Abstract
Introduction:
Female Sexual dysfunction is an important health concern caused by several factors. This study aimed to compare the sexual function of women who have primary headaches in order to investigate the relationship between sexual dysfunction and the features of headaches.
Materials and Methods:
95 consecutive patients aged 18 to 65 years with a history of headache for at least 1 month and sexually active in the last 6 months presenting to Psychiatry OPD of a tertiary care hospital in New Delhi giving informed consent were taken. The diagnosis of headache type was confirmed according to the 2nd edition of International Headache Society (IHS) International Classification of Headache Disorders (ICHD-II) in 2004. The Female Sexual Function Index (FSFI), visual analog scale (VAS) score and Migraine disability assessment scale score (MIDAS) were applied.
Results:
Those with migraines reported a greater intensity of pain than those with tension headaches. Individuals with tension headaches reported more frequent headaches. The mean MIDAS score in the migraine group was 14.64 (±2.59); 30% of the migraine group fell into the most severe category in MIDAS. Women with headaches had lower scores (indicating impaired sexual functioning) on all FSFI subscales, as well as on the total score when the prescribed cutoffs were applied as compared to controls (66.3% vs. 30% in controls).
Conclusion:
The present study showed that patients with either type of primary headache experience problems in several aspects of sexuality compared with controls.
Keywords: Female sexual dysfunction, headache, India
INTRODUCTION
Given that chronic illnesses are related to sexual dysfunction, especially pain and disease severity in rheumatoid arthritis, fibromyalgia, etc., headache as a chronic condition is mainly seen in women is known to negatively affect the quality of life as well as sexual function. Alteration of sexual desire, genital arousal, and orgasm along with pain threshold changes are known to occur in migraineurs. Previous studies have suggested that sexual dysfunction in migraine and tension-type headache may not be the direct result of migraine-related disability but probably be moderated by other factors. There is no published data examining the relationship between migraine frequency/severity and sexual functioning in Indian women.
The global prevalence of the adult members of the population with an active headache disorder is 46% for headache in general, 11% for migraine, 42% for tension-type headache, and 3% for chronic daily headache.[1] In a nationwide epidemiological study in India, the lifetime prevalence of migraine was found to be 10.9% in men and 21.8% in women.[2] Migraine is a chronic disorder affecting several women worldwide and is associated with different psychological problems such as depression, poor sleep, and sexual dysfunction. The burden of primary headaches and its impact on the quality of life and psychosocial functioning is very high. Head pain affects several aspects of a person's life (family relations, work, love, and sex life), especially when the condition is chronic.[1,3] Sexual complaints in individuals with migraine need to be addressed in order to improve their overall quality of life. Recent studies showed that all aspects of sexual health in women with migraine are affected. Alteration of sexual desire, genital arousal, and orgasm along with pain threshold changes are possible reasons for sexual dysfunction in migraineurs.[4] Data from a prospective follow-up mail survey in a Finnish adult population highlights that the association between migraine and sex life issues was different for men and women, the women being found to lose interest in their sex life and the men the opposite.
A study conducted by Nappi et al. in 2012 reported that more than 90% of the women with primary headaches had sexual dysfunction.[5,6] Despite the large proportion of the female population affected by recurrent acute or chronic pain and the significant impact this has on their quality of life; data on sexual function in women with primary headaches are limited[7,8,9] Sexual dysfunction in women with primary is a neglected individual in India. This study examined the prevalence and severity of sexual dysfunction in women with primary headache identified in an outpatient clinic. An attempt was also made to identify sociodemographic and clinical determinants.
MATERIALS AND METHODS
Aim
The aim of this study is to compare the incidence of sexual dysfunction between patients with tension-type headaches (T), migraines (M), and healthy controls (C) to study the relationship between sexual dysfunction and the features of primary headaches.
