Abstract
Intimate partner violence is prevalent among female sex workers (FSWs) in China, and it is significantly associated with mental health problems among FSWs. However, limited studies have explored the mechanisms/process by which violence affects mental health. The purpose of this study was to explore the relationships among partner violence, internalized stigma, and mental health problems among FSWs. Data were collected using a self-administered cross-sectional survey administered to 1,022 FSWs in Guangxi Zhuang Autonomous Region (Guangxi), China during 2008–2009. We used structural equation modeling to test the hypothesized relationships. Results indicated that violence perpetrated by either stable sexual partners or clients was directly and positively associated with mental health problems. Violence also had indirect relation to mental health problems through stigma. Results highlight the need for interventions on counseling and care for FSWs who have experienced violence and for interventions to increase FSWs’ coping skills and empowerment strategies.
Keywords: Violence, Stigma, Mental health, Female sex worker, China
Introduction
Among all forms of violence against women, interpersonal violence is the most universal form, including intimate partner violence (Davidson & Gervais, 2015). Intimate partner violence is defined as “behaviors within an intimate relationship that cause physical, sexual or psychological harm, including acts of physical aggression, sexual coercion, psychological abuse and controlling behaviors” (World Health Organization, 2010, p11). Female sex workers (FSWs) comprise a vulnerable population who can be victimized by violence either from their stable partners (e.g., husbands, or long-term commercial partners) (Zhang et al., 2012) or from clients (Semple et al., 2015). Other than increasing vulnerability to HIV infection (Ulibarri et al., 2010), unwanted pregnancy (Silverman, Gupta, Decker, Kapur, & Raj, 2007), and physical injury (Antai, 2011), violence often causes adverse health consequences, including mental health problems (e.g., depression, loneliness, and suicidal behavior) among FSWs (Hong, Zhang, Li, Liu, & Zhou, 2013; O’Campo, Woods, Jones, Dienemann, & Campbell, 2006; Ouellet-Morin et al., 2015). Women victims of partner violence often experience loneliness (Rokach, 2007) and suicide attempts (Guillen, Panadero, Rivas, & Vazquez, 2015). Loneliness occurs often across all psychotic disorders (Badcock et al., 2015). Although FSWs have a high prevalence of mental health problems due to partner violence (Patel, Saggurti, Pachauri, & Prabhakar, 2015), the mechanism of the effects of violence on mental health problems among FSWs has been understudied. Furthermore, most of FSWs affected by violence may not seek or receive the social support they need because of stigmatization due to intimate partner violence (Overstreet & Quinn, 2013). According to Overstreet and Quinn (2013), people who experience intimate partner violence fear prejudice or discrimination if they disclose the experience of violence and may increase internalization of such prejudice or stigma. In the general population, after victimization more than half of women sought social support from family members (Postmus, 2015). A substantial proportion of women could not seek support because of many societal barriers (Sabri et al., 2015). FSWs may have more difficulty seeking support from their family members.
Among FSWs experiencing violence, an added stigma may occur for being engaged in commercial sex work (Sallmann, 2010). FSWs are often labeled as the vector of the HIV epidemic (Pirkle, Soundardjee, & Stella, 2007). They are often stereotyped as dirty, immoral, callous and undeserving women(Vijayakumar, Chacko, & Panchanadeswaran, 2015). This stigmatization can lead to feelings of self-blame and guilt, distancing themselves from others, and decreasing accessibility to social and health resources (Sallmann, 2010).
Stigma is the process of labeling, stereotyping, linking to undesirable characteristics for stigmatized persons/groups and treating stigmatized groups as discredited or discreditable with deviations from the ‘normal’ (Kleinman & Hall-Clifford, 2009). Stigma has two distinguished but related forms: public stigma and internalized stigma (self-stigma) (Corrigan, Larson, & Rusch, 2009). Public stigma refers to the stigmatizing perceptions from the public with stereotypes, prejudice, and discrimination to stigmatized group, while the internalized stigma refers to the internalized perceptions of public devaluation and discrimination by the stigmatized individuals (Corrigan, Larson, & Rusch, 2009; Vogel, Bitman, Hammer, & Wade, 2013). Public stigma can be internalized, and it is a primary trigger for internalized stigma (Padurariu, Ciobica, Persson, & Stefanescu, 2011; Sallmann, 2010). Using a cross-lagged panel study design among college students in the United States, Vogel et al. (2013) found that public stigma may predict internalized stigma three months later. According to Corrigan et al. (2009), internalized stigma is a cognitive process through which a stigmatized individual is aware of the stereotypes, agrees with the stereotypes, and applies the stereotypes to one’s self. As Corrigan and colleagues (2009) argued, to experience internalized stigma, before agreeing with and applying the stereotypes to one’s self the person must be aware of stereotypes among the general public (Corrigan, Larson, & Rusch, 2009).
Internalized stigma decreases individual’s self-esteem and self-efficacy, leading people to perceive themselves as inferior (Padurariu et al., 2011). The impact of internalized stigma on psychological distress may be the result of reducing self-esteem and fostering social avoidance (Corrigan, 2004; Herek, Saha, & Burack, 2013). Although few studies have addressed the protective factors (e.g., resilience and empowerment) in overcoming stigma (Boardman et al., 2011), a large body of literature has reported that internalized stigma is associated with poor quality of life and increased disease progression among people with mental illness (Mashiach-Eizenberg, Hasson-Ohayon, Yanos, Lysaker, & Roe, 2013; Padurariu et al., 2011). However, limited studies to date have examined the role of internalized stigma on mental health problems among vulnerable population, including FSWs. A meta analysis of 49 empirical studies examined major types of stigma for mental illness, sexual orientation and HIV/AIDS and synthesized the association of stigma and mental health problems (Mak, Poon, Pun, & Cheung, 2007). They found that the stigma-mental health relationship varied from strong negative to zero correlations in the previous research (Mak et al., 2007).
