Abstract
Purpose
To investigate the pathophysiologic effects of chronic kidney disease (CKD) on brain function in children with CKD by correlating cerebral blood flow (CBF) with clinical and behavioral indexes.
Materials and Methods
In this prospective study, 73 pediatric patients with CKD (mean age, 15.80 years ± 3.63; range, 9–25 years) and 57 control subjects (mean age, 15.65 years ± 3.76; range, 9–25 years) were recruited. CBF measurements were acquired with an MRI arterial spin labeling scheme. Neurocognitive measurements were performed with traditional and computerized neurocognitive batteries. Clinical data were also collected. Group-level global and regional CBF differences between patients with CKD and control subjects were assessed. Regression analyses were conducted to evaluate the associations among regional CBF, clinical variables, and cognitive performance.
Results
Patients with CKD showed higher global CBF compared with control subjects that was attributable to reduced hematocrit level (mean, 60.2 mL/100 g/min ± 9.0 vs 56.5 mL/100 g/min ± 8.0, respectively). White matter CBF showed correlation with blood pressure (r = 0.244, P = .039), a finding suggestive of altered cerebrovascular autoregulation. Regional CBF differences between patients and control subjects included regions in the “default mode” network. In patients with CKD, positive extrema in the precuneus showed a strong correlation with executive function (ρ = 0.608, P = .001).
Conclusion
Systemic effects of estimated glomerular filtration rate, hematocrit level, and blood pressure on CBF and alterations in regional CBF may reflect impaired brain function underlying neurocognitive symptoms in CKD. These findings further characterize the nature of alterations in brain physiologic features in children, adolescents, and young adults with CKD.
© RSNA, 2018
Introduction
Chronic kidney disease (CKD) is associated with alterations in blood pressure, blood chemistry, and red blood cell production (1) that can potentially affect brain function. Previous studies in adults have shown that CKD is associated with subcortical ischemic lesions, atrophy, and deficits in cognitive performance (2,3). However, the mechanisms by which CKD affects brain function and the time course of such effects are unknown.
CKD-associated structural brain changes are characteristic of ischemic small-vessel disease, which manifests as white matter hyperintensities at T2-weighted MRI, and are most commonly seen in adults with chronic atherosclerotic vascular disease and hypertension. Moreover, even mild CKD significantly increases the risk for transient ischemic attack and stroke (4). Given the high incidence of cardiovascular disease in CKD and the associations between CKD and neurologic dysfunction (1,5,6), further characterization of cerebrovascular function in CKD is highly relevant; however, studies of cerebrovascular function in adults with CKD are confounded by long-standing hypertension—itself a leading cerebrovascular risk factor. Although CKD in adults is often a consequence of age-related disorders such as hypertension and diabetes, childhood CKD often occurs congenitally, yet still affects brain development and cognitive function (2,7). Examining cerebrovascular function in a pediatric population with CKD provides the potential to dissociate CKD effects from those of associated chronic hypertensive vasculopathy.
Cerebral blood flow (CBF) provides a direct measure of cerebrovascular integrity by providing quantification of cerebral perfusion. Regional CBF also serves as a marker of regional neural activity owing to the tight coupling between regional CBF and neural activity and metabolism (8–10). However, existing data on regional CBF in CKD are limited, particularly for pediatric CKD. This limitation is partly due to the contraindication to intravenous contrast agents in patients with kidney dysfunction because the majority of MRI perfusion studies rely on dynamic contrast material approaches.
Herein, we report the findings of arterial spin labeling (ASL) MRI data acquired in the Neurocognitive Assessment and Magnetic Resonance Imaging Analysis of Children and Young Adults with Chronic Kidney Disease (NiCK) study cohort (11). We used ASL MRI in combination with individual hematocrit level–corrected blood T1 to investigate CBF differences between pediatric patients and healthy control subjects. We hypothesized that CKD-associated systemic factors such as anemia (12) and hypertension would cause global abnormalities in CBF and that regional alterations in CBF would be associated with changes in neurocognitive performance in patients with CKD.
Materials and Methods
This prospective study was approved by the institutional review board of the Children’s Hospital of Philadelphia and compliant with the Health Insurance Portability and Accountability Act. Informed consent was obtained from each participant and/or his or her parent or guardian. Study data were collected and managed by using REDCap (Research Electronic Data Capture) electronic data capture tools hosted at The Children’s Hospital of Philadelphia (13). REDCap is a secure, web-based application designed to support data capture for research studies, providing (a) an intuitive interface for validated data entry, (b) audit trails for tracking data manipulation and export procedures, (c) automated export procedures for seamless data downloads to common statistical packages, and (d) procedures for importing data from external sources.
Participants
Between August 2011 and October 2014, 73 patients with stage II–V CKD aged 8–25 years and 57 age-matched control subjects were included (Table 1, Appendix E1 [online], Fig E1 [online]) (11). Patients were excluded if they had (a) a history of traumatic brain injury or other significant medical or neurologic abnormality affecting motor or higher cortical functioning, (b) profound developmental disability or sensory-motor difficulties that would preclude valid use of diagnostic instruments or measurements based on eye tracking or MRI, (c) a Diagnostic and Statistical Manual of Mental Disorders, fourth edition, text revision axis I disorder or other psychiatric symptoms that would interfere with the subject’s ability to participate in the study (eg, active psychosis), or (d) known drug or alcohol use within 24 hours of any assessment. For control subjects, individuals matched in age were recruited. Participants in the typically developing control group had no history of CKD, nor any reported history of other neurologic or psychiatric conditions.
Table 1:
Subject Demographics and Selected Clinical Measurements
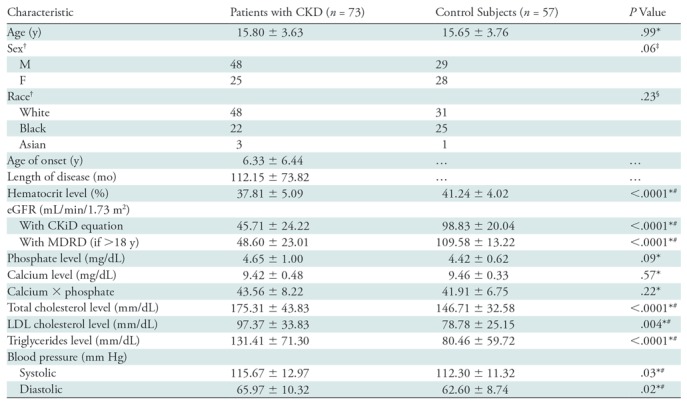
Note.—Except where indicated, data are means ± standard deviations. CKD = chronic kidney disease, CKiD = Chronic Kidney Disease in Children, eGFR = estimated glomerular filtration rate, MDRD = Modification of Diet in Renal Disease, LDL = low-density lipoprotein.
