Abstract
Background:
Being able to measure the acute effects of alcohol consumption on psychomotor functions in natural settings could be useful in injury prevention interventions. This study examined the feasibility and acceptability of collecting app-based measures of information processing, working memory and gait stability during times of typical alcohol consumption among young adults.
Methods:
Ten young adults (aged 21–26) with hazardous drinking completed a baseline assessment and ecological momentary assessments (EMA) on 4 consecutive Fridays and Saturdays, every hour from 8pm to 12am. EMA assessed alcohol consumption and perceived intoxication followed by a digit symbol substitution task (DSST), a visuospatial memory task (VSWMT), and a 5-step tandem gait task (TGT). Exit interviews probed user experiences. Multi-level models explored relationships between estimated blood alcohol concentration (eBAC; mg/dl) and DSST and VSWMT performance.
Results:
Participants completed 32% of EMA. Higher rates of non-initiation occurred later in the evening and over time. In multi-level models, higher eBAC was associated with lower DSST scores. 8 out of 10 individuals had at least one drinking occasion when they did not perceive any intoxication. Lower DSST scores would identify impairment in 45% of these occasions. Exit interviews indicated that adding real-time feedback on task performance could increase awareness of alcohol effects.
Conclusions:
Collecting app-based psychomotor performance data from young adults during drinking occasions is feasible and acceptable, but strategies to reduce barriers to task initiation are needed. Mobile DSST is sensitive to eBAC levels and could identify occasions when an individual may not perceive impairments.
INTRODUCTION
Young adults have the highest rates of injuries due to effects of alcohol.1,2 Many of these consequences stem from alcohol’s acute impairments on psychomotor performance3 and decision-making4. Because many individuals may not be aware of their own psychomotor impairments during drinking episodes5, strategies to make alcohol-related psychomotor impairments more apparent to young adults during drinking occasions could deter involvement in activities requiring psychomotor function, thus reducing likelihood of injury.6
To date, the ability to both measure and provide real-time feedback on psychomotor performance outside of controlled laboratories has been limited. The rapid growth of smartphone ownership7 suggests that these devices could be useful to deliver just-in-time interventions that incorporate psychomotor performance feedback. However, fundamental questions need to be addressed. The first is whether target populations (in this case young adults) find completing psychomotor tasks during target occasions (in this case typical periods of drinking) acceptable. Prior studies have shown young adults will complete survey assessments during drinking episodes8,9, but it remains unknown whether they will complete psychomotor tasks during drinking episodes in the natural environment.
The second question is whether brief psychomotor tasks conducted in uncontrolled field settings would be sensitive to levels of blood alcohol concentration (BAC). There is a considerable body of literature showing the deleterious effect of alcohol on psychmotor functioning in controlled settings10–12 and some evidence indicating cognitive assessments conducted by smartphones in a person’s natural environment are reliable and valid13, but none has shown dose-related effects of alcohol on psychomotor performance in the real world.
The third fundamental question is whether actual psychomotor impairments are recognized by young adults when drinking. Prior research has shown following lab-based alcohol administration, young adults report increased willingness to drive after drinking.14 Little is known about whether young adults are aware of impairment in psychomotor functioning during drinking episodes in the natural environment. If impairments are not recognized, this would justify developing interventons aimed at reconciling the “perception-impairment” gap.
The primary aim of this study was to evaluate the feasibility and acceptability of collecting app-based measurement of psychomotor task performance in young adults during typical drinking occasions. The secondary aims were to explore the relationships between estimated blood alcohol concentration (eBAC), task performance and perceived intoxication. To accomplish these aims, we designed an iPhone app to collect ecological momentary assessment (EMA) measures of information processing, working memory and gait stability as well as self-reported drinks consumed and perceived intoxication each hour over weekend evenings (Friday, Saturday) among a cohort of young adults with past hazardous drinking. We hypothesized that young adults would find the EMA tasks acceptable and completion of EMA tasks in the natural environment would be feasible. We predicted task performance would decrease as eBAC increased, psychomotor impairment would exist on occasions when there was no perceived intoxication, and there would be greater psychomotor impairment during the descending limb than the ascending limb of eBAC11,15. Results from this study could be useful in designing effective prevention interventions focused on reducing alcohol-related injuries.
METHODS
This prospective study recruited a convenience sample of young adults who were identified in the emergency department (ED) as reporting past hazardous drinking from February 19th to May 9th, 2016. All participants completed informed consent and were provided with resources for alcohol treatment. This study was approved by the Institutional Review Board at the University of Pittsburgh.
Participants
Participants were young adults (aged 21–26 years) who presented to an urban ED. A total of 28 medically stable ED patients who were not seeking treatment for substance use or intoxicated and were going to be discharged to home were approached by research staff. We did not systematically record the reasons for ED visit. Among those eligible to be approached, 23 provided consent to complete an alcohol use severity screen. Those who reported recent hazardous alcohol consumption based on Alcohol Use Disorder Identification Test for Consumption (AUDIT-C) score of ≥3 for women or ≥4 for men16 and drank primarily on weekends were eligible for participation. We excluded those who reported any medical condition that resulted in impaired thinking or memory or gait, those who reported current or past treatment for alcohol or other substance use disorder, and those without an iOS phone. A total of 10 participants met enrollment criteria and uploaded the DrinkTRAC app to their phone. We instructed all participants to refrain from any non-drinking substance use (excluding cigarette use) during the sampling days. We also informed participants that they would receive $10 for completing the baseline survey and app-based tasks in the ED, $10 for completing the exit survey at 4-weeks, and $1 per completed EMA (up to an additional $40).
