Abstract
Haemorrhage in the neuraxial region following spinal and epidural interventions is a rare and unexpected complication. Subdural haemorrhage is the most frequently occurring type. A 64-year-old male patient was admitted with complaints of severe headache and intermittent fever after 14 days of spinal anaesthesia and inguinal hernia operation. Neurological examination and systemic examination showed no features other than that for postural tremor. Cranial and spinal magnetic resonance (MR) imaging were requested for the differential diagnosis of the patient with secondary headaches. In MR, subacute subdural haemorrhage adjacent to the dura, limiting the posterior sulcus, and extra axial distance (not clearly distinguishable epidural-subdural distinction) along the entire spinal canal were detected. The patient who had no neurological deficit and no culture recruitment underwent conservative treatment. We would like to emphasize here that the coexistence of both intracranial subdural and spinal subdural-epidural haemorrhage can be seen as a complication after spinal anaesthesia, which has not been previously observed in the literature, along with the importance of headache after regional anaesthesia.
Keywords: Spinal epidural hematoma, spinal anaesthesia, headache, complication
Introduction
It is known that complications such as epidural, subdural or subarachnoid haemorrhage, epidural abscess, cerebrospinal fluid (CSF) hypotension, anterior spinal artery thrombosis secondary to prolonged hypotension, arachnoiditis, myelitis and intervertebral disc prolapse may occur following spinal or epidural anaesthesia.
Haemorrhage in the neuraxial region following spinal or epidural anaesthesia is a rare and unexpected complication. Subdural haemorrhage is the most common type of haemorrhage. Haemorrhage during the procedure may occur because of vessel puncture, as well as because of pressure differences between the CSF and intravascular spaces.
We present a case of spinal epidural–subdural haemorrhage and intracranial subdural haemorrhage following spinal anaesthesia, which we did not encounter in the literature. We hope to increase the awareness in this regard (1–3).
Case Presentation
A 64-year-old man complaining of a headache was admitted. He underwent an inguinal hernia surgery with spinal anaesthesia 14 days prior. On postoperative day 1, the patient complained of an imploding severe headache with a feeling of pressure in the head along with sweating. The headache responded to non-steroidal anti-inflammatory drugs (NSAIDs) for a few hours and then recurred, initiated every morning, had bilateral frontal and occipital localisation, was position independent and relieved only with the hyperextension of the head. The patient consumed approximately 3 litres of fluid per day and frequently consumed caffeinated beverages, which resulted in a partial benefit. Nausea accompanied headache. According to the information obtained from the patient’s history, the body temperature increased along with trembling up to 38.5°C first week postoperatively and continued for 3 days; consequently, the patient received subfebrile and intermittent fever heights continually until admission to our clinic. The patient additionally complained of increasing body trembling and shoulder pain and continuously took 250 mg paracetamol, 150 mg propifenazone and 50 mg caffeine-containing medication. The patient had known essential hypertension and was taking nebivolol (beta blocker) 5 mg 1×1 and did not receive antiaggregant or anticoagulant therapy. Neurological examination of the patient revealed no additional features in the systemic examination was at normal limits except for postural tremor. Spinal anaesthesia was applied and was successful after three attempts using a 22-gauge Quincke spinal needle. The patient’s blood tests revealed a sedimentation rate of 36 mm h−1, CRP level of 35.3 mg dL−1 and WBC count of 10.6 103 μL−1. Cephalexin monohydrate 1 g 2×1 was initiated during the emergency department as the patient’s fever recurred. Because of an ongoing headache and high fever, the patient was hospitalised for evaluation in the third postoperative week. There was no growth in the blood and urine cultures of the patient as examined by the Infectious Diseases Department. Cranial and spinal imaging were performed in the patient; subacute, subdural haemorrhage adjacent to the dura that confined the posterior sulcus and haemorrhage at the extra-axial distance (epidural–subdural distinction could not be clearly distinguished) along the entire spinal canal were observed. The haematoma was located in the posterior and had a maximum thickness of 10 mm maximum, most of which was in the lower lumbar region. The spinal canal narrowed secondary to the bleeding in the lower cervical and thoracic regions (Figure 1–6).
Figure 1.