*Determined with the Wilcoxon rank test.
†Data are numbers of patients.
‡Determined with the Fisher exact test.
§Determined with the χ2 test.
#Statistically significant.
Neurocognitive Assessment
Assessments of the traditional neurocognitive battery and a locally developed computerized neurocognitive battery (14,15) were performed. For the traditional neurocognitive battery, a battery of age-specific standardized neurocognitive assessments was performed to assess targeted areas of neurocognition, including intellectual and executive functioning, attention, memory, and visual spatial processing (16). The computerized neurocognitive battery includes 14 tests assessing five neurobehavioral functions: executive control, episodic memory, complex cognition, social cognition, and praxis speed. Each test provides measures of both accuracy and speed (17). All tests were administered by a trained examiner supervised by a licensed psychologist. The details of those measurements are described in Appendix E1 (online), along with laboratory and blood pressure measurements.
Data Acquisition
MRI data were acquired with a 3.0-T whole-body MR unit (Verio; Siemens, Erlangen, Germany) with an eight-channel receive-only head coil and body coil transmission. High-spatial-resolution structural MRI (magnetization-prepared rapid acquisition gradient-echo sequence, 0.9 × 0.8 × 0.8 mm3; repetition time msec/echo time msec, 2000/3.3) and T2-weighted fluid-attenuated inversion recovery data were collected for each participant. Resting CBF measurements were acquired with a pseudocontinuous ASL labeling scheme (18) implemented with a two-dimensional gradient-echo echo-planar imaging sequence. The labeling duration was 1.5 seconds, with a postlabeling delay of 1.2 seconds. Multisection perfusion maps were acquired with the following parameters: 4000/12; flip angle, 90°; bandwidth, 3005 Hz per pixel; section thickness, 5 mm with 25% distance factor; matrix size, 64 × 64; field of view, 220 × 220 mm2; section number, 20; and generalized autocalibrating partial parallel acquisition factor, 2 in phase-encoding direction. The total ASL MRI acquisition time was approximately 5 minutes for 40 label-control pairs.
Data Processing and Analysis
MRI data were processed with software (Statistical Parametric Mapping, version SPM8, and customized MATLAB scripts; MathWorks, Natick, Mass). CBF maps were calculated with a modified perfusion data processing toolbox (ASLtbx) (19). Global CBF values of whole brain, gray matter, and white matter areas were obtained from nonnormalized segmented images (Fig E2 [online]). To optimally address the confounding effect of hematocrit changes in ASL CBF quantification in CKD, we used the method of hematocrit-based T1 estimation (20) for the CBF quantification.
Statistical Analysis
Sample size justification.—The NiCK study had a targeted recruitment of 90 control subjects without CKD and 90 subjects with CKD (estimated glomerular filtration rate [eGFR] <60 mL/min/1.73 m2). On the basis of a review article that reported a 12%–50% prevalence of either white matter lesions or atrophy in children with kidney disease (21), we assumed that in the 90 patients with CKD the prevalence of MRI abnormalities would be 12.5% and that it would be 1% in the control subjects without CKD; the study therefore would have 80% power to detect such a difference with 95% confidence. The NiCK study ultimately recruited 92 patients and 70 control subjects. Data from study subjects with successful ASL MRI acquisitions were included in the present report.
Statistical mapping of group comparison in CBF maps.—Group-level voxel-wise differences in normalized CBF maps between patients with CKD and control subjects were assessed with a cluster-wise permutation-based method thresholded at P < .05, with hematocrit level, age, and sex as covariates of no interest. Subject-specific voxel-wise analysis was also performed to delineate regions with abnormally increased or decreased CBF (extreme voxels) in each individual participant with use of the distribution-corrected z score, or DisCo-Z, method (22) (Appendix E1 [online]).
The general linear model (type III sum of squares) was used to evaluate differences of global CBF values between patients with CKD and control subjects, with comparison of group, sex, and the interaction of group by sex and adjustment for age and hematocrit level. To further explore whether group differences in global CBF were driven by hematocrit level changes in CKD, we performed a stepwise regression analysis to examine the relationship between CBF outcome and factors of CKD (group), hematocrit level, age, and sex. The regression analysis was used to predict each CBF outcome (gray matter, white matter, and whole brain) with use of group, age, sex, hematocrit level, and the interactions of group by sex, group by age, and group by hematocrit level as predictors. Because CKD has been associated with white matter disease and white matter was reported to be particularly susceptible to ischemic injury with impaired CBF autoregulation owing to its blood supply (23,24), we further investigated the effect of altered blood pressure on CBF changes, focusing on the white matter. We examined the correlation between blood pressure and white matter CBF by controlling for hematocrit level, age, and sex.
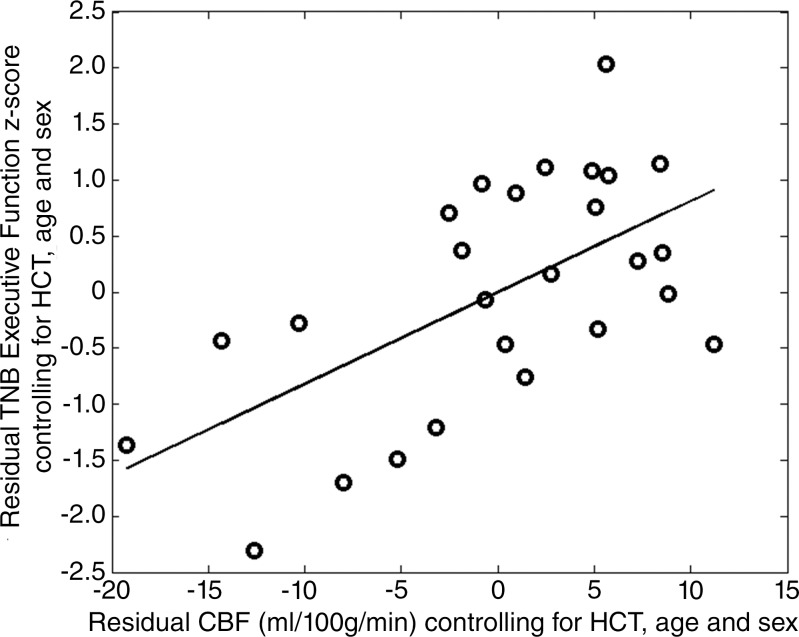
To examine how regional CBF related to cognitive performance between the two groups, we performed correlation analyses on memory, executive function, language reasoning, and spatial processing. Wilcoxon rank sum tests were used to evaluate the group differences in neurocognitive performance for each test between patients with CKD and control subjects. Extreme value maps calculated from the subject-specific voxel-wise analysis were used as masks to extract CBF for each subject. The method of generalized estimating equations was used to test the difference in neurocognitive performance between CKD subgroups with and without the presence of positive extrema in CBF. Spearman rank correlation analysis was then used to evaluate the association of extracted CBF and neurocognitive performance for both patients with CKD and control subjects. Qualitative inspection of common locations of subject-specific increases in CBF for patients with CKD showed high intersubject overlap of clusters in the precuneus, which is similar to the group-level voxel-wise comparison (Figs 1, 2). Therefore, an exploratory analysis was conducted to investigate the relationship between the CBF changes in the precuneus and neurocognitive impairment.