App design
The DrinkTRAC app was developed by healthStratica LLC using Apple’s ResearchKit platform, as it allowed for convenient and professional-appearing modular builds that incorporated timed psychomotor tasks. Upon opening the app for the first time, participants were presented with elements of the informed consent document and were asked 4 questions to test comprehension of study procedures. Once participants answered all 4 questions correctly, verified their email address and provided their electronic signature, they were then asked to set up a password to access the app and complete a baseline questionnaire in the ED. Baseline survey questions included measures of socio-demographics and alcohol use severity. The app then presented participants with EMA including two questions (cumulative drinks consumed and, perceived intoxication) followed by psychomotor tasks measuring information processing, working memory and gait stability. The research associate was present to ensure understanding and to observe compliance with instructions on the initial trial of the app’s tasks, conducted in the ED.
Over 4 consecutive Fridays and Saturdays, every hour from 8pm to 12am, participants were sent an electronic notification to log in to the DrinkTRAC app and complete EMA. We chose to sample data on weekend evenings given that this is the time when young adults typically drink alcohol.15 We collected EMA hourly from 8pm to midnight on those nights with the intention of capturing both the ascending and descending limbs of alcohol intoxication. We used fixed hourly assessment times given that it would provide a predictable framework for participants and would allow us to calculate eBAC changes over the evening more easily. We designed each task to take less than 45 seconds to optimize completion and reduce potential for disruptions that could interfere with task performance. The IRB asked that participants be required to enter their username and password on the app prior to entering any data at each time point. Tasks were given in a fixed order. Basic text instructions were given prior to each task, and when tasks were completed, participants were presented with a figure of their completion rates for the day. DrinkTRAC screenshots can be seen in the Appendix.
Measures
Baseline.
Demographics. We collected data on age, sex, race & ethnicity, weight (to calculate eBAC), highest education achieved, employment, and marital status. Drug use. Participants reported frequency of drug use over the last 3 months, including tobacco, cannabis, prescription opioids, street opioids (heroin), stimulants and sedatives using the NM-ASSIST.17 Alcohol Consumption. Alcohol Use Disorder Identification Test for Consumption (AUDIT-C)16 includes three questions about alcohol use over the past 3 months: “How often do you have a drink containing alcohol?”, “How many drinks containing alcohol do you have on a typical day when you are drinking?”, and “How often do you have 5 or more drinks on any one occasion?” The AUDIT-C is scored on a scale of 0–12 (scores of 0 reflect no alcohol use). For men, a score ≥4 is considered positive; for women, a score ≥3 is considered positive.18
Event-Level Alcohol Use and Perception of Intoxication.
Alcohol Consumption. Each hour during the sampling period, the app presented participants with a color picture of standard drink sizes and asked: “How many standard drinks did you have in the past hour?” with a drop-down menu ranging from 0–30. Perceived Intoxication. The app then asked: “How drunk do you feel right now, on a scale from 1 (totally sober) to 10 (completely drunk)?” (adapted from Cromer et al.19).
EMA Psychomotor Tasks.
Digit Symbol Substitution Test (DSST)20 is a well-studied psychomotor task that primarily measures information processing. In a recent review21, four of eleven lab-based studies found effects of BAC on DSST correct responses; at a high BAC, impairment was found in sixteen out of seventeen studies. In our mobile DSST, participants were instructed to respond as quickly and accurately as possible over a period of 45 seconds to visually presented symbols by touching the corresponding digit (0–9) provided in a reference key.22 The reference key differed with each new selection to minimize learning effects. We recorded the number of correct and incorrect symbols identified on each 45-second trial. In analyses, we used the total number of correct responses as our primary variable of interest given that it represents a combination of accuracy and speed.
Visuo-Spatial Working Memory Test (VSWMT)23 measures short-term visual memory, defined as the ability to actively but temporarily maintain information about spatial relations among visually presented stimuli24. Prior research has shown that acute alcohol administration impairs executive functions, including working memory.25,26 In our VSWMT, participants were instructed to first watch the ordered pattern of flowers light up (demonstration phase) and then replicate the illumination pattern by touching the flowers in the same order as they appeared (interactive phase). In the first round, a 3×3 grid of flowers was presented, and a random sequence of 3 flowers was illuminated for one second each. The span (that is, the length of the pattern sequence) is adaptively varied, increasing after users succeed and decreasing after they fail. The VSWMT finishes when the user has either completed the maximum number of tests (n=5) or made the maximum number of errors (n=2). Scores were calculated based on the number of correct choices relative to the number of errors. A similar VSWMT demonstrated good psychometric properties.27
Tandem Gait Task (TGT) was designed as a measure of gait stability. Prior research has shown that alcohol affects both postural stability28 and ataxia29,30. In our TGT, participants were instructed to walk in a straight line for 5 steps. We advised participants to not continue if they felt they could not safely walk unassisted 5 steps in a straight line. If participants clicked “next” they were shown a picture of a phone in a front pocket and told: “Find a place where you can safely walk unassisted for about 5 steps in a straight line”. Followed by: “Put the phone in a pocket or bag and follow the audio instructions. If you do not have somewhere to put the phone, keep it in your hand”. When the participant clicked “Get Started”, the app displayed a timer and played an audio recording of a voice counting down from 5 to 1. If the audio option was turned on, participants heard “Walk up to 5 steps in a straight line, then stand still.” We recorded the acceleration with gyroscope sensors embedded in the phone to collect 3-axis acceleration and angular velocity at a sampling frequency of 0.01 Hz for 30 seconds.
Exit-Interviews.
