (30–60), was higher in Group H during surgery than in Group N, this result was not found to be statistically significant. When higher doses and concentrations of remifentanil were used, it was observed that the desflurane MAC decreased (8). In this case, it could have actually been expected that the desflurane concentration and the corresponding MAC value used in Group H, in which more remifentanil was used, would have been lower. However, hypertension is one of the factors that increase MAC, and presumably for this reason despite the additional remifentanil application, we still needed a higher concentration of desflurane in hypertensive patients in our study group, and the corresponding MAC value was determined as slightly higher.
The secondary targets such as the extubation time, duration of intensive care and hospital stay, and postoperative complications were found to be similar in both groups. Although not considered as statistically significant, it was observed that the extubation time was delayed in Group H. In a study examining the effects of remifentanil and sufentanil on early extubation in cardiac surgery, the duration of extubation in the remifentanil+isoflurane group was reported as 386 min (9). The extubation time in our study was 192 min in Group N and 276 min in Group H. The reason for our patients’ early extubation might be the shorter elimination time of desflurane compared to that of isoflurane. It is known that, independently of the dose and duration of remifentanil infusion, the clearance of desflurane is rapid, and it provides a rapid wake-up (10). However, desflurane application at higher concentrations may cause the clearance prolongation. This is probably why the duration of extubation was longer in Group H in which higher concentrations of desflurane were used.
The OPCAB surgery might be accompanied by various degrees of hypotension that result from a reduced cardiac output due to heart retraction and position changes of the heart (11, 12). The development of hypotension in the intraoperative period may occur more dramatically in hypertensive patients due to a decrease in the high systemic venous resistance via anaesthesia. To prevent this, in resistant cases, the use of preload, up–down position, alpha agonists and noradrenalin are recommended (13). In OPCAB surgeries, rather than retraction and position changes, the use of advanced stabilisation devices such as the ‘octopus’ stabiliser minimised the cardiac output decline and thus reduced the risk of hypotension (14). However, whether normotensive or hypertensive, systolic arterial blood pressures of patients are needed to be well controlled. A high arterial blood pressure causes the cardiac stress to increase and heart’s pumping blood due to an increased afterload, and it also predisposes the development of aortic dissection during a proximal graft anastomosis (2). For this reason, it may be necessary to use nitroglycerin in addition to anaesthetic medications in cases of high blood pressure. However, a careful titration is also necessary to avoid hypotension that may occur with vasodilators. In our study, the arterial blood pressure was higher in the hypertensive group, but no elevation was necessary enough to use nitroglycerin in any patient. The elevation was under control by adding bolus additives to the dose of remifentanil infusion.
Bradycardia used to be a necessity for surgeons to work comfortably on the heart at the onset of OPCAB surgery, and the application of beta-blockers for this purpose was a frequent method (14). The development of stabilisation techniques also made bradycardia unnecessary. However, there is no doubt that tachycardia should be meticulously avoided. There were no differences in the HR in our study and no additional remifentanil-induced bradycardia was observed. The selected anaesthetic technique is important to maintain a haemodynamic stability. Although high-opioid techniques that used to be performed provided a good haemodynamic control, they have become less used today since they cause delayed postoperative awakening and extubation. Today, anaesthetists avoid the administration of high doses of long-acting opioids due to the side effects such as prolonged respiratory depression and ventilation requirement, hypotension and delay in returning to normal bowel movements (1). The fast-track anaesthesia method involves patients’ being extubated within the first 6 hours in the postoperative period and improves recovery by reducing the length of hospital stay and intensive care in the postoperative period (15–17). In the fast-track method, among the preferred anaesthesia, ‘volatile anaesthetics+short-acting opioid combination’ is also included (2). Since desflurane provides rapid recovery and is cardioprotective, it is advantageous in fast-track anaesthesia (18, 19). Remifentanil is a very short-acting opioid and thus allows early extubation via quality haemodynamic stability (20). Moreover, it has a catecholamine-reducing effect that can also control the increased autonomic activity due to desflurane. Other publications have reported that the desflurane–remifentanil combination provides a good haemodynamic stability in critical surgical procedures such as cardiac pheochromocytoma and thoracic surgery, that no additional vasodilator is needed, and that microcirculation improves (21, 22). In our study, the desflurane–remifentanil combination was also found to provide an adequate intraoperative haemodynamic stability in hypertensive patients who underwent fast-track OPCAB surgery and by increasing the remifentanil dose, the desired HR and arterial blood pressure values could be reached without nitroglycerin.