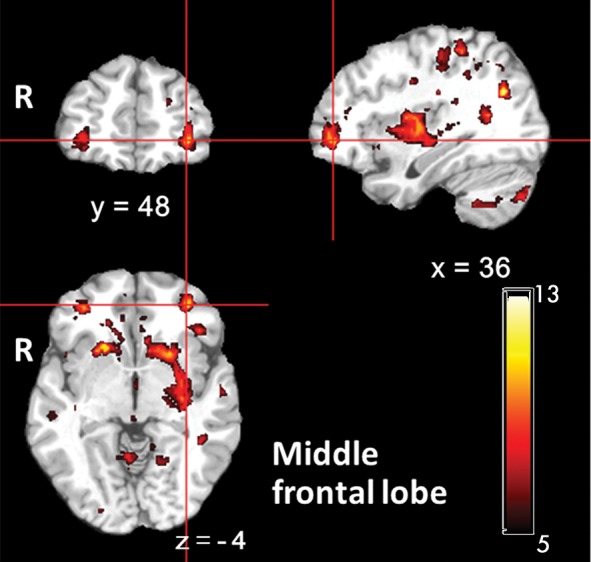
Figure 1:

Voxel-wise group comparison of cerebral blood flow (CBF) after removal of effects of hematocrit level, age, and sex. Contrast shown demonstrates regions where CBF in patients with chronic kidney disease (CKD) is greater than that in control subjects. There were no regions where control subjects showed greater CBF than patients with CKD. Color bar indicates t scores. x, y, z = coordinates in Montreal Neurological Institute (MNI) space.
Figure 2a:
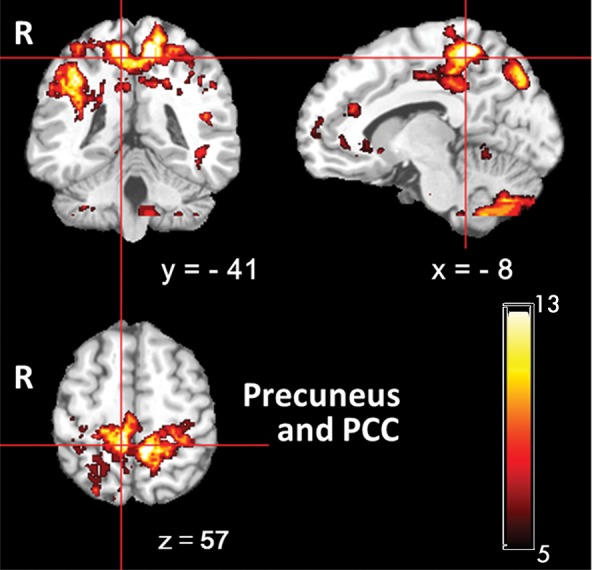
Images show overlapped clusters from all individual patients with chronic kidney disease with positive extrema in cerebral blood flow (CBF) in subject-specific voxel-wise analysis. Color bar indicates total number of subjects who had subject-specific clusters with increased CBF. x, y, z = coordinates in Montreal Neurological Institute (MNI) space.
Figure 2b:
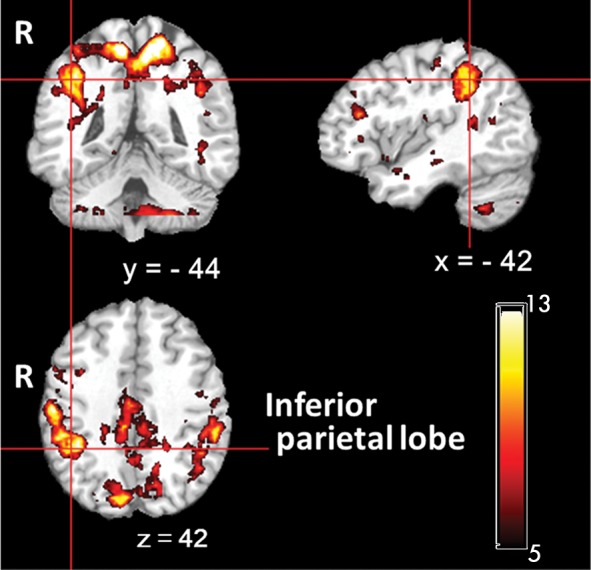
Images show overlapped clusters from all individual patients with chronic kidney disease with positive extrema in cerebral blood flow (CBF) in subject-specific voxel-wise analysis. Color bar indicates total number of subjects who had subject-specific clusters with increased CBF. x, y, z = coordinates in Montreal Neurological Institute (MNI) space.
Figure 2c:
Images show overlapped clusters from all individual patients with chronic kidney disease with positive extrema in cerebral blood flow (CBF) in subject-specific voxel-wise analysis. Color bar indicates total number of subjects who had subject-specific clusters with increased CBF. x, y, z = coordinates in Montreal Neurological Institute (MNI) space.
Figure 2d:
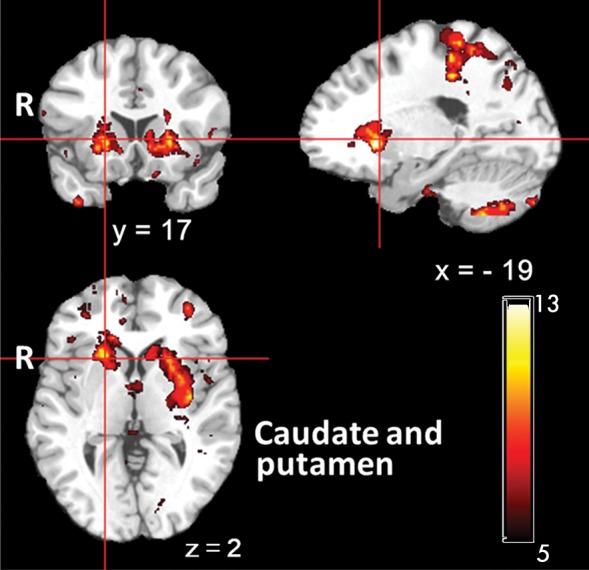
Images show overlapped clusters from all individual patients with chronic kidney disease with positive extrema in cerebral blood flow (CBF) in subject-specific voxel-wise analysis. Color bar indicates total number of subjects who had subject-specific clusters with increased CBF. x, y, z = coordinates in Montreal Neurological Institute (MNI) space.
