Abstract
Objective
Mental health (MH) diagnoses, which are prevalent among persons living with human immunodeficiency virus (HIV) infection, might be linked to failed retention in HIV care. This review synthesized the quantitative evidence regarding associations between MH diagnoses or symptoms and retention in HIV care, as well as determined if MH service utilization (MHSU) is associated with improved retention in HIV care.
Methods
A comprehensive search of the Centers for Disease Control and Prevention’s HIV/AIDS Prevention Research Synthesis database of electronic (e.g., MEDLINE, EMBASE, PsycINFO) and manual searches was conducted to identify relevant studies published during January 2002–August 2017. Effect estimates from individual studies were pooled by using random-effects meta-analysis, and a moderator analysis was conducted.
Results
Forty-five studies, involving approximately 57,334 participants in total, met the inclusion criteria: 39 examined MH diagnoses or symptoms, and 14 examined MHSU. Overall, a significant association existed between MH diagnoses or symptoms and lower odds of being retained in HIV care (odds ratio [OR] = 0.94; 95% confidence interval [CI] = 0.90–0.99). Health insurance status (β = 0.004; Z = 3.47; p = 0.001) significantly modified the association between MH diagnoses or symptoms and retention in HIV care. In addition, MHSU was associated with an increased odds of being retained in HIV care (OR = 1.84; 95% CI = 1.45–2.33).
Conclusions
Results indicate that MH diagnoses or symptoms are a barrier to retention in HIV care and emphasize the importance of providing MH treatment to HIV patients in need.
Keywords: meta-analysis [publication type], mental health, retention in care, mental health services, human immunodeficiency virus
Retention in HIV care, defined as consistency in HIV care appointment attendance over time (Horstmann, Brown, Islam, Buck, & Agins, 2010), increases the likelihood that a person living with HIV (PLWH) will be prescribed and adhere to their antiretroviral medications (Thompson et al., 2012). Among persons living with diagnosed HIV infection in the United States during 2014, 56.9% were retained in HIV care (Centers for Disease Control and Prevention, 2017b). Consequently, not being in care is associated with increased viral load, lower CD4+ cell count, and increased mortality (Rao et al., 2013).
A primary goal of HIV care guidelines is to increase retention in HIV care to achieve viral suppression (White House Office of National AIDS Policy, 2015). PLWH who are virally suppressed (i.e., have an undetectable viral load), have a negligible risk of transmitting the virus to others (Prevention Access Campaign, 2016). Individual and social factors might affect the likelihood that PLWH can achieve optimal retention in HIV care (Holtzman, Brady, & Yehia, 2015).
Mental health (MH) is one individual-level factor that might merit targeted efforts to improve HIV care. PLWH who also have MH diagnoses or symptoms are less likely to achieve viral suppression than those without the additional comorbidity (Yehia et al., 2015). The burden of HIV among those with MH diagnoses or symptoms is far greater than among the general population; approximately half of all PLWH screen positive for one or more psychiatric disorders (Health Resources and Services Administration, 2015).
Research on MH and HIV care has focused on medication adherence (Gonzalez, Batchelder, Psaros, & Safren, 2011; Langebeek et al., 2014; Sin & DiMatteo, 2014). Because adherence is affected by retention in care, understanding how MH is related to retention in HIV care is important for public health practice in attaining the goal of viral load suppression and lowering the HIV transmission risk. In semi-structured interviews with PLWH, mental illness was identified as a barrier to retention in HIV care because it can lead to apathy about health care and missed HIV care appointments (Holtzman, Shea, et al., 2015).
In addition to psychiatric diagnoses, MH treatment is an individual-level factor that might facilitate a patient’s retention in care. A previous systematic review of integrated HIV care reported an association between MH service utilization (MHSU), other ancillary services (e.g., case management or transportation), and retention in HIV care (Soto, Bell, & Pillen, 2004). Additionally, a positive association between a person’s receipt of MH and substance abuse treatment or counseling and retention in HIV care has also been observed (Ashman, Conviser, & Pounds, 2002). Those previous studies assessed MH services in combination with other services (e.g., substance abuse treatment); thus, individual effects (i.e., MH care usage effect on retention) could not be determined.
Although research indicates MH conditions are a barrier to retention in HIV care (Horstmann et al., 2010), other studies have reported that a MH diagnosis increases retention in HIV care (Byrd, Furtado, Bush, & Gardner, 2015; Ulett et al., 2009; Yehia et al., 2015). It remains unclear whether all MH diagnoses or symptoms affect a patient’s retention in care equally or whether certain factors modify the association between MH diagnoses or symptoms and retention in care. Additionally, is MHSU associated with retention in care when assessed independently from other ancillary services? This systematic review examined the association between different MH diagnoses or symptoms and retention in HIV care. Secondly, this study examined whether MHSU is associated with retention in HIV care.
Methods
Search Strategy
A systematic review of the literature was conducted, and this report follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement (Appendix A) (Moher et al., 2015). The Centers for Disease Control and Prevention’s (CDC) Prevention Research Synthesis (PRS) Project’s cumulative HIV, acquired immunodeficiency syndrome (AIDS), and sexually transmitted disease (STD) research database was used for identifying relevant reports. The PRS database comprises published literature located through automated and manual searches developed by librarians with expertise in developing and conducting comprehensive systematic searches (DeLuca et al., 2011). The searches included MEDLINE (OVID), EMBASE (OVID), CINHAL (EBSCOhost), PsycINFO (OVID), and Sociological Abstracts (ProQuest) databases. Each of the automated searches were developed in the MEDLINE database with indexing and keyword terms cross-referenced by using Boolean logic with no language limits. The finalized search was translated into the other databases to adhere to each proprietary indexing system. The PRS database comprises search strategies focused on (1) behavioral risk reduction, (2) medication adherence, and (3) linkage to, retention in, and re-engagement in HIV care (see Appendix B for the three searches as implemented in MEDLINE [OVID] with any restrictions applied). Other searches are available from the corresponding author.
The search of the PRS database for this review consisted of two separate queries, (1) a title, abstract, and keyword search using MH terms (e.g., bipolar, depression, mental disorder, mood states, posttraumatic stress disorder, psychotic disorder) (see Appendix C for the full list of MH terms); and (2) a search of citations coded with an indexing term for linkage or retention in HIV care (Appendix C). The two queries were initially conducted in July 2015 (search period: January 2002–July 2015) and were repeated in March 2016 and August 2017. Additionally, a separate hand-search was conducted to identify articles in non-HIV–related literature that might have been missing in the PRS database including checking the reference lists of included citations (Appendix D).
Inclusion Criteria
Studies were included in the review if they (1) were conducted in the United States; (2) assessed persons with HIV; (3) contained a measurement of MH status and a measure of retention in HIV care; (4) measured any of the following MH variables: Diagnostic and Statistical Manual of Mental Disorders (DSM) psychiatric diagnosis (American Psychiatric Association, 2013), MH-related symptoms, or MHSU (e.g., visit to a health professional for MH treatment or psychological counseling); (5) included children, adolescents, or adults with diagnosed HIV/AIDS; and (6) assessed MH symptoms or diagnosed MH disorders by self-report measures, interviews, or medical record abstraction. This review examined the entire range of MH diagnoses and symptoms that PLWH can experience by including the full continuum of MH diagnoses and symptoms that might affect retention in HIV care.
This review exclusively focused on MH diagnoses or symptoms and excluded studies that only reported a measure of substance abuse and did not assess MH status. Additionally, to ensure that the association between MH and retention in HIV care was not confounded by any ongoing HIV− or mental health–related interventions, intervention reports were excluded. Lastly, studies whose target population was an HIV provider or caregiver were excluded because PLWH were the target population for this review.