This cross-sectional, pilot study was carried out on women with headache attending the psychiatry outpatient department (OPD) of HAHC Hospital, New Delhi, India. The study was conducted between June 2015 and December 2015. The study was approved by the Institutional Ethics Committee. A total of 110 individuals met the inclusion criteria; however, 15 refused to complete the evaluation form; hence, the study sample was comprised of 95 women with headache (50 migraine cases and 45 tension-type headache cases) and 30 age-and sex-matched healthy controls. The size of the sample was arbitrarily decided with a view to obtain as much of representativeness and precision of information as possible within the scope of a pilot study. All cases met the International Headache Society criteria for headache diagnosis.[10] A total of 95 consecutive patients with a history of headache for at least 1 month and sexually active in the last 6 months presenting to psychiatry OPD were taken up for the study sample.
Controls were sourced from among the relatives of patients attending the other OPDs; that is, from the same socioeconomic and cultural population as the cases. The control subjects did not meet the criteria for either migraine or nonmigraine headache. Written informed consent was obtained from all participants. Patients were eligible for the selection if they were aged 18–45 years, were in a stable heterosexual relationship, and willingly gave written informed consent. Exclusion criteria were diabetes, hypertension, thyroid disorders, history of substance abuse, pregnancy, and other acute and chronic medical conditions that could influence sexual functioning. Those using antidepressants/any other psychotropic medication with known sexual function effect and the presence of mental retardation were also excluded from the study. Clinical diagnosis of depression was done according to International Statistical Classification of Diseases and Related Health Problems, 10th revision criteria by the consulting psychiatrist.
Survey instruments
Sociodemographic questionnaire – all participants were asked to fill in semi-structured forms that had been prepared by the investigators. These forms included questions on age, marital status, education level, occupation, age of sex partner, and so on.
Visual Analog Scale – A 100-mm visual analog scale was used for participants to rate their level of headache pain over the preceding 30 days.[11]
Sexual functioning was assessed using the Female Sexual Function Index (FSFI), which is a 19-item, a self-rate instrument that assesses six key domains of sexual functioning in women. Each item is scored on a scale of 0 (or 1) to 5; a total score is also obtained, and higher scores indicate better sexual functioning. The FSFI domains are desire, arousal, lubrication, orgasm, satisfaction, and pain. Participants completed the FSFI alone, in a private room. Women who were not sufficiently literate to complete the FSFI on their own were assisted by multilingual female health professional. An FSFI score <26.55 is classified as female sexual dysfunction; cutoffs for individual domains are also described.[12,13]
Migraine Disability Assessment (MIDAS) scale is a tool assessing headache-related disability. Headache sufferers are asked to answer five questions scoring the number of days in the past 3 months and activity limitations due to migraine.[16]
Statistical methods
The descriptive statistics were computed for each of the variables in all three groups studied. Correlation coefficients were computed between age, years of education, income, duration, and frequency of headache per week, etc., on the one hand and FSFI subscale and total scale scores on the other hand. The Spearman correlation coefficient was calculated to find the direction of correlation. The linear regression analysis was carried out to find the strength of association between FSFI score and visual analog scale (VAS) and MIDAS. P < 0.05 was considered statistically significant. All the analysis was carried out on SPSS 16.0 version (SPSS for Windows, Chicago, SPSS Inc., USA).
RESULTS
Characteristics of the study sample
The mean ages for the three groups were 35.32 years in group migraine (M) (standard deviation [SD].: 7.51); 34.53 years in group tension type (T) (SD: 6.80); 34.90 years in group controls (C) (SD: 6.80), with no clinically or statistically significant difference noted. P > 0.05. The average number of years of education were 5.7 years (SD: 2.71), 5.3 years (SD: 2.76) and 6.4 years (SD: 2.67) in the three groups, respectively. In all, 92.8% of the participants (n = 116) were married, and the remainder had steady sex partners. All of the participants had a single partner at the time of the study. Majority of the patients in all the 3 groups were from urban area. In addition, only (n = 4) of the patients in all the groups had attained menopause. About 28% of migraine, 24.4% of tension type, and 33.3% of Controls were overweight. There was no significant (P > 0.05) difference in terms of place of residence, body mass index among the groups.