Results
Demographic and Clinical Characteristics
Table 1 shows the demographic and clinical characteristics of the subjects recruited for the study. As expected, the hematocrit level and eGFR were lower in patients with CKD than in control subjects (P < .0001). Patients with CKD showed significantly elevated lipid levels (P < .005). A significant difference was also noted between these two groups in systolic (P = .03) and diastolic (P = .02) blood pressure.
Global CBF Group Comparison and Clinical Correlates
Patients showed a trend toward higher mean gray matter and whole-brain CBF values compared with control subjects (Table 2). However, general linear model type III analysis showed that group differences in CBF were not significant after controlling for hematocrit level (Table 2). Both patients with CKD and control subjects showed significant correlations of CBF with age and hematocrit level. In control subjects, the eGFR showed a significant correlation with hematocrit level (ρ = −0.456, P < .0005) and CBF (P < .0005) (Fig E3 [online], Table 3); however, after controlling for hematocrit level, significant correlations between CBF and eGFR became much weaker in gray matter (ρ = 0.342, P = .01) and whole brain (ρ = 0.291, P = .03). For patients with CKD, there was no significant correlation between eGFR and hematocrit level (ρ = 0.221, P = .06) or between eGFR and CBF (P > .05) (Table 3). White matter and whole-brain CBF showed a negative correlation with the length of disease in patients with CKD. Patients with CKD also showed a significant correlation of CBF with phosphate in gray matter, white matter, and whole-brain areas, but not after controlling for hematocrit level.
Table 2:
Differences in CBF between Patients with CKD and Control Subjects in Group Comparison for Gray Matter, White Matter, and Whole Brain with General Linear Model Type III Sum of Squares
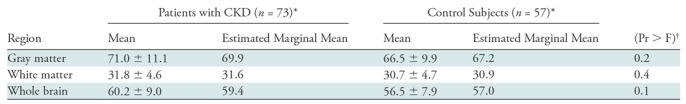
Note.—CBF = cerebral blood flow, CKD = chronic kidney disease
*Data are given in milliliters per 100 grams per minute.
†General linear model type III sum of squares, comparing group, sex, and interation of group by sex and adjusting for age and hematocrit level.
Table 3.
: Univariate Spearman Correlation Coefficients for CBF and Clinical and Demographic Variables
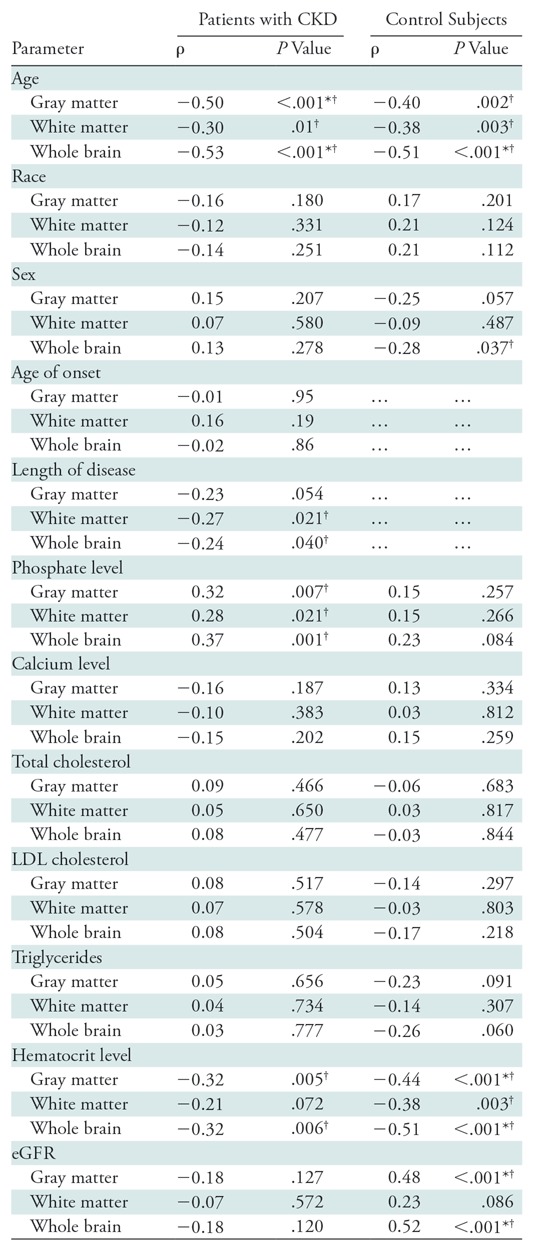
Note.—CBF = cerebral blood flow, CKD = chronic kidney disease, eGFR = estimated glomerular filtration rate, LDL = low-density lipoprotein.
*P < .001, statistically significant after Bonferroni correction.
†Statistically significant.
We found that age, hematocrit level, and interaction of CKD by sex explained most of the variability in CBF for both gray matter and whole brain (gray matter CBF: regression coefficient = −1.09, −0.52, and 3.89, respectively; P = 5 × 10−6, .003, and .02 for age, hematocrit level, and interaction of CKD by sex, respectively; whole-brain CBF: regression coefficient = −1.00, −0.44, and 2.82, and P = 10−7, .001, and .03 for age, hematocrit level, and interaction of CKD by sex, respectively) (Table E1 [online]). Age explained most of the variability in white matter CBF (regression coefficient = −0.43, P = 6.2 × 10−5). The effect of sex on CBF within each group was further explored by using analysis of covariance and controlling for age. Table E2 (online) presents results comparing participants’ sex within each study group. In the control group, female subjects showed higher whole-brain CBF values than did male subjects. However, the effect of sex on global CBF was not significant after controlling for hematocrit level (analysis of covariance: F = 1.021, 0.962, and 1.384 for CBF in gray matter, white matter, and whole brain, respectively [P = .317, 0.331, and 0.245]). In the control group, the hematocrit level in male subjects was significantly higher than that in female subjects (Table E2 [online]). In patients with CKD, no significant sex differences in either CBF or hematocrit level were observed (Table E2 [online]).
