Abstract
Keratosis pilaris (KP) and nevus comedonicus (NC) are congenital keratinized dermatoses; however, the exact etiology of these two diseases is unclear. The objective of the present study was to identify the disease-causing genes and their association with functional alterations in the development of KP and NC. Peripheral blood samples of one KP family, two NC families and 100 unrelated healthy controls were collected. The genomic sequences of 147 genes associated with 143 genetic skin diseases were initially analyzed from the KP proband using a custom-designed GeneChip. A novel heterozygous missense mutation in the ATP-binding cassette sub-family A member 12 (ABCA12) gene, designated c.6694G>T (p.Asp2232Tyr), was identified in the KP proband and confirmed by Sanger sequencing. The same mutation was also present in the affected family members but not in the healthy family members, the two patients with NC or population-matched controls. The predictions provided by PolyPhen-2 and SIFT analyses suggested that the mutation may produce a damaged protein. The region surrounding the mutation is the extra-membrane domain, which is conserved among particular species, as suggested by ClustalX; however, no ABCA12 mutations were reported in the patients with NC. As observed by immunofluorescence, ABCA12 expression was upregulated in the sebaceous glands of the patients with NC compared with that of normal controls. In summary, ABCA12-associated mutations or alterations in expression may exhibit causative or contributive effects to the development of keratinized dermatoses, including KP and NC.
Keywords: keratosis pilaris, nevus comedonicus, ATP-binding cassette sub-family A member 12, missense mutation
Introduction
Keratosis pilaris (KP; OMIM #604093), also known as lichen pilaris, is a benign genodermatosis that is estimated to effect ~40% of the population (1). KP is characterized by the presence of symmetric, asymptomatic and grouped keratotic follicular papules with varying degrees of perifollicular erythema. KP lesions often involve the proximal and extended parts of extremities, the cheeks and the buttocks (2). Cases may be generalized or unilateral (2). Most patients develop KP in their childhood, with a peak in incidence during adolescence (3). The incidence of KP subsequently decreases with age in 35% of those affected, but can persist in adulthood within 43%, and worsen in 22% of patients (4). KP can exist as an independent condition or in association with other diseases, such as xerosis, ichthyosis, atopic dermatitis and various conditions, including keratitis-ichthyosiss-deafness syndrome, Noonan syndrome and cardiofaciocutaneous syndrome (4–6). Genetic epidemiology surveys have indicated that KP is an autosomal dominant-inherited disease (4). A study reported a deletion of the short arm of chromosome 18 may be associated with KP (7). Brown et al (8), Mevorah et al (9) and Sandilands et al (10) identified mutations in the filaggrin (FLG) gene associated with atopic dermatitis and ichthyosis vulgaris in KP. Gruber et al (3) revealed that only 35% of patients with KP have mutations in FLG, suggesting that FLG mutations only partially result in the KP phenotype. Other genes may be the causative genetic factor contributing to the development of KP; however, further investigation is required.
Nevus comedonicus (NC) is a rare skin disorder caused by abnormal development of the pilosebaceous unit. The prevalence of NC has been estimated to occur in 1/45,000 to 1/100,000 individuals, with no gender or racial association (11). The pathogenesis of NC is yet to be investigated. Genetic studies have revealed that the fibroblast growth factor (FGF) and FGF receptor-2 signaling pathways, and somatic mutations of tyrosine kinase receptors or never in mitosis gene A-related kinase 9 (12) may be associated with the development of NC (13). The clinical features of NC include grouped, dilated hair follicles with a dark, firm hyperkeratotic plug at the center. NC can present with open or closed comedo, which primarily occur on the face, neck and upper trunk, and may be linear, interrupted, unilateral, bilateral or segmental (14). Clinically, there are two types of NC: Noninflammatory and inflammatory, with the formation of cysts, fistulas, and pustules (15).
In the present study, a novel heterozygous missense mutation was identified in ATP-binding cassette sub-family A member 12 (ABCA12) within a family afflicted with KP. In addition, upregulated ABCA12 expression levels in the sebaceous glands of patients with NC were investigated.