The commercial sex industry in China has surged rapidly in recent decades (Zhang, Detels, Liao, Cohen, & Yu, 2008). The estimated number of FSWs in China was about 4–10 million (Kaufman, 2011). In China, stigmatization against FSWs is rooted in social norms that FSWs are stereotyped as the “dregs of society” (Pirkle et al., 2007). Commercial sex is illegal and highly stigmatized, and most FSWs have reported feeling ashamed of their occupation (Sallmann, 2010). A recent study reported that about 45% of FSWs experienced violence from clients and 58% from stable partners (Zhang et al., 2012). Previous studies have explored the stigma against FSWs and its link with mental health problems in China (Hong et al., 2010). However, no research of which we are aware has explored the role of stigma on the relationship between violence and mental health problems among FSWs in China. The objective of this study was to assess the direct association of violence with mental health problems and indirect association through stigma among FSWs in China. Based on the existing literature, we constructed a conceptual model. In this model, we hypothesized that violence from either stable partners or commercial clients would have a direct positive association with mental health problems; and violence from stable partners or violence from commercial clients would have an indirect association with mental health problems through stigma.
Methods
Study site
Data used in the current study were derived from a cross-sectional survey conducted from 2008 to 2009 in Beihai and Guilin, Guangxi Zhuang Autonomous Region (Guangxi) of China. Guangxi is located in Southern China, bordering Viet Nam on the southwest. According to the Sixth National Population Census of China, the total population of Guangxi was 46 million in 2010 (National Bureau of Statistics of China, 2011), with 85% being ethnic minority populations. Beihai and Guilin are famous tourist spots in Guangxi, and each year millions of tourists visit these two cities. Many young women from rural areas or small townships with little formal education or occupational skills have migrated to urban areas and worked in the entertainment industry. Among FSW population in Guangxi, the prevalence of HIV was about 1% (Zhou et al., 2013). An estimated 2,000 FSWs work in each of the two cities.
Sample and data collection
Participants were recruited from 60 commercial sex establishments identified through ethnographic mapping among an estimate of 150 commercial sex venues in total. The local research team informed the Guangxi Center for Disease Control and Prevention (CDC) who had long-term experience working with FSWs and conducted ethnographic mapping, the technique used to learn about the geographic location of hidden populations (Oliver-Velez et al., 2002). The entertainment establishments, including Karaoke venues, bars, mini-hotels, restaurants and personal service sectors, including hair salons and massage parlors, represented most known commercial sex venues in this area (Zhang et al., 2014). Based on the information from ethnographic mapping, the local research team contacted managers or gatekeepers of these establishments for their permission to conduct the survey. After receiving permission from managers or gatekeepers, trained outreach health workers from the local CDC recruited FSWs within these venues until we reached our desired sample size. FSWs in the 60 selected establishments who did not deny engaging in commercial sex and were aged 18 years and above were eligible to take part in the survey. A total of 1,022 women agreed to participate and provided written informed consent. Fifty-one cases were excluded from the data analyses due to out of range data for the study variables. Thus, the final sample size for the present analyses was 971.
Each woman completed a self-administered questionnaire in Mandarin in a private room. Researchers at Wayne State University in the United States conducted translation and back-translation for standardized scales that were not used in China before. Each participant received a small gift with a cash value equivalent to $5 U.S. as a token of appreciation for their time in the study. Trained local health workers provided necessary assistance if the participant had questions about the survey. For those women who were illiterate (less than 5%), interviewers read the items and response options to the participants. The Institutional Review Boards at Wayne State University in the United States and Guangxi CDC, China approved the study protocol.
Measures
Partner violence.
We adapted items measuring violence perpetrated by stable partners (20 items) and by clients (17 items) from the questionnaire of the World Health Organization multi-country study on Women’s Health and Life Experiences (World Health Organization, 2003). This measure has been used previously (Hong, Zhang, Li, Liu, & Zhou, 2013; Zhang et al., 2012). All items are the same for both stable partners and clients except three items (i.e., “threatened you to separate you from your child/forced you to have induced abortion”; “restricted you from going out or having contact with others”; “ignored you for a long time”) that were only applicable for stable partners. A stable partner was defined in this study as a sexual partner with a long-term relationship (e.g., more than 6 months), including a husband, boyfriend, lover, or commercial partner. Three domains of partner violence were covered, including physical violence (e.g., “slapped you”; “kicked you”; “dragged you”), psychological abuse (e.g., “belittled you or humiliated you”), and sexual violence (e.g., “forced you into intercourse”). In the current study, we combined items of physical violence with sexual violence because the sexual violence scale had a lower Cronbach’s alpha. These items had a 4-point response option (e.g., 0=never, 1=occasionally, 2=sometimes, 3=frequently). For stable partners, the internal consistency estimates (Cronbach’s alpha) were 0.83 for the subscale of physical violence and 0.71 for the subscale of psychological abuse. For clients, the internal consistency estimates (Cronbach’s alpha) were 0.72 for subscale of physical violence and 0.77 for subscale of psychological abuse. The Cronbach’s alpha for the overall scale of violence was 0.85 (20 items) for stable partners and 0.83 for clients (17 items).
Stigma.
Stigma against FSWs was assessed using 15 items (Table 1). This scale was developed based on our qualitative interviews with participants. FSWs were asked their perceptions of the proportion of people in the society who held negative attitudes (stereotypes) toward FSWs (e.g., “Once a woman becomes a FSW, her whole life is over”; “Once a woman becomes a FSW, she cannot raise her head in front of others”; “FSWs are only ‘sex toys’ for men”). These items had a 4-point response option (e.g., 1=no people, 2=few people, 3=some people, 4=many people). Reverse scoring was used for the items related to positive attitudes (3 items). We performed exploratory factor analysis to identify subscales. The criteria used to determine the number of factors was the eigenvalue-one criterion and the scree test. Loading values of 0.35 or greater were considered “meaningful loadings” (Liu, Feng, & Rhodes, 2009). The principal component analysis yielded two factors, including “devalue” (6 items; Cronbach’s alpha=0.61), which had low reliability, and “discredit” (9 items; Cronbach’s alpha=0.80), which had good reliability. We still elected to retain the devalue subscale in the structural equation modeling (SEM) for multiple reasons: 1) stigma is a very important construct in the SEM and only has two indicators (i.e., “discredit” and “devalue”); 2) overall reliability for stigma was high (0.81); 3) the correlation between the two subscales was high; and 4) a Cronbach’s alpha of 0.6 in social science research is considered acceptable (for the purpose of developing instruments) (Elklit & Shevlin, 2007). A composite score was calculated as mean score across all 15 items in both the “discredit” and “devalue” subscales, with a higher score indicating a higher level of stigma.