The CKD group showed a marginally positive correlation between blood pressure and CBF in white matter (r = 0.244, P = .039, controlling for hematocrit level, age, and sex) (Fig E4 [online]), whereas no significant correlation between blood pressure and white matter CBF was observed in control subjects (r = −0.11, P = .411).
Regional CBF Differences between CKD and Control Groups
In a group-level analysis, after removing the effects of hematocrit level, age, and sex, we found residual clusters in bilateral prefrontal cortices, middle and inferior temporal cortices, the posterior cingulate cortex, the precuneus, the left hippocampus, the striatum, and the thalamus. Patients with CKD showed higher CBF than did control subjects in these regions (Fig 1). There were no regions in which control subjects showed significantly higher CBF than patients with CKD.
Using the subject-specific distribution-corrected z score method, we detected regions of positive extrema in 26 of the 73 patients with CKD and seven of the 57 control subjects and negative extrema in 11 of the 73 patients with CKD and 12 of the 57 control subjects (Table E3 [online]). Patients with CKD showed a significantly higher incidence (P = .002, Table E3 [online]) and larger total volume (P = .0016, Table E4 [online]) of positive extreme clusters with increased CBF as compared with the control group. There was a nonsignificant trend (P = .071) for a greater mean CBF within positive extreme clusters in patients with CKD relative to control subjects (Table E5 [online]). There was no difference in the incidence, total volume, or mean CBF values of negative extreme clusters between patients and control subjects. Qualitative inspection of common locations of subject-specific increases in CBF for patients with CKD showed high intersubject overlap of clusters in bilateral precuneus, posterior cingulate cortex, middle cingulate cortex, inferior parietal lobe, middle frontal lobe, caudate, and left putamen (Fig 2).
Correlation of CBF with Neurocognitive Performance
Patients with CKD performed worse than control subjects in traditional neurocognitive battery measures of verbal memory, working memory, and executive function. Patients with CKD scored worse in computerized neurocognitive battery measures of language reasoning, nonverbal reasoning, and spatial processing (P < .05, Wilcoxon rank sum test) (Table 4). In general, patients with CKD with positive extrema in CBF measurements showed poorer neurocognitive function than those without the presence of positive extrema (generalized estimating equations, B = 0.883, Exp(B) = 2.417, P = .003). Patients with CKD with positive extrema had significantly worse scores in traditional neurocognitive battery measures of verbal memory (P = .003, Wilcoxon rank sum test) (Table 4). CBF extracted from the positive extreme clusters in patients with CKD showed a strong correlation with executive function deficits (ρ = 0.670 and P = 4.76 × 10−4, controlling for age, sex, and hematocrit level (Table 5). Adjustments for the additional confounders listed in Table 1 did not change this association (ρ = 0.696 and P = 1.61 × 10−4, controlling for age, sex, hematocrit level, eGFR, cholesterol levels, triglycerides, and blood pressure). An exploratory correlation analysis was restricted to the precuneus because this region exhibited reliable differences for both the group-level and subject-specific methods. A significant correlation between executive function and CBF in the precuneus for patients with CKD was also observed (ρ = 0.608, P = .001) (Fig 3).
Table 4:
Neurocognitive Performance in Patients with CKD, Control Subjects, and Subgroups of CKD with Presence and Absence of Positive Extrema CBF
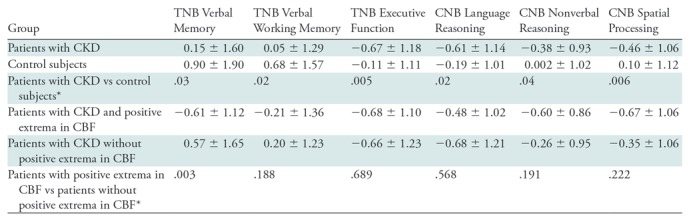
Note.—Except where indicated, data are mean age-normalized z scores ± standard deviations. In general, patients with CKD showed poorer neurocognitive functions than did control subjects. Patients with CKD with presence of positive extrema in CBF measurements showed poorer neurocognitive functions than did those without positive extrema. CBF = cerebral blood flow, CKD = chronic kidney disease, CNB = computerized neurocognitive battery, TNB = traditional neurocognitive battery.
*Data are P values and were determined with the Wilcoxon rank sum test.
Table 5:
Partial Correlation Analyses for CBF Extracted from Positive Extrema and Neurocognitive Performance in Subjects with Positive Extrema in CBF Measurements

Note.—Regions with abnormally increased or decreased cerebral blood flow (extreme voxels) in each individual participant were delineated with the distribution-corrected z score method. Analysis was controlled for age, sex, and hematocrit level. CBF = cerebral blood flow, CKD = chronic kidney disease, CNB = computerized neurocognitive battery, TNB = traditional neurocognitive battery.
*Statistically significant.
Figure 3:
Scatter plot shows partial residual values of precuneus cerebral blood flow (CBF) and executive function in patients with chronic kidney disease with presence of positive extrema CBF, indicating significant correlation between precuneus CBF and executive function after controlling for hematocrit (HCT), age, and sex (ρ = 0.608, P = .001). TNB = traditional neurocognitive battery.
Discussion
We characterized regional CBF alterations in pediatric and young adult patients with CKD by using ASL perfusion MRI. To minimize the potential confounding effect of hematocrit changes on CBF quantification, we used hematocrit-corrected blood T1 to derive CBF from ASL MRI data. We found markedly higher CBF in patients with CKD than in control subjects and confirmed known effects of age and hematocrit level on global CBF (25,26). Our results also confirmed an association between kidney function as manifested in eGFR and CBF in control subjects, whereas the association between these two physiologic parameters was disrupted in patients with CKD. Similarly, the effects of sex on global CBF were seen in control subjects, but not patients with CKD. Patients with CKD showed a subtle association between blood pressure and white matter CBF.
Hematocrit is a well-known modulator of CBF, and CKD is associated with anemia due to a decrease in erythropoietin production (27). Hematocrit-related effects on CBF explained most of the observed group differences in CBF. Chronic anemia could potentially cause endothelial damage because of increased flow as well as deficits in tissue oxygen delivery and is a potential therapeutic target. In adult patients with CKD, anemia has been associated with deterioration in cardiac function, decreased mental acuity, and increased mortality (28,29), whereas an improvement in GFR was demonstrated after correction of anemia with erythropoietin (28,30–32). The significant correlations between hematocrit level and CBF in our cohorts underscore the importance of accounting for hematocrit both in ASL MRI quantification and in the interpretation of CBF changes more generally. After application of the hematocrit-corrected blood T1 in CBF calculations, residual correlations between ASL CBF and hematocrit level likely reflect true hyperperfusion rather than purely artifactual hyperperfusion due to T1 underestimation. The absence of sex differences in CBF in patients with CKD might reflect delayed sexual differentiation that is known to occur in this condition (33) but may also be partly or even wholly attributable to the absence of sex difference in hematocrit level in this group.
