Abstract
Moral injury refers to acts of commission or omission that violate individuals’ moral or ethical standards. Morally injurious events are often synonymous with psychological trauma, especially in combat situations; thus, morally injurious events are often implicated in the development of PTSD for military service members and veterans. Although Prolonged Exposure (PE) and Cognitive Processing Therapy (CPT) have been well-established as effective treatments for veterans who are struggling with posttraumatic stress disorder (PTSD), it has been suggested that these two evidence-based therapies may not be sufficient for treating veterans whose PTSD resulted from morally injurious events. The purpose of this manuscript is to detail how the underlying theories of PE and CPT can account for moral-injury based PTSD and to describe two case examples of veterans with PTSD stemming from morally injurious events who were successfully treated with PE and CPT. The manuscript concludes with a summary of challenges that clinicians may face when treating veterans with PTSD resulting from moral injury using either PE or CPT.
Keywords: Prolonged Exposure, Cognitive Processing Therapy, Treatment, Moral Injury, PTSD, Veterans, Case Study
Posttraumatic stress disorder (PTSD) affects approximately 23% of all Operation Enduring Freedom/Operation Iraqi Freedom service members and veterans (Fulton et al., 2015; Hoge, Riviere, Wilk, Herrell, & Weathers, 2014; Wisco et al., 2014). Given the large number of military personnel that are affected by traumatic events, researchers and clinicians have been interested in better understanding the complex and multifaceted nature of military trauma (e.g., Gray et al., 2012; Litz, Lebowitz, Gray & Nash, 2016; Stein et al., 2012). Researchers have begun to categorize traumatic experiences into three distinct categories: Fear-based trauma (e.g., fearing for losing one’s life in a firefight), loss-based trauma (e.g., losing a close friend in an explosion), and moral injury-based trauma (Gray et al., 2012; Litz, Lebowitz, Gray & Nash, 2016). Moral injury, or the violation of one’s deeply held moral or ethical standards, is often synonymous with psychological trauma (Litz et al., 2009).
One relatively common example of moral injury among post-9/11 service members and veterans is directly or indirectly causing or witnessing harm, injury, or death to innocent civilians while on deployment. In one survey study, Hoge and colleagues (2004) found that nearly ten percent of the sample of deployed soldiers and Marines endorsed responsibility for the death of non-combatants. Other examples of moral injury include disproportionate violence, violence within ranks, and betrayal, to name a few (Drescher et al., 2011). In response to participating in or witnessing potentially morally injurious events, such as the examples above, service members and veterans tend to experience a wide range of emotions, including guilt, shame, sadness, anger, humiliation, and numbness (Litz et al., 2009; Stein et al., 2012). When the diagnostic criteria for PTSD are met, this phenomenon can be referred to as moral injury-based PTSD.
While similar emotional reactions can be observed in individuals with PTSD based on loss and fear, the presence of moral injury is believed to further intensify feelings of guilt and shame, complicate the forgiveness process, and interfere with recovery (Bryan, Ray-Sannerud, Morrow, & Etienne, 2013; Currier, Holland, & Malott, 2015; Litz et al., 2009). Although the aforementioned cycle may resemble one model describing the development and maintenance of PTSD (e.g., Ehlers & Clark, 2000), some have suggested that moral injury-based PTSD may be characterized by more intense re-experiencing and less intense hyperarousal symptoms compared to fear- or loss-based PTSD (Gray et al., 2012; Litz et al., 2009). Because of the potential differences between fear- or loss-based PTSD and moral injury-based PTSD, there have been discussions about the effectiveness of existing evidence-based therapies for PTSD when treating service members and veterans who are struggling with moral injury-based PTSD (Gray et al., 2012; Litz, Lebowitz, Gray, & Nash, 2016; Steenkamp, Litz, Hoge, & Marmar, 2015). Both the Veteran’s Administration (VA) and the Department of Defense (DoD) guidelines endorse two cognitive behavioral therapies, Prolonged Exposure (PE) and Cognitive Processing Therapy (CPT), as front-line treatments for veterans experiencing PTSD (Acierno & Department of Veterans Affairs & Department of Defense, 2010). A key concern that has been expressed is that existing evidence-based treatments, such as PE and CPT, were developed when PTSD was conceptualized mostly as a fear-based disorder (Gray et al., 2012; Litz et al., 2016).
Two arguments have been proposed as to why existing evidence-based, cognitive behavioral PTSD treatment protocols may not be effective for treating moral injury-based PTSD (Steenkamp, Nash, Lebowitz, & Litz, 2013). First, PTSD was originally conceptualized as a fear-based disorder, and PE and CPT, to some extent, rely on habituation to decrease fear and anxiety, thereby reducing PTSD symptoms. Moral injury-based PTSD, on the other hand, involves more complex experiences than simple life threat, and as such, produces more complex emotional responses that may not respond to habituation. Therefore, in cases where guilt and shame are prominent, exposure-based treatments would be contraindicated. Second, Steenkamp and colleagues (2013) have argued that cognitions that are purported to underlie fear- or loss-based PTSD (e.g., “I am incompetent” and “The world is completely dangerous”) are completely different from those that underlie moral injury-based PTSD (e.g., “I am a monster” or “I can never be good again because of what I have done”). They argue that cognitions dealing with morality may need a different approach than the non-directive processing involved in PE or the active rational discussion of CPT. To address the cognitions that underlie moral injury-based PTSD, some have suggested that veterans with moral injury-based PTSD need to engage in an imaginary dialogue with a benevolent, forgiving moral authority (Gray et al., 2012). Specifically, Gray and colleagues (2012) suggested that “existing CBT may not sufficiently address the needs of war veterans because the fear conditioning and learning model does not sufficiently explain, predict, or address the diverse psychic injuries of war” (p. 408). Consistent with this concept, higher rates of moral injury-based PTSD in veteran populations may explain why treatment outcomes for veterans produce smaller effects compared with civilian samples (Monson et al., 2006; Steenkamp, Litz, Hoge, & Marmar, 2015). However, no empirical study to date has explicitly tested the claim that existing frontline treatments are less successful in treating moral-injury based PTSD.
Although it has been proposed that existing evidence-based treatments for PTSD do not sufficiently address PTSD that stems from a morally injurious traumatic event, we have repeatedly found in our clinical practice that PE and CPT have effectively reduced symptoms that stem from moral injury-based PTSD. The purpose of this manuscript is to describe how the theories underlying PE and CPT can account for moral-injury based PTSD and provide two clinical case examples that demonstrate the effective use of PE and CPT for PTSD that developed from a morally injurious events. Specifically, we detail the two cases of Carlos and David (both are pseudonyms), as they represent two clear examples of moral injury-based PTSD and appear to demonstrate how a shift in meaning making, as facilitated by the PE and CPT protocols, explained a reduction in PTSD symptoms and lessening of the cognitions commonly associated with moral injury.
Prolonged Exposure
Prolonged Exposure (PE; Foa, Hembree, & Rothbaum, 2007) is an evidence-based treatment modality developed to reduce the intensity and frequency of PTSD symptoms. PE is a structured treatment that involves approximately 10 sessions lasting 90 minutes each (Foa et al., 2007). It largely consists of imaginal exposure conducted in session and in vivo exposure conducted as homework assignments. The overall goal of the treatment is to actively address the two major criteria that are thought to prolong the symptoms of PTSD - avoidance and erroneous beliefs about oneself, others, and the world (Foa et al., 2007). In a meta-analysis of 13 studies with over 675 patients examining the effectiveness of PE, patients who received PE reported more significant reductions in symptoms than 86% of patients in control conditions (Powers, Halpern, Ferenschak, Gillihan, & Foa, 2010). A second meta-analysis showed that on average, 68% of those who complete treatment no longer meet the diagnostic criteria for PTSD (Bradley, Greene, Russ, Dutra, & Westen, 2005). Based on these research findings, PE is consistently recommended as a front-line treatment for PTSD (Department of Veterans Affairs & Department of Defense, 2010; Ursano et al., 2004).