Within 7 days of completing the 4-week study, study staff called participants to obtain qualitative feedback on acceptability and feasibility using a standardized, semi-structured qualitative guide to assess user experiences, as in our prior work31. Before each interview began, participants were informed that they would be audio recorded, and recordings would be used for research purposes only and would not be accessible to anyone outside the research team. It was stressed that participants’ opinions were important and that there were no right or wrong answers. We started by asking general questions about likes and dislikes of the DrinkTRAC app. We then asked participants to comment on each task specifically. Finally, we asked participants whether they thought that real-time feedback based on their task performance would be of interest to them and whether this feedback might influence how much they drank.
Analyses
EMA Compliance. We first assessed engagement, including patterns of task initiation and completion rates over time, by day of week, and by time of day. We also examined whether baseline factors (e.g., gender) were associated with completion rates. Qualitative Experiences. After one research team member (JCP) transcribed the audio files verbatim, another research team member (BS) organized the quotes into themes based on prior qualitative research done in an identical population of young adults31. The assignment of quotes to themes was then checked by the original team member (JCP), and any disagreements were discussed and rectified. The most salient quotes representing each theme are included in the results. Estimated Blood Alcohol Concentration. We calculated eBAC each hour when data was available using a formula created by Matthews and Miller32. Estimates produced by this formula correlate with breath alcohol concentration and were found to perform best relative to estimates from other commonly used eBAC formulas33. Effects of Alcohol on DSST and VSWMT. We do not analyze effects of alcohol on gait stability in this study due to the complexity of the phone sensor data, which will be explored in a separate study. To model the relationship between eBAC and DSST and VSWMT performance, we used multi-level linear regressions (XTMIXED) in Stata 14.0 (Stata Inc) where task performance served as the dependent variable and was predicted from linear effects of eBAC. The model featured a 3-level structure with assessments (i.e., up to 4 EMA per day) nested within days and days nested within participants. A random intercept was included at both the day and participant levels. We also fit a similar series of multi-level models in which perceived intoxication, instead of eBAC, served as the main predictor. Models controlled for covariates at the participant-level (gender, baseline AUDIT-C score, college education) which were chosen because studies have shown that women respond differently to alcohol than men34, young adults with higher alcohol consumption perform worse on psychomotor tasks35, and education level affects psychomotor performance36. We used full-information maximum likelihood to handle missing data. Ascending versus Descending Limb of Intoxication. Ascending limb was defined as a period when eBAC was increasing and descending limb was defined as a period when eBAC was decreasing from prior available eBAC. We explored whether associations differed on the ascending versus descending limbs of eBAC by running separate regression models for each.
RESULTS
Baseline Assessments
Sample demographics and substance use history are presented in Table 1. Most (70%) of the participants were female and white (60%). Half were college-educated and 30% were still enrolled as students. Roughly one-third of participants used daily tobacco (30%) and 30% used cannabis at least weekly in the past three months. At baseline, the mean number of correct choices made in 45 seconds on DSST was 23.4 (SD 4.3), with a range of 17 to 28. There were very few errors on DSST: two participants had one error and two participants had 2 errors on testing in the ED. The mean score on the VSWMT was 271 (SD 61.1), with a range of scores from 210 to 400. Participant age, sex, race and alcohol severity were not associated with DSST or VSWMT performance at baseline.
Table 1:
Participant Characteristics
| Characteristics | N=10 |
|---|---|
| Age in years, mean (SD) | 23.1 (2.6) |
| Female, n (%) | 7 (70%) |
| Race, n (%) | |
| African American | 2 (20%) |
| White | 6 (60%) |
| Other | 2 (20%) |
| Hispanic Ethnicity, n (%) | 1 (10%) |
| Education, n (%) | |
| Some college | 5 (50%) |
| College graduate or post-graduate | 5 (50%) |
| Employment, n (%) | |
| For wages | 7 (70%) |
| Student | 3 (30%) |
| Married, n (%) | 1 (10%) |
| Alcohol Use Severity (AUDIT-C score), mean (SD) | 5 (1.3) |
| Substance Use in the past 3 months, n (%) | |
| Daily tobacco products | 3 (30%) |
| At least weekly cannabis | 3 (30%) |
| Other drugs | 0 |
| Weight in pounds, mean (SD) | 179 (35) |
Legend: n=number of participants; SD=standard deviation.
Event-Level Drinking & Perception of Intoxication
Over the 4-week sampling period, we sent out 400 timed prompts (aka “Notifications”; 40 per participant). EMA batteries were initiated 128 times (32%). Once initiated, EMA tasks were completed 98% of the time. In fact, only 3 DSST tasks remained incomplete. Individual participants completed a mean of 14 out of 40 EMA batteries (range of 5 to 21). Completion rates decreased over hours in a given evening (60% missing at 8pm; 91.3% missing at 12am) as well as by length of time in study (42% missing on day 1; 86% missing on day 8). Participant age, sex, race and alcohol severity were not associated with EMA completion rates.
Within the 128 completed EMA, we captured 38 unique drinking episodes, with each participant reporting at least 3 drinking episodes. 60 EMA (46.9%) were completed either prior to drinking or on non-drinking evenings, 55 EMA (43.0%) were completed on the ascending eBAC limb, and 13 (10.1%) were completed on the descending eBAC limb.