We observed a correlation between eGFR and CBF in our control cohort, consistent with a previous report (34), implying that kidney function is associated with the regulation of blood flow in the brain. However, the association between eGFR and CBF was largely explained by differences in hematocrit level, further underscoring the importance of hematocrit level as a determinant of CBF and suggesting that this association is largely mediated through renal effects on hematopoiesis. The lack of association between eGFR and CBF in patients with CKD may have resulted from the heterogeneity of CKD in the group, which included patients with variable duration of CKD and some who had undergone kidney transplantation. In addition, our subjects were undergoing a variety of treatments for the comorbidities of CKD (ie, anemia, hypertension, and acidosis), which could have further obscured associations between eGFR and brain function. Another recently published study also showed that reduced eGFR was associated with a higher CBF in patients with CKD. However, hematocrit level was not assessed and corrected for in the ASL CBF measurements in that study (23).
Cerebrovascular disease is highly prevalent in adult patients with CKD, primarily in subcortical white matter (1,5). Our patients with CKD were found to have elevated blood pressure, dyslipidemia, and anemia. We observed a weak but significantly positive correlation between systolic blood pressure and white matter CBF in patients with CKD, suggesting the possibility of an alteration in cerebral microvascular autoregulation that may ultimately contribute to the development of white matter ischemic injury in CKD, although very minimal white matter ischemic injury was seen in the cohort. Cerebral autoregulation is thought to protect the brain from ischemia caused by acute arterial pressure fluctuations (35–37) and may become impaired during ischemia or other chronic insults such as hypertension (4,5,35). Early changes in white matter physiologic characteristics may also interfere with developmental trajectories of myelination and synaptic pruning thought to be responsible for decreasing CBF and metabolism that occurs in late childhood and adolescence during healthy human development (25,38,39).
The neuropsychological impairment in CKD has been reported to closely resemble a cerebral microangiopathy wherein chronic disturbances of regional CBF are known to occur (40). In addition to the global CBF differences between patients with CKD and control subjects, which were largely driven by group differences in hematocrit level, we also observed residual increases in CBF in the prefrontal cortex, posterior cingulate cortex, precuneus, basal ganglia, and parts of the limbic system. This observed distribution of regional CBF changes includes regions of the “default mode” network (41), which is consistent with a previous report of reduced default mode network functional connectivity in adult patients with CKD (42).
To better classify how spatially heterogeneous brain injury varies among patients with CKD, we used an individualized approach to characterize the spatial distribution of CBF changes in each patient with CKD (43). The subset of patients with CKD who showed positive extreme clusters of CBF demonstrated a larger incidence and total volume of positive extreme clusters along with higher CBF extracted from those clusters than did control subjects. Patients with CKD with positive extreme clusters showed significantly worse neurocognitive performance as compared with patients without positive extreme clusters. Altered brain perfusion in CKD was correlated with reduced executive function, which suggests that CBF differences between patients with CKD and control subjects reflect a neural correlate of observed neurocognitive deficits and highlights the potential usefulness of CBF as an objective and physiologic-based biomarker of brain dysfunction in this disorder.
We also identified a significant association between CBF changes in the precuneus and executive function. The precuneus represents the functional core of the default mode network and has been implicated in the integration of both internally and externally driven information (44). Structural changes in this brain region have been associated with executive dysfunction in patients with dementia (45). Note, however, that in this study significant regional differences between groups were observed only for regions that showed increased CBF in CKD versus control subjects. This may reflect either compensatory hyperactivity of these regions in the presence of normal coupling between regional CBF and regional neural activity or, potentially, a pathologic dysregulation of the normal coupling between regional CBF and regional neural activity in highly metabolic brain regions such as the precuneus. Our findings are consistent with those from a previous study in which ASL was used in adult patients with CKD (46) and which showed that abnormal CBF change in CKD was associated with poor performance in cognitive tests. However, those findings may not have fully accounted for effects of anemia on ASL CBF.
Our study had limitations. First, as described in the statistical analysis, in the absence of any previous report concerning CBF changes in pediatric CKD, this study was powered for structural MRI changes. The lack of associations after hematocrit correction in the correlation analyses may reflect a power issue with the limited statistical justification for sample size in ASL CBF measurements. Second, this study included a relatively heterogeneous population of patients with CKD, with a wide range of kidney function and posttransplant and dialysis patients (16,17). Third, although we controlled for the effect of age in our CBF group analysis, we could not exclude possible residual confounding effects of age in our results. Future work with much larger numbers of participants in each of these subgroups will be needed for additional analyses that account for those potentially confounding factors. Fourth, all results presented herein are cross-sectional. Ongoing longitudinal data will allow assessment of developmental changes in regional brain function in this population. Finally, ASL MRI data were acquired with a two-dimensional echo-planar imaging readout scheme without the background suppression, in which the instabilities in the background signal can potentially affect the accuracy and precision of the ASL measurements (47–49). Although the quality of the images we obtained with ASL was generally excellent, the use of three-dimensional readout sequences combined with background suppression would increase the sensitivity of future ASL MRI studies (47–53).
In conclusion, our results confirmed systemic effects of eGFR, hematocrit level, and blood pressure on CBF and alterations in regional CBF that may reflect impaired brain function underlying neurocognitive symptoms in CKD.
Summary
Our results confirmed that systemic effects of estimated glomerular filtration rate, hematocrit level, and blood pressure on cerebral blood flow and alterations in regional cerebral blood flow may reflect impaired brain function underlying neurocognitive symptoms in pediatric patients with chronic kidney disease.
Implications for Patient Care
■ Quantification and interpretation of perfusion imaging data acquired with arterial spin labeled MR imaging in patients with chronic kidney disease (CKD) and other populations with anemia must be carried out with careful attention to effects related to hematocrit.
■ Correlations between regional cerebral blood flow (CBF) and alterations in cognitive performance are suggestive of the potential value of CBF as an objective and physiologic-based biomarker of cognitive decline in pediatric CKD.
APPENDIX
SUPPLEMENTAL FIGURES
Acknowledgments
Acknowledgments
We thank the patients and families who participated in the study.