Emotional Processing Theory (Foa & Cahill, 2001; Foa & Kozak, 1986) serves as the theoretical foundation for PE. According to EPT, fear structures in memory encode and connect representations of feared stimuli, responses, and the meaning of stimuli and responses. This structure is activated when input matches the information stored in the structure. In PTSD, the fear structures associated with the trauma memory become pathological when the associations between stimulus, response, and meaning elements do not accurately reflect reality. Most commonly, stimulus elements become erroneously associated with the meaning of danger and response elements become erroneously associated self-incompetence. Avoidance and inaccurate perceptions of oneself and the world maintain this pathological fear structure. Specifically, cognitive and behavioral avoidance of trauma reminders prevent the individual from learning information that would disconfirm inaccurate beliefs. In turn, having beliefs that “the world is completely dangerous” or “I am incompetent” further fuels avoidance. According to EPT, interventions can reduce pathological fear by promoting “emotional processing” in which accurate information is incorporated into the fear structure and modifies or competes with the pathological elements of the structure. In order for emotional processing to occur, the fear structure must be activated and new information must be available and integrated into the fear structure. PE aims to meet these two conditions and achieve emotional processing through imaginal and in vivo exposures that activate the fear structure through systematic confrontation with trauma reminders.
Although PE was developed around the concept of a fear structure, EPT can easily be applied to emotions other than fear (e.g., guilt, shame, disgust) by relying on the core concept of a memory structure that involves erroneous associations between stimulus, response, and meaning elements and promotes avoidance when activated (Foa & Cahill, 2001). In cases of moral injury, stimulus and response elements become erroneously connected with the meaning of “I’m a bad person” or “I’m a monster.” When activated by trauma reminders, these meaning elements evoke feelings of guilt and shame that promote cognitive and behavioral avoidance. This avoidance maintains erroneous beliefs about oneself as a bad person. In turn, thinking of oneself as a bad person promotes avoidance of others and situations in which those traits might be expressed and harm others. For example, imagine a veteran who shot a child and experienced an adrenaline rush while in the midst of a combat situation and goes on to develop PTSD as a result of this event. The presence of a child or the feeling of an adrenaline rush would activate the memory structure including the meaning “I’m a monster,” and evoke feelings of guilt and shame. These feelings would likely promote avoidance of children and situations that might produce an adrenaline rush (e.g., previously enjoyed activities). By avoiding these activities, that veteran would never have the opportunity to learn that he is warm and caring with children and that experiencing excitement does not make him a bad person. In PE for moral injury, imaginal and in vivo exposure serve the same purpose of promoting emotional processing by activating the memory structure and presenting incompatible information to modify the pathological memory structure and associated erroneous perceptions. Smith, Duax and Rauch (2013) have argued that in cases where perceived perpetration exists alongside trauma exposure, PE serves to counteract avoidance and place the event in its appropriate context, which would allow the veteran to focus on incompatible information that had been previously ignored. Thus, EPT and application of PE can easily be extended to cases of moral injury. Consistent with this conceptualization, research has shown that PE can effectively reduce guilt and shame (Øktedalen, Hoffart, & Langkaas, 2015; Resick, Nishith, Weaver, Astin, & Feuer, 2002; Stapleton, Taylor, & Asmundson, 2006) and that the reduction of negative cognitions, including negative beliefs about the self, is an important mechanism of change in PE treatment (Zalta et al., 2014).
Cognitive Processing Therapy
Cognitive Processing Therapy (CPT) is an evidence-based psychosocial intervention designed to treat PTSD in adults. CPT is typically conducted as a 12-session protocol, although findings from recent research advocate for a variable treatment length approach (Galovski, Blain, Mott, Elwood, & Houle, 2012; Resick, Monson, & Chard, 2014). CPT largely relies on the use of cognitive restructuring techniques to identify and modify maladaptive trauma-related cognitions known as stuck points. CPT has significant empirical support for treating veterans with PTSD (Monson et al., 2006). Significant gains in the primary outcomes of PTSD and depression as well as in secondary outcomes such as guilt, shame, dissociation, health-related concerns, anger and psychosocial functioning have been demonstrated and maintained in the long-term follow-up intervals up to five years (Galovski, Blain, Chappuis, & Fletcher, 2013; Resick et al., 2002; Resick, Williams, Suvak, Monson, & Gradus, 2012). CPT is consistently recommended as a front-line treatment for PTSD (Department of Veterans Affairs & Department of Defense, 2010) based on these strong research findings.
CPT is based in social cognitive theory (SCT; Bandura, 1991; Resick & Schnicke, 1992) and focuses on individuals’ beliefs about traumatic events and how they impact individuals’ emotions and behavior. According to SCT, individuals have three ways in which they can incorporate new information about the trauma into their existing schemata; they can alter the new information to match prior beliefs (assimilation), adjust their prior beliefs to incorporate the new information (accommodation), or change their prior beliefs to completely match the new information (over-accommodation). Accommodation of traumatic information leads to positive functioning whereas assimilation and over-accommodation of traumatic information leads to erroneous beliefs about oneself, others, and the world (referred to in CPT as stuck points). Trauma survivors often develop assimilated stuck points to help explain why the trauma occurred. For example, if a person believed that they could keep others safe (schemata), then lost friends in combat (new information), they might come to believe “If I had paid more attention to my surroundings, they wouldn’t have died.” Over-accommodated stuck points are present- and future-oriented beliefs that an individual has developed as a result of the trauma. For example, if a person previously believed that the world was generally safe (schemata), then experienced combat (new information), they might come to believe “the whole world is not safe at all.” CPT is structured around the idea that over-accommodated stuck points typically fall within one of five categories: safety, trust, power/control, esteem, and intimacy. CPT uses cognitive restructuring techniques to promote the examination of these beliefs and the discovery of evidence that disproves stuck points. By doing so, individuals are able to more accurately evaluate the traumatic event and appropriately assign responsibility and blame. The goal of this approach is to help individuals develop more appropriate accommodated beliefs, which results in a changed emotional response and a reduction of PTSD symptoms.
In cases of moral injury, assimilated stuck points typically focus on the idea that the individual should not have engaged in actions of commission or omission, during the morally injurious event or that betrayal directly or indirectly influenced an outcome. Thus, assimilated stuck points typically involve excessive guilt, self-blame, and, in some cases, betrayal. Guilt, self-blame, and betrayal are topics that have been addressed in CPT since its inception, thus CPT is easily applied to these assimilated beliefs in cases of moral injury. Over-accommodated stuck points for individuals with moral injury typically involve thinking of oneself as a “monster”, “unworthy”, or “a bad person”. These over-accommodated beliefs stem from the Just World belief that good people do good things and bad people do bad things. In the context of the five over-accommodated categories addressed in CPT, these beliefs often manifest in a lack of trust in oneself to not harm others (trust), poor self-esteem (esteem), low confidence in receiving esteem from others if they knew how the individual acted (esteem), an unwillingness to get close to others for fear of harming them (intimacy), and potentially a sense of lack of control over baser human instincts (power/control). Thus, CPT is structured to address all of the components of moral injury.
Clinical Case Examples: Carlos and David
The following two case examples of Carlos and David were drawn directly from our clinical care at the Road Home Program at Rush University Medical Center in Chicago, IL, a non-VA outpatient mental health treatment facility for veterans and their families. Informed consent was obtained from both individuals whose cases are presented in the paper and the authors disclosed any potential conflicts of interests. There was no particular rationale for providing PE to Carlos and CPT to David. The respective treatment choices were not based on clinical presentations and it is likely that each individual would have benefited equally from either one of the two interventions.
Assessments
Before beginning their respective treatment, each veteran participated in two 60-minute intake sessions during which they completed a semi-structured psychosocial interview, and then were assessed for PTSD using the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5; Weathers et al., 2015). It is important to note that neither Carlos nor David initially reported their index traumas during their clinical evaluations, likely due the intense guilt and shame associated with these events. Over the course of therapy, veterans were given self-report assessments at each session to monitor treatment progress.