Materials and methods
High-throughput sequencing
Written informed consent was obtained from patients and individuals involved in the present study. The present study was approved by the ethics committee of Nanfang Hospital of Southern Medical University (Guangzhou, China). A total of 5 ml of peripheral blood was obtained from one KP and two NC probands, family members and 100 unrelated healthy controls (aged 18–28 years old, 44 males and 56 females, recruited in December 2015). The KP proband was a 12-year-old female (recruited August 2013). The NC probands were an 8-year-old male (recruited May 2014) and a 17-year-old male (recruited December 2015). Genomic DNA was extracted using the Blood DNA Mini kit (cat. no. 3001050; Hangzhou Simgen Biotechnology Co., Ltd., Hangzhou, China) according to the manufacturer's protocol. The genomic sequences of 147 genes associated with 143 skin diseases were initially analyzed in the KP proband using a custom-designed GeneChip [Skin single-gene genetic disease detection package, Illumina High-throughput sequencing platform (Illumina, Inc., San Diego, CA, USA), Beijing Genomics Institute, Guangdong, China] (P<0.05). The details of the gene and skin disease analysis were not presented.
Polymerase chain reaction (PCR) and Sanger sequencing
Specific primers for the ABCA12 gene were designed using the web-based tool Primer 3 (http://primer3.ut.ee/; ABCA12 primer sequences available on reasonable request). All exons and exon-intron boundaries of the ABCA12 gene were amplified using PCR with a 20 µl total reaction volume containing 1 µl genomic DNA with a final concentration of 30 ng/µl, 10 µl 2X Taq PCR StarMix (Taq DNA polymerase, Mg2+, dNTPs and reaction buffer solution; cat. no. A112-05, GenStar Biosolutions Co., Ltd.), 1 µl (10 µM) forward and reverse primers, and 7 µl ddH2O. The thermocycling conditions were as follows: Initial denaturation at 94°C for 5 min, 35 cycles of 94°C for 30 sec, annealing at 57°C for 30 sec and 72°C for 15 sec, followed by a final extension at 72°C for 15 sec. PCR products were confirmed using 1% agarose gel electrophoresis and sequenced. The sequencing results were analyzed on an ABI 3130 genetic analyzer (Applied Biosystems; Thermo Fisher Scientific, Inc., Waltham, MA, USA). The functional alterations in the protein were predicted by web-based tools PolyPhen-2 (genetics.bwh.harvard.edu/pph2/) and SIFT release 63 (sift.jcvi.org/). Sequence conservation surrounding the mutated region was verified using ClustalX version 2.1 (http://www.clustal.org/).
Immunofluorescence
Skin lesions from two patients with NC and the patient with KP were collected (one per patient; ~0.8×1 cm). The lesion from the KP proband was obtained from the left leg. NC samples were obtained from the waist and neck. Samples were fixed at room temperature by immersion in 10% formalin solution and, after 12 h the samples were processed into paraffin blocks. Sections (~3–4 µm) were obtained, and the prepared paraffin sections were placed on adhesive slides and incubated overnight at 37°C. Immunofluorescence staining was performed as described below. The slides were de-waxed in 100% dimethylbenzene twice and subsequently dehydrated via a descending alcohol (100, 95, 85 and 70%) gradient. The antigen was retrieved via incubation in a water bath (95°C) for 6 min and then cooled to room temperature. The samples were blocked with 3% peroxide-methanol for 20 min at room temperature to quench endogenous peroxidase activity and then rinsed in PBS three times. The following steps were conducted in a moisture chamber: i) Samples were incubated with rabbit anti-ABCA12 antibody (cat. no. bs-11906R; BIOSS, Beijing, China) diluted 1:50 in antibody diluent (cat. no. IH0340; Beijing Leagene Biotech Co., Ltd., Beijing, China) at 37°C for 1 h and then 4°C overnight. ii) Following rinsing with PBS three times, DyLight goat anti-rabbit green fluorescent protein (cat. no. 4412; CST Biological Reagents Co., Ltd., Shanghai, China) diluted 1:500 in antibody diluent was applied; the samples were then incubated at room temperature without light for 90 min. iii) Following three rinses with PBS, the slides were stained with DAPI at room temperature for 10 min. iv) After washing with PBS for 5 min, the slides were sealed with glycerin. v) The slides were allowed to dry naturally and then visualized under a fluorescence microscope at 360 and 488 nm (magnification, ×200). A total of 5 samples of normal skin were also analyzed which was obtained from a normal skin biopsy. Immunohistochemistry was conducted in the Central Laboratory of Nanfang Hospital of the Southern Medical University.