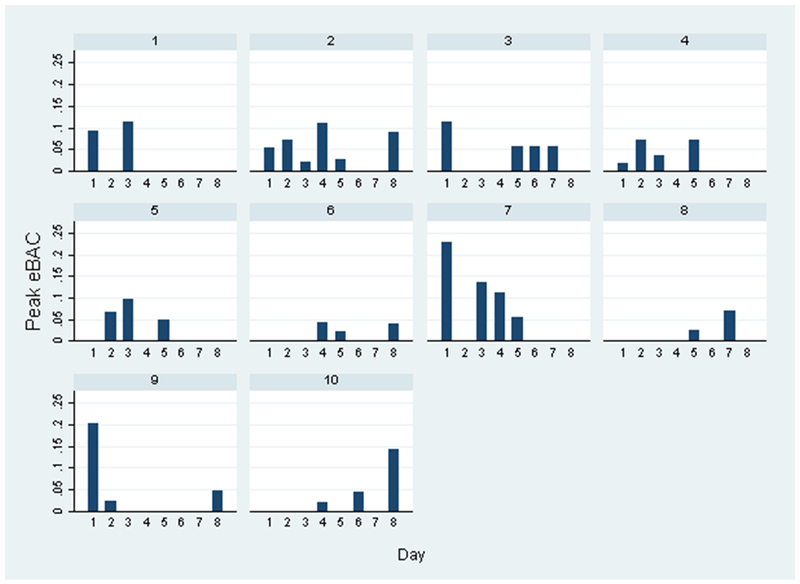
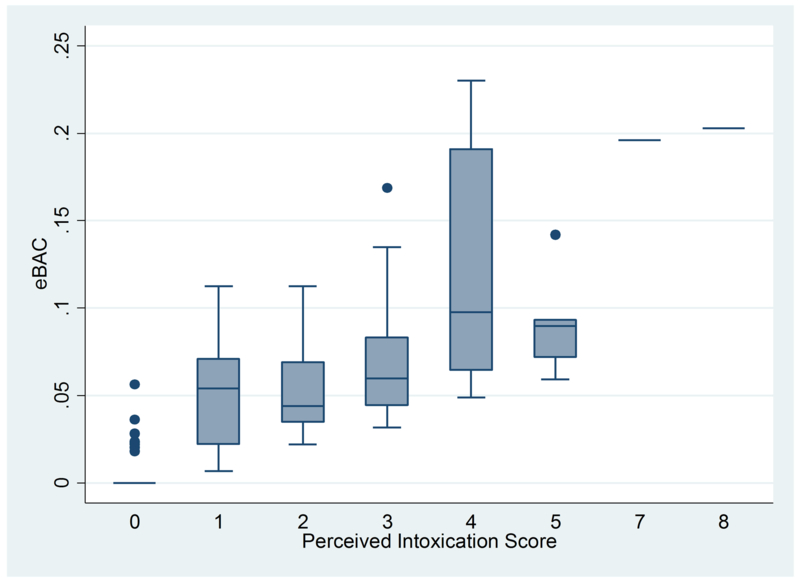
On a drinking day, participants reported consuming a mean of 3.6 drinks (SD=2.2; range: 1–10). The mean eBAC was 0.04 (SD=0.05), with a peak of 0.23 (reported by one individual at one time point). The peak eBACs did not significantly decrease over time, as seen in Figure 1. Participants reported various levels of perceived intoxication, with a mean score of 2.3 (SD=1.8) during a drinking session. There was a fairly high pair-wise correlation between eBAC and perceived level of intoxication (r=0.65). As shown in Figure 2, there was a large variability of eBACs at each level of perceived intoxication.
Figure 1: Peak eBAC over Days by Individual.
Figure shows the peak eBAC calculated for each day in the Study by Participant.
Figure 2: Relationship between eBAC and Perceived Intoxication Score.
Figure shows the median (center line), interquartile range (box), outer bounds (end caps) and outliers (dots) of eBAC (mg/dl) at each reported perceived intoxication score (1=totally sober; 8=completely drunk).
Event-Level DSST and VSWMT Performance
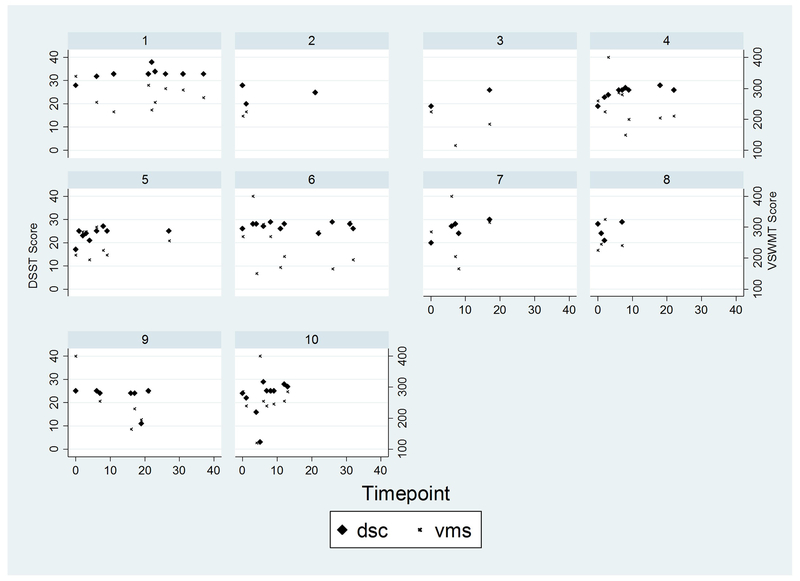
Among the 125 DSST completed during weekend evenings, mean number of correct choices made in 45 seconds on DSST was 24.5 (SD 5.0), with a range of 3 to 38. There were no errors on DSST 90 times (72%), one error 26 times (20.8%), two errors 6 times (4.8%) and 3 or 4 errors 3 times (2.4%). Among the 128 VSWMT completed during weekend evenings, mean score was 239 (SD 59.0), with a range of 90 to 400. The within-person variability in DSST and VSWMT scores over time when eBAC was 0 is shown in Figure 3. For each number of times that someone completed the DSST when eBAC was 0, there was an increase in DSST score (Coef.=0.27; 95% CI 0.05 to 0.48). There were no significant learning effects on VSWMT scores. There were no significant effects of time of day of task completion (i.e. 8p to 12a) on DSST or VSWMT performance.