PTSD Symptoms
PTSD symptom severity over the previous week was measured with the PTSD Checklist for DSM-5 (Weathers et al., 2013). The PCL-5 contains 20 items which mirror the DSM-5 diagnostic criteria for PTSD. Veterans are cued to consider their level of distress as related to their index trauma; each item on the PCL-5 is rated on a scale of 0 (Not at all) to 4 (Extremely). Scores of 31 or higher on the PCL-5 suggest probable PTSD, and the total score of the PCL-5 has been shown to be a reliable and valid measure of PTSD symptom severity in veteran populations (Bovin et al., 2015; Wortmann et al., 2016). Although score reductions of 10 or more have been labeled as clinically significant change on previous versions of the PCL (Monson et al., 2008), such guidelines for the PCL-5 have not yet been released (Wortmann et al., 2016).
Depressive Symptoms
Because depression is highly comorbid with PTSD, especially in veteran populations (Campbell et al., 2007), veterans were also assessed weekly with the Patient Health Questionnaire-9 (PHQ-9; Kroenke, Spitzer, & Williams, 2001), a reliable and valid self-report measure of depressive symptom severity. The PHQ-9 is comprised of nine items that mirror the DSM criteria for a Major Depressive Episode, with scores of 13 or greater suggesting probable Major Depressive Disorder (Beard, Hsu, Rifkin, Busch, & Björgvinsson, 2016). Each item is rated on a scale of 0 (Not at all) to 3 (Nearly every day) with higher scores indicating greater depressive symptoms.
Case Example #1: Carlos, Prolonged Exposure
Carlos, a 43-year old divorced father of four, served in the Army from 2003–2005, and deployed to Iraq twice with the military occupational specialty of 11-Bravo (Infantry). He received a General Discharge Under Honorable Conditions. Per his intake assessment, he first sought mental health treatment for PTSD in 2012 at the urging of his family. At the time, the veteran was homeless, not attending to hygiene, very symptomatic, and functioning poorly. He had held eleven jobs since his separation from the Army and reported constant tension with his family. The veteran, who obtained a 50% service-connected disability rating for PTSD with the VA, was prescribed Mirtazapine and Prazosin but acknowledged he was non-adherent. He also reported using cannabis daily to help ease intrusive thoughts and anxiety.
Trauma Description
The veteran provided the following trauma account during the third session of PE, when he began imaginal exposures. Notably, the veteran had been engaged in weekly psychotherapy in our clinic for almost one year, and had completed several residential programs for PTSD prior to disclosing this event. While in a group therapy session a few weeks prior, the veteran heard another group member speak about a similar morally injurious event.
I had to go on guard duty… I remember being really, really hot that day. We were bored, there wasn’t much to do. I remember Connor [fellow soldier; pseudonym used] saying, “here comes your girlfriend”. I looked up and I seen the little girl. She would always come dressed up because I would give her things, so she thought I was just a nice person. [sigh]…so…so…I remember Connor, he had the eyes [i.e. binoculars] on him. And he looked and said “something’s not right”, and I said “what are you talking about” and he said “looks like she’s crying or something” and he gave me the eyes and I looked through them…I remember seeing the girl, and I could visibly see that she had something under her clothes. I told Connor “something’s not right” and I passed him the eyes again. He called in to my command and told them what was going on. I remember they told us not to let the girl approach our position. I remember yelling out stop, stop, stop! I remember calling through on the radio again and telling them the girl is still approaching our position, what do we do? I remember looking over to the house then somebody over the radio say “don’t let her come near us, if she gets too close you got to take her out”. Ugh…[sigh]…I kept yelling stop, stop, stop! But she kept coming. I told Connor “shoot her in the legs man, stop her!” He froze. He wasn’t going to do it. I remember doing a combat roll out the turret. I remember snatching Connor’s rifle from his hands. It was hot. It was so hot. [sigh]. It was hot…the rifle was hot. I didn’t really have time to aim like I wanted to aim. I didn’t have time to position myself. I tried really, really hard to shoot her legs. I could have positioned myself. I could have done a lot of things. I didn’t take a sound shot. I took my shot and the girl fell. … Afterwards, I couldn’t talk to nobody. I couldn’t do nothing. I was just…I thought I was…[long pause]…I remember the engineers coming. I remember them getting ready to approach the little girl. I remember the little girl exploding. I remember screaming a second time. I remember cursing and swearing and being very upset. I remember being relieved of duty. I remember going to the safe house. I took a hot shower and I laid in bed and fell asleep. When I woke up, I thought I had a bad dream that that happened.
Case Conceptualization
Although the above situation meets DSM-5 definition of a criterion A traumatic event (American Psychiatric Association, 2013), it also typifies a morally injurious event. Carlos was forced to act against some of his most deeply held values in this situation and end the life of his friend, a young Iraqi girl, who was coerced by insurgents into carrying an explosive device towards Carlos’ checkpoint. Because Carlos felt he was completely to blame for taking the life of an innocent young girl, he endorsed prominent guilt (“I shouldn’t have shot the girl”) and shame (“I am a monster” and “people would be disgusted if they knew what I’ve done”) that lead to considerable experiential and interpersonal avoidance. For example, as described above he did not disclose this specific trauma until he had been in treatment for nearly two years, with a number of providers. Furthermore, his clinical presentation included poor occupational and social functioning (frequently changing jobs, quickly entering romantic relationships and then treating his partners so poorly that they left on bad terms, and daily marijuana use). In addition to the above symptoms, the veteran described frequent re-experiencing:
Carlos: “When you see a little girl and the first thing you think of is that little girl in Iraq. When you see a woman with kids, you think of that little girl in Iraq. When you see kids playing, you think about that little girl in Iraq. You see red shoes, you think about that little girl in Iraq. You go to a store and you pass by the little kids section, you think about that little girl in Iraq. I go to the store to buy toothbrushes and deodorant, I think about that little girl in Iraq. She’s constantly in my fucking head!”
Treatment Experiences
Carlos was offered a course of PE (Foa et al., 2007). Carlos’s therapist was a licensed clinical social worker who had received previous training in PE and was supervised by a licensed psychologist. Following suggestions from Smith, Duax and Rauch (2013), the therapist was careful to emphasize that guilt and shame were natural and expected reactions to trauma during the second session in which the therapist and client review the Common Reactions to Trauma worksheet. Broaching the topic of the veteran’s guilt and shame early in treatment may have served to increase the veteran’s hope that PE would be effective and relevant to his concerns; discussing guilt and shame early in treatment may have also further decreased the veteran’s sense of isolation, as many others have dealt with similar issues. The therapist used the in vivo exercises to specifically target the erroneous associations between stimulus, response, and meaning elements (i.e., “I’m a monster”) and the avoidance that maintained these associations. Indeed, the veteran’s in vivo hierarchy was notable for including many items having to do with social connection and self-care. For example, the veteran noted that sitting in a park where children were playing would yield a 50 on the Subjective Units of Distress Scale (SUDS). He also noted that looking at himself in the mirror would yield a 70 on the SUDS, which was driven by his feelings of disgust and self-hatred. Consistent with the PE protocol, the therapist collaborated with the veteran to complete relatively less challenging in vivo exercises early in treatment (i.e. riding the bus, going to the store during busy times) to increase his self-efficacy and provide the corrective emotional experience that he can be accepted and tolerated by others. Towards the end of treatment, the veteran was assigned in vivo exercises that were more provocative and elicited higher ratings on the SUDS of 80–90. For example, Carlos was assigned to take his nieces (who were about the same age as the Iraqi girl) to the park for the afternoon, which he eventually agreed to after exhibiting some ambivalence. This in vivo exercise was discussed in the following exchange, which was notable for the veteran’s ambivalence, but also the therapist’s compassionate yet assertive provision of the rationale:
Carlos: “I’m always going to have this guilt when I see little girls”
Therapist: “Can I give you some feedback on that? If you touch a hot Humvee, what do you learn?”
Carlos: “Don’t touch the Humvee”
Therapist: “Exactly. So you experience this event in Iraq…what do you think you learned about little girls?”