Results
Familial background
The familial association between the proband in a family with KP was presented in Fig. 1A; that of the two NC families were presented in Fig. 1B and C.
Figure 1.
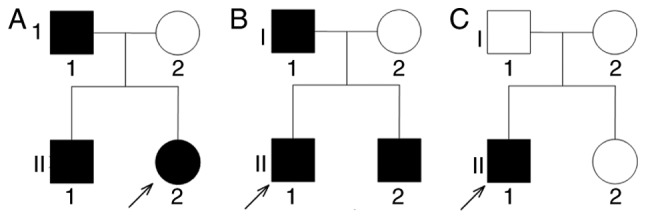
Family trees. (A) Family with keratosis pilaris. (B) First NC pedigree. (C) Second NC pedigree. NC, nevus comedonicus. The arrows indicate the proband.
Clinical and histopathological findings
KP family
A Chinese pedigree family with three members afflicted with KP across two generations (Fig. 1A) were employed in the present study. The proband, a 12-year-old female, presented symmetric, asymptomatic and rough keratotic follicular papules, and mild perifollicular erythema at the cheek. The extensor of the upper arms and anterior thighs (Fig. 2A-C) were analyzed. The patient had no notable medical or family history and no mental retardation. The father and younger brother of the proband presented similar phenotypes.
Figure 2.
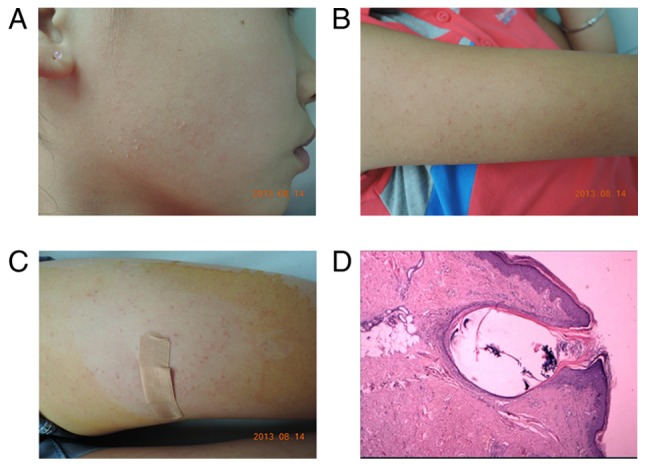
Clinical and pathological features of keratosis pilaris. (A-C) Clinical images of the proband: Symmetric, rough keratotic follicular papule and mild perifollicular erythema on the cheek, extensor of the upper arms and the anterior thighs. (D) Histopathology of a skin biopsy of the right thigh of the proband revealed that the follicular orifice was distended by a keratin plug; mild infiltration of mononuclear cells in the superficial dermis was observed (hematoxylin and eosin, magnification, ×200).
Histopathology of skin biopsies
Samples were fixed at room temperature by immersion in 10% formalin solution (at room temperature) and after 12 h the samples were processed into paraffin blocks. Sections (~3–4 µm) were obtained, and the prepared paraffin sections were placed on adhesive slides and incubated overnight at 37°C. The slides were de-waxed in 100% dimethylbenzene twice and subsequently dehydrated via a descending alcohol (100, 95, 85 and 70%) gradient. Then the slides were stained with hematoxylin (cat. no. DH0001; Beijing Leagene Biotech Co., Ltd., Beijing, China) for 8 min, then wash in pure water for 3 sec and finally stained with eosin (cat. no. DH0050; Beijing Leagene Biotech Co., Ltd.) for 1 min at room temperature. Finally the slides were visualized under a light microscope (magnification, ×200). The samples were obtained from the left thigh of the proband and revealed that the follicular orifice was distended by a keratin plug; mild infiltration of mononuclear cells in the superficial dermis was observed (Fig. 2D), supporting a diagnosis of KP.