Data Abstraction and Quality Assessment
Citations and full articles from the search were reviewed by a varying combination of two independent reviewers from a pool of 4 authors (RR, MW, AA, CP) at the title and abstract level, followed by each full text by using DistillerSR v.2 (Evidence Partners, Ottawa, Canada) (Evidence Partners, 2016). Data were abstracted from each paper that met the inclusion criteria by using standardized forms developed by study staff (MW, AA). Information abstracted included study characteristics (i.e., study location, study design, target population, and inclusion criteria), sample characteristics (i.e., analytic sample size, age, sex, race/ethnicity, sexual orientation, substance use status, and health insurance status), MH variable information (i.e., type of MH diagnosis or symptoms, MH measurement tool, type of MH service, and provider type), retention outcome, and study quality. Effect estimates were abstracted that assessed the association between MH diagnoses or symptoms or MHSU as the exposure variable and retention in HIV care as the outcome variable. Additionally, adjusted effect sizes that accounted for potential confounders were abstracted for analysis when available.
Study quality was evaluated by using the National Heart, Lung, and Blood Institute (NHLBI) quality-assessment tool for observational cohort and cross-sectional studies (National Heart Lung Blood Institute, 2014). Responses to each of the 13 items included “Yes,” “No,” “Not Applicable,” or “Not Reported.” Items with a “No” response were considered a limitation of the study. We removed a single question from the NHLBI tool on sample power description, since it did not apply to the included studies. Citations were given an overall quality rating of “Good,” “Fair,” or “Poor,” based on a priori criteria. Prospective and retrospective cohort studies that assessed the MH variable before measuring the outcome with sufficient time between measurements and controlled for confounders were scored as “good.” Cross-sectional studies were categorized as “fair.” Cross-sectional and retrospective studies that failed to account for confounders and did not describe the exposure or outcome variable were categorized as “poor.” Responses were reconciled to resolve mismatches.
Publication bias was assessed by visual inspection of funnel plot asymmetry (Egger, Davey Smith, Schneider, & Minder, 1997) and validated by Begg and Mazumdar rank correlation (Begg & Mazumdar, 1994). Additionally, the random effects fail-safe N was estimated to determine what number of missing studies would be required to nullify the overall mean effect estimate (Rosenberg, 2005).
Outcome Variables
The primary outcome of interest was retention in primary HIV care. Retention in care was defined as continuity in HIV care appointments over a duration of time (Mugavero et al., 2012) and is operationalized as multiple, completed outpatient HIV care visits with a health care professional. Retention in HIV care include gaps in care (e.g., discontinuities in care), visit constancy (e.g., consecutive time intervals with one or more kept medical appointments), and appointment adherence (e.g., percentage of appointments attended or missed out of the number scheduled).
Data Analysis
Effect sizes were converted to log odds ratios (ORs), weighted by the inverse variance, and then aggregated by using a random effects model (Hedges & Olkin, 2014). Effect sizes were then converted back to an OR for interpretation. Effect sizes that were reported in the opposite direction (association between MH and poor retention in care) were transformed so that an OR ≥1.0 indicated an improvement in retention in HIV care and a value <1.0 was indicative of a lower odds of retention in HIV care. The summary effect estimate, reported as an OR, was calculated by using Comprehensive Meta-Analysis v.2 (Biostat, Englewood, New Jersey) (Borenstein, Hedges, Higgins, & Rothstein, 2005). The likelihood of heterogeneity across studies was determined by the Q statistic, and the percentage of variability caused by heterogeneity was calculated by I2 (Higgins, Thompson, Deeks, & Altman, 2003). I2 values of 25%, 50%, and 75% were categorized as low, medium, and high heterogeneity, respectively.
A moderator analysis was then conducted by examining whether factors identified a priori might modify the effect estimate or explain any heterogeneity included: age (mean age), sex (percentage male), race/ethnicity (percentage black race), sexual orientation (percentage men who have sex with men [MSM]), substance abuse status (percentage currently or within the previous year using illegal substances), health insurance status (percentage receiving public health insurance), education status (percentage with a high school education or less), type of MH diagnosis or symptoms (depression diagnosis or symptoms versus other MH diagnosis or symptoms), measurement of MH status (MH clinical diagnosis versus self-reported symptoms), assessment period for retention in HIV care, retention in care measurement, and study design (prospective cohort, cross-sectional, or retrospective). Studies that did not report a specific population or study level characteristic were not included in the respective moderator analysis. Meta-regression was used to assess how continuous population level variables modify the overall effect estimate. Mixed model analysis was used to assess between group (QB) differences in dichotomous or categorical study level variables.
Studies that examined the association between more than one form of a MH diagnosis or symptoms (e.g., both depression and posttraumatic stress disorder [PTSD]) and retention in care outcome contributed multiple effect estimates to the overall summary effect. A sensitivity analysis was conducted to determine whether including multiple dependent effects from a single study substantially changed the overall results. The analysis was repeated with only one effect per study by using a pooled MH outcome (e.g., psychosis, psychiatric diagnoses, or mood disorders). If no pooled MH outcome variable was reported, the association between depression and retention in care was used as the single effect size, because depression was the most commonly assessed MH outcome. Only one effect size was included for studies that examined MHSU and retention in care.
Results
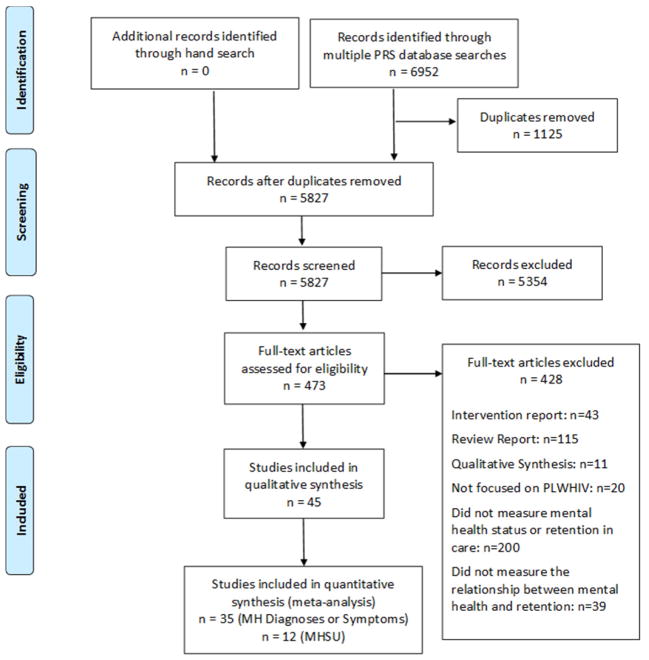
After de-duplication, a total of 5,827 studies were identified that were published during 2002–2017. No relevant articles were identified in any of the hand-searched non-HIV–related journals. A total of 5,354 articles were excluded at title and abstract level, and 428 articles were excluded after full text review. After excluding irrelevant studies, 45 studies, involving approximately 57,334 participants in total, met the inclusion criteria (Figure 1). Data were abstracted from the included studies and analyzed (Appendix E). A total of 39 (52 effects) studies reported on MH diagnoses or symptoms, and 14 (12 effects) studies reported on MHSU.
Figure 1.
Flow diagram of the study selection process.