Study supported in part by a Commonwealth Universal Research Enhancement grant with the Pennsylvania Department of Health (SAP 4100054843). The Department of Health specifically disclaims responsibility for any analyses, interpretations, or conclusions. The Clinical and Translational Research Center at the Children’s Hospital of Philadelphia is supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health (grants UL1RR024134, UL1TR000003). Supported by the National Institutes of Health (grants EB015893, MH080729). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. H.S.L. supported by Taipei Medical University (grant TMU103-AE1-B29), Taipei Medical University Hospital (grants 105TMU-TMUH-05, 106TMU-TMUH-21), and the Ministry of Science and Technology in Taiwan (grants MOST105-2218-E-038-003-MY2, MOST106-2221-E-038-004-MY2).
Disclosures of Conflicts of Interest: H.S.L. disclosed no relevant relationships. E.A.H. disclosed no relevant relationships. A.F.J. disclosed no relevant relationships. J.B.W. disclosed no relevant relationships. N.L. disclosed no relevant relationships. A.M.P. disclosed no relevant relationships. R.C.G. Activities related to the present article: disclosed no relevant relationships. Activities not related to the present article: received money for expert testimony; receives royalties from the Brain Resource Centre. Other relationships: institution has a patent issued to Joggle Research; institution has a patent licensed to MindPrint Learning; receives royalties from Brain Resource Center. S.R.H. disclosed no relevant relationships. J.R. disclosed no relevant relationships. S.L.F. disclosed no relevant relationships. J.A.D. disclosed no relevant relationships.
Abbreviations:
- ASL
- arterial spin labeling
- CBF
- cerebral blood flow
- CKD
- chronic kidney disease
- eGFR
- estimated glomerular filtration rate
- NiCK
- Neurocognitive Assessment and Magnetic Resonance Imaging Analysis of Children and Young Adults with Chronic Kidney Disease
References
- 1.Moodalbail DG, Reiser KA, Detre JA, et al. Systematic review of structural and functional neuroimaging findings in children and adults with CKD. Clin J Am Soc Nephrol 2013;8(8):1429–1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hooper SR, Gerson AC, Butler RW, et al. Neurocognitive functioning of children and adolescents with mild-to-moderate chronic kidney disease. Clin J Am Soc Nephrol 2011;6(8):1824–1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seidel UK, Gronewold J, Volsek M, et al. The prevalence, severity, and association with HbA1c and fibrinogen of cognitive impairment in chronic kidney disease. Kidney Int 2014;85(3):693–702. [DOI] [PubMed] [Google Scholar]
- 4.Koren-Morag N, Goldbourt U, Tanne D. Renal dysfunction and risk of ischemic stroke or TIA in patients with cardiovascular disease. Neurology 2006;67(2):224–228. [DOI] [PubMed] [Google Scholar]
- 5.Yahalom G, Schwartz R, Schwammenthal Y, et al. Chronic kidney disease and clinical outcome in patients with acute stroke. Stroke 2009;40(4):1296–1303. [DOI] [PubMed] [Google Scholar]
- 6.Drew DA, Weiner DE. Cognitive impairment in chronic kidney disease: keep vascular disease in mind. Kidney Int 2014;85(3):505–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hartung EA, Matheson M, Lande MB, et al. Neurocognition in children with autosomal recessive polycystic kidney disease in the CKiD cohort study. Pediatr Nephrol 2014;29(10):1957–1965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reivich M. Blood flow metabolism couple in brain. Res Publ Assoc Res Nerv Ment Dis 1974;53:125–140. [PubMed] [Google Scholar]
- 9.Sokoloff L. Relationships among local functional activity, energy metabolism, and blood flow in the central nervous system. Fed Proc 1981;40(8):2311–2316. [PubMed] [Google Scholar]
- 10.Gur RC, Ragland JD, Reivich M, Greenberg JH, Alavi A, Gur RE. Regional differences in the coupling between resting cerebral blood flow and metabolism may indicate action preparedness as a default state. Cereb Cortex 2009;19(2):375–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hartung EA, Laney N, Kim JY, et al. Design and methods of the NiCK study: neurocognitive assessment and magnetic resonance imaging analysis of children and young adults with chronic kidney disease. BMC Nephrol 2015;16:66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gottesman RF, Sojkova J, Beason-Held LL, et al. Patterns of regional cerebral blood flow associated with low hemoglobin in the Baltimore Longitudinal Study of Aging. J Gerontol A Biol Sci Med Sci 2012;67(9):963–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gur RC, Richard J, Hughett P, et al. A cognitive neuroscience-based computerized battery for efficient measurement of individual differences: standardization and initial construct validation. J Neurosci Methods 2010;187(2):254–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gur RC, Richard J, Calkins ME, et al. Age group and sex differences in performance on a computerized neurocognitive battery in children age 8–21. Neuropsychology 2012;26(2):251–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ruebner RL, Laney N, Kim JY, et al. Neurocognitive dysfunction in children, adolescents, and young adults with CKD. Am J Kidney Dis 2016;67(4):567–575. [DOI] [PubMed] [Google Scholar]
- 17.Hartung EA, Kim JY, Laney N, et al. Evaluation of neurocognition in youth with CKD using a novel computerized neurocognitive battery. Clin J Am Soc Nephrol 2016;11(1):39–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu WC, Fernández-Seara M, Detre JA, Wehrli FW, Wang J. A theoretical and experimental investigation of the tagging efficiency of pseudocontinuous arterial spin labeling. Magn Reson Med 2007;58(5):1020–1027. [DOI] [PubMed] [Google Scholar]
- 19.Wang Z, Aguirre GK, Rao H, et al. Empirical optimization of ASL data analysis using an ASL data processing toolbox: ASLtbx. Magn Reson Imaging 2008;26(2):261–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lu H, Clingman C, Golay X, van Zijl PC. Determining the longitudinal relaxation time (T1) of blood at 3.0 Tesla. Magn Reson Med 2004;52(3):679–682. [DOI] [PubMed] [Google Scholar]