Table 1.
Items of stigma scale
| Items | Mean (S.D.) | Corrected item- total correlation |
|---|---|---|
| 1. Most FSWs engage in sex industry because they do not have other options/jobs (R). |
2.14 (0.93) | −0.01 |
| 2. FSWs should not be blamed because sex work is a different way to make money (R). |
2.17 (0.94) | −0.06 |
| 3. Working as a FSW for one day do not differ from working as a FSW the whole life. |
2.31 (1.02) | 0.38 |
| 4. If there is a FSW in a family, her family will lose face. | 2.70 (1.11) | 0.46 |
| 5. Nowadays, people stigmatize the poor but not FSWs (R). | 2.31 (1.03) | −0.29 |
| 6. Most FSWs engage in sex industry because they do not want to a hard-work. |
2.38 (0.94) | 0.46 |
| 7. Once a woman becomes a FSW, her whole life is over. | 2.28 (1.02) | 0.56 |
| 8. Most FSWs are lazy. | 2.36 (0.96) | 0.59 |
| 9. Most FSWs do not need to be sympathized. | 2.28 (0.91) | 0.60 |
| 10. If a FSW contacts HIV, it is a punishment for doing sex work. |
1.89 (0.98) | 0.71 |
| 11. If a FSW contacts HIV, it is her own fault. | 1.93 (1.00) | 0.72 |
| 12. Once a woman becomes a FSW, she cannot ‘raise her head’ (look down upon herself) in front of others. |
2.31 (1.04) | 0.68 |
| 13. Most FSWs have less education and low quality (Suzhi). | 2.18 (0.94) | 0.70 |
| 14. FSWs are only ‘sex toys’ for men. | 2.19 (1.07) | 0.71 |
| 15. FSWs do not deserve respect. | 2.13 (1.04) | 0.69 |
| Scale mean score (Cronbach’s alpha=0.83) | 2.24 (0.54) | - |
(R): Reversed items. The range of the stigma scale mean score is: 1.13-3.80.
Mental health problems.
Mental health problems in this study covered three domains, including suicidal behaviors, depressive symptoms, and loneliness. Suicidal behaviors were measured using two items related to frequency of having suicidal ideation (e.g., “had seriously considered killing yourself”) and frequency of having suicidal attempts (e.g., “had tried to kill yourself”) that happened in the last year prior to the survey. These two items had a 5-point response option (1=never, 2=several time a year, 3=at least once a month, 4=at least once a week, 5=almost every day). Depressive symptoms were measured using Center for Epidemiologic Studies Depression Scale (CES-D) (Radloff, 1970), which has been validated in Chinese populations (Lin, 1989). The scale included 20 items about frequency of feelings or symptoms, with a 4-point response option (0=rarely or none of the time, 1=some or little of the time, 2=moderately or much of the time, 3=most or almost all the time). Frequency of loneliness was measured using the UCLA Loneliness Scale (Russell, Peplau, & Ferguson, 1978). The scale included 20 items with a 4-point response option (0=never, 1=rarely, 2=sometimes, 3=often). Respondents were asked the frequency of their depressive symptoms and loneliness in the week prior to the survey. A mean score was calculated for each mental health measure as the composite score, with a higher score indicating a high level of mental health problems. The Cronbach’s alpha was 0.70 for suicidal behavior, 0.88 for depressive symptoms, and 0.76 for loneliness.
Statistical analysis
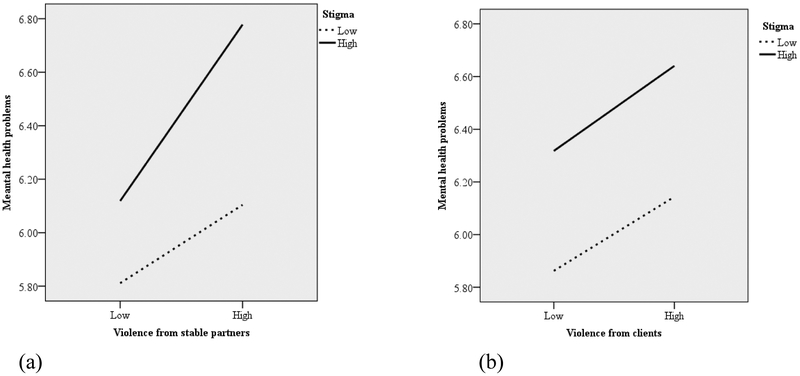
We calculated the frequency distribution of sociodemographic characteristics first and then conducted bivariate analyses. The overall scales of violence from stable partners and clients were categorized into two groups based upon the mean score of the scale. If the overall score of violence either from stable partners of from clients was higher than the median (because the scores were not normally distributed), it was coded as “1”; otherwise, it was coded as “0”. We created a new variable for the number of occurrences of each of the four-point responses (i.e., Never, Occasionally, Sometimes, Frequently) for both the violence from stable partners and from clients. If the number of occurrences of each of the four-point responses was less than “1”, it was coded as “no”; otherwise, it was coded as “yes”. Then, the proportion of “yes” responses was calculated. The McNemar test was used to test the differences in prevalence of violence from stable partners and that from clients. Multivariate linear regression analyses were used to examine the associations between the overall scale and subscales of violence from stable partners and clients with the scales of mental health problems. We calculated standardized coefficients (β) and 95% confidence interval (95% CI) to depict the relationships among the overall scale and subscales of violence from stable partners and from clients. Independent variables in bivariate analysis that showed associations with the dependent variable at a significance level of p<0.05 were retained in the multivariate linear regression analyses. The overall scale of stigma was categorized into two groups for the moderation analysis based upon the mean score of the scale. If the overall stigma scale score was higher than the median, it was coded as “1”, otherwise, it was coded as “0”. The interaction of violence from stable partners and violence from clients with mental health problems at low or high stigma level were assessed and plotted (Figure 1-a, and Figure 1-b). Two-way ANOVA was used to test the significance of the interaction.
Fig. 1.