Carlos: [tearing up] “I get close to them, and then I kill them”
Therapist: This is why I suggested that you take your nieces to the park. You’re not around your family much, even though it sounds to me like they want you around. If you spend some time with your nieces, you’ll be creating some new experiences for yourself.
Carlos: I don’t know, man. I don’t think I can do that one.
Therapist: Why not? Let’s slow down and talk about it for a few minutes.
Carlos: It is just too much.
Therapist: What is too much?
Carlos: I hear what you are saying, but it is just too much. I destroy everything I touch. I’m scared of what would happen to them.
Therapist: What do you mean? What is the worst thing that would happen?
Carlos: I get overwhelmed and leave them there. I yell at them and make them cry. I run home. If I left them unattended…I…I couldn’t imagine. [laughing] How many more sessions are we going to be talking about this, anyway?
Therapist: [laughing] As many as it takes.
Carlos completed roughly half of the in vivo exercises that were assigned. The exercises may have assisted Carlos with increasing self-care and self-efficacy as well as re-establishing relationships with his family. Concurrent with the in vivo exercises, Carlos also completed six sessions of imaginal exposure focused on his index trauma. During the imaginal exposures, the therapist was mindful to cue the veteran to include increasing levels of detail to help the veteran place the event in its proper context. The inclusion of greater levels of detail, further reinforced by the post-exposure processing, may have helped the veteran incorporate new information that was incompatible with the erroneous meaning he had made of the event. The therapist’s stance in the post-exposure processing also typified the non-directive style of processing that is encouraged following completion of imaginal exposures (Foa et al., 2007; Smith et al., 2013). Below is an example of post-exposure processing in the fourth session in which the veteran, completely unprompted by the therapist, began to integrate his original intent into his understanding of the situation. Carlos had apparently not considered up until this point that he wanted to protect the little girl.
Therapist: How was that for you today?
Carlos: I’m really fucking angry right now.
Therapist: Oh? Tell me more.
Carlos: I was in that country to help people like her. I wasn’t there to shoot little kids! She was helpless! …I didn’t go into that situation wanting her to die. [begins to tear up]
Therapist: What did you want to happen that day?
Carlos: I don’t know, but not that.
Through repeatedly revisiting the index event and adding greater levels of contextual detail, the veteran showed increasing evidence that he was beginning to doubt his original interpretation of the event. This may have meant that his original, erroneous associations between the stimulus, response and meaning elements of the morally injurious event were beginning to loosen. His greater exploration of the event may have been facilitated by the lessening of the painful emotions that accompanied the memory through habituation. The following exchange occurred after the imaginal exposure in the fifth session:
Carlos: I feel sick about it. I just have this feeling like if I had composed myself. If I had taken a better shot. I think sometimes I could have gotten in the prone position. I could have most definitely shot her legs that way. If I had just taken the time. Wiped the sweat off my face. I could have taken a solid shot. My command wanted us to put the wire up [to keep children away from the checkpoint], but we didn’t do it because the kids were playing there and they had nowhere else to go. If we had listened to our mind instead of our heart, then she wouldn’t have been able to get close!
Therapist: If you could go back, what would you do differently?
Carlos: I think about that a lot…I could have done something to give her a better chance.…I think so, but I don’t know…I don’t know.
Upon arriving for seventh session, however, the therapist noticed that Carlos’ PCL-5 had decreased 18 points, a marked change. The change in PCL-5 score was accompanied by a change in the veteran’s understanding of the event. The following exchange between Carlos and his therapist demonstrates Carlos’ significant progress towards acknowledging an appropriate level of culpability in the event, without resorting to self-condemnation.
Therapist: What do you think has changed since starting PE?
Carlos: I was part of a fucked up situation that I didn’t want no part of. I realized I didn’t want to be a part of that. I didn’t want that to happen. It lets me know that …it happened, I could have probably did some shit that might have changed it a little bit but I know that girl would have died all the same. It is shitty that I had to be a part of that, but it happened.
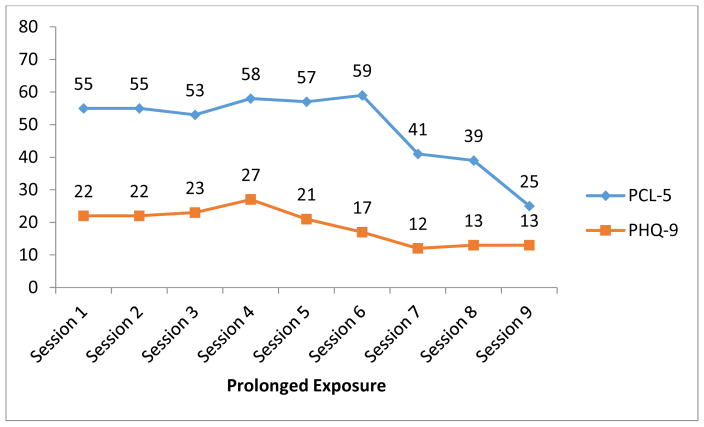
Carlos’ session-by-session scores on the PCL-5 and PHQ-9 are presented in Figure 1. By the time Carlos had terminated PE, he had experienced a precipitous drop of 30 points in his self-reported PTSD symptoms as measured by the PCL-5. Also notably, he was below the suggested diagnostic threshold of 31 for the PCL-5 (Bovin et al., 2015), and he was at the suggested threshold for Major Depression (Beard et al., 2016), having fallen from a 22 on the PHQ-9 at the start of PE to a 13 at termination. In addition to reduced symptoms, the veteran described significantly reduced guilt at termination:
Therapist: Anything new come out of the exposure today?
Carlos: [laughing] Ok…Maybe I’m not 100% to blame for what happened to that little girl.
Therapist: [laughing] What do you mean, maybe?
Carlos: No. I’m certain I’m not to blame. Last week was really powerful for me…I realized I had all this guilt. So much guilt over that situation. I realized I let the guilt overwhelm me. I let the guilt consume me.
Figure 1.
PTSD and Depression Scores Across Prolonged Exposure Sessions.
He also described tighter social connections with his family and nieces, and especially his girlfriend. He stated: “It feels wonderful to have the kind of love I want from somebody” and he spoke about sharing some of his personal effects from his deployment with her, including showing her the uniform he was wearing the day he shot the little girl. He recalled: “We both just cried and cried, and she hugged me. I knew that she understood, and everything was OK”. Lastly, Carlos had reduced his use of cannabis from daily at the start of treatment to once a week.
Conclusion
The above case example illustrated the successful application of PE to a veteran with PTSD resulting from a morally injurious event. In addition to PTSD, the veteran also exhibited problems consistent with current conceptualizations of moral injury, such as prominent guilt and shame, as well as social isolation and poor social and occupational functioning. The therapist who delivered PE was able to apply the techniques of PE – in vivo exposures and imaginal exposures – to these symptoms and achieve a good outcome for the veteran. Psychoeducation may have helped destigmatize the veteran’s reactions to his index trauma by normalizing his experiences. The therapist used in vivo exercises to target his social isolation and self-hatred by collaborating with the veteran to engineer experiences that may have provided corrective emotional experiences (i.e., that he is capable of taking care of children). Imaginal exposures may have reduced the veteran’s painful emotions associated with the memory and helped him integrate more contextual detail in his memory, perhaps making it possible to reappraise his role in the trauma and obtain symptom relief.
Case Example #2: David, Cognitive Processing Therapy
David is a 36-year old Army veteran. He served from 2002–2008 and deployed to Iraq twice with the military occupational specialty of 12-Bravo (Combat Engineer). David received a General Discharge Under Honorable Conditions and did not seek mental health services prior to coming to our clinic. Per his intake assessment, David’s struggle with PTSD symptoms began shortly after returning from his second deployment where his index trauma occurred. David reported difficulties in his long-term relationship, which he attributed to his inability to control his anger and substance use. David also reported several legal issues including numerous driving under the influence charges and a history of alcohol dependence and drug abuse. David explained that he initially used alcohol to help him sleep but that he was unable to control his drinking. David reported no longer being dependent on alcohol when he sought treatment through our clinic but explained that he still abused alcohol and drugs and that his use was commonly preceded by trauma-related reminders.