Figure 3: Stability of Psychomotor Performance over Time by Individual.
Data are presented for timepoints when estimated blood alcohol concentration is 0. DSST = Digit Symbol Substitution Test. VSWMT = Visuo-Spatial Working Memory Task
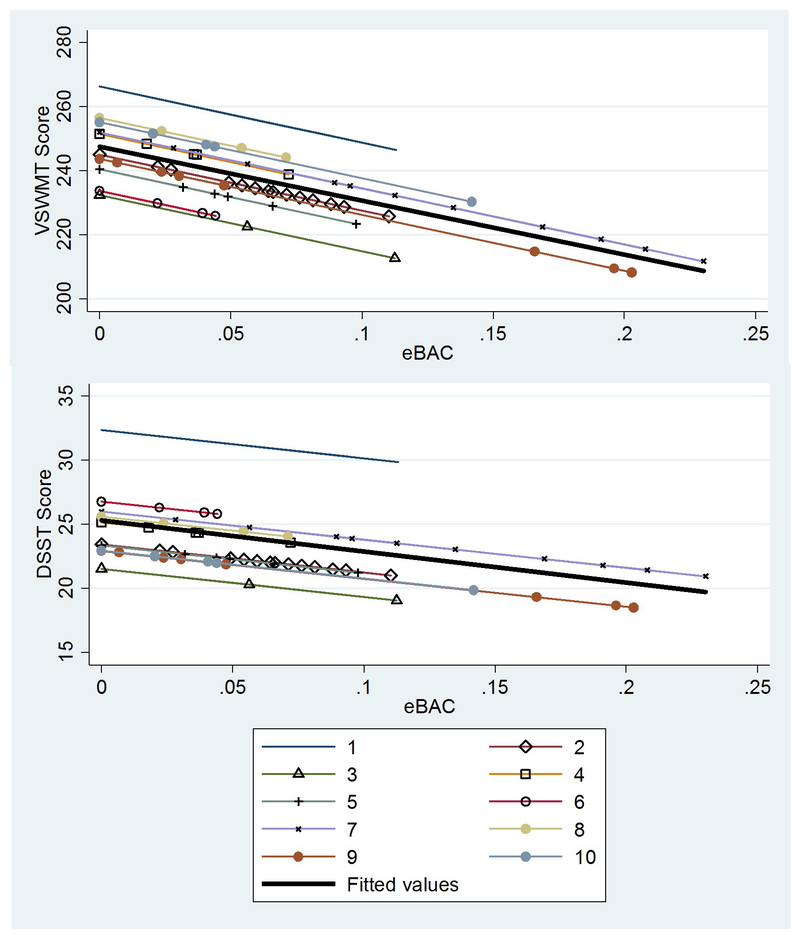
Controlling for sex, baseline drinking severity, and college education, each increase in eBAC of 0.1 mg/dl was associated with a decrease in DSST score of 2.2 (95% CI 0.7 to 3.7). When examining the ascending versus descending limb of drinking separately, the association between eBAC and DSST score was only significant during the descending limb (Coef=−7.0; 95% CI −1.0 to −12.9). Controlling for sex, baseline drinking severity, and college education, for each increase in eBAC of 0.1 mg/dl, there was a non-significant decrease in VSWMT score of 16.6 (95% CI −37 to 4.4). Figure 4 illustrates fixed- and random-effects linear models of eBAC on DSST and VSWMT scores.
Figure 4: Association of eBAC with Psychomotor Performance.
Figures show both fixed- (bold line) and random-effects of eBAC (mg/dl) on DSST and VSWMT scores. Models adjust for gender, baseline alcohol use severity (AUDIT-C score), college education.
There was no significant association of perceived intoxication with performance on DSST or VSWMT scores. There were 11 occasions in 8 participants when eBAC was greater than 0 and there was no perceived intoxication (score= 1). When comparing the mean DSST score in each individual when eBAC=0 to the DSST score on those occasions when eBAC >0 and intoxication was not perceived, there would have been 5 occasions (45%) when the decrease in DSST could have triggered an alert indicating decreased psychomotor performance.
Qualitative User Experience Data
All 10 participants completed exit interviews. In general, participants reported the DrinkTRAC app was easy to use and the EMA tasks were enjoyable. Participants commented they found the tasks more difficult when drinking. One participant explained: “It was a really good learning experience to see the effect that drinking had on my brain. I could tell I had difficulty doing [the app tasks] when I was drunk. I felt like I was doing them pretty fast when didn’t have alcohol and I know I was doing it like ten times slower trying to do them when I was drinking.”
Participant feedback on the DSST specifically indicated it was fun and challenging. One participant said: “I think that was a good one as well because you had to think about what you were looking for and then locate it and if you had a few drinks you weren’t cognitively aware so it took a while to figure out.” However, one participant commented there was too much information on the screen to process at any one time. For the VSWMT, several participants remarked it was the more difficult task when they were drinking, and mistakes increased when distracted. Regarding the gait stability task, participants described barriers to completion, especially if they were in a public place. For example, one participant said: “sometimes you’re in a public place…if they were kind of crowded, it made the walking task difficult.”
Regarding compliance in completing the EMA tasks, participants stated they missed completing some because they were either still at work (for the 8pm EMA) or asleep (for the 11pm and 12am tasks). Participants relayed there were a few times when they were either distracted or interrupted while completing the tasks, which might have affected their performance. We probed other barriers to task completion and found although participants supported receiving push notifications during drinking episodes, almost all felt that the need to enter a password every time they were asked to complete EMA (as required by the IRB) was a nuisance that reduced compliance. Many participants commented they often forgot their password, especially when drinking and several suggested incorporating the iOS fingerprint “Touch ID” feature in future versions.
