Abstract
Local recurrence after an autologous breast reconstruction is uncommon. We describe 2 patients with local recurrence 3 and 9 years, respectively, after mastectomy with DIEAP (deep inferior epigastric artery perforator) flap breast reconstruction. Patients generally present with a palpable mass, pain, or other visible abnormalities. Various imaging techniques are helpful, always completed by biopsy to characterize the tumour. A repeated sentinel node procedure can be useful in staging. The treatment of the local recurrence needs to be determined in a multidisciplinary team consultation.
Keywords: Recurrence of breast cancer, Autologous breast reconstruction, Mammography, MRI, Ultrasound, Repeated sentinel node
Introduction
After mastectomy, DIEAP (deep inferior epigastric artery perforator) flap breast reconstruction is an increasingly popular option in delayed as well as in immediate reconstructions.
Rates of a local recurrence after a mastectomy followed by an autologous reconstruction vary between 2.1 and 11.7%, with a wide variety of disease-free intervals [1, 2, 3]. In this case report we describe 2 patients with a local recurrence after mastectomy and DIEAP flap breast reconstruction.
Case Reports
Patient A, a 42-year-old woman, underwent a right mastectomy and sentinel node procedure, with immediate DIEAP flap reconstruction. Pathology showed a pT1cN1(mi) invasive ductal carcinoma (IDC), oestrogen and progesterone receptor positive and HER2/neu negative. The patient received adjuvant chemotherapy followed by endocrine therapy, without radiation therapy.
After 3 years of uneventful follow-up, an abnormality of the right breast was identified by the patient. Physical examination showed slight erythema and oedema lateral to the scar over an area of 0.5–1 cm (Fig. 1). Ultrasound showed focal thickening of the cutis without suspicious lymph nodes (Fig. 2). Biopsy revealed an IDC, oestrogen and progesterone receptor positive and HER2/neu negative. Wide local excision of the recurrence which included the underlying subcutis was followed by a repeated sentinel node procedure. Pathology confirmed a completely removed 17-mm IDC grade III, oestrogen and progesterone receptor positive, HER2 negative, sentinel node negative. The multidisciplinary tumour board proposed radiation therapy, adjuvant chemotherapy, which the patient renounced, and aromatase inhibitors.
Fig. 1.

Patient A. Physical examination: slightly erythematous skin thickening of the right breast near the scar with a size of 0.5–1 cm. The crusta is the entrance point of the histologic needle biopsy.
Fig. 2.

Patient A. Ultrasound: focal skin thickening of 5 mm (normal cutis is 2 mm). Diffuse hypoechogenic lesion with diffuse boundaries.
Patient B, a 49-year-old woman, underwent a left mastectomy and sentinel node procedure, with immediate reconstruction with a tissue expander. Pathology showed a completely removed pT2N0 IDC grade I, oestrogen and progesterone receptor positive and HER2/neu negative. Due to an infection, the tissue expander had to be removed and subsequently the patient opted for a DIEAP flap breast reconstruction. The patient received adjuvant chemotherapy followed by endocrine therapy. However, due to vascular irritation of the chemotherapy infusions, the patient declined the last chemotherapy infusion.
After 9 years of uneventful follow-up, the patient identified a dent in combination with a pulling sensation in the left breast. Physical examination showed a palpable mass and retraction laterally (Fig. 3). Ultrasound revealed a subcutaneous suspicious area near the scar. Biopsy revealed IDC, oestrogen and progesterone receptor positive and HER2/neu negative, similar to the previously treated tumour. CT and bone scan showed no signs of metastases. The patient was treated with a wide local excision of the recurrence with a reconstruction of the resulting defect of the breast tissue followed by a repeated sentinel node procedure. Pathology confirmed a completely removed 37-mm IDC grade II, oestrogen and progesterone receptor-positive, HER2/neu negative. The sentinel node showed a macro-metastasis, staged pT2N1(sn). The multidisciplinary tumour board proposed radiation therapy of the chest wall and the lymph region, adjuvant chemotherapy, which the patient renounced, and aromatase inhibitors.