Mental Health Diagnoses or Symptoms and Retention in HIV Care
Characteristics of Included Studies
Thirty-nine studies examined the association between MH diagnoses or symptoms and retention in HIV care. Among those studies, 16 were prospective (Aidala, Lee, Abramson, Messeri, & Siegler, 2007; Ashman et al., 2002; Buchberg et al., 2015; Byrd et al., 2015; Dang, Westbrook, Hartman, & Giordano, 2016; Dietz et al., 2010; Jacks et al., 2015; Kushel et al., 2006; Mellins, Kang, Leu, Havens, & Chesney, 2003; Merlin et al., 2012; Minniear et al., 2013; Outlaw et al., 2010; Schumacher et al., 2013; Traeger, O’Cleirigh, Skeer, Mayer, & Safren, 2012; Waddell & Messeri, 2006; Zuniga, Yoo-Jeong, Dai, Guo, & Waldrop-Valverde, 2016); 13 were cross-sectional (Conover & Whetten-Goldstein, 2002; Du Bois & McKirnan, 2012; Gardner et al., 2002; Hightow-Weidman et al., 2017; Hussen, Harper, Bauermeister, Hightow-Weidman, & Adolescent Medicine Trials Network for HIV/AIDS Interventions, 2015; Leserman et al., 2005; Meade, Hansen, Kochman, & Sikkema, 2009; Saint-Jean et al., 2011; Schafer et al., 2012; Siddiqui, Bell, Sangi-Haghpeykar, Minard, & Levison, 2014; Tobias et al., 2007; van Servellen, Chang, Garcia, & Lombardi, 2002; Wohl et al., 2011); and ten were retrospective (Bofill, Waldrop-Valverde, Metsch, Pereyra, & Kolber, 2011; Colasanti, Stahl, Farber, Del Rio, & Armstrong, 2017; Giordano, Hartman, Gifford, Backus, & Morgan, 2009; Jones, Cook, Rodriguez, & Waldrop-Valverde, 2013; Rana, Gillani, Flanigan, Nash, & Beckwith, 2010; Rana et al., 2015; Rao et al., 2013; Ulett et al., 2009; Wawrzyniak et al., 2015; Yehia et al., 2015). The most common MH variables examined were depression (21 studies), followed by any psychiatric disorder (12 studies), and stress (eight studies) (Table 1). Various methods were used to measure retention in care, including visit constancy (eight studies), kept visits (21 studies), no-show rates (five studies), and gaps in care (two studies). The majority of studies were conducted with adults (31 studies); four studies included youth aged 12–24 years; three studies targeted males; and five targeted females. Further, more studies were conducted in the U.S. South (15 studies) than other U.S. regions, and three studies provided data from a nationally representative sample.
Table 1.
Meta-Analysis Examining the Association Between Mental Health Diagnosis or Symptoms and Retention in HIV Care (35 Studies), Stratified by Mental Health Type
| Variable | Effects (k) | Odds ratio | 95% CI | p-value | I2 (%) |
|---|---|---|---|---|---|
| Mental health variable | |||||
| Anxiety | 2 | 0.69 | 0.23–2.05 | 0.50 | 66.9 |
| Bipolar | 1 | 0.86 | 0.23–3.21 | 0.82 | NA |
| Depression | 19 | 0.88 | 0.80–0.97 | 0.01 | 68.9 |
| Mood disorder | 5 | 1.09 | 0.78–1.51 | 0.61 | 84.6 |
| Mental health composite score | 3 | 1.01 | 0.94–1.08 | 0.86 | 10.1 |
| Psychiatric disorder | 11 | 0.88 | 0.71–1.09 | 0.25 | 83.1 |
| Posttraumatic stress disorder | 4 | 1.08 | 0.89–1.31 | 0.44 | 0.0 |
| Stress | 7 | 0.92 | 0.82–1.03 | 0.15 | 72.0 |
| Overall | 52 | 0.94 | 0.90–0.99 | 0.01 | 71.9 |
CI = confidence interval.
Meta-Analysis
Of the 39 studies that reported on MH diagnoses or symptoms, 35 studies (52 effects) reported an effect size that could be summarized. Overall, a significant association existed between MH diagnoses or symptoms and retention in HIV care (OR = 0.94; 95% CI = 0.90–0.99) (Z = −2.58; p = 0.01) (Figure 2). The effect was heterogeneous (Q46 = 181.6; p <0.001; I2 = 71.9%). When the data were stratified on the basis of type of MH diagnoses or symptoms depression was significantly related to retention in HIV care (OR = 0.88; 95% CI = 0.80–0.97), whereas other diagnosis categories were not significantly related (Table 1). There was no statistically significant difference in the size of the relationship among types of mental health diagnoses or symptoms and retention in care (QB = 7.86; p = 0.35).
Figure 2.
Forest plot for the random effects meta-analysis examining the association between mental health diagnosis or symptoms and retention in HIV care. Effects are categorized by mental health variable type.
CI: Confidence Interval; PTSD: Posttraumatic stress disorder; MCS: Mental health composite score
Four studies (Du Bois & McKirnan, 2012; Hussen et al., 2015; Rana et al., 2010; van Servellen et al., 2002) did not provide an effect size that could be summarized and were qualitatively synthesized. Three of these four studies (Du Bois & McKirnan, 2012; Hussen et al., 2015; Rana et al., 2010) reported non-significant findings regarding the association between MH diagnoses or symptoms and retention in HIV care, but those studies did not provide an effect size or the direction of the effect. One study (van Servellen et al., 2002) examined anxiety and depression symptoms by using the Hospital Anxiety and Depression Scale (Zigmond & Snaith, 1983). Van Servellen et al. (2002) reported that persons not retained in HIV care, determined by clinical chart review, had a mean depression score within the normal range and a mean anxiety score in the borderline clinical range.
Moderator Analysis
Subgroup analysis and meta-regression were performed to determine whether the association between MH diagnoses or symptoms and retention in HIV care were modified by population- or study-level characteristics (Table 2). Age, sex, race/ethnicity, sexual orientation, substance abuse status, education, measurement of MH status, and type of MH diagnosis did not significantly modify the overall effect estimate. Public health insurance status (β = 0.004; Z = 3.47; p = 0.001) significantly modified the association between MH diagnoses or symptoms and retention in HIV care. In the subgroup analysis, no significant differences in the effect estimates were observed when effects were stratified by study design, mental health measurement, study quality, retention assessment period, or retention in care measurement.
Table 2.
Association Between Mental Health Diagnosis or Symptoms (35 Studies) or Mental Health Service Utilization (12 Studies) and Retention in Care Across Groups, Including Meta-Regression and Stratified Analysis Presented for Each Population and Study-Level Characteristic
| Population characteristic | Mental health diagnosis or symptoms | Mental health service utilization | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of studies | Effects (k) | β-coefficient | Standard error | Z-value | p-value | Effects (k) | β-coefficient | Standard error | Z-value | p-value | |
| Meta-regression analysis | |||||||||||
| Mean age | 24 | 35 | −0.007 | 0.004 | −1.57 | 0.12 | 8 | −0.02 | 0.06 | −0.31 | 0.75 |
| Percentage male | 35 | 52 | 0.0002 | 0.001 | 0.27 | 0.79 | 12 | −0.02 | 0.009 | −1.80 | 0.07 |
| Percentage black | 32 | 49 | 0.001 | 0.001 | 1.08 | 0.28 | 12 | 0.004 | 0.006 | 0.66 | 0.51 |
| Percentage MSM | 16 | 25 | 0.001 | 0.001 | 0.50 | 0.62 | 7 | 0.005 | 0.01 | 0.55 | 0.58 |