Finally, when we asked participants whether including real-time feedback on task performance would influence them in any way, most participants said it would either influence them to stop drinking (if they performed poorly) or to make different post-drinking transportation plans (i.e., catch a cab). One participant commented: “I think it would be interesting because people don’t really think about [how alcohol causes impairments]. I wouldn’t have thought about it until I did this study.” A couple of male participants with heavier past drinking stated they did not think it would influence their behavior.
DISCUSSION
Our results suggest that using app-based assessments of psychomotor performance during typical drinking occasions with young adults is feasible and acceptable despite sub-optimal EMA completion rate. Participants by and large supported the ease of completing the app-based tasks and the usefulness of such tasks to identify performance deficits produced by alcohol. Event-level analyses suggest that psychomotor tasks, including the DSST, are sensitive to estimated blood alcohol content, and could be useful in identifying drinking occasions when a young adult is exhibiting impairments that they may not appreciate. Together, these findings suggest the potential utility of mobile psychomotor tasks to guide real-time feedback on task performance as a component of an injury prevention intervention for young adult drinkers.
Although the EMA completion rates were low, especially later in the evenings and as the number of days in the study increased, it is unclear what completion rates one should expect when prompting young adults to complete psychomotor tasks during drinking occasions in the field. In Tiplady et al.12, 38 social drinkers (ages 18–54) were randomly prompted twice a day, from 9am to 10pm, over a 2-week assessment period to complete EMA of alcohol consumption and psychomotor tasks. Although the completion rate was 80.3%, the vast majority of completed EMA were prior to 8pm. In Schuster et al.27, 287 young adults completed an average of 38 random EMA prompts, which included substance use (including alcohol) assessment and a working memory task, over 7 days. Participants completed 92.6% of EMA prompts, reporting an average of 2.8 alcohol use occasions over that week. It was not reported how many assessments occurred in the evenings. Another study found that only 41% of young adults reported using a brief alcohol intervention app.37 Taken together, existing studies indicate a wide range in compliance with EMA and alcohol intervention apps. In the current study, the main barriers to compliance included required log-in to access the tasks, and fixed (rather than personalized) timing of EMA. Future designs should allow some personalization of timing of tasks and more streamlined app task completion.
We did not find that task performance degraded as a function of time of day, but did find there were small learning effects on DSST scores over days in study, which is consistent with prior literature on repeated cognitive testing38. Despite this, we found that after controlling for relevant covariates, there was a dose-response relationship between eBAC and DSST scores. Additionally, consistent with prior literature10, this effect seemed to be pronounced during the descending limb of drinking. Prior laboratory-based studies have found 5 or more drinks in the past 6 hours results in more incorrect memory scanning choices and slower reaction time than when not drinking12 and alcohol results in a lower working memory27, but no prior study to our knowledge has examined dose-response relationship between eBAC and psychomotor performance in the natural environment. The absence of a significant association of eBAC with the mobile VSWMT suggests the task might be less sensitive to alcohol effects, relative to the DSST. However, alcohol effects on VSWMT performance were in the expected direction, and this study had limited statistical power.
Finally, we found, despite a fairly high correlation between eBAC and perceived level of intoxication, there was no significant association between perceived intoxication and scores on the DSST and VSWMT. 8 out of 10 participants had at least one occasion when they had a eBAC>0 and did not perceived intoxication. On these occasions, 45% of the time their DSST score was lower than their average when they had no alcohol in their system. These findings suggest opportunity exists to increase awareness of alcohol effects on psychomotor impairment with real-time feedback for certain individuals. Qualitative data also suggest that performing the tasks during periods of acute alcohol intoxication could help to increase an individual’s awareness of the effects of alcohol on cognition and behavior.
Limitations
This study is limited by the small sample size and missing data, which could limit validity of stated associations between task performance and eBACs. Given that these were exploratory aims, they should be replicated in larger studies. As well, we did not measure concurrent drug use (i.e. cannabis) with drinking events, which could have influenced task performance. We attempted to minimize this by asking participants to refrain from other drug use during days of study involvement. Findings may not be applicable to other populations, such as young adults with less severe alcohol use, other age groups such as adolescents or individuals who use other types of phones (e.g. Android). Self-report of alcohol use using EMA has demonstrated reliability and validity39, but may be subject to bias. As well, the reporting accuracy of drinks consumed at higher BACs is prone to errors. We attempt to minimize bias through the use of use of experience sampling methods, by using a computer interface, and including a picture reference of standardized drinks each time a user reported consumption over the last hour. Future work could use transdermal alcohol sensors to validate eBAC levels, but they have been found to be less useful in detecting lower drinking quantities as compared to self-reports40 and BAC levels tend to lag behind consumption by up to several hours41. Despite exit-interview reports indicating that some individuals became more aware of their drinking due to self-monitoring, we did not find evidence of actual reductions in peak eBAC over days in study. There is evidence that messaging interventions can reduce hazardous drinking in young adults42, so it is likely that incorporating just-in-time messaging based on task performance could potentially enhance intervention effects, especially in reducing alcohol-related risky activities (i.e. driving).
Conclusions
App-based assessments of psychomotor performance are feasible and acceptable to young adults during typical drinking occasions and could be useful in providing real-time feedback to reduce alcohol-related injuries. Design optimization could improve engagement. Larger studies are needed to understand strength of associations between BAC and psychomotor impairments.
Acknowledgments
FUNDING
Financial support provided to BS by the National Institute of Alcohol Abuse and Alcoholism, National Institute of Health (K23 AA023284). The funding organization had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
BS has received royalties for an exclusive license for a text message program for alcohol from healthStratica LLC.