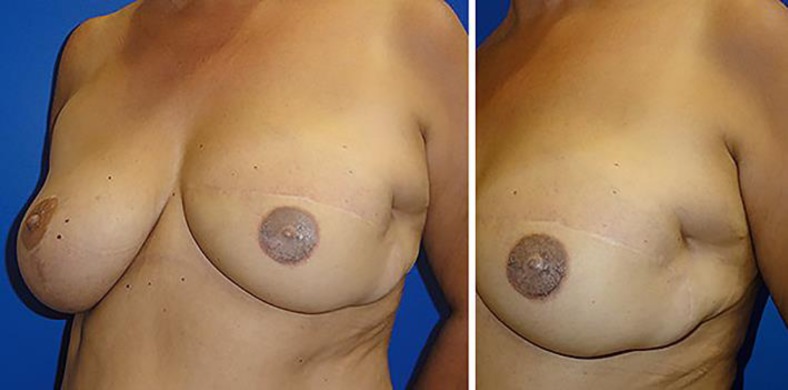
Fig. 3.
Patient B. Physical examination: palpable mass and skin retraction laterally of the reconstructed left breast.
Discussion
Retrospective research suggests that locoregional recurrence risk after mastectomy followed by breast reconstruction is similar to the risk after mastectomy alone [4, 5].
The most common area of a local recurrence is between the autogenous tissue flap and the residual breast tissue, because there is a risk that tumour cells remain after the mastectomy [6]. Because of the superficial location of this area, local recurrence can often be recognized by a palpable mass as well as pain, skin or scar changes, irregularity, or increased tenderness, all first and foremost detected by the patient [5, 6, 7, 8].
Routine mammographic screening after a DIEAP flap breast reconstruction is controversial [9]. Mammographic screening could lead to an early detection of a local recurrence before noticing a palpable mass at physical examination [10]. Postoperative benign abnormal findings such as fat necrosis (6–18% of DIEAP flap breast reconstructions and 10–24% of TRAM flap breast reconstructions) [6], oil cysts, and fibrosis could cause a palpable mass or a false-positive finding on imaging. Mammography has been described as a very sensitive test to differentiate a local recurrence from benign findings [7]. MRI, however, is often superior in differentiating between benign findings and recurrent breast cancer [11]. As a problem-solving modality, MRI is becoming the first choice in breast imaging. This holds especially true in the case of fat necrosis, which is difficult to differentiate on ultrasound or mammography [6, 12]. Ultrasound contributes to the evaluation of palpable masses. In comparison with mammography, ultrasound is better in the detection of small (< 0.5 cm) and peripheral recurrences, because the recurrences could be located outside the imaging field of the mammography [13].
A biopsy is mandatory in the case of suspicious findings on physical examination or imaging.
Treatment of a local recurrence can consist of breast-conserving surgery, given that the local recurrence is discovered in an early stage and no initial radiotherapy was used. A repeated sentinel node procedure is appropriate [14]. Adjuvant systemic treatment, preferably in combination with radiation therapy, decreases the recurrence risk.
Conclusions
A local recurrence after autologous breast reconstruction is relatively rare. It is often characterized by subtle changes like a palpable mass, pain, or a visible abnormality. Physical examination is often the proper tool to identify local recurrences because of their superficial location. Routine physical examination by both patient and physician is important. Suspicious findings are followed by imaging and biopsy, mandatory for proper further therapeutic planning.
Statement of Ethics
Patient consent to publish images was received. The authors have no ethical conflicts to declare.