| Percentage using illegal substances | 28 | 44 | −0.0003 | 0.001 | −0.22 | 0.83 | 11 | −0.005 | 0.006 | −0.85 | 0.40 |
| Percentage with high school education or less | 19 | 32 | −0.003 | 0.002 | −1.53 | 0.12 | 7 | 0.005 | 0.01 | 0.37 | 0.71 |
| Percentage on public health insurance | 17 | 26 | 0.004 | 0.001 | 3.47 | 0.001* | 9 | 0.01 | 0.01 | 1.28 | 0.20 |
| Mental health diagnosis or symptoms | Mental health service utilization | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. in study | Effects (k) | Odds ratio | 95% CI | I2 | QB | p-value | Effects (k) | Odds ratio | 95% CI | I2 | QB | p-value | |
| Random effects meta-analysis and stratified analysis | |||||||||||||
| Overall | 35 | 52 | 0.94 | 0.90–0.99 | 71.9 | — | — | 12 | 1.84 | 1.45–2.33 | 84.8 | ||
| Mental health variable | 1.57 | 0.21 | — | — | |||||||||
| Depression | 19 | 19 | 0.88 | 0.80–0.97 | 68.9 | — | — | — | — | — | — | ||
| Other mental health diagnosis or symptoms | 24 | 33 | 0.95 | 0.89–1.02 | 74.1 | — | — | — | — | — | — | ||
| Mental health measurement | 0.54 | 0.46 | — | — | |||||||||
| Diagnostic - interview | 14 | 18 | 0.89 | 0.74–1.08 | 82.7 | — | — | — | — | — | — | ||
| Self-report | 23 | 34 | 0.96 | 0.92–1.00 | 59.6 | — | — | — | — | — | — | ||
| Study quality | 4.55 | 0.10 | 2.33 | 0.31 | |||||||||
| Good | 14 | 18 | 0.98 | 0.88–1.10 | 74.5 | 3 | 1.65 | 1.05–2.60 | 51.0 | ||||
| Fair | 19 | 31 | 0.93 | 0.88–0.97 | 72.7 | 8 | 1.97 | 1.45–2.67 | 89.5 | ||||
| Poor | 2 | 3 | 0.55 | 0.31–0.95 | 0 | 1 | 0.81 | 0.26–2.54 | NA | ||||
| Study design | 4.82 | 0.09 | 0.72 | 0.70 | |||||||||
| Prospective | 15 | 20 | 0.86 | 0.76–0.97 | 78.2 | 4 | 1.50 | 1.29–1.75 | 32.9 | ||||
| Cross-sectional | 11 | 20 | 0.99 | 0.95–1.04 | 59.2 | 6 | 1.96 | 1.07–3.58 | 88.3 | ||||
| Retrospective | 9 | 12 | 0.98 | 0.81–1.17 | 66.1 | 2 | 1.55 | 0.66–3.63 | 60.7 | ||||
| Retention Assessment Period | 7.77 | 0.17 | 4.20 | 0.52 | |||||||||
| ≥1 visit/6 mos. | 4 | 7 | 1.14 | 0.80–1.61 | 57.7 | 3 | 2.89 | 1.07–7.82 | 94.2 | ||||
| ≥2 visits/6 mos. | 6 | 9 | 0.91 | 0.82–1.01 | 75.7 | 1 | 1.56 | 1.26–1.94 | NA | ||||
| ≥2 visits/12 mos. | 12 | 17 | 0.96 | 0.89–1.03 | 27.7 | 4 | 1.41 | 0.83–2.40 | 63.1 | ||||
| ≥3 visits/12 mos. | 4 | 7 | 0.91 | 0.85–0.97 | 0 | 1 | 0.81 | 0.26–2.54 | NA | ||||
| ≥4 visits/12 mos. | 6 | 9 | 0.72 | 0.56–0.94 | 40.7 | 2 | 2.88 | 0.80–10.37 | 65.8 | ||||
| ≥4 visits/24 mos. | 3 | 3 | 1.25 | 0.79–1.98 | 97.0 | 1 | 1.46 | 1.36–1.57 | NA | ||||
| Retention in Care Measurement | 2.76 | 0.43 | 1.19 | 0.27 | |||||||||
| Kept Visits | 17 | 27 | 0.93 | 0.88–0.98 | 73.5 | 7 | 2.04 | 1.44–2.88 | 90.6 | ||||
| Visit Constancy | 11 | 15 | 0.94 | 0.81–1.10 | 70.7 | 5 | 1.57 | 1.14–2.15 | 53.6 | ||||
| Gap in care | 2 | 2 | 1.13 | 0.88–1.45 | 80.7 | — | — | — | — | ||||
| No-show rates | 5 | 8 | 0.91 | 0.86–0.97 | 0 | — | — | — | — | ||||
Mos.: months; QB = between groups effect; k = number of effects; MSM = men who have sex with men.
The number of effects (k) for mental health service utilization is equal to the number of studies.
p ≤ 0.05
Sensitivity Analysis and Publication Bias
Eleven studies (Dietz et al., 2010; Hightow-Weidman et al., 2017; Kushel et al., 2006; Meade et al., 2009; Mellins et al., 2003; Outlaw et al., 2010; Rao et al., 2013; Saint-Jean et al., 2011; Schafer et al., 2012; Traeger et al., 2012; Yehia et al., 2015) contributed multiple effect estimates to the summary effect. Sensitivity analysis was first conducted by including only one MH variable effect per study; the association between MH diagnoses or symptoms and retention in HIV care remained significant (OR = 0.95; 95% CI = 0.90–0.99; p = 0.03). A second sensitivity analysis was conducted to determine the impact of removal of one study at a time from the summary effect estimate; the overall effect estimate remained similar and significant, except for removal of one study (OR = 0.96; 95% CI = 0.92–1.00; p = 0.06) (Ashman et al., 2002). Ashman et al. (2002) had the largest sample size, compared with all other studies. No evidence was identified of publication bias, on the basis of visual inspection of the funnel plot and Begg test (Z = 0.02; p = 0.99). The fail-safe N was 135.
MHSU and Retention in HIV Care
Characteristics of Included Studies
Fourteen studies examined the association between MHSU and retention in HIV care. Among the included studies six were prospective studies (Aidala et al., 2007; Ashman et al., 2002; Magnus, Schmidt, Brown, & Kissinger, 2002; Messeri, Abramson, Aidala, Lee, & Lee, 2002; Naar-King et al., 2007; Waddell & Messeri, 2006); six were cross-sectional studies (Colasanti et al., 2017; Conover & Whetten-Goldstein, 2002; Lo, MacGovern, & Bradford, 2002; Meade et al., 2009; Mitchell et al., 2017; Tobias et al., 2007); and two were retrospective cohort studies (Rao et al., 2013; Sherer et al., 2002). MHSU was accessed through ancillary services in nine studies and through outpatient services in four. Retention was assessed by visit constancy (six studies), kept visits (seven studies), and gaps in care (one study). The majority of studies included adults (nine studies); three studies included youth; and two studies provided data from a nationally representative sample. Six studies examining MHSU were located in the Northeast; three were conducted in the South; and three were conducted in the Midwest.
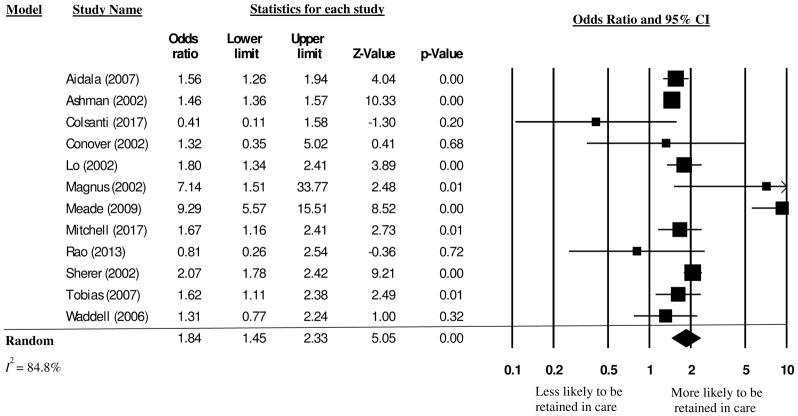
Meta-Analysis
Overall, a significant association existed between MHSU and retention in HIV care (OR = 1.84; 95% CI = 1.45–2.33) (Z = 5.05; p < 0.001) (Figure 3). The Q test and I2 indicated heterogeneity among studies that assessed the association between MHSU and retention in HIV care (Q10= 72.3; p < 0.001; I2 = 84.8 %).
Figure 3.
Forest plot for the random effects meta-analysis examining the association between mental health service usage and retention in HIV care.
CI: Confidence Interval
Two additional studies (Messeri et al., 2002; Naar-King et al., 2007) did not provide an effect size that could be summarized and were qualitatively synthesized. Naar-King et al. (2007) reported that the provision of counseling services was significantly associated with fewer gaps in retention in HIV care. Similarly, Messeri et al. (2002) determined that MHSU improved retention in HIV care (OR = 1.5), although the association was not statistically significant.
Moderator Analysis
Subgroup analysis and meta-regression were performed to determine whether the association between MHSU and retention in HIV care were modified by population- or study-level characteristics (Table 2). Age, sex, race, sexual orientation, substance abuse status, education, and health insurance status did not significantly modify the association between MHSU and retention in HIV care. In the subgroup analysis, no significant differences existed in the overall effect estimate when effects were stratified by study design or retention assessment period.