The interaction relation between violence from stable partners and mental health problems by stigma level (a, F=4.373, p<0.05), and the interaction relation between violence from client and mental health problems by stigma level (b, F=0.067, p>0.05).
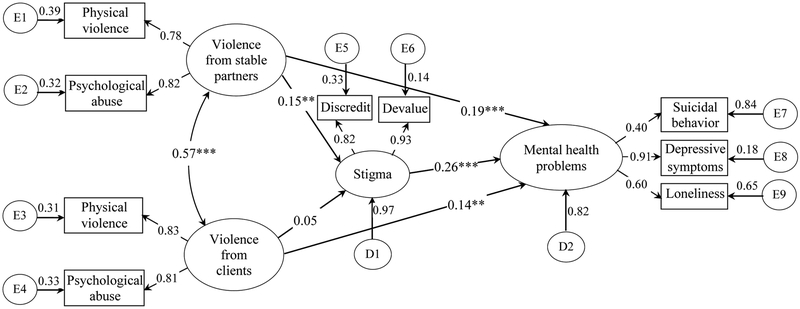
Structural equation modeling (SEM) (Schumacker & Lomax, 2004) was employed to test the hypothesized model that specified the relationships among violence from stable partners, violence from clients, stigma, and mental health problems. Missing data accounted for less than 1% of any variables; thus, missing values were imputed using mean replacement method. A correlation matrix for all indicator variables of the latent variables was used in the SEM model. The relationships among four latent variables (path 1: violence from stable partners → mental health; path 2: violence from stable partners → stigma → mental health; path 3: violence from clients → mental health; path 4: violence from clients → stigma → mental health; path 5: stigma → mental health) were tested, and standardized regression coefficients for all paths were estimated. Model goodness of fit was evaluated using the χ2 test, the comparative fit indices (CFI, >0.90) and root mean square error of approximation (RMSEA, ≤ 0.08), the Tucker-Lewis index (TLI, ≥ 0.90), and χ2/df (≤ 3) (Neumann, Hare, & Johansson, 2013; Schumacker & Lomax, 2004). SPSS 18.0 for Windows was used for bivariate analyses and multivariate linear regression analyses, and M-plus 7.2 was used for SEM.
Results
The mean age of the FSWs in the study sample was 25.3 (SD=6.56) years. About 57% of FSWs were ≤24 years of age. The majority of FSWs were Han (84.7%) ethnicity, came from rural areas (54.3%), and had completed no more than middle school education (62.2%). The average monthly income of these FSWs was 2,657 Yuan (approximately US$422). About half (51.3%) of the FSWs were never married, and 7.0 % FSWs were from outdoor venues, and 93.0% were from indoor venues.
Prevalence of violence
About 36.9% of participants reported experiencing violence from stable partners occasionally, 16.0% sometimes, and 6.0% frequently. Significant differences were observed in prevalence of frequently occurring of violence from stable partners and from clients (6.0% vs. 1.9%, p<0.001), while the prevalence of never having experienced violence from stable partners was lower than the prevalence of never having experienced from clients (72.6% vs. 91.2%, p<0.001). About 38.0% of women reported experiencing violence from clients occasionally, 13.1% sometimes, and 1.9% frequently (Table 2). Educational attainment was significantly associated with prevalence of violence from stable partners (p<0.05). FSWs with primary school education or less were more likely to report experiencing violence from stable partners compared to those FSWs with higher education attainment. FSWs who were drug users were more likely to report experiencing violence from both stable partners (p<0.01) and clients (p<0.05) than non-drug users.
Table 2.
Prevalence of violence among FSWs by demographic characteristics, (N=971)
| Variables | N (%) | Violence from stable partners (% of FSWs above the mean) |
Chi- Square/ t-values |
Violence from clients (% of FSWs above the mean) |
Chi- Square/ t-values |
|---|---|---|---|---|---|
| Age, years, mean (SD) | 25.33 (6.56) | 25.64 (7.36) | 0.134 | 25.23 (6.67) | 0.153 |
| 18~24 | 553 (57.0) | 36.0 | 2.097 | 32.7 | 0.000 |
| ≥25 | 418 (43.0) | 30.8 | 32.7 | ||
| Ethnicity | |||||
| Han | 814 (84.7) | 32.3 | 3.052 | 31.1 | 5.349 |
| Minority | 147 (15.3) | 41.5 | 41.4 | ||
| Residence | |||||
| City | 225 (23.6) | 34.0 | 1.843 | 32.4 | 0.096 |
| County | 210 (22.1) | 29.3 | 33.2 | ||
| Township | 294 (30.9) | 35.8 | 31.8 | ||
| Village | 223 (23.4) | 34.6 | 32.7 | ||
| Educational attainment | |||||
| ≤ Primary school | 95 (9.9) | 44.9 * | 10.673 | 34.1 | 4.121 |
| Middle school | 501 (52.3) | 35.9 | 34.7 | ||
| High school | 335 (35.0) | 27.9 | 28.0 | ||
| ≥ College | 27 (2.8) | 16.7 | 36.0 | ||
| Monthly incomea, mean (SD) | 2657.8 yuan (2371.4) | 2506.80 yuan (2161.56) | 0.446 | 2787.10 (2354.52) | 0.616 |
| ≤ 1000 | 294 (30.6) | 34.7 | 2.296 | 30.6 | 1.339 |
| 1001~2000 | 280 (29.2) | 35.3 | 32.0 | ||
| 2001~3000 | 187 (19.5) | 28.0 | 34.5 | ||
| ≥ 3000 | 199 (20.7) | 34.8 | 35.1 | ||
| Marital status | |||||
| Never married | 492 (51.3) | 33.9 | 1.736 | 32.1 | 1.593 |
| Cohabitation | 180 (18.8) | 31.7 | 34.6 | ||
| Married | 169 (17.6) | 35.8 | 32.9 | ||
| Separated | 47 (4.9) | 25.6 | 25.0 | ||
| Widowed | 72 (7.5) | 34.1 | 34.3 | ||
| Drug use (life time) | |||||
| Yes | 156 (16.2) | 47.0 ** | 11.924 | 38.7 | 3.057 |
| No | 805 (83.8) | 30.5 | 31.3 | ||
| Venue type | |||||
| Indoor | 903 (93.0) | - | - | ||
| Outdoor | 68 (7.0) | - | - | ||
| Violence from stable partners | |||||
| Never (yes%) | 705 (72.6)*** | - | - | ||
| Occasionally (yes%) | 358 (36.9) | - | - | ||
| Sometimes (yes%) | 155 (16.0) | - | - | ||
| Frequently (yes%) | 58 (6.0)*** | - | - | ||
| Violence from clients | |||||
| Never (yes%) | 886 (91.2)*** | - | - | ||
| Occasionally (yes%) | 369 (38.0) | - | - | ||
| Sometimes (yes%) | 127 (13.1) | - | - | ||
| Frequently (yes%) | 18 (1.9)*** | - | - |
Note. The currency exchange rate for RMB yuan and USD was $1=6.3 yuan.
p<0.05
p<0.01
p<0.001.