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- 1.Casey WJ, 3rd, Rebecca AM, Silverman A, Macias LH, Kreymerman PA, Pockaj BA, et al. Etiology of breast masses after autologous breast reconstruction. Ann Surg Oncol. 2013 Feb;20((2)):607–14. doi: 10.1245/s10434-012-2605-y. [DOI] [PubMed] [Google Scholar]
- 2.Gerber B, Krause A, Dieterich M, Kundt G, Reimer T. The oncological safety of skin sparing mastectomy with conservation of the nipple-areola complex and autologous reconstruction: an extended follow-up study. Ann Surg. 2009 Mar;249((3)):461–8. doi: 10.1097/SLA.0b013e31819a044f. [DOI] [PubMed] [Google Scholar]
- 3.Langstein HN, Cheng MH, Singletary SE, Robb GL, Hoy E, Smith TL, et al. Breast cancer recurrence after immediate reconstruction: patterns and significance. Plast Reconstr Surg. 2003 Feb;111((2)):712–20. doi: 10.1097/01.PRS.0000041441.42563.95. [DOI] [PubMed] [Google Scholar]
- 4.Reddy S, Colakoglu S, Curtis MS, Yueh JH, Ogunleye A, Tobias AM, et al. Breast cancer recurrence following postmastectomy reconstruction compared to mastectomy with no reconstruction. Ann Plast Surg. 2011 May;66((5)):466–71. doi: 10.1097/SAP.0b013e318214e575. [DOI] [PubMed] [Google Scholar]
- 5.Patterson SG, Teller P, Iyengar R, Carlson GW, Gabram-Mendola SG, Losken A, et al. Locoregional recurrence after mastectomy with immediate transverse rectus abdominis myocutaneous (TRAM) flap reconstruction. Ann Surg Oncol. 2012 Aug;19((8)):2679–84. doi: 10.1245/s10434-012-2329-z. [DOI] [PubMed] [Google Scholar]
- 6.Hedegard W, Niell B, Specht M, Winograd J, Rafferty E. Breast reconstruction with a deep inferior epigastric perforator flap: imaging appearances of the normal flap and common complications. AJR Am J Roentgenol. 2013 Jan;200((1)):W75-84. doi: 10.2214/AJR.12.9270. [DOI] [PubMed] [Google Scholar]
- 7.Freyvogel M, Padia S, Larson K, Dietz J, Grobmyer S, O'Rourke C, et al. Screening mammography following autologous breast reconstruction: an unnecessary effort. Ann Surg Oncol. 2014 Oct;21((10)):3256–60. doi: 10.1245/s10434-014-3913-1. [DOI] [PubMed] [Google Scholar]
- 8.Howard MA, Polo K, Pusic AL, Cordeiro PG, Hidalgo DA, Mehrara B, et al. Breast cancer local recurrence after mastectomy and TRAM flap reconstruction: incidence and treatment options. Plast Reconstr Surg. 2006 Apr;117((5)):1381–6. doi: 10.1097/01.prs.0000208116.86765.4a. [DOI] [PubMed] [Google Scholar]
- 9.Barnsley GP, Grunfeld E, Coyle D, Paszat L. Surveillance mammography following the treatment of primary breast cancer with breast reconstruction: a systematic review. Plast Reconstr Surg. 2007 Oct;120((5)):1125–32. doi: 10.1097/01.prs.0000279143.66781.9a. [DOI] [PubMed] [Google Scholar]
- 10.Helvie MA, Bailey JE, Roubidoux MA, Pass HA, Chang AE, Pierce LJ, et al. Mammographic screening of TRAM flap breast reconstructions for detection of nonpalpable recurrent cancer. Radiology. 2002 Jul;224((1)):211–6. doi: 10.1148/radiol.2241010061. [DOI] [PubMed] [Google Scholar]
- 11.Dialani V, Lai KC, Slanetz PJ. MR imaging of the reconstructed breast: what the radiologist needs to know. Insights Imaging. 2012 Jun;3((3)):201–13. doi: 10.1007/s13244-012-0150-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pinel-Giroux FM, El Khoury MM, Trop I, Bernier C, David J, Lalonde L. Breast reconstruction: review of surgical methods and spectrum of imaging findings. Radiographics. 2013 Mar-Apr;33((2)):435–53. doi: 10.1148/rg.332125108. [DOI] [PubMed] [Google Scholar]
- 13.Edeiken BS, Fornage BD, Bedi DG, Sneige N, Parulekar SG, Pleasure J. Recurrence in autogenous myocutaneous flap reconstruction after mastectomy for primary breast cancer: US diagnosis. Radiology. 2003 May;227((2)):542–8. doi: 10.1148/radiol.2272011175. [DOI] [PubMed] [Google Scholar]
- 14.Vugts G, Maaskant-Braat AJ, Voogd AC, van Riet YE, Luiten EJ, Rutgers EJ, et al. Repeat sentinel node biopsy should be considered in patients with locally recurrent breast cancer. Breast Cancer Res Treat. 2015 Oct;153((3)):549–56. doi: 10.1007/s10549-015-3571-4. [DOI] [PubMed] [Google Scholar]