Sensitivity Analysis and Publication Bias
A sensitivity analysis was conducted by first removing outlying effects (Magnus et al., 2002; Meade et al., 2009). Magnus et al. (2002) was the only study conducted among young children (newborn–age 13 years); it assessed MHSU and retention in HIV care by using data obtained regarding children aged ≥1 year from pediatric medical databases. Meade et al. (2009) assessed baseline data collected as part of a clinical trial of a group-coping intervention for HIV-positive adults who had experienced sexual abuse before age 18 years. The majority of participants (99%) in the Meade et al. study were enrolled in HIV medical treatment. After the two effects (Magnus et al., 2002; Meade et al., 2009) were removed, the effect size decreased slightly but remained statistically significant (OR = 1.61; 95% CI = 1.38–1.87) (Z = 6.22; p <0.001). Additionally, the heterogeneity statistic decreased (Q10 = 22.7; p = 0.007; I2 = 60.3%) but remained >50%. Secondly, a sensitivity analysis was conducted by removal of one study, which did not significantly change the effect estimate examining MHSU and retention in HIV care. The effect estimates changed slightly and ranged from OR = 1.62 (95% CI = 1.39–1.90) to OR = 1.91 (95% CI = 1.51–2.42). Removal of studies with a smaller sample size (Magnus et al., 2002; Meade et al., 2009) resulted in a smaller overall effect estimate, and removal of larger studies resulted in a larger overall effect estimate. No evidence of publication bias was detected on the basis of visual inspection of the funnel plot and Begg test (z = 0.55; p = 0.58). Fail-safe N was 480.
Quality Assessment
The quality scores for each study are provided in Appendix F. The most common limitations among studies were exposure being assessed before the outcome measurement; lack of a sufficient time frame to measure an effect; and repeated exposure of assessment. Sample size justification and blinding of the outcome measurement were not determined to apply to the majority of the included studies. Similarly, because the majority of studies were cross-sectional or retrospective, loss to follow-up was also not applicable. Overall, we determined that the quality of evidence was fair because the majority of studies were cross-sectional or retrospective cohort design that did not account for confounders. In the subgroup analysis for MH diagnoses or symptoms and retention in HIV care (Table 2), studies that were rated poor had a larger effect estimate, compared with good and fair studies. However, study quality was not statistically significantly different across levels (QB = 4.55; p = 0.10).
Discussion
The results of this study demonstrate that having MH diagnoses or symptoms is statistically significantly associated with lower odds of being retained in HIV care and are consistent with multiple quantitative and qualitative primary studies (Holtzman, Shea, et al., 2015; Sprague & Simon, 2014) that report poor MH is a salient barrier to retention in care. The present study attempted to examine specific types of MH diagnoses or symptoms and identify statistically significant modifiers of the association between MH and retention in care. Unfortunately, few studies reported on specific MH diagnoses or symptoms (e.g., anxiety or bipolar disorder) other than depression. However, depression was identified as statistically related to lower odds of being retained in HIV care. Although MH diagnoses or symptoms were a barrier to retention in HIV care, these results also reveal that increased MHSU was associated with higher odds of being retained in HIV care. The clinical implications of this study are that persons with HIV who are treated for their MH diagnoses or symptoms might have better HIV clinical outcomes than those whose MH diagnoses or symptoms remain untreated. Current HIV prevention strategies, such as ‘test-and-treat’ (Cambiano, Rodger, & Phillips, 2011; Cohen et al., 2016) and ‘treatment as prevention’(Centers for Disease Control and Prevention, 2017a), emphasize ART medication as key components. The results of this study suggest that the clinical treatment of HIV may need also to address mental health for patients to achieve optimal HIV outcomes, including retention in care. If persons living with HIV are retained in care, they more likely to be virally suppressed (Centers for Disease Control and Prevention, 2017c).
Use of ancillary services (e.g., MH treatment) has been previously reported to improve retention in HIV care by addressing the complex health care needs of persons who have multiple diagnoses (Conover & Whetten-Goldstein, 2002). This is the first systematic review to quantitatively examine the association between MHSU and retention in HIV care. The results of this review examining correlational studies demonstrated a larger association between MHSU and retention in HIV care than reports of intervention studies examining MH interventions (e.g., cognitive behavior therapy or motivational interviewing) (Crepaz et al., 2008; Mbuagbaw, Ye, & Thabane, 2012). Previous studies have demonstrated that the benefits of MHSU in PLWH include improvements in CD4+ count and mortality outcomes (Blashill, Perry, & Safren, 2011). Recent evidence indicates the need for MH services continues to be unmet (DeGroote, Korhonen, Shouse, Valleroy, & Bradley, 2016; Korhonen et al., 2016), and in the case of HIV care, this can affect retention. Thus, more methods are needed for improving retention in HIV care among these populations, including provision of access to and support for MH services.
A small, negative association was observed between MH diagnoses and symptoms and retention in HIV care. Sensitivity analysis revealed that the association was no longer statistically significant after removing one study (Ashman et al., 2002) that had a larger effect size and the largest population of all included studies. However, the effect estimate remained fairly stable thus did not change the interpretation of the results. Multiple studies have demonstrated that patients with a MH diagnosis who are receiving MH care are 10%–40% more likely to be retained in HIV care, compared with patients whose need for MH services remains unmet (Himelhoch, Brown, et al., 2009; Himelhoch, Josephs, et al., 2009; Meade et al., 2009; Sherer et al., 2002; Weiser et al., 2006). Therefore, the small negative association between having MH diagnoses or symptoms and retention in HIV care might have been larger if the populations studied only included patients not receiving any MH services. The patients in the included studies who were suffering from MH diagnoses in this review might have received other ancillary services (e.g., substance abuse treatment) that are also likely to improve retention in HIV care (Lucas et al., 2010). Future research examining the association between MH diagnoses or symptoms and retention in HIV care can explore this association by accounting for MHSU.
In the moderator analysis, public health insurance was determined to modify the association between MH diagnoses or symptoms and retention in HIV care. Studies with a lower proportion of participants with public health insurance had lower rates of retention in HIV care, compared with studies with a higher percentage of public health–insured persons. Moreover, one study (Byrd et al., 2015) that examined only Medicaid-insured participants reported that 61% of the population was retained in HIV care and a MH diagnosis was related to fewer gaps in HIV care. The higher odds of being retained in care among publically insured populations with a MH diagnosis might be attributable to their ability to receive more follow-up, compared with uninsured populations. In addition to health insurance, study design was identified as a substantial moderator in that prospective studies observed a larger effect estimate, compared with retrospective and cross-sectional studies. When assessing the long-term effects of a MH diagnoses or symptoms on retention in HIV care, prospective study designs are able to assess this association temporally. Because retention is defined as extending over a period, examination of variables affecting retention in care longitudinally is needed (Horstmann et al., 2010). Lastly, in the stratified analysis, no difference in effect size occurred when comparing studies that measured MH status by using diagnostic interview versus self-report assessments, which indicates that the association between retention in HIV care and MH is similar, regardless if it is a MH diagnosis or self-reported symptom. Furthermore, it might also indicate that self-reported assessment of MH symptoms with valid tools might be as useful as clinician assessments in identifying those in need of MH services while in HIV care.
This review had certain limitations. First, serious mental illness (e.g., schizophrenia or bipolar disorder) was not well-represented in the included studies; therefore, the results are not generalizable to all MH conditions. Further, the moderator analysis did not identify any factors that substantially reduced the heterogeneity. Therefore, other unidentified factors might account for the variation in the overall effect estimate. Few studies reported on a specific MH diagnoses other than depression, and the non-significant association between other types of MH diagnoses and retention may be due to lack of power. Moreover, the lack of power made it difficult to detect significant differences in the size of the relationship between retention and other types of mental health diagnoses or symptoms. Additionally, few studies reported subgroup data; therefore, this review was limited in assessing the association of MH and retention in HIV care across different populations and settings.
This review identified gaps in the literature, which limits generalizability to certain populations. Multiple studies examined black populations primarily; however, few studies examined other minority populations (e.g., Latinos or Hispanics). In addition, few studies specified the type of MH professionals providing the services, and only three studies were conducted in rural settings. Furthermore, although youth living with HIV suffer from high rates of mental illness (Mellins et al., 2009), few studies reported on that population. This review, however, did not find an effect of age on the association between MH diagnoses or symptoms or MHSU and retention in HIV care. Future research examining effects of MH on retention in HIV care and the benefit of MHSU on retention is needed among various MH diagnoses (e.g., generalized anxiety or bipolar disorder) and among specific populations (e.g., youth, Latinos, or Hispanics). Also needed are studies in rural settings and among different types of MH service deliverer (e.g., psychologist or social worker) because the associations might differ on the basis of these factors. Lastly, studies among general populations can provide stratified analyses to understand differences in association among certain subgroups.