REFERENCES
- 1.Hingson RW, Zha W, Weitzman ER. Magnitude of and trends in alcohol-related mortality and morbidity among U.S. college students ages 18–24, 1998–2005. J Stud Alcohol Drugs, Suppl. 2009;(16):12–20. doi: 10.15288/jsads.2009.s16.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Traffic Safety Facts: Alcohol-Impaired Driving: 2010 Data. PsycEXTRA Dataset. doi: 10.1037/e624682012-001. [DOI] [Google Scholar]
- 3.Christoforou Z, Karlaftis MG, Yannis G. Reaction times of young alcohol-impaired drivers. Accid Anal Prev. 2013;61:54–62. doi: 10.1016/j.aap.2012.12.030. [DOI] [PubMed] [Google Scholar]
- 4.Steele CM, Josephs RA. Alcohol myopia: Its prized and dangerous effects. Am Psychol. 1990;45(8):921–933. doi: 10.1037//0003-066x.45.8.921. [DOI] [PubMed] [Google Scholar]
- 5.Morris DH, Treloar HR, Niculete ME, Mccarthy DM. Perceived danger while intoxicated uniquely contributes to driving after drinking. Alcohol Clin Exp Res. 2013;38(2):521–528. doi: 10.1111/acer.12252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shults RA, Elder RW, Sleet DA, et al. Reviews of evidence regarding interventions to reduce alcohol-impaired driving. Am J Prev Med. 2001;21(4):66–88. doi: 10.1016/s0749-3797(01)00381-6. [DOI] [PubMed] [Google Scholar]
- 7.Anderson Monica. Pew Research Center. Technology Device Ownership: 2015. http://www.pewinternet.org/2015/10/29/technology-device-ownership-2015/ Accessed 12/13/16. [Google Scholar]
- 8.Piasecki TM, Alley KJ, Slutske WS, et al. Low Sensitivity to Alcohol: Relations with hangover occurrence and susceptibility in an ecological momentary assessment investigation. J Stud Alcohol Drugs. 2012;73(6):925–932. doi: 10.15288/jsad.2012.73.925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scholey AB, Benson S, Neale C, Owen L, Tiplady B. Neurocognitive and mood effects of alcohol in a naturalistic setting. Hum Psychopharmacol. 2012;27(5):514–516. doi: 10.1002/hup.2245. [DOI] [PubMed] [Google Scholar]
- 10.Starkey NJ, Charlton SG. The effects of moderate alcohol concentrations on driving and cognitive performance during ascending and descending blood alcohol concentrations. Hum Psychopharmacol. 2014;29(4):370–383. doi: 10.1002/hup.2415. [DOI] [PubMed] [Google Scholar]
- 11.Marczinski CA, Fillmore MT. Acute alcohol tolerance on subjective intoxication and simulated driving performance in binge drinkers. Psychol Addict Behav. 2009;23(2):238–247. doi: 10.1037/a0014633. [DOI] [PubMed] [Google Scholar]
- 12.Tiplady B, Oshinowo B, Thomson J, Drummond GB. Alcohol and cognitive function: assessment in everyday life and laboratory settings using mobile phones. Alcohol Clin Exp Res. 2009;33(12):2094–2102. doi: 10.1111/j.1530-0277.2009.01049.x. [DOI] [PubMed] [Google Scholar]
- 13.Sliwinski MJ, Mogle JA, Hyun J, Munoz E, Smyth JM, Lipton RB. Reliability and validity of ambulatory cognitive assessments. Assessment. 2016. doi: 10.1177/1073191116643164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Amlung MT, Morris DH, McCarthy DM. Effects of acute alcohol tolerance on perceptions of danger and willingness to drive after drinking. Psychopharmacol (Berl). 2014;231(22):4271–4279. doi: 10.1007/s00213-014-3579-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maggs JL, Williams LR, Lee CM. Ups and downs of alcohol use among first-year college students: number of drinks, heavy drinking, and stumble and pass out drinking days. Addict Behav. 2011;36(3):197–202. doi: 10.1016/j.addbeh.2010.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bradley KA, Debenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol Clin Exp Res. 2007;31(7):1208–1217. doi: 10.1111/j.1530-0277.2007.00403. [DOI] [PubMed] [Google Scholar]
- 17.Humeniuk R, Ali R, Babor TF, et al. Validation of the alcohol, smoking and substance involvement screening test (ASSIST). Addiction. 2008;103(6):1039–1047. doi: 10.1111/j.1360-0443.2007.02114.x. [DOI] [PubMed] [Google Scholar]
- 18.Rubinsky AD, Dawson DA, Williams EC, Kivlahan DR, Bradley KA. AUDIT-C scores as a scaled marker of mean daily drinking, alcohol use disorder severity, and probability of alcohol dependence in a U.S. general population sample of drinkers. Alcohol Clin Exp Res. 2013;37(8):1380–1390. doi: 10.1111/acer.12092. [DOI] [PubMed] [Google Scholar]
- 19.Cromer JR, Cromer JA, Maruff P, Snyder PJ. Perception of alcohol intoxication shows acute tolerance while executive functions remain impaired. Exp Clin Psychopharmacol. 2010;18(4):329–339. doi: 10.1037/a0019591. [DOI] [PubMed] [Google Scholar]
- 20.Wechsler D The Measurement and Appraisal of Adult Intelligence. Baltimore, MD: Williams & Wilkins; 1958. [Google Scholar]
- 21.Jongen S, Vuurman EF, Ramaekers JG, Vermeeren A. The sensitivity of laboratory tests assessing driving related skills to dose-related impairment of alcohol: A literature review. Accid Anal Prev. 2016;89:31–48. doi: 10.1016/j.aap.2016.01.001. [DOI] [PubMed] [Google Scholar]
- 22.Cameron E, Sinclair W, Tiplady B. Validity and sensitivity of a pen computer battery of performance tests. J Psychopharmacol. 2001;15(2):105–110. doi: 10.1177/026988110101500207. [DOI] [PubMed] [Google Scholar]