In a study comparing the cardiovascular safety of remifentanil–sevoflurane and fentanyl–etomidate in the anaesthesia induction in coronary surgery, of all the patients on remifentanil, 1 patient had asystole and 3 patients had severe bradycardia and hypotension (23). In this study, the remifentanil dose used in the induction of anaesthesia was set at 0.33 μg kg−1 min, and the duration of anaesthesia induction was set at 90 seconds. In our study, severe hypotension and bradycardia were observed during the induction of anaesthesia in 1 patient in Group N, and the patient was excluded from the study. No cardiovascular depression was observed during anaesthesia induction in other patients. We think that this difference is due to a longer induction of anaesthesia (4 min) and the patients having been hydrated before the anaesthesia induction, despite the higher anaesthesia induction dose. In a study performed by Kessler et al. (24), the authors compared three separate anaesthetic techniques that consisted of propofol+remifentanil, thoracic epidural anaesthesia and combinations of these in an OPCAB surgery, and they reported that they used intravenous esmolol in 7 patients due to the significant increase in HR during coronary anastomosis in the general anaesthesia group. In our study, during anastomoses, ephedrine was also applied in 1 of the hypertensive patients in whom more remifentanil was used due to hypotension that developed.
Conclusion
It has been concluded that an optimal intraoperative haemodynamic stabilisation was provided in hypertensive patients undergoing OPCAB surgery under desflurane–remifentanil anaesthesia facilitated by BIS monitoring, although higher doses of remifentanil were required. It was observed that complications did not increase because of the additional remifentanil applied. Thus, remifentanil can be safely used.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Yüksek İhtisas Training and Research Hospital (Date: 14.05.2009, No: 222).
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - Ü.K., Ö.E.; Design - Ü.K., B.Ö., A.D.; Supervision – Ü.K., Ö.E.; Resources – B.Ö., Ş.B., Ü.K.; Materials – B.Ö.; Data Collection and/or Processing – B.Ö., Ş.B., K.Ç.; Analysis and/or Interpretation – B.Ö., Ü.K., A.D., Ş.B., K.Ç., Ö.E.; Literature Search – B.Ö., Ü.K., A.D.; Writing Manuscript – B.Ö., Ü.K., A.D.; Critical Review – Ü.K., Ö.E.; Other – B.Ö., Ü.K., A.D.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Bovill JG, Sebel PS, Stanley TH. Opioid analgesics in anesthesia:with special reference to their use in cardiovascular anesthesia. Anesthesiology. 1984;61:731–55. doi: 10.1097/00000542-198412000-00018. [DOI] [PubMed] [Google Scholar]
- 2.Hemmerling TM, Romano G, Terrasini N, Noiseux N. Anesthesia for off-pump coronary artery bypass surgery. Ann Card Anaesth. 2013;16:28–39. doi: 10.4103/0971-9784.105367. [DOI] [PubMed] [Google Scholar]
- 3.Mandel JE. Considerations for the use of short-acting opioids in general anesthesia. J Clin Anesth. 2014;26(Suppl 1):S1–7. doi: 10.1016/j.jclinane.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 4.Engoren M, Luther G, Fenn-Buderer N. A comparison of fentanil, sufentanil and remifentanil for fast-track cardiac anesthesia. Anesth Analg. 2001;93:859–64. doi: 10.1097/00000539-200110000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Carl C, Hug, Jack S. Shonewise Anesthesia for adult cardiac surgery. In: Miller RD, editor. Anesthesia. ch(53) New York: Churchill Livingstone Ltd; 1994. pp. 1757–809. [Google Scholar]
- 6.Morgan EG, Mikhail MS. Anesthesia for cardiovascular surgery. clinical Anesthesiology, Los Angeles Prentice Hall Inc. 1992;Ch21(21):37–361. [Google Scholar]
- 7.Bauer M, Wilhelm W, Kraemer T, Kreuer S, Brandt A, Adams HA, et al. Impact of bispectral index monitoring on stress response and propofol consumption in patients undergoing coronary artery bypass surgery. Anesthesiology. 2004;101:1096–104. doi: 10.1097/00000542-200411000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Han SS, Han S, Kim BG, Kim DH, Ryu JH. The concentration of desflurane preventing spectral entropy change during surgical stimulation: A prospective randomized trial. J Clin Anesth. 2017;37:86–91. doi: 10.1016/j.jclinane.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Lison S, Schill M, Conzen P. Fast-track cardiac anesthesia: efficacy and safety of remifentanil versus sufentanil. J Cardiothorac Vasc Anesth. 2007;21:35–40. doi: 10.1053/j.jvca.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 10.Wilhelm W, Berg K, Langhammer A, Bauer C, Biedler A, Larsen R. Remifentanil in gynecologic laparoscopy. A comparison of consciousness and circulatory effects of a combination with desflurane and propofol. Anasthesiol Intensivmed Notfallmed Schmerzther. 1998;33:552–6. doi: 10.1055/s-2007-994810. [DOI] [PubMed] [Google Scholar]