Comparisons of headache characteristics across the two headache groups
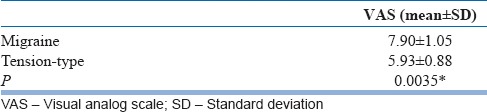
Those with migraines reported a greater intensity of pain than those with tension headaches on VAS participants with tension headaches reported more frequent headaches per month on an average than their migraine counterparts. The mean duration of illness in migraine and tension type group was 2.98 (±1.59) and 3.20 (±1.60) years, respectively. There was no significant (P > 0.05) difference in the duration among the groups. The mean MIDAS score in the migraine group was 14.64 (±2.59). Our findings revealed that 30% of the migraine group fell into the most severe category in MIDAS. These participants were also most significantly affected with respect to sexual functioning. The frequency of sexual intercourse was significantly less in those with headaches versus controls (P = 0.001). Comparisons of headache characteristics across the two headache groups are summarized in Tables 1a and b.
Table 1a.
Distribution of cases according to frequency of headache
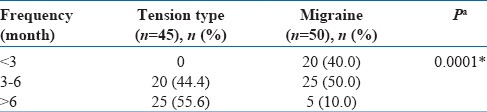
Table 1b.
Distribution of cases according to severity of headache
Women with headaches had lower scores (indicating impaired sexual functioning) on all FSFI subscales, as well as on the total score when the prescribed cut-offs were applied as compared to controls. The mean (SD) FSFI score of participants with headache was 20.01 (M) and 22.53 (T) out of a maximum of 36. Based on total FSFI score, women had scores less than the validated cutoff point of 26.55, which is accepted as sexual dysfunction.
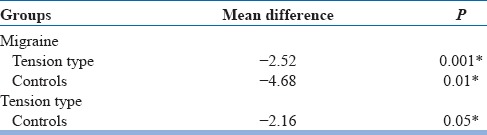
The mean (SD) domain scores were as follows: desire 3.4 (1.0), arousal 4.0 (1.3), orgasm 4.2 (1.4), satisfaction 4.5 (1.5), and pain 4.9 (1.6) out of a maximum domain score of six for each. Nearly, 66.3% of these women were rated as dysfunctional vis a vis 30% in controls. Our results suggest that people suffering from headaches experience dysfunction in all domains of sexuality relative to those who are healthy as shown by mean FSFI value in Tables 2 and 3 which shows significance. However, some differences exist between those with migraines and those with tension headaches. Results suggest that women with migraine have higher levels of sexual dysfunction than those suffering from tension-type headaches.
Table 2.
Comparison of total score of Female Sexual Function Index among the groups Kruskal-Wallis test
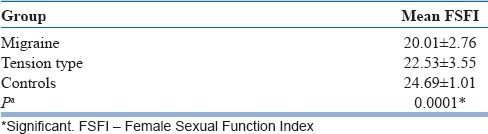
Table 3.
Post hoc tests comparing total scores between the groups
There was also a negative association of FSFI total scores seen with MIDAS scores, migraine duration, attack frequency, and severity as per VAS which indicates that these factors may influence the sexual functioning of participants with migraine type headache. Among the headache population, N = 47 had clinical depression. Depression also showed an independent positive correlation with sexual dysfunction in the affected population (r = 0.63, P = 0.001).[14]
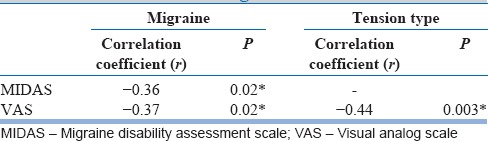
Table 4 shows the correlation of FSFI score with MIDAS and VAS in migraine and tension-type groups. A significant moderately negative correlation (r = −0.36, P = 0.02) was observed between MIDAS and FSFI score in migraine group. Similarly, VAS was also found to be moderately negatively correlated with FSFI in Migraine (r = −0.37, P = 0.02) and tension type (r = −0.44, P = 0.003) groups.
Table 4.