- 23.Ichikawa S Verbal memory span, visual memory span, and their correlations with cognitive tasks. Jpn Psychol Res. 1983;25:173–180. [Google Scholar]
- 24.Luck SJ, Vogel EK. Visual working memory capacity: from psychophysics and neurobiology to individual differences. Trends Cogn Sci. 2013;17(8):391–400. doi: 10.1016/j.tics.2013.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weissenborn R, Duka T. Acute alcohol effects on cognitive function in social drinkers: their relationship to drinking habits. Psychopharmacology (Berl). 2003;165(3):306–312. doi: 10.1007/s00213-002-1281-1. [DOI] [PubMed] [Google Scholar]
- 26.Tapert SF, Pulido C, Paulus MP, Schuckit MA, Burke C Level of response to alcohol and brain response during visual working memory. J Stud Alcohol 2004; 65: 692–700. doi: 10.15288/jsa.2004.65.692. [DOI] [PubMed] [Google Scholar]
- 27.Schuster RM, Mermelstein RJ, Hedeker D. Ecological momentary assessment of working memory under conditions of simultaneous marijuana and tobacco use. Addiction. 2016;111(8):1466–1476. doi: 10.1111/add.13342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nieschalk M, Ortmann C, West A, SchmWe F, Stoll W, Fechner G. Effects of alcohol on body-sway patterns in human subjects. Int J Legal Med. 1999;112(4):253–260. doi: 10.1007/s004140050245. [DOI] [PubMed] [Google Scholar]
- 29.Mills KC, Bisgrove EZ. Body sway and divided attention performance under the influence of alcohol: dose-response differences between males and females. Alcohol Clin Exp Res. 1983;7(4):393–397. doi: 10.1111/j.1530-0277.1983.tb05492.x. [DOI] [PubMed] [Google Scholar]
- 30.Jansen EC, Thyssen HH, Brynskov J. Gait analysis after intake of increasing amounts of alcohol. Z Rechtsmed. 1985;94(2):103–107. doi: 10.1007/BF00198678. [DOI] [PubMed] [Google Scholar]
- 31.Suffoletto B, Kristan J, Person Mecca L, Chung T, Clark DB. Optimizing a text message intervention to reduce heavy drinking in young adults: focus group findings. JMIR Mhealth Uhealth. 2016;4(2):e73. doi: 10.2196/mhealth.5330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Matthews DB, Miller WR. Estimating blood alcohol concentration: two computer programs and their applications in therapy and research. Addict Behav. 1979;4(1):55–60. doi: 10.1016/0306-4603(79)90021-2. [DOI] [PubMed] [Google Scholar]
- 33.Hustad JT, Carey KB. Using calculations to estimate blood alcohol concentrations for naturally occurring drinking episodes: a validity study. J Stud Alcohol. 2005;66(1):130–138. doi: 10.15288/jsa.2005.66.130. [DOI] [PubMed] [Google Scholar]
- 34.Carey KB, Henson JM, Carey MP, Maisto SA. Which heavy drinking college students benefit from a brief motivational intervention? J Consult Clin Psychol. 2007;75(4):663–669. doi: 10.1037/0022-006X.75.4.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sullivan EV, Brumback T, Tapert SF, et al. Cognitive, emotion control, and motor performance of adolescents in the NCANDA study: contributions from alcohol consumption, age, sex, ethnicity, and family history of addiction. Neuropsychology. 2016;30(4):449–473. doi: 10.1037/neu0000259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Avolio BJ, Waldman DA. Variations in cognitive, perceptual, and psychomotor abilities across the working life span: examining the effects of race, sex, experience, education, and occupational type. Psychol Aging. 1994;9(3):430–442. doi: 10.1037/0882-7974.9.3.430. [DOI] [PubMed] [Google Scholar]
- 37.Gajecki M, Berman AH, Sinadinovic K, Rosendahl I, Andersson C. Mobile phone brief intervention applications for risky alcohol use among university students: a randomized controlled study. Addict Sci Clin Pract. 2014;9:11. doi: 10.1186/1940-0640-9-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bartels C, Wegrzyn M, Wiedl A, Ackermann V, Ehrenreich H. Practice effects in healthy adults: a longitudinal study on frequent repetitive cognitive testing. BMC Neurosci. 2010;11:118. doi: 10.1186/1471-2202-11-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wray TB, Merrill JE, Monti PM. Using ecological momentary assessment (EMA) to assess situation-level predictors of alcohol use and alcohol-related consequences. Alcohol Res. 2014;36(1):19–27. [PMC free article] [PubMed] [Google Scholar]
- 40.Karns-Wright TE, Roache JD, Hill-Kapturczak N, Liang Y, Mullen J, Dougherty DM. Time delays in transdermal alcohol concentrations relative to breath alcohol concentrations. Alcohol Alcohol. 2017;52(1):35–41. doi: 10.1093/alcalc/agw058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Leffingwell TR, Cooney NJ, Murphy JG, et al. Continuous objective monitoring of alcohol use: twenty-first century measurement using transdermal sensors. Alcohol Clin Exp Res. 2013;37(1):16–22. doi: 10.1111/j.1530-0277.2012.01869.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Suffoletto B, Kristan J, Chung T, et al. An interactive text message intervention to reduce binge drinking in young adults: a randomized controlled trial with 9-month outcomes. PLoS One. 2015;10(11):e0142877. doi: 10.1371/journal.pone.0142877. [DOI] [PMC free article] [PubMed] [Google Scholar]