Trauma Description
David provided the following brief description of his index trauma during the third CPT session. After his therapist noticed that David had very balanced views related to the traumatic experience he initially chose to focus on in treatment, his therapist inquired about other traumatic experiences that still “haunted” David to that day. This was when David disclosed the following:
“We were driving in a convoy when the squad leader spotted children who looked like they were digging holes in the ground for the enemy to bury IEDs. As the gunner, it was my role to take them out, as the scenario posed a potential threat to future missions. The rules of engagement regarding potential threats had just changed and we were ordered to consider all suspicious activity a potential threat. When the squad leader tapped me on my boot, I knew that I had to take them out… I really didn’t want to… I mean… They were children… They probably didn’t even know why they were digging holes but were just told to do so by their parents… They looked so innocent… I prayed that I wouldn’t have to fire my weapon… That something would happen to prevent me from having to shoot. My squad leaders tapping became more intense. I knew it was time to pull the trigger. I tried to aim the weapon away from them to fire a warning shot. I was hoping that would be enough to scare them away so that a quick reaction force could come out and inspect the holes these kids dug… [sigh] I blasted them. I really didn’t mean to... [starts crying]… I really wanted to aim away but my .50 cal was set on auto and the combination of the driving vehicle and the automatic setting on my weapon… I killed those kids… [long pause]… And then I laughed [begins to sob]… I laughed right after I blasted them. Who [expletive] does that?! How in the world am I ever supposed to live with this?”
David’s experience meets the diagnostic criteria for a Criterion A traumatic event according to the DSM-5 (American Psychiatric Association, 2013). The content of the event also reflects a situation that has the potential to violate an individual’s morals and deeply held beliefs. It is evident from David’s trauma description that he struggled with the fact that he shot seemingly innocent children after his squad leader ordered him to do so. David assumed full responsibility for the event and answered his own question about who would commit such actions by calling himself “heartless” and “a monster”. David reiterated throughout therapy that he did not believe that he had a right to live because he took innocent children’s lives.
Treatment Experiences
David was offered a course of CPT by a licensed clinical social worker who was trained in CPT and supervised by a licensed clinical psychologist. David participated actively in all 12 of his CPT sessions and was moderately compliant with homework assignments, usually bringing at least one completed worksheet to session. In the beginning of therapy, David was not clear about his index trauma; he was nervous about using it as the focus for treatment because he was concerned about what his therapist would think of him. David voiced this concern early on and indicated that he would rather focus on another traumatic event that was also disturbing, though was much less morally ambiguous. David’s therapist validated his concerns and explained that some gains could likely be achieved by focusing on a different traumatic event, but also highlighted how much distress the index event appeared to be causing David on a daily basis. Further, the therapist reflected that the index trauma seemed to be the underlying cause of much of his distress. After an open discussion during the third session and exploration of sources of distress, David chose to focus on the index trauma described above for the remainder of treatment.
David’s therapist focused all of the early session content directly on David’s trauma. Specifically, rather than using hypothetical instances or remotely related situations from David’s life to explain the cognitive model and associated ABC worksheets, all examples were assimilated stuck points directly taken from David’s trauma. Doing so helped David clearly see in his third CPT session that his guilt-based thoughts, such as “I should not have pulled the trigger” or “I should have known they were just playing,” were thoughts that were likely fueling his feelings of guilt, shame, sadness, and anger at himself. It is important to note that although David saw the connection between his thoughts and feelings early in his treatment, his view of the situation was still too narrow to experience any shift in his thinking. Despite being able to make connections between his perception of the event itself and the resulting emotions, David repeatedly reminded his therapist that he was to blame for the event and that he saw himself as a monster. Rather than challenging David’s beliefs in these moments, his therapist assured David that it is perfectly normal to think this way given that these cognitions developed years ago when the event occurred and have been reinforced over time. David was encouraged to continue his homework with the goal of practicing making connections between cognitions and emotions rather than challenging his way of thinking. Framing the homework assignments in this light allowed David to not get caught up in feeling as though he was told that his thinking was somehow wrong and that he had to change it.
Toward the end of the third session and going forward, David and his therapist spent a lot of time exploring the index event. David’s therapist used a large number of clarifying questions to be able to gain a better understanding of the situation. The use of clarifying questions as part of the Socratic process may have helped broaden the context of the situation and allowed both David and his therapist to begin to see important aspects of the event that would be helpful to consider when evaluating responsibility and blame. The exchange below is a brief example of how clarifying questions can be used to broaden the context of the situation:
David: “I really didn’t want to blast [the kids]!”
Therapist: “What do you mean?”
David: “I knew I had to shoot after the squad leader told me to… I knew I had to. It was an order and I follow orders. But I thought if I aim next to them and fire a warning shot… That that would scare them away or something.”
Therapist: “So you knew that you had to fire your weapon but also thought of ways to follow orders and not to shoot the kids?”
David: “Right. I thought aiming next to them with my .50 cal would be enough…”
Therapist: “I didn’t realize you wanted to aim away. Were you able to?”
David: “Yeah… I was… I made sure I aimed to their right... We were just going so fast and my weapon was set on automatic that I ended up tearing them to shreds. I am such an idiot. Who sets their .50 cal on auto?!”
Therapist: “I hear you’re upset and if I am tracking you actually aimed away when you fired the shot? And the reason you ended up hitting them was the result of the driving vehicle and your weapon setup? Am I getting this right?”
David confirmed that his therapist was understanding him correctly. Though the exchange above may appear somewhat slow, slowing down the pace of the Socratic dialogue likely allowed David to process information and draw his own conclusions. The continued use of clarifying questions led David to generate additional insight that became extremely important in the later stages of CPT. Specifically, David explained that the weapon setup played a key role: David struggled with the belief that he should have visually checked his weapon’s setup before firing a shot. David also explained that he felt guilty for laughing immediately after he shot the children. Instead of moving slower and exploring important pieces of information in great detail, a therapist could have simply highlighted that David did not want to shoot the children. While an accurate observation and possibly an important and effective challenge during the Socratic process, it is plausible that the immediate challenging of stuck points would have obscured the critical information highlighted above. Challenging stuck points too early and limiting the amount of clarifying questions can prevent individuals from generating sufficient context necessary to effectively challenge stuck points. Thus, building context in itself can be an effective way of indirectly challenging stuck points PTSD stemming from morally injurious events.
Based on the exchange detailed above and the following discussion, David and his therapist realized that the event itself was divided into three different pieces of evidence to support his beliefs: weapon check, shooting, and laughing. Dividing the event into these three different, yet related pieces of evidence allowed for the Socratic process to occur in a more focused manner. Furthermore, the specificity of each piece of evidence within the larger event made challenging stuck points much easier. David’s therapist took his time challenging various stuck points, including “I should have visually inspected the weapon setup”, “I should not have fired my weapon”, and “I should not have laughed after I shot the kids.” Examining all of the relevant context and evidence may have made it easier for David to see the situation from a different perspective, as shown in the exchange below.
Therapist: “We’ve talked about a ton of stuff, let me make sure that I got it all. First we talked about your weapon setup for quite some time and you explained that while you wish you had visually inspected your weapon right before you fired you were also under a lot of pressure since your squad leader kept ordering you to fire. You also mentioned that you inspected the weapon not too long before the incident and that it was set on single shot like usual. Then you explained that the switch of the weapon is in a place where left-handed guys like you are more prone to accidentally switch the setting. Lastly you mentioned to me that you were so focused on the kids, trying to see if they were just digging or if they really had explosives they were burying, or if you could see any other individuals in the area and that it would have been difficult to spend any more time visually inspecting your weapon given that the situation occurred within a matter of seconds between you getting the order and you having to shoot. Am I getting all of that?”
David: “Yeah, that’s pretty much what we’ve talked about. It’s strange hearing it all from you.”
Therapist: “What do you mean?”