NC patients
A total of two NC pedigrees were employed in the present study. The proband of the first family was an 8-year-old male with a 4-year medical history. The clinical manifestations of the proband constituted numerous keratotic papules and comedo-like lesions on the waist, buttocks and legs (data not shown). Physical examination revealed symmetric, light brown-colored papules 2–5 mm in size (Fig. 3A). The father and younger brother of the proband (Fig. 1B) exhibited the same symptoms. The second patient, a 17-year-old male, presented aggregated, dilated hair follicles, blackheads with cysts, fistulas and abscesses on the neck (Fig. 3B). Family disease history was not positive for the second NC family (Fig. 1C). The pathology of both patients demonstrated dilated follicular ostia filled with keratin layers (Fig. 3C and D).
Figure 3.
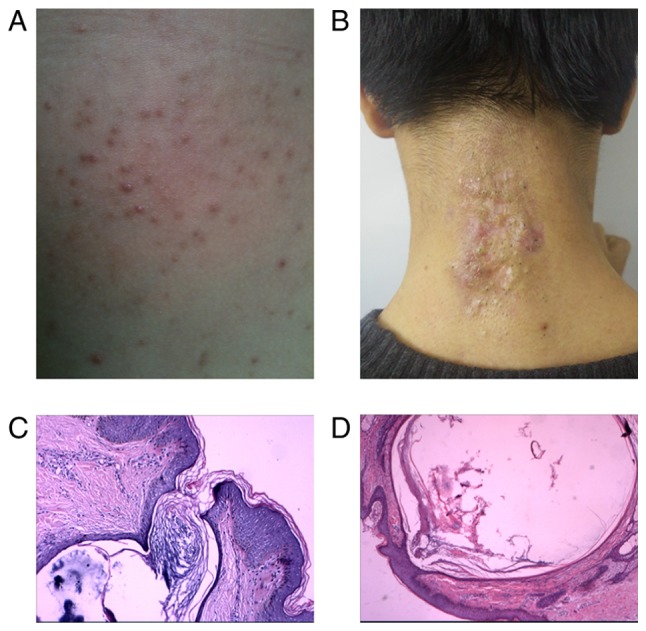
Clinical and pathological features of two patients with NC. (A) Clinical features of the first patient with NC: Numerous keratotic papules and comedo-like lesions on the waist and blackheads on parts of the lesions. (B) Clinical manifestation of the second patient: Aggregated, dilated hair follicles, blackheads with cysts, fistulas and abscesses on the neck. (C and D) Histopathology images of the two patients with NC; dilated follicular ostia filled with keratin layers were observed (hematoxylin and eosin, magnification, ×200). NC, nevus comedonicus.
Mutation screening for the ABCA12 genomic sequence
High-throughput sequencing revealed a heterozygous missense c.6694G>T (p.Asp2232Tyr) mutation in ABCA12 in the KP proband (Fig. 4A), and direct sequencing of all coding and exon-intron boundaries confirmed that this mutation was present in all of the affected KP family members, but not present in healthy family members, patients with NC or 100 population-matched controls (Fig. 4B). PolyPhen-2 and SIFT-based investigations suggested that this mutation may produce a damaged protein. The region surrounding this mutation is highly conserved among other species, according to ClustalX (Fig. 4C). The aforementioned results support the hypothesis that the p.Asp2232Tyr mutation in ABCA12 may be one of the pathological factors that contribute to KP.
Figure 4.