Conclusion
The results of our study indicate that depression is statistically related to retention in care and that other types of MH diagnoses or symptoms need further examination (e.g., anxiety, bipolar disorder, and PTSD) in PLWH. To our knowledge, this is first meta-analysis to specifically identify public health insurance as a significant moderator of the association between mental health and retention in care. Although the effect of MH on retention in care was limited, few studies accounted for whether persons were concurrently receiving MH services. Future studies that investigate the role MH plays on retaining populations whose need for MH services remain unmet (i.e., have underutilization of MH services) will aid in identifying the importance of MH care for HIV outcomes. Moreover, results of this study demonstrate the need for addressing barriers to MH treatment in interventions focused on improving retention in care because mental health treatment is a strong facilitator of retention in HIV care.
Supplementary Material
Acknowledgments
We thank members of the Prevention Research Synthesis team for their contribution to the PRS database, including Terrika Barham, Jeff Becasen, Julia DeLuca, and Emiko Kamitani. The work of Rebecca Ramshaw was supported by the Emory University Rollins Earn and Learn (REAL) internship program.
Footnotes
Disclaimer: Findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Contributor Information
Cherie R. Rooks-Peck, Division of HIV/AIDS Prevention, Centers for Disease Control and Prevention
Adebukola H. Adegbite, ICF International
Megan E. Wichser, ICF International
Rebecca Ramshaw, Emory University, Division of HIV/AIDS, Centers for Disease Control and Prevention.
Mary M. Mullins, Division of HIV/AIDS Prevention, Centers for Disease Control and Prevention
Darrel Higa, Division of HIV/AIDS Prevention, Centers for Disease Control and Prevention.
Theresa Ann Sipe, Division of HIV/AIDS Prevention, Centers for Disease Control and Prevention.
the Prevention Research Synthesis Project, Division of HIV/AIDS Prevention, Centers for Disease Control and Prevention.
References
*An asterisk indicates an included study.
- *.Aidala AA, Lee G, Abramson DM, Messeri P, Siegler A. Housing need, housing assistance, and connection to HIV medical care. AIDS and Behavior. 2007;11:S101–S115. doi: 10.1007/s10461-007-9276-x. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®) American Psychiatric Pub; 2013. [Google Scholar]
- *.Ashman JJ, Conviser R, Pounds MB. Associations between HIV-positive individuals’ receipt of ancillary services and medical care receipt and retention. AIDS Care. 2002;14:S109–S118. doi: 10.1080/09540120220149993a. [DOI] [PubMed] [Google Scholar]
- Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. [PubMed] [Google Scholar]
- Blashill AJ, Perry N, Safren SA. Mental health: A focus on stress, coping, and mental illness as it relates to treatment retention, adherence, and other health outcomes. Current HIV/AIDS Reports. 2011;8:215–222. doi: 10.1007/s11904-011-0089-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Bofill L, Waldrop-Valverde D, Metsch L, Pereyra M, Kolber M. Demographic and psychosocial factors associated with appointment attendance among HIV-positive outpatients. AIDS Care. 2011;23:1219–1225. doi: 10.1080/09540121.2011.555743. [DOI] [PubMed] [Google Scholar]
- Borenstein M, Hedges L, Higgins J, Rothstein H. Comprehensive meta-analysis (version 2) [Software] 2005 Retrieved from [ http://www.meta-analysis.com]
- *.Buchberg MK, Fletcher FE, Vidrine DJ, Levison J, Peters MY, Hardwicke R, … Bell TK. A mixed-methods approach to understanding barriers to postpartum retention in care among low-income, HIV-infected women. AIDS Patient Care and STDs. 2015;29:126–132. doi: 10.1089/apc.2014.0227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Byrd KK, Furtado M, Bush T, Gardner L. Evaluating patterns in retention, continuation, gaps, and re-engagement in HIV care in a Medicaid-insured population, 2006 – 2012, United States. AIDS Care. 2015;27:1387–1395. doi: 10.1080/09540121.2015.1114991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cambiano V, Rodger AJ, Phillips AN. ‘Test-and-treat’: the end of the HIV epidemic? Curr Opin Infect Dis. 2011;24:19–26. doi: 10.1097/QCO.0b013e3283422c8c. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. HIV Treatment as Prevention. 2017a Retrieved from https://www.cdc.gov/hiv/risk/art/index.html.
- Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas, 2015. HIV Surveillance Supplemental Report. 2017b;22(2) from http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. [Google Scholar]
- Centers for Disease Control and Prevention. Selected National HIV Prevention and Care Outcomes in the United States. 2017c Retrieved from https://www.cdc.gov/hiv/pdf/library/factsheets/cdc-hiv-national-hiv-care-outcomes.pdf.
- Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, … Fleming TR. Antiretroviral Therapy for the Prevention of HIV-1 Transmission. N Engl J Med. 2016;375:830–839. doi: 10.1056/NEJMoa1600693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Colasanti J, Stahl N, Farber EW, Del Rio C, Armstrong WS. An Exploratory Study to Assess Individual and Structural Level Barriers Associated With Poor Retention and Re-engagement in Care Among Persons Living With HIV/AIDS. J Acquir Immune Defic Syndr. 2017;74(Suppl 2):S113–s120. doi: 10.1097/qai.0000000000001242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Conover CJ, Whetten-Goldstein K. The impact of ancillary services on primary care use and outcomes for HIV/AIDS patients with public insurance coverage. AIDS Care. 2002;14:S59–S71. doi: 10.1080/09540120220149957. [DOI] [PubMed] [Google Scholar]
- Crepaz N, Passin WF, Herbst JH, Rama SM, Malow RM, Purcell DW … and the HIVAPRST. Meta-analysis of cognitive-behavioral interventions on HIV-positive persons’ mental health and immune functioning. Health Psychology. 2008;27:4–14. doi: 10.1037/0278-6133.27.1.4. [DOI] [PubMed] [Google Scholar]
- *.Dang BN, Westbrook RA, Hartman CM, Giordano TP. Retaining HIV Patients in Care: The Role of Initial Patient Care Experiences. AIDS Behav. 2016;20:2477–2487. doi: 10.1007/s10461-016-1340-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeGroote NP, Korhonen LC, Shouse RL, Valleroy LA, Bradley H. Unmet needs for ancillary services among men who have sex with men and who are receiving HIV medical care - United States, 2013–2014. MMWR Morb Mortal Wkly Rep. 2016;65:1004–1007. doi: 10.15585/mmwr.mm6537a4. [DOI] [PubMed] [Google Scholar]
- *.Dietz E, Clum GA, Chung SE, Leonard L, Murphy DA, Perez LV, … Ellen JM. Adherence to scheduled appointments among HIV-infected female youth in five U.S. cities. Journal of Adolescent Health. 2010;46:278–283. doi: 10.1016/j.jadohealth.2009.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Du Bois SN, McKirnan DJ. A longitudinal analysis of HIV treatment adherence among men who have sex with men: A cognitive escape perspective. AIDS Care. 2012;24:1425–1431. doi: 10.1080/09540121.2011.650676. [DOI] [PubMed] [Google Scholar]
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evidence Partners. DistillerSR (Version 2) [Software] 2016 Retrieved from https://v2.systematic-review.ca.
- *.Gardner LI, Holmberg SD, Moore J, Arnsten JH, Mayer KH, Rompalo A … Group, H. I. V. E. R. S. Use of highly active antiretroviral therapy in HIV-infected women: Impact of HIV specialist care. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2002;29:69–75. doi: 10.1097/00126334-200201010-00010. [DOI] [PubMed] [Google Scholar]
- *.Giordano TP, Hartman C, Gifford AL, Backus LI, Morgan RO. Predictors of retention in HIV care among a national cohort of US veterans. HIV Clinical Trials. 2009;10:299–305. doi: 10.1310/hct1005-299. [DOI] [PubMed] [Google Scholar]
- Gonzalez JS, Batchelder AW, Psaros C, Safren SA. Depression and HIV/AIDS treatment nonadherence: A review and meta-analysis. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2011;58:181–187. doi: 10.1097/QAI.0b013e31822d490a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Resources and Services Administration. HRSA CARE ACTION: Impact of Mental Illness on People Living with HIV. 2015 Retrieved from http://hab.hrsa.gov/deliverhivaidscare/mentalhealth.pdf.