David: “I mean… I know I told you all of this, and all of this is true, but… I guess I never put all of this together. That’s some heavy [stuff]”
Therapist: “Heavy [stuff]?”
David: “Yeah… [Expletive]… This is really messing with me... This is so different than what I’ve been telling myself all this time.”
The summary that David’s therapist provided was not the first summary. In fact, every time David provided important contextual information or key evidence that would contradict one of his stuck points, his therapist summarized the new information along with evidence that David provided previously. Though summaries were getting lengthier with every piece of additional evidence that David provided, they allowed him to constantly be reminded of information that he initially tended to omit when evaluating the situation. Furthermore, using selective summaries allowed David’s therapist to subtly challenge David’s beliefs using David’s own statements, without creating a sense of conflict that some clients experience when therapists attempt to challenge stuck points. Especially in cases of moral injury, when individuals already believe that society views them extremely negatively for the things they have or have not done or the person they believe they are, we have found that a more confrontational Socratic approach is not beneficial and further alienates the clients and therapists.
Most individuals who are affected by PTSD know, at least on some level, that they behaved in the best way possible given the difficult situation they faced. However, if direct challenging questions, such as “Was there anything else you could have realistically done?” are asked too early in the process, clients will lack the evidence to appropriately integrate the logical answer (e.g., “There wasn’t anything else I could have realistically done”) to this question. Such exchanges frequently result in clients expressing an understanding that they could not have done anything different, but still feeling guilty about what they have done. This discrepancy is likely due to unchallenged and inaccurate information the clients use to support their guilt. The key to internalizing a more accurate belief about the specific situation is to explore various pieces of evidence. For example, had the fact that the vehicle was moving not been explored in its entirety, David may have stated that he really did not want to shoot the children and that the situation was made more difficult by the fact that his weapon was set on automatic, but he would be likely to blame himself for not taking a better shot and making sure that the bullets hit next to the children. Once David and his therapist explored the role that the moving vehicle played in this situation, David was able to realize that it further impaired his ability to keep the children from getting hit by his bullets, no matter how hard he had tried to aim away. By this point, the third area of focus, David’s laughter immediately after shooting the children, required minimal exploration. David had already begun to appreciate that his intent in the situation had not been to harm anyone and that the end result, as well as his laughter, were the product of a situation, time, and place, rather than the product of an enduring character deficit. Without prompting from the therapist, David was able to present his own evidence that sometimes we behave in ways that are not voluntary (e.g., reflexes) and that periods of extreme stress can produce strange behavior (e.g., inappropriate affect). Thus, he was able to see the assimilated stuck point “I should not have laughed after I shot the kids” in a new light, and decrease the degree to which he held himself responsible for laughing at an inappropriate moment. We have seen repeatedly that, in many cases, veterans experience a general decrease in the intensity of guilt and shame-related beliefs (e.g., “I should have visually inspected the weapon setup” and “I should not have fired my weapon”) after the index trauma has been sufficiently contextualized and the assimilated stuck points have been successfully challenged.
Examining all of the pieces of evidence helped David realize that he tried to inflict no or as little harm as possible to the children in order to diffuse the situation and minimize the danger. The in-depth exploration of his stuck points through Socratic questioning helped David realize the complexity of these situations and combat more broadly. This, in turn, led to David’s over-accommodated stuck points, such as “I am a monster” to automatically become looser, as he was able to realize that a monster would have acted with a different intent and would show less remorse. David stated from the beginning of therapy that he viewed himself as a monster and expressed repeatedly how much this view of himself affected him and destroyed his life. His therapist, however, appropriately waited to challenge this stuck point until all of the initial evidence from assimilated stuck points that David used to reinforce this over-accommodated belief was effectively challenged in earlier sessions. Had David’s therapist started challenging the over-accommodated stuck point before challenging the assimilated stuck points that were supporting it, it is very likely that challenging “I am a monster” would have only resulted in temporary relief. David’s unchallenged assimilated beliefs would have led to a re-formation of the belief that he was a monster after all because the underlying beliefs would not have been challenged.
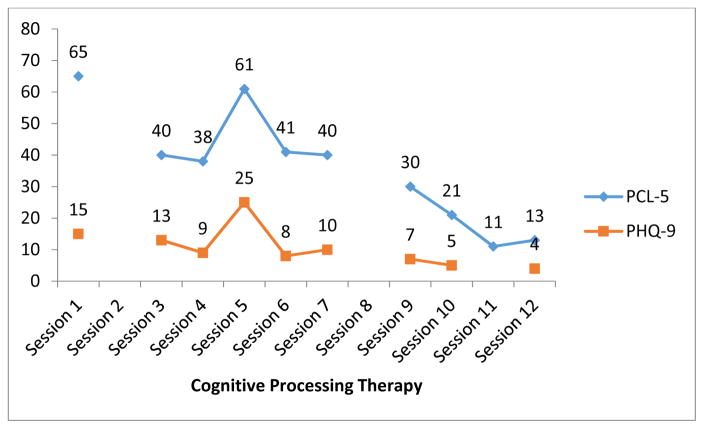
David’s session-by session scores on the PCL5 and PHQ-9 are reported in Figure 2. Despite having missing self-report data for the second and eighth session, a clear downward trend is noticeable when examining David’s self-reported scores for PTSD and depression severity. David’s self-reported PCL-5 score dropped 52 points over the course of treatment. Starting with the ninth CPT session, David no longer scored above the probable PTSD threshold of 31 for the PCL-5 (Bovin et al., 2015). A similar reduction can be observed for his self-reported depression scores, which reduced by 11 points on the PHQ-9. It is noteworthy that his PTSD and depressive symptoms increased drastically during the fifth CPT session after he was asked to rewrite his trauma account and to include more details and sensory information, as we believe this provided an important opportunity for David to confront the morally injurious memory and incorporate new information into his appraisals of the event. Although this assignment was initially difficult for David, his scores following the session suggested that completing the assignment had a positive effect on his recovery. David reported reduced feelings of guilt and shame and expressed a desire to re-engage in life and reconnect with friends and family, whom he had avoided as a result of his trauma.
Figure 2.
PTSD and Depression Scores Across Cognitive Processing Therapy Sessions.
Conclusion
In sum, the use of clarifying questions early on in CPT allowed David to build a solid context that helped both David and his therapist understand under what circumstances the event occurred. Through clarifying questions, it also became apparent that the single index event actually consisted of three pieces of evidence. Being specific about which piece of evidence was targeted in the Socratic process made challenging stuck points easier and more effective because exploration could be very specific. Continuous summarizing of potential evidence that David’s therapist heard allowed David to be reminded of all of the evidence he had generated himself. The therapist’s naïve attitude encouraged David to explain various situations, which, in turn, allowed him to think of certain aspects that he had not considered to be important before. Lastly, it was important for David to understand that the goal of the therapy was not to feel good about what he had done but rather to accurately evaluate what happened. Understanding that he was not supposed to feel proud of what he had done and that sadness related to shooting children was a normal response, allowed David to accept the difficult situation. Being able to clearly distinguish his actions during the situation from his evaluation of himself allowed David to begin the natural grieving process.
Discussion
The two case examples for Carlos (PE) and David (CPT) described above clearly show that participation in evidence-based treatments for PTSD helped both individuals achieve significant PTSD and depression symptom reductions, despite their index traumas being based on morally injurious events. Although moral injury was not directly measured, which is a limitation of the present case report, both Carlos and David experienced events that can be considered morally injurious (cf. Litz et al., 2009). We believe that improvements over the course of PE and CPT were the result of confronting avoidance and adding greater levels of contextual detail to the traumatic memory, which helped these patients reappraise and restructure their original, erroneous interpretations of the events. It is important to note that neither PE nor CPT are intended to justify, normalize, or excuse atrocious actions. Instead, both approaches help the individuals affected by morally injurious experiences to view their actions in the context in which they occurred. Broadening the context of the situation will help individuals more accurately attribute responsibilities to the parties involved. In the examples described above, Carlos and David continue to carry some of the responsibility for the events that occurred but also realized that other people were involved and that the circumstances of the situations were unique, thus providing information that was inconsistent with the erroneous global, stable, and internal attributions they had made of the event. Both Carlos and David were able to incorporate their intent during the morally injurious events into their new understanding of the memory and to separate their actions during the event from their more stable view of themselves. Arriving at this stage during PE and CPT allowed both Carlos and David to achieve significant symptom reduction.