Correlation of Female Sexual Function Index with migraine disability assessment scale and visual analog scale
DISCUSSION
Research on sexuality in people suffering from headaches is very limited in the Indian scenario.[15] In this study, sexual dysfunction in female patients suffering either from migraine or tension-type headaches was compared with that reported by matched healthy controls. The prevalence of sexual dysfunction in women with headache varies widely in literature depending on the nature of the sample studied, the definition of sexual dysfunction, and other variables studied. A recent Indian study comparing the prevalence of FSD in women with or without depression reported 70%vs 46% in the normal population.[16,17]
Female sexual dysfunctions can be manifestations of biological (biogenic) problems or intrapsychic or interpersonal (psychogenic) conflicts or even a combination of these factors. Stress plays an important role in pathogenesis of FSDs. In general, chronic pain exerts adverse effects on sexual desire, stimulation, and activity.[19] Indeed, women with a long history of primary headaches are affected by a chronic condition capable of influencing their pain threshold and nociceptive pathways at different levels, and of inducing the impairment of genital arousal and orgasmic function.[18,19]
In our study also, patients with migraines reported more headache pain during intercourse than controls which is consistent with the findings of Ifergane et al.[20,21,22] The frequency of sexual intercourse was significantly less in those with headaches as compared to controls (P < 0.001). Our findings suggest that female migraine sufferers experience a considerable decline in their sex drive and have difficulties with sexual stimulation, vaginal lubrication, and achieving orgasm. They also appear to be less satisfied with sex.
The frequency, severity, and duration of headaches also impacts the individual's sexual life. In previous studies, the relationship between sexuality and these aforementioned characteristics have not been examined sufficiently.[23,24]
Although it was observed that migraine and tension-type headache patients differ somewhat in their difficulties within certain domains of sexuality, this does not seem to be related to headache characteristics, which suggests that other variables may have had a role.
In addition, psychiatric comorbidities such as mood disorders[25] are very frequent in primary headaches and may significantly affect the neuroendocrine balance involved in the mechanisms controlling sexual drive, mental arousal, and general satisfaction. Depression is one of the most common mood disorders in patients with both migraine as well as tension type headache.[26] Nearly 30%–40% cases with migraine suffer from depression. In addition, primary headaches can be comorbid with other medical conditions, such as mood and anxiety disorders with which they probably share a common neurobiological substrate.[27] There is no exact reason for depression in patients with migraine, but serotoninergic and dopaminergic dysfunction, ovarian hormone fluctuation, central sensitization to pain, and excessive use of over-the-counter medications are among probable causes. However, Maizels and Burchette have reported that the prevalence of sexual dysfunction does not differ in the presence of depression or anxiety[24] which was contrary to our findings. Consistent with Jelinkski's study, we found that migraine related disability was also significantly correlated with the level of depressive symptoms as well as sexual dysfunction. Even though migraine and tension type headache are underlain by different etiopathogenetic mechanisms our data suggest that these two categories share a significant impairment of sexual function, especially in the pain domain.[17,18] Our finding supports the necessity of treatment for psychiatric disorders in migraine patients since it significantly reduce the quality of life and lead to a worse prognosis, chronicity, and a reduced response to treatment. It has been indicated that migraine comorbid with depression causes higher medical costs than does migraine alone.[18,23]
Although the aim of our study was not to reveal the causes of sexual difficulties per se; depression was found to be an independent predictor. Finally, several intrapersonal and interpersonal factors related to the headache condition[28] may be responsible for a negative attitude toward sexual behavior in a stable couple.