Multivariate linear regression
FSWs who experienced a higher level of violence from stable partners were more likely to report suicide ideation/attempts (β=0.112, 95% CI=0.058–0.284), depressive symptoms (β=0.193, 95% CI=0.260–0.580) and loneliness (β=0.176, 95% CI=0.184–0.454), adjusting for education and drug use. The overall scale of violence from clients was also significantly associated with all three mental health problems (suicide β=0.113, 95% CI=0.085–0.325; depressive symptoms β=0.190, 95% CI=0.312–0.637; loneliness β=0.141, 95% CI=0.154–0.425), again adjusting for education and drug use (Table 3). Moreover, the two subscales of violence from stable partners and clients were significantly associated with mental health problems, except the relationship between the subscale of physical violence from stable partners and suicide (p>0.05). For instance, the subscale of physical violence from stable partners was significantly associated with depressive symptoms (β=0.136, 95% CI=0.149–0.505), and loneliness (β=0.135, 95% CI=0.122–0.422). The subscale of psychological abuse from stable partners was significantly associated with suicide (β=0.136, 95% CI=0.065–0.222), depressive symptoms (β=0.211, 95% CI=0.207–0.429), and loneliness (β=0.176, 95% CI=0.127–0.315), adjusting for education and drug use.
Table 3.
Multivariate linear regression of mental health problems on violence and stigma
| Suicide |
Depressive symptoms |
Loneliness |
|
|---|---|---|---|
| β(95% CI) | β(95% CI) | β(95% CI) | |
| Violence from stable partners | |||
| Overall scale of violence | 0.112 (0.058-0.284)** | 0.193 (0.260-0.580)*** | 0.176 (0.184-0.454)*** |
| Physical violence | 0.063 (−0.018-0.232) | 0.136 (0.149-0.505)*** | 0.135 (0.122-0.422)*** |
| Psychological abuse | 0.136 (0.065-0.222)*** | 0.211 (0.207-0.429)*** | 0.176 (0.127-0.315)*** |
| Violence from clients | |||
| Overall scale of violence | 0.113 (0.085-0.325)** | 0.190 (0.312-0.637)*** | 0.141 (0.154-0.425)*** |
| Physical violence | 0.132 (0.152-0.457)*** | 0.172 (0.340-0.755)*** | 0.134 (0.176-0.521)*** |
| Psychological abuse | 0.075 (0.008-0.141)* | 0.177 (0.153-0.331)*** | 0.126 (0.067-0.216)*** |
| Stigma | |||
| Overall scale of stigma | 0.095 (0.020-0.100)** | 0.261 (0.177-0.286)*** | 0.148 (0.062-0.154)*** |
| Discredit subscale | 0.061 (−0.001-0.071) | 0.235 (0.140-0.239)*** | 0.118 (0.036-0.120)*** |
| Devalue subscale | 0.110 (0.029-0.106)** | 0.254 (0.165-0.270)*** | 0.155 (0.065-0.153)*** |
Note. β=Standardized coefficient; CI=Confidence Interval; Covariates were education and drug use in the models.
p<0.05
p<0.01
p<0.001.
FSWs who experienced a higher level of stigma were more likely to report suicide, (β=0.095, 95% CI=0.020–0.100), depressive symptoms (β=0.261, 95% CI=0.177–0.286), and loneliness (β=0.148, 95% CI=0.062–0.154) adjusting for education and drug use. Moreover, the two subscales of stigma were significantly associated with mental health problems, except the relationship between the discredit subscale and suicide (p>0.05). For instance, the discredit subscale was significantly associated with depressive symptoms (β=0.254, 95% CI=0.140–0.239), and loneliness (β=0.155, 95% CI=0.036–0.120), adjusting for education and drug use
FSWs who reported a lower level of stigma had a weaker positive relationship between violence from stable partners and mental health problems. A higher level of stigma was more strongly positively related to violence from stable partners and mental health problems (Figure 1-a). However, the moderation effect of stigma was not evident in the relationship between violence from clients and mental health problems (Figure 1-b).
Structural equation modeling
Almost all of the correlation coefficients for indicator variables were statistically significant (p<0.01), except the one between discredit and physical violence from clients (Table 4). All indicators of standardized loadings were statistically significant (p<0.001). In addition, standardized loadings for most indicators’ were higher than 0.70 (except suicide and loneliness indicators), suggesting that all of these indicators were reliable. Because removal of the indicators with standardized loading lower than 0.60 from the scale did not lead to an increase in reliability of mental health problems, we kept all of the indicators in the model. The initial hypothesized model including five paths among latent constructs was tested. Two exogenous variables (i.e., “violence from stable partners”, “violence from clients”) and two endogenous variables (i.e., “stigma” and “mental health”) were included in the model. This structural model demonstrated the direct and indirect associations of intimate partner violence with mental health problems. The overall fit of the final model (Figure 2) was good (χ2/df = 2.98, CFI = 0.98, TLI = 0.97, and RMSEA = 0.05). Both violence from stable partners (standardized path coefficients = 0.19, p<0.001) and violence from clients (standardized path coefficients = 0.14, p<0.01) had significant direct positive associations with mental health problems. However, only violence from stable partners showed an indirect significant association with mental health problems through stigma. Violence from stable partners was positively associated with stigma (standardized path coefficients = 0.15, p<0.01), which in turn was associated with mental health problems. Stigma (standardized path coefficients = 0.26, p<0.001) was directly positively associated with mental health problems.