- Hedges LV, Olkin I. Statistical methods for meta-analysis. Orlando: Academic press; 2014. [Google Scholar]
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Hightow-Weidman L, LeGrand S, Choi SK, Egger J, Hurt CB, Muessig KE. Exploring the HIV continuum of care among young black MSM. PLoS One. 2017;12:e0179688. doi: 10.1371/journal.pone.0179688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himelhoch S, Brown CH, Walkup J, Chander G, Korthius PT, Afful J, Gebo KA. HIV patients with psychiatric disorders are less likely to discontinue HAART. AIDS. 2009;23:1735–1742. doi: 10.1097/QAD.0b013e32832b428f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himelhoch S, Josephs JS, Chander G, Korthuis PT, Gebo KA, Network HIVR. Use of outpatient mental health services and psychotropic medications among HIV-infected patients in a multisite, multistate study. General Hospital Psychiatry. 2009;31:538–545. doi: 10.1016/j.genhosppsych.2009.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtzman CW, Brady KA, Yehia BR. Retention in care and medication adherence: Current challenges to antiretroviral therapy success. Drugs. 2015;75:445–454. doi: 10.1007/s40265-015-0373-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtzman CW, Shea JA, Glanz K, Jacobs LM, Gross R, Hines J, … Yehia BR. Mapping patient-identified barriers and facilitators to retention in HIV care and antiretroviral therapy adherence to Andersen’s Behavioral Model. AIDS Care. 2015;27:817–828. doi: 10.1080/09540121.2015.1009362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horstmann E, Brown J, Islam F, Buck J, Agins BD. Retaining HIV-infected patients in care: Where are we? Where do we go from here? Clinical Infectious Diseases. 2010;50:752–761. doi: 10.1086/649933. [DOI] [PubMed] [Google Scholar]
- *.Hussen SA, Harper GW, Bauermeister JA, Hightow-Weidman LB Adolescent Medicine Trials Network for HIV/AIDS Interventions. Psychosocial influences on engagement in care among HIV-positive young black gay/bisexual and other men who have sex with men. AIDS Patient Care and STDs. 2015;29:77–85. doi: 10.1089/apc.2014.0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Jacks A, Wainwright D, Salazar L, Grimes R, York M, Strutt AM, … Hasbun R. Neurocognitive deficits increase risk of poor retention in care among older adults with newly diagnosed HIV infection. AIDS. 2015;29:1711–1714. doi: 10.1097/QAD.0000000000000700. [DOI] [PubMed] [Google Scholar]
- *.Jones D, Cook R, Rodriguez A, Waldrop-Valverde D. Personal HIV knowledge, appointment adherence and HIV outcomes. AIDS and Behavior. 2013;17:242–249. doi: 10.1007/s10461-012-0367-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korhonen LC, DeGroote NP, Shouse RL, Valleroy LA, Prejean J, Bradley H. Unmet needs for ancillary services among hispanics/latinos receiving HIV medical care - United States, 2013–2014. MMWR Morb Mortal Wkly Rep. 2016;65:1104–1107. doi: 10.15585/mmwr.mm6540a3. [DOI] [PubMed] [Google Scholar]
- *.Kushel MB, Colfax G, Ragland K, Heineman A, Palacio H, Bangsberg DR. Case management is associated with improved antiretroviral adherence and CD4+ cell counts in homeless and marginally housed individuals with HIV infection. Clinical Infectious Diseases. 2006;43:234–242. doi: 10.1086/505212. [DOI] [PubMed] [Google Scholar]
- Langebeek N, Gisolf EH, Reiss P, Vervoort SC, Hafsteinsdottir TB, Richter C, … Nieuwkerk PT. Predictors and correlates of adherence to combination antiretroviral therapy (ART) for chronic HIV infection: a meta-analysis. BMC Med. 2014;12:142. doi: 10.1186/preaccept-1453408941291432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Leserman J, Whetten K, Lowe K, Stangl D, Swartz MS, Thielman NM. How trauma, recent stressful events, and PTSD affect functional health status and health utilization in HIV-infected patients in the South. Psychosomatic Medicine. 2005;67:500–507. doi: 10.1097/01.psy.0000160459.78182.d9. [DOI] [PubMed] [Google Scholar]
- *.Lo W, MacGovern T, Bradford J. Association of ancillary services with primary care utilization and retention for patients with HIV/AIDS. AIDS Care. 2002;14:S45–S57. doi: 10.1080/0954012022014992049984. [DOI] [PubMed] [Google Scholar]
- Lucas GM, Chaudhry A, Hsu J, Woodson T, Lau B, Olsen Y, … Moore RD. Clinic-based treatment of opioid-dependent HIV-infected patients versus referral to an opioid treatment program: A randomized trial. Annals of Internal Medicine. 2010;152:704–711. doi: 10.1059/0003-4819-152-11-201006010-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Magnus M, Schmidt N, Brown B, Kissinger PJ. A profile of an HIV− and child-specific programme in New Orleans, Louisiana, USA. AIDS Care. 2002;14:S85–S94. doi: 10.1080/09540120220149966. [DOI] [PubMed] [Google Scholar]
- Mbuagbaw L, Ye C, Thabane L. Motivational interviewing for improving outcomes in youth living with HIV. Cochrane Database Syst Rev. 2012:Cd009748. doi: 10.1002/14651858.CD009748.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Meade CS, Hansen NB, Kochman A, Sikkema KJ. Utilization of medical treatments and adherence to antiretroviral therapy among HIV-positive adults with histories of childhood sexual abuse. AIDS Patient Care and STDs. 2009;23:259–266. doi: 10.1089/apc.2008.0210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Mellins CA, Brackis-Cott E, Leu CS, Elkington KS, Dolezal C, Wiznia A, … Abrams EJ. Rates and types of psychiatric disorders in perinatally human immunodeficiency virus-infected youth and seroreverters. J Child Psychol Psychiatry. 2009;50:1131–1138. doi: 10.1111/j.1469-7610.2009.02069.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellins CA, Kang E, Leu C, Havens JF, Chesney MA. Longitudinal study of mental health and psychosocial predictors of medical treatment adherence in mothers living with HIV disease. AIDS Patient Care and STDs. 2003;17:407–416. doi: 10.1089/108729103322277420. [DOI] [PubMed] [Google Scholar]
- *.Merlin JS, Westfall AO, Raper JL, Zinski A, Norton WE, Willig JH, … Mugavero MJ. Pain, mood, and substance abuse in HIV: Implications for clinic visit utilization, antiretroviral therapy adherence, and virologic failure. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2012;61:164–170. doi: 10.1097/QAI.0b013e3182662215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Messeri PA, Abramson DM, Aidala AA, Lee F, Lee G. The impact of ancillary HIV services on engagement in medical care in New York City. AIDS Care. 2002;14:S15–S29. doi: 10.1080/09540120220149948. [DOI] [PubMed] [Google Scholar]
- *.Minniear TD, Gaur AH, Thridandapani A, Sinnock C, Tolley EA, Flynn PM. Delayed entry into and failure to remain in HIV care among HIV-infected adolescents. AIDS Research and Human Retroviruses. 2013;29:99–104. doi: 10.1089/AID.2012.0267. [DOI] [PubMed] [Google Scholar]
- *.Mitchell MM, Nguyen TQ, Isenberg SR, Maragh-Bass AC, Keruly J, Knowlton AR. Psychosocial and Service Use Correlates of Health-Related Quality of Life Among a Vulnerable Population Living with HIV/AIDS. AIDS Behav. 2017;21:1580–1587. doi: 10.1007/s10461-016-1589-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, … Stewart LA. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mugavero MJ, Westfall AO, Zinski A, Davila J, Drainoni ML, Gardner LI, … Giordano TP. Measuring retention in HIV care: the elusive gold standard. J Acquir Immune Defic Syndr. 2012;61:574–580. doi: 10.1097/QAI.0b013e318273762f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Naar-King S, Green M, Wright A, Outlaw B, Wang B, Liu H. Ancillary services and retention of youth in HIV care. AIDS Care. 2007;19:248–251. doi: 10.1080/09540120600726958. [DOI] [PubMed] [Google Scholar]
- National Heart Lung Blood Institute (Producer) Quality assessment tool for observational cohort and cross-sectional studies. 2014 Retrieved from https://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/cohort.