CONCLUSION
Collectively, these preliminary results suggest that sexual function should be routinely assessed in specialized headache centers because women referred for severe head pain report a high rate of sexual dysfunction, including hypoactive sexual desire disorder and sexual pain. Despite the large proportion of the female population affected by recurrent acute or chronic primary headaches, and the significant impact this has on quality of life and psychosocial functioning across age groups, data on sexual function in women in India are limited.[29,30] One of the strengths of the present study is that it is the first such study to explore both this psychopathology in a sample of Indian women with different types of primary headaches referred for evaluation and treatment at a specialized tertiary care center. On the other hand, our findings are limited by the fact that they were collected in a highly selected sample. In addition, the sociocultural environment may be a factor infiuencing a woman's readiness to engage in sexual intercourse, irrespective of the presence of genital pain, or a lack of sexual desire.[31,32] The complexity of the sexual response is universally recognized and there are thus many possible explanations for the link between primary headaches and sexual dysfunction in women. The study is a cross-sectional analysis and consecutive follow-up of the patients periodically for a longer period could have enabled a more detailed understanding of the illness course and outcome.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Rasmussen BK, Olesen J. Epidemiology of migraine and tension-type headache. Curr Opin Neurol. 1994;7:264–71. doi: 10.1097/00019052-199406000-00015. [DOI] [PubMed] [Google Scholar]
- 2.Rasmussen BK. Epidemiology of headache. Cephalalgia. 2001;21:774–7. doi: 10.1177/033310240102100708. [DOI] [PubMed] [Google Scholar]
- 3.Kalichman L. Association between fibromyalgia and sexual dysfunction in women. Clin Rheumatol. 2009;28:365–9. doi: 10.1007/s10067-009-1093-3. [DOI] [PubMed] [Google Scholar]
- 4.Ambler N, Williams AC, Hill P, Gunary R, Cratchley G. Sexual difficulties of chronic pain patients. Clin J Pain. 2001;17:138–45. doi: 10.1097/00002508-200106000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Nappi RE, Terreno E, Tassorelli C, Sances G, Allena M, Guaschino E, et al. Sexual function and distress in women treated for primary headaches in a tertiary university center. J Sex Med. 2012;9:761–9. doi: 10.1111/j.1743-6109.2011.02601.x. [DOI] [PubMed] [Google Scholar]
- 6.Ifergane G, Ben-Zion IZ, Plakht Y, Regev K, Wirguin I. Not only headache: Higher degree of sexual pain symptoms among migraine sufferers. J Headache Pain. 2008;9:113–7. doi: 10.1007/s10194-008-0028-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bestepe E, Cabalar M, Kucukgoncu S, Calıkusu C, Ornek F, Yayla V, et al. Sexual dysfunction in women with migraine versus tension-type headaches: A comparative study. Int J Impot Res. 2011;23:122–7. doi: 10.1038/ijir.2011.16. [DOI] [PubMed] [Google Scholar]
- 8.Sumanen MP, Ojanlatva A, Rantala A, Sillanmäki LH, Mattila KJ. Gender differences in sex life issues – A population-based study of migraine sufferers. BMC Fam Pract. 2008;9:19. doi: 10.1186/1471-2296-9-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Houle TT, Dhingra LK, Remble TA, Rokicki LA, Penzien DB. Not tonight, I have a headache? Headache. 2006;46:983–90. doi: 10.1111/j.1526-4610.2006.00470.x. [DOI] [PubMed] [Google Scholar]
- 10.Headache Classification Subcommitee of the International Headache Society. The international classification of headache disorders. Cephalalgia. (2nd edition) 2004;24(Suppl 1):9–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- 11.Gallagher EJ, Bijur PE, Latimer C, Silver W. Reliability and validity of a visual analog scale for acute abdominal pain in the ED. Am J Emerg Med. 2002;20:287–90. doi: 10.1053/ajem.2002.33778. [DOI] [PubMed] [Google Scholar]
- 12.Wiegel M, Meston C, Rosen R. The female sexual function index (FSFI): Cross-validation and development of clinical cutoff scores. J Sex Marital Ther. 2005;31:1–20. doi: 10.1080/00926230590475206. [DOI] [PubMed] [Google Scholar]