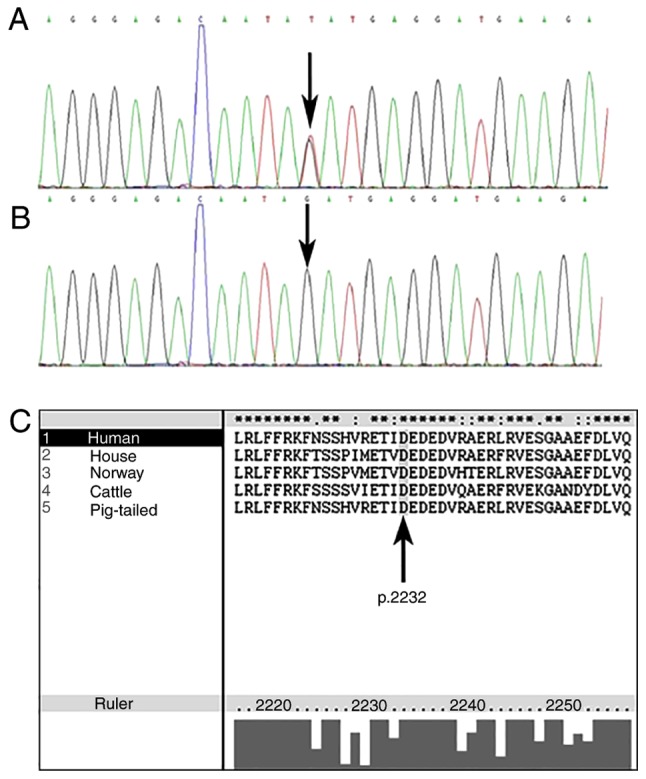
(A) Heterozygous missense c.6694G>T (p.Asp2232Tyr) mutation in ABCA12 in the proband of the keratosis pilaris family, the proband's father and younger brother. (B) No mutations of ABCA12 were detected in the mother of the proband or the control group. (C) Amino acid sequence of the region surrounding the mutation revealed highly conserved residues. The aspartic acid ‘D’ residue at position 2232 (arrow) presented high conservation among human, horse, Norway rat, cattle, and pig ABCA12 genes. ABCA12, ATP-binding cassette sub-family A member 12.
ABCA12 is highly expressed in the sebaceous gland
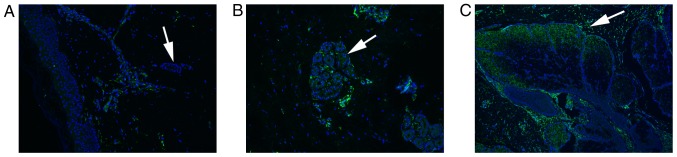
To understand whether ABCA12, which regulates lipid transport, is involved in the development of NC, the expression levels of ABCA12 were examined using immunofluorescence. The results demonstrated that ABCA12 expression was upregulated in the sebaceous glands of patients with NC (Fig. 5B and C) compared with in normal controls (Fig. 5A). Therefore, high expression levels of ABCA12 in the sebaceous gland may be associated with the development of NC.
Figure 5.
Immunofluorescence staining. (A) Healthy individual without NC. (B and C) The results from the two patients with NC. ATP-binding cassette sub-family A member 12 expression was observed to be stronger in the sebaceous glands of patients with NC compared with that of normal skin (white arrow). Magnification, ×200. NC, nevus comedonicus.
Discussion
The putative pathogenesis of KP suggests a disorder of keratinization. The papules may arise from the excessive accumulation of keratin within the follicular orifices (6). Perifollicular erythema results from mechanical irritation from hyperkeratosis and increased skin pH, caused by a reduction in moisturizing amino acids (16). Several genetic studies have reported null mutations in the FLG gene of patients with KP, which has been associated with ichthyosis vulgaris and atopic dermatitis (17). FLG, a multifunctional protein expressed in the epidermis, not only aggregates and aligns keratin intermediate filaments within corneocytes, but also facilitates the release of a variety of amino acids, which contribute to natural moisture levels or reduced skin surface pH. Loss of function of FLG may lead to reduced natural moisture, resulting in epithelial barrier abnormalities (3); however, Gruber et al (3) reported that mutations of FLG may only partially result in the KP phenotype. Therefore, other genes may serve as causative genetic factors contributing to the development of KP; however, further research is required.