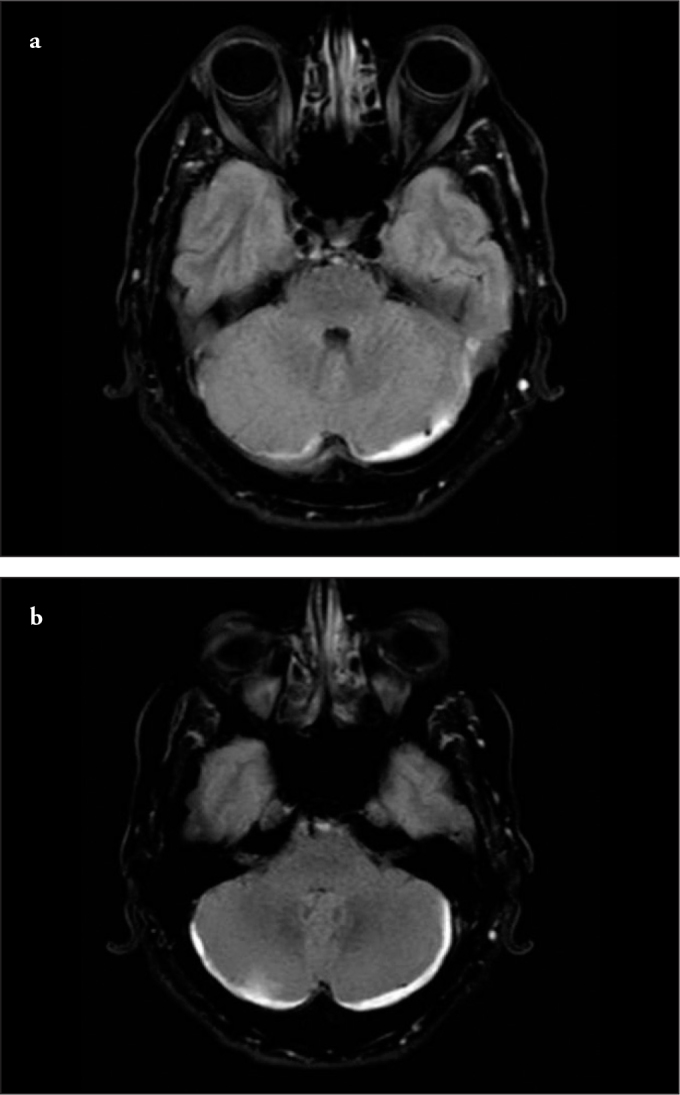
a, b. FLAIR axial section, appearance that is compatible with hyperintense subdural haemorrhage in the posterior fossa
Figure 2.
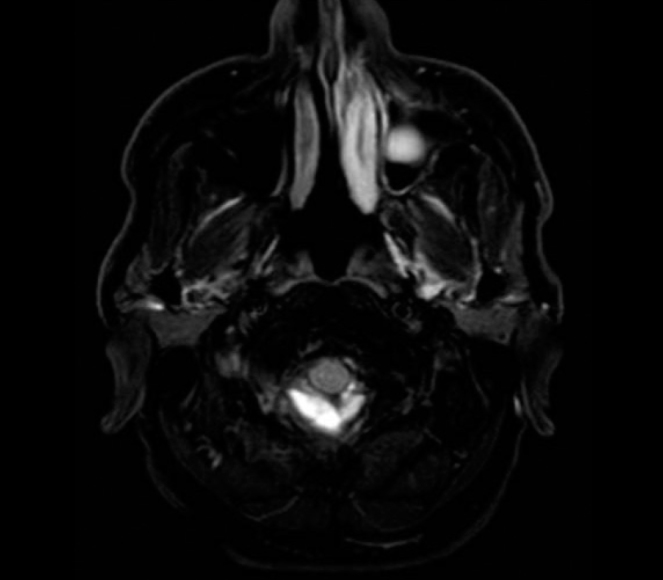
FLAIR axial section, hyperintense appearance that is compatible with haemorrhage in the posterior cervical spinal region
Figure 3.
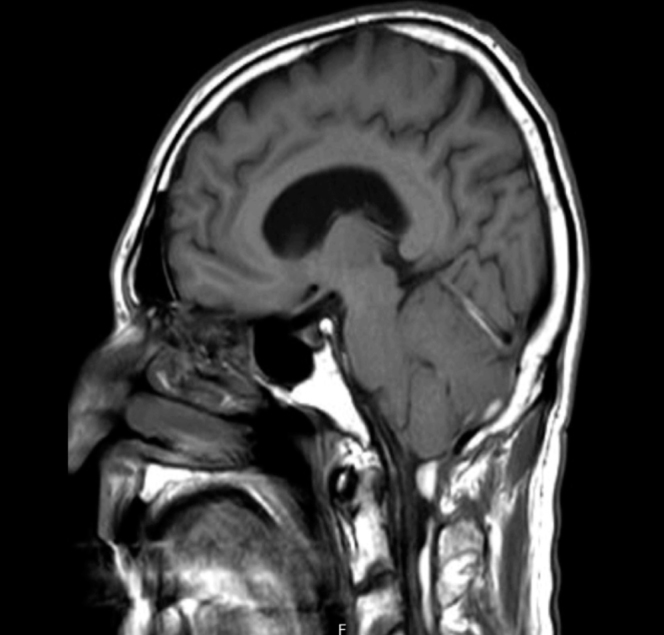
T1 sagittal section, hyperintense appearance in the cervical spinal epidural and posterior fossa
Figure 4.