- 13.Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The female sexual function index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26:191–208. doi: 10.1080/009262300278597. [DOI] [PubMed] [Google Scholar]
- 14.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967;6:278–96. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- 16.Stewart WF, Lipton RB, Dowson AJ, Sawyer J. Development and testing of the Migraine Disability Assessment (MIDAS) questionnaire to assess headache-related disability. Neurology. 2001;56:S20–8. doi: 10.1212/wnl.56.suppl_1.s20. [DOI] [PubMed] [Google Scholar]
- 17.Bezov D, Ashina S, Jensen R, Bendtsen L. Pain perception studies in tension-type headache. Headache. 2011;51:262–71. doi: 10.1111/j.1526-4610.2010.01768.x. [DOI] [PubMed] [Google Scholar]
- 18.Antonaci F, Nappi G, Galli F, Manzoni GC, Calabresi P, Costa A, et al. Migraine and psychiatric comorbidity: A review of clinical findings. J Headache Pain. 2011;12:115–25. doi: 10.1007/s10194-010-0282-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goadsby PJ. Pathophysiology of migraine. Neurol Clin. 2009;27:335–60. doi: 10.1016/j.ncl.2008.11.012. [DOI] [PubMed] [Google Scholar]
- 20.Ifergane G, Ben-Zion IZ, Plakht Y, Regev K, Wirguin I. Not only headache: Higher degree of sexual pain symptoms among migraine sufferers. J Headache Pain. 2008;9:113–7. doi: 10.1007/s10194-008-0028-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Magon N, Babu KM. Medicalisation of female sexuality. Int J Clin Cases Investig. 2011;2:1–2. [Google Scholar]
- 22.Holroyd KA, Stensland M, Lipchik GL, Hill KR, O’Donnell FS, Cordingley G, et al. Psychosocial correlates and impact of chronic tension-type headaches. Headache. 2000;40:3–16. doi: 10.1046/j.1526-4610.2000.00001.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mitsikostas DD, Thomas AM. Comorbidity of headache and depressive disorders. Cephalalgia. 1999;19:211–7. doi: 10.1046/j.1468-2982.1999.019004211.x. [DOI] [PubMed] [Google Scholar]
- 24.Maizels M, Burchette R. Somatic symptoms in headache patients: The influence of headache diagnosis, frequency, and comorbidity. Headache. 2004;44:983–93. doi: 10.1111/j.1526-4610.2004.04192.x. [DOI] [PubMed] [Google Scholar]
- 25.Juang KD, Wang SJ, Fuh JL, Lu SR, Su TP. Comorbidity of depressive and anxiety disorders in chronic daily headache and its subtypes. Headache. 2000;40:818–23. doi: 10.1046/j.1526-4610.2000.00148.x. [DOI] [PubMed] [Google Scholar]
- 26.Breslau N, Rasmussen BK. The impact of migraine: Epidemiology, risk factors, and co-morbidities. Neurology. 2001;56:S4–12. doi: 10.1212/wnl.56.suppl_1.s4. [DOI] [PubMed] [Google Scholar]
- 27.Kwan KS, Roberts LJ, Swalm DM. Sexual dysfunction and chronic pain: The role of psychological variables and impact on quality of life. Eur J Pain. 2005;9:643–52. doi: 10.1016/j.ejpain.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 28.Prakash O, Rao TS. Sexuality research in India: An update. Indian J Psychiatry. 2010;52:S260–3. doi: 10.4103/0019-5545.69243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Roy P, Manohar S, Raman R, Sathyanarayana Rao TS, Darshan MS. Female sexual dysfunction: A comparative study in drug naive 1st episode of depression in a general hospital of South Asia. Indian J Psychiatry. 2015;57:242–8. doi: 10.4103/0019-5545.166623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Singh JC, Tharyan P, Kekre NS, Singh G, Gopalakrishnan G. Prevalence and risk factors for female sexual dysfunction in women attending a medical clinic in South India. J Postgrad Med. 2009;55:113–20. doi: 10.4103/0022-3859.52842. [DOI] [PubMed] [Google Scholar]
- 31.Kar N, Koola MM. A pilot survey of sexual functioning and preferences in a sample of English-speaking adults from a small South Indian town. J Sex Med. 2007;4:1254–61. doi: 10.1111/j.1743-6109.2007.00543.x. [DOI] [PubMed] [Google Scholar]
- 32.Kalra G, Subramanyam A, Pinto C. Sexuality: Desire, activity and intimacy in the elderly. Indian J Psychiatry. 2011;53:300–6. doi: 10.4103/0019-5545.91902. [DOI] [PMC free article] [PubMed] [Google Scholar]