- *.Outlaw A, Naar-King S, Green-Jones M, Wright K, Condon K, Sherry L, Janisse H. Brief report: Predictors of optimal HIV appointment adherence in minority youth: A prospective study. Journal of Pediatric Psychology. 2010;35:1011–1015. doi: 10.1093/jpepsy/jsq002. [DOI] [PubMed] [Google Scholar]
- Prevention Access Campaign. Risk of Sexual Transmission of HIV from a Person with HIV who has an Undetectable Viral Load: Messaging Primer & Consesus Statement. 2016 Retrieved from http://www.preventionaccess.org/consensus.
- *.Rana AI, Gillani FS, Flanigan TP, Nash BT, Beckwith CG. Follow-up care among HIV-infected pregnant women in Mississippi. Journal of Women’s Health. 2010;19:1863–1867. doi: 10.1089/jwh.2009.1880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Rana AI, Liu T, Gillani FS, Reece R, Kojic EM, Zlotnick C, Wilson IB. Multiple gaps in care common among newly diagnosed HIV patients. AIDS Care. 2015;27:679–687. doi: 10.1080/09540121.2015.1005002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Rao KC, Enriquez M, Gantt TC, Gerkovich MM, Bonham AJ, Griffin RG, Bamberger DM. Nonengagement in HIV care: A descriptive and qualitative study in hospitalized patients and community-based analysis. Journal of the International Association of Providers of AIDS Care. 2013;12:178–184. doi: 10.1177/2325957412472058. [DOI] [PubMed] [Google Scholar]
- Rosenberg MS. The file-drawer problem revisited: a general weighted method for calculating fail-safe numbers in meta-analysis. Evolution. 2005;59:464–468. [PubMed] [Google Scholar]
- *.Saint-Jean G, Metsch L, Gomez-Marin O, Pierre C, Jeanty Y, Rodriguez A, Malow R. Use of HIV primary care by HIV-positive Haitian immigrants in Miami, Florida. AIDS Care. 2011;23:486–493. doi: 10.1080/09540121.2010.516339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Schafer KR, Brant J, Gupta S, Thorpe J, Winstead-Derlega C, Pinkerton R, … Dillingham R. Intimate partner violence: A predictor of worse HIV outcomes and engagement in care. AIDS Patient Care and STDs. 2012;26:356–365. doi: 10.1089/apc.2011.0409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Schumacher JE, McCullumsmith C, Mugavero MJ, Ingle-Pang PE, Raper JL, Willig JH, … Saag MS. Routine depression screening in an HIV clinic cohort identifies patients with complex psychiatric co-morbidities who show significant response to treatment. AIDS Behav. 2013;17:2781–2791. doi: 10.1007/s10461-012-0342-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Sherer R, Stieglitz K, Narra J, Jasek J, Green L, Moore B, … Cohen M. HIV multidisciplinary teams work: Support services improve access to and retention in HIV primary care. AIDS Care. 2002;14:S31–S44. doi: 10.1080/09540120220149975. [DOI] [PubMed] [Google Scholar]
- *.Siddiqui R, Bell T, Sangi-Haghpeykar H, Minard C, Levison J. Predictive factors for loss to postpartum follow-up among low income HIV-infected women in Texas. AIDS Patient Care and STDs. 2014;28:248–253. doi: 10.1089/apc.2013.0321. [DOI] [PubMed] [Google Scholar]
- Sin NL, DiMatteo MR. Depression treatment enhances adherence to antiretroviral therapy: A meta-analysis. Annals of Behavioral Medicine. 2014;47:259–269. doi: 10.1007/s12160-013-9559-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soto TA, Bell J, Pillen MB. Literature on integrated HIV care: A review. AIDS Care. 2004;16:S43–S55. doi: 10.1080/09540120412331315295. [DOI] [PubMed] [Google Scholar]
- Sprague C, Simon SE. Understanding HIV care delays in the US South and the role of the social-level in HIV care engagement/retention: A qualitative study. International Journal for Equity in Health. 2014;13:28.14. doi: 10.1186/1475-9276-13-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson MA, Mugavero MJ, Amico KR, Cargill VA, Chang LW, … Gross R, et al. Guidelines for improving entry into and retention in care and antiretroviral adherence for persons with HIV: Evidence-based recommendations from an international association of physicians in AIDS care panel. Annals of Internal Medicine. 2012;156:817–833. doi: 10.7326/0003-4819-156-11-201206050-00419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Tobias CR, Cunningham W, Cabral HD, Cunningham CO, Eldred L, Naar-King S, … Drainoni ML. Living with HIV but without medical care: Barriers to engagement. AIDS Patient Care and STDs. 2007;21:426–434. doi: 10.1089/apc.2006.0138. [DOI] [PubMed] [Google Scholar]
- *.Traeger L, O’Cleirigh C, Skeer MR, Mayer KH, Safren SA. Risk factors for missed HIV primary care visits among men who have sex with men. Journal of Behavioral Medicine. 2012;35:548–556. doi: 10.1007/s10865-011-9383-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Ulett KB, Willig JH, Lin HY, Routman JS, Abroms S, Allison J, … Mugavero MJ. The therapeutic implications of timely linkage and early retention in HIV care. AIDS Patient Care and STDs. 2009;23:41–49. doi: 10.1089/apc.2008.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.van Servellen G, Chang B, Garcia L, Lombardi E. Individual and system level factors associated with treatment nonadherence in human immunodeficiency virus-infected men and women. AIDS Patient Care and STDs. 2002;16:269–281. doi: 10.1089/10872910260066705. [DOI] [PubMed] [Google Scholar]
- *.Waddell EN, Messeri P. Informal social support for HIV medical care. Journal of HIV/AIDS & Social Services. 2006;5:121–139. [Google Scholar]
- *.Wawrzyniak AJ, Rodriguez AE, Falcon AE, Chakrabarti A, Parra A, Park J, … Metsch LR. Association of individual and systemic barriers to optimal medical care in people living with HIV/AIDS in Miami-Dade County. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2015;69:S63–S72. doi: 10.1097/QAI.0000000000000572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiser SD, Riley ED, Ragland K, Hammer G, Clark R, Bangsberg DR. Brief report: Factors associated with depression among homeless and marginally housed HIV-infected men in San Francisco. Journal of General Internal Medicine. 2006;21:61–64. doi: 10.1111/j.1525-1497.2005.0282.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White House Office of National AIDS Policy. NATIONAL HIV/AIDS STRATEGY for the UNITED STATES: Updated to 2020. 2015 Retrieved from https://www.aids.gov/federal-resources/national-hiv-aids-strategy/nhas-update.pdf.
- *.Wohl AR, Galvan FH, Myers HF, Garland W, George S, Witt M, … Lee ML. Do social support, stress, disclosure and stigma influence retention in HIV care for Latino and African American men who have sex with men and women? AIDS and Behavior. 2011;15:1098–1110. doi: 10.1007/s10461-010-9833-6. [DOI] [PubMed] [Google Scholar]
- *.Yehia BR, Stephens-Shield AJ, Momplaisir F, Taylor L, Gross R, Dube B, … Brady KA. Health outcomes of HIV-infected people with mental illness. AIDS and Behavior. 2015;19:1491–1500. doi: 10.1007/s10461-015-1080-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- *.Zuniga JA, Yoo-Jeong M, Dai T, Guo Y, Waldrop-Valverde D. The Role of Depression in Retention in Care for Persons Living with HIV. AIDS Patient Care STDS. 2016;30:34–38. doi: 10.1089/apc.2015.0214. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.