Most individuals who engage in PE or CPT show either a rapid decrease in symptoms or a more gradual, linear decrease over the course of treatment (e.g., Clapp, Kemp, Cox, & Tuerk, 2016; Galovski, Blain, Mott, Elwood, & Houle, 2012). In contrast, Carlos and David made large gains toward the end of their treatment. It is possible that Carlos and David demonstrated more delayed responses to treatment because of the role that overaccommodated beliefs (e.g., “I am a monster”) played in the maintenance of their moral-injury based PTSD symptoms. Overaccommodated beliefs are typically not addressed until later in treatment in both protocols. Further research is needed to explore how modification of assimilated and overaccomodated beliefs leads to symptom changes in fear-, loss-, and moral injury-based PTSD.
While we have observed treatment successes, which suggest that PE and CPT can be effective in the treatment of moral injury-based PTSD, treating moral injury-based PTSD can be more difficult and complex compared to the treatment of other trauma types. Difficulties may be attributed to the fact that individuals who are deeply affected by moral injury often require additional time before they discuss their traumatic experiences, possibly due to feelings of betrayal and/or intense guilt and shame associated with their actions and inactions during the traumatic event. Because of the intense guilt and shame that is associated with moral injury, neither Carlos nor David initially reported these specific index traumas in a broader discussion during their clinical evaluations about which trauma to target in treatment. Indeed, Carlos was in treatment for about two years before he disclosed his index trauma. Only after the respective clinicians noticed that the initially reported traumas were described in seemingly accurate and balanced ways did they educate their clients that some bothersome traumatic experiences seem culturally unacceptable, but are important to discuss in treatment where confidentiality prevents clients from facing legal repercussions. Demonstrating awareness and opening the door for the clients to discuss possible morally injurious experiences likely facilitated the veterans’ willingness to explore these traumas in more detail and focus on them over the course of treatment. Rather than assuming that the true index event is always revealed during intake evaluations, it is important to bear in mind that they can be revealed over the course of treatment as well, at which point the clinicians should adjust treatment accordingly.
For individuals with moral-injury based PTSD, negative self-perceptions may be further intensified by generally negative societal views about perpetration-based events that are frequently the foundation of moral injury. Therapists are not excluded from these biases; when working with veterans who are struggling with moral injury, clinicians may sometimes notice that their own morals and values interfere with their ability to effectively treat a veteran who may have acted or witnessed actions that violated such moral codes. Thus, it is imperative for clinicians to remain as open, unbiased, and nonjudgmental as possible, and to not repeat the societal stigma that exists related to many potentially morally injurious situations. Because moral injury is associated with intense guilt and shame, as well as feelings of betrayal, sensing judgment from the therapist about what one has done or witnessed, can alienate the client, intensify the moral injury cycle, and further reinforce veterans’ existing maladaptive beliefs.
Lastly, in attempts to minimize their own discomfort with different morally injurious situations, some clinicians may be inclined to insert their own opinions or values (e.g., “It wasn’t your fault; you didn’t mean to harm the children,” or “You shouldn’t have shot those children”) into the therapeutic process. It is important to note that the therapists’ own opinions and values may prematurely stop the exploration of the maladaptive beliefs and the gathering of disconfirming evidence. For clinicians working with veterans affected by moral injury it is therefore important to remember that these veterans would not seek help if they did not feel remorse for the ways in which they have acted or seen others act.
The two cases described above illustrate how PE and CPT, with no modification, can successfully treat moral injury-based PTSD. We have been able to reproduce similar results with other cases where moral injury-based PTSD was present, suggesting that the examples presented in this manuscript are not findings produced by chance. Consistent with existing research (Zalta, 2015), it appeared that the key mechanism through which change occurred in both treatments was the reduction of erroneous cognitions. It is possible that although both PE and CPT appear to be effective for moral injury-based PTSD, these treatments may not achieve the same effects as they do for fear- or loss-based PTSD. It is also possible that interventions specifically developed to address moral injury, such as Adaptive Disclosure (Gray et al., 2012), may produce superior results for moral-injury based PTSD than PE or CPT. Moreover, moral injury is a separate construct from PTSD, though the two overlap to some extent. Some individuals who have experienced moral injury may not meet the diagnostic criteria for PTSD. These individuals may rightly not be offered PE or CPT, which were both developed as treatments for individuals who meet the diagnostic criteria for PTSD. Further empirical research is needed to determine whether existing evidence-based treatments (e.g., PE and CPT) are maximally effective for treating moral-injury based PTSD and moral injury more broadly.
Acknowledgments
Philip Held receives grant support from the Cohn Family Foundation. Alyson Zalta receives grant support from the National Institute of Mental Health (K23 MH103394). We thank our research assistant Darian Weaver for her assistance with the formatting of this manuscript.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. Washington D.C: American Psychiatric Association; 2013. [DOI] [Google Scholar]
- Bandura A. Social cognitive theory of self-regulation. Organizational Behavior and Human Decision Processes. 1991;50(2):248–287. [Google Scholar]
- Beard C, Hsu KJ, Rifkin LS, Busch AB, Björgvinsson T. Validation of the PHQ-9 in a psychiatric sample. Journal of Affective Disorders. 2016;193:267–273. doi: 10.1016/j.jad.2015. [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, Keane TM. Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (PCL-5) in veterans. Psychological Assessment. 2015 doi: 10.1037/pas0000254. [DOI] [PubMed] [Google Scholar]
- Bradley R, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. American Journal of Psychiatry. 2005;162(2):214–227. doi: 10.1176/appi.ajp.162.2.214. [DOI] [PubMed] [Google Scholar]
- Campbell DG, Felker BL, Liu CFCF, Yano EM, Kirchner JE, Chan D, … Chaney EF. Prevalence of depression–PTSD comorbidity: Implications for clinical practice guidelines and primary care-based interventions. Journal of General Internal Medicine. 2007;22(6):711–718. doi: 10.1007/s11606-006-0101-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clapp JD, Kemp JJ, Cox KS, Tuerk PW. Patterns of change in response to prolonged exposure: Implications for treatment outcome. Depression and Anxiety. 2016;33(9):807–815. doi: 10.1002/da.22534. [DOI] [PubMed] [Google Scholar]
- Department of Veterans Affairs & Department of Defense. The VA/DoD clinical practice guideline for the management of post-traumatic stress. 2010 Retrieved from http://www.healthquality.va.gov/PTSD-FULL-2010c.pdf.