- 21.Gipson DS, Duquette PJ, Icard PF, Hooper SR. The central nervous system in childhood chronic kidney disease. Pediatr Nephrol 2007;22(10):1703–1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mayer AR, Bedrick EJ, Ling JM, Toulouse T, Dodd A. Methods for identifying subject-specific abnormalities in neuroimaging data. Hum Brain Mapp 2014;35(11):5457–5470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tamura MK, Pajewski NM, Bryan RN, et al. Chronic kidney disease, cerebral blood flow, and white matter volume in hypertensive adults. Neurology 2016;86(13):1208–1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pantoni L, Garcia JH. Pathogenesis of leukoaraiosis: a review. Stroke 1997;28(3):652–659. [DOI] [PubMed] [Google Scholar]
- 25.Biagi L, Abbruzzese A, Bianchi MC, Alsop DC, Del Guerra A, Tosetti M. Age dependence of cerebral perfusion assessed by magnetic resonance continuous arterial spin labeling. J Magn Reson Imaging 2007;25(4):696–702. [DOI] [PubMed] [Google Scholar]
- 26.Vorstrup S, Lass P, Waldemar G, et al. Increased cerebral blood flow in anemic patients on long-term hemodialytic treatment. J Cereb Blood Flow Metab 1992;12(5):745–749. [DOI] [PubMed] [Google Scholar]
- 27.Kuwabara Y, Sasaki M, Hirakata H, et al. Cerebral blood flow and vasodilatory capacity in anemia secondary to chronic renal failure. Kidney Int 2002;61(2):564–569. [DOI] [PubMed] [Google Scholar]
- 28.Cană-Ruiu D, Moţa E, Istrate N, Văduva C, Trican E. Renal anemia: risk factor for chronic kidney disease. Curr Health Sci J 2013;39(4):214–217. [PMC free article] [PubMed] [Google Scholar]
- 29.Fishbane S. Anemia and cardiovascular risk in the patient with kidney disease. Heart Fail Clin 2008;4(4):401–410. [DOI] [PubMed] [Google Scholar]
- 30.Silverberg D. Outcomes of anaemia management in renal insufficiency and cardiac disease. Nephrol Dial Transplant 2003;18(Suppl 2):ii7–ii12. [PubMed] [Google Scholar]
- 31.Al-Ahmad A, Rand WM, Manjunath G, et al. Reduced kidney function and anemia as risk factors for mortality in patients with left ventricular dysfunction. J Am Coll Cardiol 2001;38(4):955–962. [DOI] [PubMed] [Google Scholar]
- 32.Hsu CY, Bates DW, Kuperman GJ, Curhan GC. Relationship between hematocrit and renal function in men and women. Kidney Int 2001;59(2):725–731. [DOI] [PubMed] [Google Scholar]
- 33.Salas P, Pinto V, Rodriguez J, Zambrano MJ, Mericq V. Growth retardation in children with kidney disease. Int J Endocrinol 2013;2013:970946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sedaghat S, Vernooij MW, Loehrer E, et al. Kidney function and cerebral blood flow: the Rotterdam Study. J Am Soc Nephrol 2016;27(3):715–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Aries MJ, Elting JW, De Keyser J, Kremer BP, Vroomen PC. Cerebral autoregulation in stroke: a review of transcranial Doppler studies. Stroke 2010;41(11):2697–2704. [DOI] [PubMed] [Google Scholar]
- 36.Ruland S, Aiyagari V. Cerebral autoregulation and blood pressure lowering. Hypertension 2007;49(5):977–978. [DOI] [PubMed] [Google Scholar]
- 37.Ono M, Joshi B, Brady K, et al. Risks for impaired cerebral autoregulation during cardiopulmonary bypass and postoperative stroke. Br J Anaesth 2012;109(3):391–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Satterthwaite TD, Shinohara RT, Wolf DH, et al. Impact of puberty on the evolution of cerebral perfusion during adolescence. Proc Natl Acad Sci U S A 2014;111(23):8643–8648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Taki Y, Hashizume H, Sassa Y, et al. Correlation between gray matter density-adjusted brain perfusion and age using brain MR images of 202 healthy children. Hum Brain Mapp 2011;32(11):1973–1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hermann DM, Kribben A, Bruck H. Cognitive impairment in chronic kidney disease: clinical findings, risk factors and consequences for patient care. J Neural Transm (Vienna) 2014;121(6):627–632. [DOI] [PubMed] [Google Scholar]
- 41.Raichle ME, MacLeod AM, Snyder AZ, Powers WJ, Gusnard DA, Shulman GL. A default mode of brain function. Proc Natl Acad Sci U S A 2001;98(2):676–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ni L, Wen J, Zhang LJ, et al. Aberrant default-mode functional connectivity in patients with end-stage renal disease: a resting-state functional MR imaging study. Radiology 2014;271(2):543–552. [DOI] [PubMed] [Google Scholar]
- 43.Meier TB, Bergamino M, Bellgowan PS, et al. Longitudinal assessment of white matter abnormalities following sports-related concussion. Hum Brain Mapp 2016;37(2):833–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Utevsky AV, Smith DV, Huettel SA. Precuneus is a functional core of the default-mode network. J Neurosci 2014;34(3):932–940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vasconcelos LG, Jackowski AP, Oliveira MO, et al. The thickness of posterior cortical areas is related to executive dysfunction in Alzheimer’s disease. Clinics (São Paulo) 2014;69(1):28–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jiang XL, Wen JQ, Zhang LJ, et al. Cerebral blood flow changes in hemodialysis and peritoneal dialysis patients: an arterial-spin labeling MR imaging. Metab Brain Dis 2016;31(4):929–936. [DOI] [PubMed] [Google Scholar]
- 47.Ye FQ, Frank JA, Weinberger DR, McLaughlin AC. Noise reduction in 3D perfusion imaging by attenuating the static signal in arterial spin tagging (ASSIST). Magn Reson Med 2000;44(1):92–100. [DOI] [PubMed] [Google Scholar]
- 48.Duyn JH, Tan CX, van Gelderen P, Yongbi MN. High-sensitivity single-shot perfusion-weighted fMRI. Magn Reson Med 2001;46(1):88–94. [DOI] [PubMed] [Google Scholar]
- 49.Maleki N, Dai W, Alsop DC. Optimization of background suppression for arterial spin labeling perfusion imaging. MAGMA 2012;25(2):127–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Günther M, Oshio K, Feinberg DA. Single-shot 3D imaging techniques improve arterial spin labeling perfusion measurements. Magn Reson Med 2005;54(2):491–498. [DOI] [PubMed] [Google Scholar]
- 51.Nielsen JF, Hernandez-Garcia L. Functional perfusion imaging using pseudocontinuous arterial spin labeling with low-flip-angle segmented 3D spiral readouts. Magn Reson Med 2013;69(2):382–390. [DOI] [PubMed] [Google Scholar]
- 52.Vidorreta M, Wang Z, Rodríguez I, Pastor MA, Detre JA, Fernández-Seara MA. Comparison of 2D and 3D single-shot ASL perfusion fMRI sequences. Neuroimage 2013;66(C):662–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fernández-Seara MA, Wang Z, Wang J, et al. Continuous arterial spin labeling perfusion measurements using single shot 3D GRASE at 3 T. Magn Reson Med 2005;54(5):1241–1247. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.