Table 4.
Correlation coefficients of indicator variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| Violence from stable partners | |||||||||
| Physical violence | 1 | ||||||||
| Psychological abuse | 0.636** | 1 | |||||||
| Violence from clients | |||||||||
| Physical violence | 0.367** | 0.411** | 1 | ||||||
| Psychological abuse | 0.270** | 0.422** | 0.676** | 1 | |||||
| Stigma | |||||||||
| Discredit | 0.083* | 0.112** | 0.065 | 0.066* | 1 | ||||
| Devalue | 0.101** | 0.168** | 0.109** | 0.112** | 0.759** | 1 | |||
| Mental health problems | |||||||||
| Suicidal behavior | 0.127** | 0.173** | 0.155** | 0.078* | 0.074* | 0.120** | 1 | ||
| Depressive symptoms | 0.183** | 0.248** | 0.209** | 0.200** | 0.251** | 0.259** | 0.355** | 1 | |
| Loneliness | 0.144** | 0.176** | 0.163** | 0.140** | 0.130** | 0.170** | 0.206** | 0.544** | 1 |
| Mean | 10.58 | 8.33 | 10.61 | 6.07 | 13.45 | 17.69 | 2.17 | 36.08 | 43.17 |
| SD | 2.07 | 2.20 | 1.58 | 1.81 | 3.58 | 4.62 | 0.69 | 9.56 | 7.83 |
Note. p<0.05
p<0.01
SD=standard deviation.
Fig. 2.
Structural model showing the relationships between violence from stable partners, violence from clients, stigma and mental health problems among female sex workers (R-square value was 0.18 for the outcome). *p<0.05; **p<0.01; ***p<0.001. (Model fit: CFI=0.981; TLI=0.970; RMSEA=0.050; Chi-Square/DF=2.98).
Discussions
The results of our study confirm and expand the findings of earlier studies. Consistent with previous research (Ellsberg et al., 2008), our study revealed that violence from either stable partners or clients, and internalized stigma had direct associations with suicidal thoughts and behaviors, depressive symptoms and loneliness. Our results also indicated that violence from stable partners had an indirect association with mental health problems through stigma.
FSWs are a stigmatized population worldwide. Because of stigmatization, FSWs who experience partner violence may lack needed social support, counseling, and access to health care resources (Overstreet & Quinn, 2013). FSWs with internalized stigma may fear future violence/abuse by their partners as a result of reaching out for help. The stigmatization faced by FSWs who experience partner violence also negatively affects their access to support and treatment and exacerbates poor mental health outcomes (Vogel, Wade, & Hackler, 2007).
This study found that violence perpetrated by stable partners had an indirect association with mental health problems through stigma. Violence perpetrated by clients did not show an indirect association through stigma perhaps because of different effects between violence from stable partners and violence from clients on mental health problems. Internalized stigma is a negative attitude toward oneself, which acts as the stressor, resulting in the mental health problem. The stress cognitive appraisal of FSWs who experience violence from stable partners or from clients may differ in stress reactions and perceived coping resources (Rusch, Corrigan, Powell, et al., 2009; Rusch, Corrigan, Wassel, et al., 2009). FSWs who experienced violence from stable partners may have had low perceived coping resources compared with those who experienced violence from clients. Usually, stigmatized individuals may prevent themselves from the negative effects through three psychological processes: compensation, selective social comparison and attributions, and multiple identities (Shih, 2004). FSWs who experienced violence from clients may have been more likely to develop social interaction skills to overcome the adversities associated with stigma. FSWs who have experienced violence from clients may have compared their situation with that of other FSWs when they perceived the violence occurred in the venues where they worked. FSWs who experienced violence from clients may have been more able to prevent themselves from poor outcomes through adopting protective strategies with less internalization of stigma and more social support. It is also possible that FSWs who were hurt by clients could avoid those clients in future, but the FSWs who were hurt by stable partners may have had less control over their relationships because FSWs may want to maintain their multiple identities, such as wife or lover. Such multiple identities of FSWs may make FSWs less likely to disclose their experience of violence from stable partners and more likely to have higher internalized stigma. All these hypotheses regarding the possible effects of violence from different perpetrators need to be explored in future research.
The limitations of this study should be noted. First, causal interpretations are precluded because the data used were from a cross-sectional study so that temporal relations could not be established. Second, data in the current study were collected through self-report which may have resulted in reporting bias. Third, the sample in the current study was from one geographical area in China; therefore, it may not be representative of FSWs in other regions of China. Fourth, the stigma subscale had a low Cronbach’s alpha value (0.61) in this study. More items are needed in future research in this area to improve this subscale. We combined items of physical violence with sexual violence in the current study because the sexual violence scale had a lower Cronbach’s alpha. However, sexual violence is one critical domain of intimate partner violence. In future research, this subscale needs to be improved by adding more items. In addition, the study sample was recruited through venue-based sampling without attempting street-based recruitment of FSWs. This recruitment strategy might have resulted in an underestimate of the prevalence of violence among FSWs because street-based FSWs may have a higher prevalence of partner violence than venue-based FSWs (Shannon et al., 2009). We did not adjust our analyses for clustering because about one third of venues (of total 60 venues) had only 2–7 FSWs each, with a very skewed distribution of indoor FSW (7.0%) compared to outdoor (93.0%) FSWs. Finally, some variables representing sex work characteristics, such as years engaged in sex work and frequency of days worked, might have affected exposure to violent victimization, but we did not collect such data in this study.