Contrast-enhanced sagittal section, dural contrast enhancement
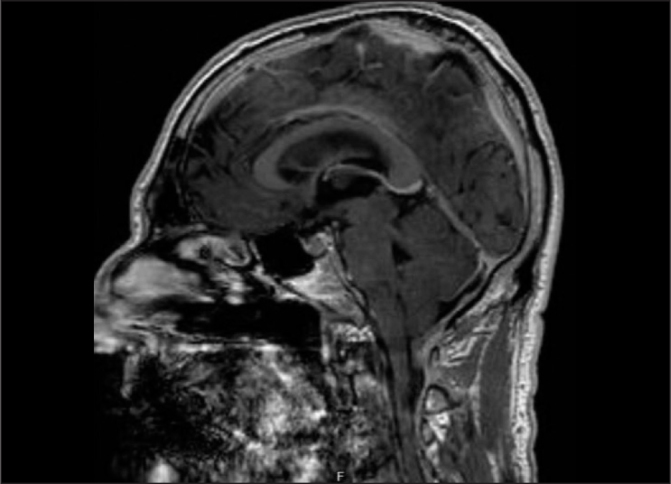
Figure 5.
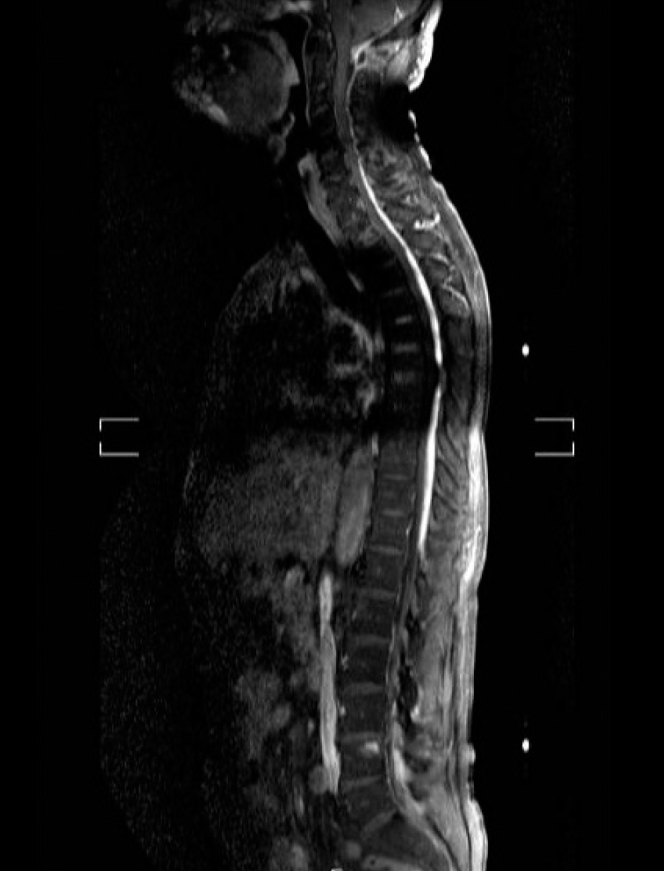
Spinal MR, hyperintense appearance of the sagittal section in the cervical and thoracic spinal epidural–subdural region
Figure 6.