In the present study, a heterozygous missense c.6694G>T (p.Asp2232Tyr) mutation within ABCA12 of the KP proband was identified. At present, no mutations in ABCA12 have been reported to be associated with the onset of KP. Mutations of ABCA12 have been considered to be a major cause of harlequin ichthyosis (18,19). ABCA12, located on chromosome 2q35, encodes a protein constituting 2595 amino acids, including two ATP nucleotide binding sites between residues 1370–1554 and 2282–2467, and two transmembrane domains (amino acid residues 1063–1271 and 1987–2293), each comprising six hydrophobic membrane spanning helices (20,21). ABCA12 belongs to the ATP-binding cassette (ABC) transmembrane transporter protein superfamily, which bind and hydrolyze ATP for the transport of lipids in lamellar granules to granular layer keratinocytes (22). The main molecular function of ABCA12 is yet to be investigated. Akiyama (19) demonstrated that a lack of ABCA12 function disrupted glucosylceramide and ganglioside transport, leading to intracellular accumulation of these substances; this phenomenon was recovered by in vitro via ABCA12-corrective gene transfer (19). Investigations conducted by Wang et al (23) and Sun et al (24) indicated that increases in the production of gangliosides may result in keratinocyte apoptosis rather than the formation of epidermal stratification. Jiang et al (25) reported that ceramides, the precursors of glucosylceramides, stimulate ABCA12 expression via the PPAR-mediated signaling pathway, subsequently regulating this lipid transporter. Conversely, Zuo et al (26) reported a lack of desquamation of the skin cells and rapid water loss from the skin in ABCA12−/− mice rather than enhanced proliferation of basal layer keratinocytes. Therefore, the mutations of ABCA12 may affect lipid transport and skin cell desquamation, which may lead to the development of solid and dry lesions associated with KP.
NC is an epidermal nevus involving the pilosebaceous unit (27); the etiology of NC requires further investigation. Recently, the underlying signaling pathways associated with acne and the somatic mutations of tyrosine kinase receptors have been identified, and may serve a role in the development of NC (11,13). The present study revealed that the typical histopathology of NC was associated with large dilated follicular ostia filled with keratinous layers, similar to that of KP. Therefore, the present study aimed to investigate whether patients with NC also possessed mutations in ABCA12, which may affect lipid transport, resulting in the accumulation of keratin. Following sequencing, no ABCA12 mutations were identified in the two NC pedigrees employed in the present study; however, immunofluorescence analysis revealed that the ABCA12 protein was highly expressed in the sebaceous glands of patients with NC compared with in normal skin. Under normal conditions, ABCA12 protein is expressed and localized in epidermal keratinocytes (28). Conversely, ABCA12 expression was identified within the sebaceous glands of the two patients NC in the present study. The findings of the present study were supported by the presence of abnormal sebaceous glands. In conclusion, a novel missense mutation c.6694G>T in ABCA12 was identified in a KP family, and it was demonstrated that ABCA12 expression was upregulated in the sebaceous glands of NC patients without ABCA12 mutation. Therefore, it was inferred that ABCA12 mutations or expression changes may be causative or contributive factors to disease development of congenital keratinized dermatoses, such as KP and NC. ABCA12 may be considered as a therapeutic target for the treatment of NC. There remained limitations to the present study; for example, further investigations are needed to clarify the genetic background of the previous generations of the probands.
Acknowledgements
Not applicable.
Funding
The present study was supported by grants from National Natural Science Foundation of China (grant no. 81371724) to YHL.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
FL and YY performed the experiments and wrote this article. YZ collected blood and skin samples. YHL and KZ designed the experiments. All authors read and approved the final manuscript.
Ethics approval and consent to participate
The present study was approved by the ethics committee of Nanfang Hospital of Southern Medical University (Guangzhou, China).