Despite these limitations, our study presents one of the first efforts to explore the direct and indirect associations of intimate partner violence with mental health problems experienced by FSWs in China. Our results have some implications for future health promotion and policy research. First, future research should include multiple mediating and moderating variables that may be related to the process by which intimate partner violence affect mental health among FSWs. Second, the relationships between self-esteem, self-efficacy, internalized stigma, help-seeking behaviors, and other social and cultural factors related to the violence in FSWs need to be studied further. Third, to promote women’s health (particularly mental health in FSWs), interventions to decrease intimate partner violence, stigma (particularly internalized stigma), as well as to increase self-esteem and self-efficacy of seeking health care services are necessary. Results from this study highlight a need for counseling and care interventions to address the experience of violence and post-violence mental health needs in FSWs. The types of violence perpetrators (stable partners, clients) of FSWs also need to be taken into account by the health care providers during counseling and treatment. Moreover, factors related to social support and service seeking behaviors after experiencing violence should be considered in future research to improve mental health outcomes. However, seeking services after experiencing violence for FSWs is particularly challenging in China, not only because it is illegal and immoral for commercial sex, but also because of their fear of stigmatization from health care providers and the general public, as well as the fear of further escalating violence from their perpetrators. Therefore, both micro- and macro-interventions to address intimate partner violence, stigma, and mental health issues among FSWs are sorely needed. For example, the services of post-violence mental health screening and counseling can be integrated into HIV related health services. The social “norm” of discrimination against FSWs also needs to be changed. FSWs who experience violence are victims themselves and should be treated with compassion and respect to encourage them to seek necessary health care services.
Acknowledgements
This study was supported by NIH Research Grant R01AA018090–02 by the National Institute for Alcohol Abuse and Alcoholism (NIAAA). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIAAA. The authors want to thank local team members at Beihai CDC and Guilin CDC for their efforts in instrument development and data collection. Thanks also go to Drs Linda Kaljee and Iqbal H Shah for their valuable comments on the draft of the manuscript.
References
- Antai D (2011). Traumatic physical health consequences of intimate partner violence against women: what is the role of community-level factors? BMC Womens Health, 11, 56–69. doi: 10.1186/1472-6874-11-56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badcock JC, Shah S, Mackinnon A, Stain HJ, Galletly C, Jablensky A, & Morgan VA (2015). Loneliness in psychotic disorders and its association with cognitive function and symptom profile. Schizophrenia Research, 169(3–4), 268–273. doi: 10.1016/j.schres.2015.10.027 [DOI] [PubMed] [Google Scholar]
- Boardman F, Griffiths F, Kokanovic R, Potiriadis M, Dowrick C, & Gunn J (2011). Resilience as a response to the stigma of depression: A mixed methods analysis. Journal of Affective Disorders, 135(1–3), 267–276. [DOI] [PubMed] [Google Scholar]
- Corrigan P (2004). How stigma interferes with mental health care. American Psychologist, 59(7), 614–625. [DOI] [PubMed] [Google Scholar]
- Davidson MM, & Gervais SJ (2015). Violence against women through the lens of objectification theory. Violence Against Women, 21(3), 330–354. doi: 10.1177/1077801214568031 [DOI] [PubMed] [Google Scholar]
- Elklit A, & Shevlin M (2007). The structure of PTSD symptoms: A test of alternative models using confirmatory factor analysis. British Journal of Clinical Psychology, 46, 299–313. doi: 10.1348/014466506X171540 [DOI] [PubMed] [Google Scholar]
- Ellsberg M, Jansen HAFM, Heise L, Watts CH, Garcia-Moreno C, & Hlth WMSW (2008). Intimate partner violence and women’s physical and mental health in the WHO multi-country study on women’s health and domestic violence: an observational study. Lancet, 371(9619), 1165–1172. doi: Doi 10.1016/S0140-6736(08)60522-X [DOI] [PubMed] [Google Scholar]
- Guillen AI, Panadero S, Rivas E, & Vazquez JJ (2015). Suicide attempts and stressful life events among female victims of intimate partner violence living in poverty in Nicaragua. Scandinavian Journal of Psychology, 56(3), 349–356. doi: 10.1111/sjop.12207 [DOI] [PubMed] [Google Scholar]
- Herek GM, Saha S, & Burack J (2013). Stigma and psychological distress in people with HIV/AIDS. Basic Appl Soc Psych, 35(1), 41–54. [Google Scholar]
- Hong Y, Fang X, Li X, Liu Y, Li M, & Tai-Seale T (2010). Self-perceived stigma, depressive symptoms, and suicidal behaviors among female sex workers in China. J Transcult Nurs, 21(1), 29–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong Y, Zhang C, Li X, Liu W, & Zhou Y (2013). Partner violence and psychosocial distress among female sex workers in China. PLoS One, 8(4), e62290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman J (2011). HIV, Sex Work, and Civil Society in China. Journal of Infectious Diseases, 204, S1218–S1222. doi: 10.1093/infdis/jir538 [DOI] [PubMed] [Google Scholar]
- Kleinman A, & Hall-Clifford R (2009). Stigma: a social, cultural and moral process. Journal of Epidemiology and Community Health, 63(6), 418–419. doi: 10.1136/jech.2008.084277 [DOI] [PubMed] [Google Scholar]
- Lin N (1989). Measuring depressive symptomatology in China. J Nerv Ment Dis, 177, 121–131. [DOI] [PubMed] [Google Scholar]
- Liu H, Feng T, & Rhodes AG (2009). Assessment of the Chinese version of HIV and homosexuality related stigma scales. Sexually Transmitted Infections, 85(1), 65–69. [DOI] [PubMed] [Google Scholar]
- Mak WWS, Poon CYM, Pun LYK, & Cheung SF (2007). Meta-analysis of stigma and mental health. Social Science & Medicine, 65(2), 245–261. doi: 10.1016/j.socscimed.2007.03.015 [DOI] [PubMed] [Google Scholar]
- Mashiach-Eizenberg M, Hasson-Ohayon I, Yanos PT, Lysaker PH, & Roe D (2013). Internalized stigma and quality of life among persons with severe mental illness: the mediating roles of self-esteem and hope. Psychiatry Research, 208(1), 15–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Bureau of Statistics of China. (2011). Population distinction by age and sex. Avaiable at http://www.stats.gov.cn/tjsj/pcsj/rkpc/6rp/html/A0107a.htm, access onhttp:// March 6, 2015.