- Drescher KD, Foy DW, Kelly C, Leshner A, Schutz K, Litz B. An exploration of the viability and usefulness of the construct of moral injury in war veterans. Traumatology. 2011;17(1):8–13. doi: 10.1177/1534765610395615. [DOI] [Google Scholar]
- Foa EB, Cahill SP. Psychological therapies: Emotional processing. In: Smelser NJ, Baltes B, editors. International Encyclopedia of the Social & Behavioral Sciences. 2001. pp. 12363–12369. [Google Scholar]
- Foa EB, Hembree EA, Rothbaum BO. Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences. Therapist guide. New York, NY: Oxford University Press; 2007. [Google Scholar]
- Foa EB, Kozak MJ. Emotional processing of fear: exposure to corrective information. Psychological Bulletin. 1986;99(1):20–35. Retrieved from papers3://publication/uuid/7D932E66-D6B6-4D33-B1EE-C42553A48B5E%5Cnhttp://www.ncbi.nlm.nih.gov/pubmed/2871574. [PubMed] [Google Scholar]
- Foa EB, Rauch SAM. Cognitive changes during prolonged exposure versus prolonged exposure plus cognitive restructuring in female assault survivors with posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2004;72(5):879–884. doi: 10.1037/0022-006X.72.5.879. [DOI] [PubMed] [Google Scholar]
- Fontana A, Rosenheck R. A model of war zone stressors and posttraumatic stress disorder. Journal of Traumatic Stress. 1999;12(1):111–126. doi: 10.1023/A:1024750417154. [DOI] [PubMed] [Google Scholar]
- Frankfurt S, Frazier P. A review of research on moral injury in combat veterans. Military Psychology. 2016 doi: 10.1037/mil0000132. [DOI] [Google Scholar]
- Fulton JJ, Calhoun PS, Wagner HR, Schry AR, Hair LP, Feeling N, … Beckham JC. The prevalence of posttraumatic stress disorder in Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) Veterans: A meta-analysis. Journal of Anxiety Disorders. 2015;31:98–107. doi: 10.1016/j.janxdis.2015.02.003. [DOI] [PubMed] [Google Scholar]
- Galovski TE, Blain LM, Chappuis C, Fletcher T. Sex differences in recovery from PTSD in male and female interpersonal assault survivors. Behaviour Research and Therapy. 2013;51(6):247–255. doi: 10.1016/j.brat.2013.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galovski TE, Blain LM, Mott JM, Elwood L, Houle T. Manualized therapy for PTSD: flexing the structure of cognitive processing therapy. Journal of Consulting and Clinical Psychology. 2012;80(6):968–81. doi: 10.1037/a0030600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray MJ, Schorr Y, Nash W, Lebowitz L, Amidon A, Lansing A, … Litz BT. Adaptive disclosure: an open trial of a novel exposure-based intervention for service members with combat-related psychological stress injuries. Behavior Therapy. 2012;43(2):407–15. doi: 10.1016/j.beth.2011.09.001. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine. 2004;351(1):13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Riviere LA, Wilk JE, Herrell RK, Weathers FW. The prevalence of post-traumatic stress disorder (PTSD) in US combat soldiers: A head-to-head comparison of DSM-5 versus DSM-IV-TR symptom criteria with the PTSD checklist. The Lancet Psychiatry. 2014;1(4):269–277. doi: 10.1016/S2215-0366(14)70235-4. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litz BT, Lebowitz L, Gray MJ, Nash WP. Adaptive disclosure: A new treatment for military trauma, loss, and moral injury. New York, NY: Guilford Press; 2016. [Google Scholar]
- Litz BT, Stein N, Delaney E, Lebowitz L, Nash WP, Silva C, Maguen S. Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clinical Psychology Review. 2009;29(8):695–706. doi: 10.1016/j.cpr.2009.07.003. [DOI] [PubMed] [Google Scholar]
- MacNair RM. Causing trauma as a form of trauma. Peace and Conflict: Journal of Peace Psychology. 2015;21(3):313–321. doi: 10.1037/pac0000116. [DOI] [Google Scholar]
- Monson CM, Gradus JL, Young-Xu Y, Schnurr PP, Price JL, Schumm JA. Change in posttraumatic stress disorder symptoms: Do clinicians and patients agree? Psychological Assessment. 2008;20(2):131–138. doi: 10.1037/1040-3590.20.2.131. [DOI] [PubMed] [Google Scholar]
- Monson CM, Schnurr PP, Resick PA, Friedman MJ, Young-Xu Y, Stevens SP. Cognitive processing therapy for veterans with military-related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2006;74(5):898–907. doi: 10.1037/0022-006X.74.5.898. [DOI] [PubMed] [Google Scholar]
- Øktedalen T, Hoffart A, Langkaas TF. Trauma-related shame and guilt as time-varying predictors of posttraumatic stress disorder symptoms during imagery exposure and imagery rescripting—A randomized controlled trial. Psychotherapy Research. 2015;25(5):518–532. doi: 10.1080/10503307.2014.917217. [DOI] [PubMed] [Google Scholar]
- Powers MB, Halpern JM, Ferenschak MP, Gillihan SJ, Foa EB. A meta-analytic review of prolonged exposure for posttraumatic stress disorder. Clinical Psychology Review. 2010 Aug; doi: 10.1016/j.cpr.2010.04.007. [DOI] [PubMed] [Google Scholar]
- Resick PA, Monson CM, Chard KM. Cognitive processing therapy treatment manual: Veteran/military version. Boston, MA: Veterans Administration; 2014. [Google Scholar]
- Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology. 2002;70(4):867–79. doi: 10.1037//0022-006x.70.4.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Schnicke MK. Cognitive processing therapy for sexual assault victims. Journal of Consulting and Clinical Psychology. 1992;60(5):748–56. doi: 10.1037//0022-006x.60.5.748. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/1401390. [DOI] [PubMed] [Google Scholar]
- Resick PA, Williams LF, Suvak MK, Monson CM, Gradus JL. Long-term outcomes of cognitive–behavioral treatments for posttraumatic stress disorder among female rape survivors. Journal of Consulting and Clinical Psychology. 2012;80(2):201–210. doi: 10.1037/a0026602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith ER, Duax JM, Rauch SAM. Perceived perpetration during traumatic events: Clinical suggestions from experts in prolonged exposure therapy. Cognitive and Behavioral Practice. 2013;20(4):461–470. [Google Scholar]
- Stapleton JA, Taylor S, Asmundson GJG. Effects of three PTSD treatments on anger and guilt: Exposure therapy, eye movement desensitization and reprocessing, and relaxation training. Journal of Traumatic Stress. 2006;19(1):19–28. doi: 10.1002/jts.20095. [DOI] [PubMed] [Google Scholar]
- Steenkamp MM, Litz BT, Hoge CW, Marmar CR. Psychotherapy for military-related PTSD: A review of randomized clinical trials. Journal of the American Medical Association. 2015;314(5):489–500. doi: 10.1001/jama.2015.8370. [DOI] [PubMed] [Google Scholar]
- Steenkamp MM, Nash WP, Lebowitz L, Litz BT. How best to treat deployment-related guilt and shame: Commentary on Smith, Duax, and Rauch (2013) Cognitive and Behavioral Practice. 2013;20(4):471–475. doi: 10.1016/j.cbpra.2013.05.002. [DOI] [Google Scholar]
- Steenkamp MM, Nash WP, Lebowitz L, Litz BT. How best to treat deployment-related guilt and shame: Commentary on Smith, Duax, and Rauch (2013) Cognitive and Behavioral Practice. 2013;20(4):471–475. doi: 10.1016/j.cbpra.2013.05.002. [DOI] [Google Scholar]
- Stein NR, Mills MA, Arditte K, Mendoza C, Borah AM, Resick PA, … Wright E. A scheme for categorizing traumatic military events. Behavior Modification. 2012;36(6):787–807. doi: 10.1177/0145445512446945. [DOI] [PubMed] [Google Scholar]
- Ursano RJ, Bell C, Eth S, Friedman M, Norwood A, Pfefferbaum B, … Yager J. Practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. The American Journal of Psychiatry. 2004;161(11 Suppl):3–31. doi: 10.1176/appi.books.9780890423363.52257. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL-5) National Center for PTSD; 2013. [Google Scholar]
- Wisco BE, Marx BP, Wolf EJ, Miller MW, Southwick SM, Pietrzak RH. Posttraumatic stress disorder in the US veteran population: results from the National Health and Resilience in Veterans Study. The Journal of Clinical Psychiatry. 2014;75(12):1338–1346. doi: 10.4088/JCP.14m09328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wortmann JH, Jordan AH, Weathers FW, Resick PA, Dondanville KA, Hall-Clark B, … Litz BT. Psychometric analysis of the PTSD Checklist-5 (PCL-5) among treatment-seeking military service members. Psychological Assessment. 2016 doi: 10.1037/pas0000260. [DOI] [PubMed] [Google Scholar]
- Zalta AK, Gillihan SJ, Fisher AJ, Mintz J, Mclean CP, Yehuda R, Foa EB. Change in negative cognitions associated with PTSD predicts symptom reduction in prolonged exposure. Journal of Consulting and Clinical Psychology. 2014;82:171–175. doi: 10.1037/a0034735. [DOI] [PMC free article] [PubMed] [Google Scholar]