Patient consent for publication
Written informed consent was obtained from patients and individuals involved in the present study.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Kootiratrakarn T, Kampirapap K, Chunhasewee C. Epidermal permeability barrier in the treatment of keratosis pilaris. Dermatol Res Pract. 2015;2015:205012. doi: 10.1155/2015/205012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ehsani A, Namazi MR, Barikbin B, Nazemi MJ. Unilaterally generalized keratosis pilaris. J Eur Acad Dermatol Venereol. 2003;17:361–362. doi: 10.1046/j.1468-3083.2003.00792_10.x. [DOI] [PubMed] [Google Scholar]
- 3.Gruber R, Sugarman JL, Crumrine D, Hupe M, Mauro TM, Mauldin EA, Thyssen JP, Brandner JM, Hennies H, Schmuth M, Elias PM. Sebaceous gland, hair shaft, and epidermal barrier abnormalities in keratosis pilaris with and without filaggrin deficiency. Am J Pathol. 2015;185:1012–1021. doi: 10.1016/j.ajpath.2014.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Poskitt L, Wilkinson JD. Natural history of keratosis pilaris. Br J Dermatol. 1994;130:711–713. doi: 10.1111/j.1365-2133.1994.tb03406.x. [DOI] [PubMed] [Google Scholar]
- 5.Park KY, Son IP, Choi SY, Seo SJ, Hong CK. Combination peel with incorporated fractional prickle coral calcium for the treatment of keratosis pilaris: A pilot study. J Dermatolog Treat. 2014;25:314–318. doi: 10.3109/09546634.2012.671914. [DOI] [PubMed] [Google Scholar]
- 6.Thai K, Sinclair RD. Keratosis pilaris and hereditary koilonychia without monilethrix. J Am Acad Dermatol. 2001;45:627–629. doi: 10.1067/mjd.2001.116225. [DOI] [PubMed] [Google Scholar]
- 7.Nazarenko SA, Ostroverkhova NV, Vasiljeva EO, Nazarenko LP, Puzyrev VP, Malet P, Nemtseva TA. Keratosis pilaris and ulerythema ophryogenes associated with an 18p deletion caused by a Y/18 translocation. Am J Med Genet. 1999;85:179–182. doi: 10.1002/(SICI)1096-8628(19990716)85:2<179::AID-AJMG14>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 8.Brown SJ, Relton CL, Liao H, Zhao Y, Sandilands A, McLean WH, Cordell HJ, Reynolds NJ. Filaggrin haploinsufficiency is highly penetrant and is associated with increased severity of eczema: Further delineation of the skin phenotype in a prospective epidemiological study of 792 school children. Br J Dermatol. 2009;161:884–889. doi: 10.1111/j.1365-2133.2009.09339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mevorah B, Marazzi A, Frenk E. The prevalence of accentuated palmoplantar markings and keratosis pilaris in atopic dermatitis, autosomal dominant ichthyosis and control dermatological patients. Br J Dermatol. 1985;112:679–685. doi: 10.1111/j.1365-2133.1985.tb02336.x. [DOI] [PubMed] [Google Scholar]
- 10.Sandilands A, O'Regan GM, Liao H, Zhao Y, Terron-Kwiatkowski A, Watson RM, Cassidy AJ, Goudie DR, Smith FJ, McLean WH, Irvine AD. Prevalent and rare mutations in the gene encoding filaggrin cause ichthyosis vulgaris and predispose individuals to atopic dermatitis. J Invest Dermatol. 2006;126:1770–1775. doi: 10.1038/sj.jid.5700459. [DOI] [PubMed] [Google Scholar]
- 11.Tchernev G, Ananiev J, Semkova K, Dourmishev LA, Schonlebe J, Wollina U. Nevus comedonicus: An updated review. Dermatol Ther (Heidelb) 2013;3:33–40. doi: 10.1007/s13555-013-0027-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Levinsohn JL, Sugarman JL, McNiff JM, Antaya RJ, Choate KA. Somatic mutations in NEK9 cause nevus comedonicus. Am J Hum Genet. 2016;98:1030–1037. doi: 10.1016/j.ajhg.2016.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mahajan RS, Shah MM, Ninama KR, Bilimoria FE. Extensive nevus comedonicus. Indian Dermatol Online J. 2014;5:520–521. doi: 10.4103/2229-5178.142535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ito T, Mitamura Y, Tsuji Y, Harada K, Urabe K. Bilateral nevus comedonicus syndrome. Yonago Acta Med. 2013;56:59–61. [PMC free article] [PubMed] [Google Scholar]
- 15.Beck MH, Dave VK. Extensive nevus comedonicus. Arch Dermatol. 1980;116:1048–1050. doi: 10.1001/archderm.116.9.1048. [DOI] [PubMed] [Google Scholar]