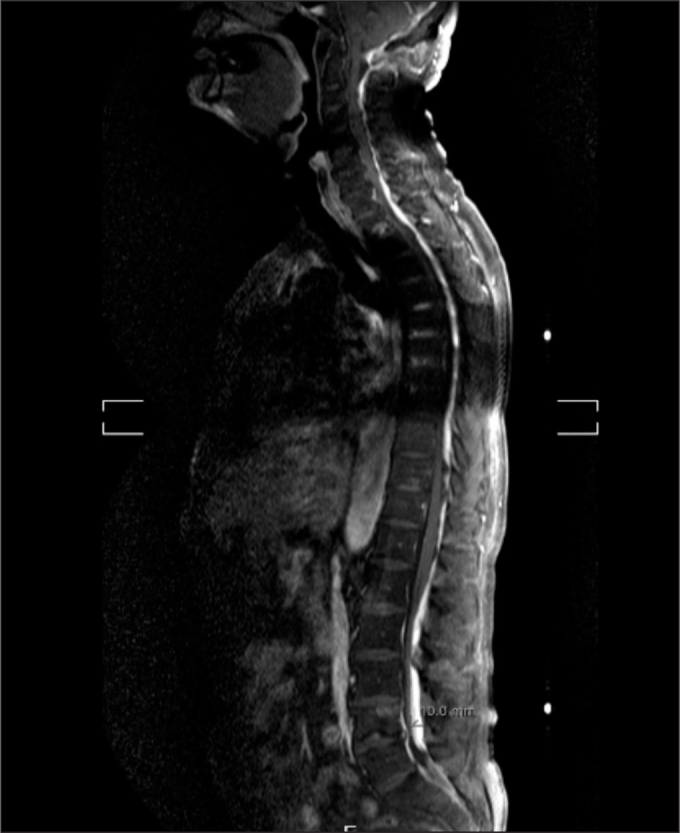
Spinal MR, hyperintense appearance reaching 10 mm in the sagittal section in the lumbar epidural region
The lumbar puncture could not be performed because the cerebellar tonsils extended inferiorly. No neurological deficit was observed during the patient’s follow-up. The headache regressed with 300 mg of paracetamol and 30 mg of codeine phosphate. Further, sedimentation rate, CRP and WBC values regressed. He had no fever without medication for 2 days after follow-up. The patient was followed up with conservative treatment and was discharged after brain and spinal MR was planned for control in the 3rd month.
Discussion
Severe complications following epidural and spinal anaesthesia occur in less than 0.05% of cases. Haemorrhagic complications were more frequent in epidural anaesthesia (1:150,000) than in spinal anaesthesia (1:220,000) in patient series comprising 1.5 million patients (1–3). In a national study, epidural haematoma was detected in 15 of 2,300,000 obstetric patients who underwent epidural catheterisation (0.6 in 100,000) (4).
Spinal epidural haematoma (SEH) may occur secondary to vessel puncture with the catheter or needle or to CSF pressure change and traction. A venous network called internal vertebral plexus is present along with fat tissue in the spinal epidural space. SEH can occur in any patient; it can also occur to patients with coagulation disorders or in anticoagulant users. The diagnosis is difficult because of the occult structure of haemorrhage. Suspicion is therefore important in diagnosis. Spinal intervention with a single entry point, reduced needle diameter and the absence of a permanent catheter decreases the risk of epidural haematoma development. Because the spinal space is incapable of expansion, even small volumes of blood can cause ischaemia by compressing the neural structures. This constitutes the symptomatology. The most common presentation is bladder and bowel dysfunction with progressive sensory loss (68%) and motor loss (8%). Cases who have radicular pain, back pain or shoulder pain can be seen. In the literature, there is a case of a severe headache such as subarachnoid haemorrhage, which occurred with neck stiffness and in which no abnormalities were found in lumbar puncture (5, 6).
The known risk factors for the development of SEH following neuraxial blockade are advanced age, female gender, abnormal bone structure and coagulopathy. Vasculitic diseases, particularly Lupus disease, arterial hypertension and pregnancy can also lead to SEH. Unknown arteriovenous malformations and undiagnosed leukaemia or lymphoma-like diseases or bleeding tendencies are also possible causes (7, 8). In the study by Li et al. (9), the risk of epidural haematoma development was observed to be higher in patients with severe bacterial infection or in patients for emergency surgery.
Makris et al. (10) reported the case of a patient who was diagnosed with acute shoulder pain and flask paraparesis 4 hours after the administration of bemiparin, which is a low molecular weight heparin, and in whom SEH was noticed at a later stage. Madhugiri et al. (7) reported a patient whose motor force was 3/5 at the 10th hour postoperatively and who had paresthaesia and progressive paraparesis at the 16th hour postoperatively. Furthermore, they stated that a phenomenon, ‘lucid interval’, which is similar to that of cranial epidural haematomas, could also be valid for SEH. Haematomas were detected away from the needle entry site in both cases.
Rapid surgical intervention (laminectomy) provides blood drainage, but the time of decompression is important. In a study in which 30 patients with SEH underwent surgery, better neurological outcomes were observed in patients who were operated in the first 12 hours (11, 12). Besides surgical intervention, there are patients in whom conservative follow-up was performed according to neurological loss.