- Neumann CS, Hare RD, & Johansson PT (2013). The psychopathy checklist-revised (PCL-R), low anxiety, and fearlessness: a structural equation modeling analysis. Personality Disorders-Theory Research and Treatment, 4(2), 129–137. [DOI] [PubMed] [Google Scholar]
- Oliver-Velez D, Finlinson HA, Deren S, Robles RR, Shedlin M, Andia J, & Colon H (2002). Mapping the air-bridge locations: The application of ethnographic mapping techniques to a study of HIV risk behavior determinant in East Harlem, New York, and Bayamon, Puerto Rico. Human Organization, 61(3), 262–276. [Google Scholar]
- Overstreet NM, & Quinn DM (2013). The intimate partner violence stigmatization model and barriers to help-seeking. Basic Appl Soc Psych, 35(1), 109–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padurariu M, Ciobica A, Persson C, & Stefanescu C (2011). Self-stigma in psychiatry: ethical and bio-psycho-social perspectives. Revista Romana De Bioetica, 9(1), 76–82. [Google Scholar]
- Patel SK, Saggurti N, Pachauri S, & Prabhakar P (2015). Correlates of mental depression among female sex workers in Southern India. Asia-Pacific Journal of Public Health, 27(8), 809–819. doi: 10.1177/1010539515601480 [DOI] [PubMed] [Google Scholar]
- Pirkle C, Soundardjee R, & Stella A (2007). Female sex workers in China: vectors of disease? Sex Transm Dis, 34(9), 695–703. [DOI] [PubMed] [Google Scholar]
- Postmus JL (2015). Women from different ethnic groups and their experiences with victimization and seeking help. Violence Against Women, 21(3), 376–393. doi: 10.1177/1077801214568254 [DOI] [PubMed] [Google Scholar]
- Radloff LS (1970). The CES-D scale: A self-report depression scale for research in the general population. Appl Psych Meas, 1(3), 385–401. [Google Scholar]
- Rokach A (2007). Loneliness and intimate partner violence: Antecedents of alienation of abused women. Soc Work Health Care, 45(1), 19–31. doi: 10.1300/J010v45n01_02 [DOI] [PubMed] [Google Scholar]
- Rusch N, Corrigan PW, Powell K, Rajah A, Olschewski M, Wilkniss S, & Batia K (2009). A stress-coping model of mental illness stigma: II. Emotional stress responses, coping behavior and outcome. Schizophrenia Research, 110(1–3), 65–71. doi: 10.1016/j.schres.2009.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rusch N, Corrigan PW, Wassel A, Michaels P, Olschewski M, Wilkniss S, & Batia K (2009). A stress-coping model of mental illness stigma: I. Predictors of cognitive stress appraisal. Schizophrenia Research, 110(1–3), 59–64. doi: 10.1016/j.schres.2009.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell D, Peplau LA, & Ferguson ML (1978). Developing a measure of loneliness. J Pers Assess, 42, 290–294. [DOI] [PubMed] [Google Scholar]
- Sabri B, Huerta J, Alexander KA, St Vil NM, Campbell JC, & Callwood GB (2015). Multiple Intimate Partner Violence Experiences: Knowledge, Access, Utilization and Barriers to Utilization of Resources by Women of the African Diaspora. Journal of Health Care for the Poor and Underserved, 26(4), 1286–1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallmann J (2010). Living with stigma: Women’s experiences of prostitution and substance use. Journal of Women and Social Work, 25(2), 146–159. [Google Scholar]
- Schumacker R, & Lomax R (2004). A beginner’s guide to structural equation modeling. Mahwah, New Jersey: Lawrence Erlbaum Associations, Inc. [Google Scholar]
- Semple SJ, Stockman JK, Pitpitan EV, Strathdee SA, Chavarin CV, Mendoza DV, . . . Patterson TL (2015). Prevalence and correlates of client-perpetrated violence against female sex workers in 13 Mexican cities. PLoS One, 10(11). doi: 10.1371/journal.pone.0143317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shannon K, Kerr T, Strathdee SA, Shoveller J, Montaner JS, & Tyndall MW (2009). Prevalence and structural correlates of gender based violence among a prospective cohort of female sex workers. British Medical Journal, 339. doi: 10.1136/Bmj.B2939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shih M (2004). Positive stigma: Examining resilience and empowerment in overcoming stigma. Annals of the American Academy of Political and Social Science, 591, 175–185. [Google Scholar]
- Silverman JG, Gupta J, Decker MR, Kapur N, & Raj A (2007). Intimate partner violence and unwanted pregnancy, miscarriage, induced abortion, and stillbirth among a national sample of Bangladeshi women. BJOG, 114(10), 1246–1252. doi: 10.1111/j.1471-0528.2007.01481.x [DOI] [PubMed] [Google Scholar]
- Ulibarri MD, Strathdee SA, Lozada R, Magis-Rodriguez C, Amaro H, O’Campo P, & Patterson TL (2010). Intimate partner violence among female sex workers in two Mexico-U.S. border cities: partner characteristics and HIV risk behaviors as correlates of abuse. Psychological Trauma, 2(4), 318–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vijayakumar G, Chacko S, & Panchanadeswaran S (2015). ‘As human beings and as workers’: Sex worker unionization in Karnataka, India. Global Labour Journal, 6(1), 79–96. [Google Scholar]
- Vogel DL, Wade NG, & Hackler AH (2007). Perceived public stigma and the willingness to seek counseling: The mediating roles of self-stigma and attitudes toward counseling. Journal of Counseling Psychology, 54(1), 40–50. [Google Scholar]
- World Health Organization. (2003). WHO multi-country study on women’s health and life experiences. Geneva: WHO. [Google Scholar]
- Zhang C, Li XM, Chen YY, Hong Y, Shan Q, Liu W, & Zhou YJ (2014). Alcohol and other drug use, partner violence, and mental health problems among female sex workers in Southwest China. Health Care Women Int, 35(1), 60–73. doi: 10.1080/07399332.2012.757317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C, Li XM, Hong Y, Chen YY, Liu W, & Zhou YJ (2012). Partner violence and HIV risk among female sex workers in China. AIDS and Behavior, 16(4), 1020–1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Y, Li X, Zhang C, Tan G, Stanton B, Zhang X, & Cui Y (2013). Rates of HIV, syphilis, and HCV infections among different demographic groups of female sex workers in Guangxi China: Evidence from 2010 national sentinel surveillance data. AIDS Care, 25(11), 1433–1441. doi: 10.1080/09540121.2013.772282 [DOI] [PMC free article] [PubMed] [Google Scholar]