- 16.Lee D, Yamasaki K, Rudsil J, Zouboulis CC, Park GT, Yang J, Gallo RL. Sebocytes express functional cathelicidin antimicrobial peptides and can act to kill propionibacterium acnes. J Invest Dermatol. 2008;128:1863–1866. doi: 10.1038/sj.jid.5701235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brown SJ, Relton CL, Liao H, Zhao Y, Sandilands A, Wilson IJ, Burn J, Reynolds NJ, McLean WH, Cordell HJ. Filaggrin null mutations and childhood atopic eczema: A population-based case-control study. J Allergy Clin Immunol. 2008;121:940–946. doi: 10.1016/j.jaci.2008.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thomas AC, Cullup T, Norgett EE, Hill T, Barton S, Dale BA, Sprecher E, Sheridan E, Taylor AE, Wilroy RS, et al. ABCA12 is the major harlequin ichthyosis gene. J Invest Dermatol. 2006;126:2408–2413. doi: 10.1038/sj.jid.5700455. [DOI] [PubMed] [Google Scholar]
- 19.Akiyama M. ABCA12 mutations and autosomal recessive congenital ichthyosis: A review of genotype/phenotype correlations and of pathogenetic concepts. Hum Mutat. 2010;31:1090–1096. doi: 10.1002/humu.21326. [DOI] [PubMed] [Google Scholar]
- 20.Annilo T, Shulenin S, Chen ZQ, Arnould I, Prades C, Lemoine C, Maintoux-Larois C, Devaud C, Dean M, Denefle P, Rosier M. Identification and characterization of a novel ABCA subfamily member, ABCA12, located in the lamellar ichthyosis region on 2q34. Cytogenet Genome Res. 2002;98:169–176. doi: 10.1159/000069811. [DOI] [PubMed] [Google Scholar]
- 21.Lefevre C, Audebert S, Jobard F, Bouadjar B, Lakhdar H, Boughdene-Stambouli O, Blanchet-Bardon C, Heilig R, Foglio M, Weissenbach J, et al. Mutations in the transporter ABCA12 are associated with lamellar ichthyosis type 2. Hum Mol Genet. 2003;12:2369–2378. doi: 10.1093/hmg/ddg235. [DOI] [PubMed] [Google Scholar]
- 22.Akiyama M, Sugiyama-Nakagiri Y, Sakai K, McMillan JR, Goto M, Arita K, Tsuji-Abe Y, Tabata N, Matsuoka K, Sasaki R, et al. Mutations in lipid transporter ABCA12 in harlequin ichthyosis and functional recovery by corrective gene transfer. J Clin Invest. 2005;115:1777–1784. doi: 10.1172/JCI24834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang XQ, Sun P, Paller AS. Inhibition of integrin-linked kinase/protein kinase B/Akt signaling: mechanism for ganglioside-induced apoptosis. J Biol Chem. 2001;276:44504–44511. doi: 10.1074/jbc.M106563200. [DOI] [PubMed] [Google Scholar]
- 24.Sun P, Wang XQ, Lopatka K, Bangash S, Paller AS. Ganglioside loss promotes survival primarily by activating integrin-linked kinase/Akt without phosphoinositide 3-OH kinase signaling. J Invest Dermatol. 2002;119:107–117. doi: 10.1046/j.1523-1747.2002.01802.x. [DOI] [PubMed] [Google Scholar]
- 25.Jiang YJ, Uchida Y, Lu B, Kim P, Mao C, Akiyama M, Elias PM, Holleran WM, Grunfeld C, Feingold KR. Ceramide stimulates ABCA12 expression via peroxisome proliferator-activated receptor in human keratinocytes. J Biol Chem. 2009;284:18942–18952. doi: 10.1074/jbc.M109.006973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zuo Y, Zhuang DZ, Han R, Isaac G, Tobin JJ, McKee M, Welti R, Brissette JL, Fitzgerald ML, Freeman MW. ABCA12 maintains the epidermal lipid permeability barrier by facilitating formation of ceramide linoleic esters. J Biol Chem. 2008;283:36624–36635. doi: 10.1074/jbc.M807377200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kurokawa I, Nakai Y, Nishimura K, Hakamada A, Isoda K, Yamanaka K, Mizutani H, Tsubura A. Cytokeratin and filaggrin expression in nevus comedonicus. J Cutan Pathol. 2007;34:338–341. doi: 10.1111/j.1600-0560.2006.00619.x. [DOI] [PubMed] [Google Scholar]
- 28.Yamanaka Y, Akiyama M, Sugiyama-Nakagiri Y, Sakai K, Goto M, McMillan JR, Ota M, Sawamura D, Shimizu H. Expression of the keratinocyte lipid transporter ABCA12 in developing and reconstituted human epidermis. Am J Pathol. 2007;171:43–52. doi: 10.2353/ajpath.2007.061207. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.