Conclusion
All patients undergoing spinal anaesthesia should be cautioned in terms of a headache, and neuroradiological imaging should be performed if necessary. Haemorrhagic complications, which are rare, may develop without any risk factors. We wish to bring attention to the complications from neuraxial regional anaesthesia by determining the coexistence of both intracranial subdural and spinal subdural–epidural haemorrhage after spinal anaesthesia, which was previously not observed in the literature.
Footnotes
Informed Consent: Written informed consent was obtained from patient who participated in this case.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – Z.I., L.İ.; Design – Z.I., L.İ., Y.E.; Supervision – L.İ., V.Ö., Y.E.; Resources – Z.I., V.Ö.; Materials – Z.I.; Data Collection and/or Processing – Z.I., V.Ö.; Analysis and/or Interpretation – Z.I., L.İ., V.Ö., Y.E.; Literature Search - Z.I., L.İ., V.Ö., Y.E.; Writing Manuscript – Z.I., L.İ.; Critical Review - Z.I., L.İ., V.Ö., Y.E.
Conflict of Interest: Authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Rocchi R, Lombardi C, Marradi I, Di Paolo M, Cerase A. Intracranial and intraspinal hemorrhage following spinal anesthesia. Neurol Sci. 2009;30:393–6. doi: 10.1007/s10072-009-0103-1. [DOI] [PubMed] [Google Scholar]
- 2.Aromaa U, Lahdensuu M, Cozanitis D. Severe complications associated with epidural and spinal anaesthesias in Finland 1987–1993 A study based on patient insurance claims. Acta Anaesthesiol Scand. 1997;41:445–52. doi: 10.1111/j.1399-6576.1997.tb04722.x. [DOI] [PubMed] [Google Scholar]
- 3.Auroy Y, Narchi P, Messiah A, Litt L, Rouvier B, Samii K. Serious Complications Related to Regional Anesthesia Results of a Prospective Survey in France. Anesthesiology. 1997;87:479–86. doi: 10.1097/00000542-199709000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Rosero E, Joshi G. Nationwide incidence of serious complications of epidural analgesia in the United States. Acta Anaesthesiol Scand. 2016;60:810–20. doi: 10.1111/aas.12702. [DOI] [PubMed] [Google Scholar]
- 5.Aristedis R, Dimitrios B. Spinal epidural hematoma mimicking subarachnoid hemorrhage: A case study. Surg Neurol Int. 2017;8:182. doi: 10.4103/sni.sni_197_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grant GJ. Adverse effects of neuraxial analgesia and anesthesia for obstetrics 2017 [updated june 28 2017] Available from: https://www.uptodate.com/contents/adverse-effects-of-neuraxial-analgesia-and-anesthesia-for-obstetrics?source=see_link§ionName=Postdural%20puncture%20headache&anchor=H13#H12561173.
- 7.Madhugiri VS, Singh M, Sasidharan GM, Kumar VR. Remote spinal epidural haematoma after spinal anaesthesia presenting with a ‘spinal lucid interval’. BMJ Case Rep. 2012;2012 doi: 10.1136/bcr-2012-007258. bcr2012007258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gottschalk A, Bischoff P, Lamszus K, Standl T. Epidural hematoma after spinal anesthesia in a patient with undiagnosed epidural lymphoma. Anesth Analg. 2004;98:1181–3. doi: 10.1213/01.ANE.0000101989.54746.4E. [DOI] [PubMed] [Google Scholar]
- 9.Li SL, Wang DX, Ma D. Epidural hematoma after neuraxial blockade: a retrospective report from China. Anesth Analg. 2010;111:1322–4. doi: 10.1213/ANE.0b013e3181f1b9ea. [DOI] [PubMed] [Google Scholar]
- 10.Makris A, Gkliatis E, Diakomi M, Karmaniolou I, Mela A. Delayed spinal epidural hematoma following spinal anesthesia, far from needle puncture site. Spinal Cord. 2014;52:S14. doi: 10.1038/sc.2013.174. [DOI] [PubMed] [Google Scholar]
- 11.Lawton MT, Porter RW, Heiserman JE, Jacobowitz R, Sonntag VK, Dickman CA. Surgical management of spinal epidural hematoma: relationship between surgical timing and neurological outcome. J Neurosurg. 1995;83:1–7. doi: 10.3171/jns.1995.83.1.0001. [DOI] [PubMed] [Google Scholar]
- 12.Vandermeulen EP, Van Aken H, Vermylen J. Anticoagulants and spinal-epidural anesthesia. Anesth Analg. 1994;79:1165–77. doi: 10.1213/00000539-199412000-00024. [DOI] [PubMed] [Google Scholar]