- 11.Porat E, Sharony R, Ivry S, Ozaki S, Meyns BP, Flameng WJ, et al. Hemodynamic changes and right heart support during vertical displacement of the beating heart. Ann Thorac Surg. 2000;70:1188–91. doi: 10.1016/S0003-4975(99)01437-X. [DOI] [PubMed] [Google Scholar]
- 12.Mathison M, Edgerton JR, Horswell JL, Akin JJ, Mack MJ. Analysis of hemodynamic changes during beating heart surgical procedures. Ann Thorac Surg. 2000;70:1355–60. doi: 10.1016/S0003-4975(00)01590-3. [DOI] [PubMed] [Google Scholar]
- 13.Grundeman PF, Borst C, Van Herwaarden JA, Verlaan CW, Jansen EW. Vertical displacement of the beating heart by the Octopus tissue stabilizer: influence on coronary flow. Ann Thorac Surg. 1998;65:1348–52. doi: 10.1016/S0003-4975(98)00226-4. [DOI] [PubMed] [Google Scholar]
- 14.Jansen EW, Borst C, Lahpor JR, Grundeman PF, Eefting FD, Nierich A, et al. Coronary artery bypass grafting without cardiopulmonary bypass using octopus method: Results of the first one hundred patients. J Thorac Cardiovasc Surg. 1998;116:60–7. doi: 10.1016/S0022-5223(98)70243-0. [DOI] [PubMed] [Google Scholar]
- 15.Westaby S, Pillai R, Parry A, O’Regan D, Giannopoulos N, Grebenik K, et al. Does modern cardiac surgery require conventional intensive care? Eur J Cardiothorac Surg. 1993;7:313–8. doi: 10.1016/1010-7940(93)90173-9. [DOI] [PubMed] [Google Scholar]
- 16.White PF, Kehlet H, Neal JM, Schricker T, Carr DB, Carli F. The role of the anesthesiologist in fast-track surgery: From multimodal analgesia to perioperative medical care. Anesth Analg. 2007;104:1380–96. doi: 10.1213/01.ane.0000263034.96885.e1. [DOI] [PubMed] [Google Scholar]
- 17.Cheng DC. Fast-track cardiac surgery: Economic implications in postoperative care. J Cardiothorac Vasc Anesth. 1998;12:72–9. doi: 10.1016/S1053-0770(98)90061-1. [DOI] [PubMed] [Google Scholar]
- 18.Zaugg M, Lucchinetti E, Garcia C, Pasch T, Spahn DR, Schaub MC. Anaesthetics and cardiac preconditioning. Part II. Clinical implications. Br J Anaesth. 2003;91:566–76. doi: 10.1093/bja/aeg206. [DOI] [PubMed] [Google Scholar]
- 19.Toma O, Weber NC, Wolter JI, Obal D, Preckel B, Schlack W. Desflurane preconditioning induces time-dependent activation of protein kinase C epsilon and extracellular signal-regulated kinase 1 and 2 in the rat heart in vivo. Anesthesiology. 2004;101:1372–80. doi: 10.1097/00000542-200412000-00018. [DOI] [PubMed] [Google Scholar]
- 20.Aşkın T, Karadeniz Ü, Ünver S, Boran E, Erdemli Ö. An efficacy comparison of fentanyl and remifentanil during off-pump coronary artery bypass graft surgery. Türk Göğüs Kalp Damar Cerrahisi Dergisi. 2013;21:683–90. doi: 10.5606/tgkdc.dergisi.2013.7309. [DOI] [Google Scholar]
- 21.Ng JM. Desflurane and remifentanil use during resection of a cardiac pheochromocytoma. J Cardiothorac Vasc Anesth. 2004;18:630–1. doi: 10.1053/j.jvca.2004.07.015. [DOI] [PubMed] [Google Scholar]
- 22.Cho YJ, Bae J, Kim TK, Hong DM, Seo JH, Bahk JH, et al. Microcirculation measured by vascular occlusion test during desflurane-remifentanil anesthesia is superior to that in propofol-remifentanil anesthesia in patients undergoing thoracic surgery: subgroup analysis of a prospective randomized study. J Clin Monit Comput. 2016 Sep 26; doi: 10.1007/s10877-016-9937-2. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 23.Wang JY, Winship SM, Thomas SD, Gin T, Russell GN. Induction of anaesthesia in patients with coronary artery disease: a comparison between sevoflurane-remifentanil and fentanyl-etomidate. Anaesth Intensive Care. 1999;27:363–8. doi: 10.1177/0310057X9902700405. [DOI] [PubMed] [Google Scholar]
- 24.Kessler P, Aybek T, Neidhart G, Doğan S, Lischke V, Bremerich DH, et al. Comparison of three anesthetic techniques for off-pump coronary artery bypass grafting. general anesthesia, combined general and high thoracic epidural anesthesia, or high thoracic epidural anesthesia alone. J Cardiothorac Vasc Anesth. 2005;19:32–9. doi: 10.1053/j.jvca.2004.11.006. [DOI] [PubMed] [Google Scholar]


