Abstract
Objective
The purpose of this study was to develop an integrated care pathway for doctors of chiropractic, primary care providers, and mental health professionals who manage veterans with low back pain, with or without mental health comorbidity, within Department of Veterans Affairs health care facilities.
Methods
The research method used was a consensus process. A multidisciplinary investigative team reviewed clinical guidelines and Veterans Affairs pain and mental health initiatives to develop seed statements and care algorithms to guide chiropractic management and collaborative care of veterans with low back pain. A5-member advisory committee approved initial recommendations. Veterans Affairs-based panelists (n = 58) evaluated the pathway via e-mail using a modified RAND/UCLA methodology. Consensus was defined as agreement by 80% of panelists.
Results
The modified Delphi process was conducted in July to December 2016. Most (93%) seed statements achieved consensus during the first round, with all statements reaching consensus after 2 rounds. The final care pathway addressed the topics of informed consent, clinical evaluation including history and examination, screening for red flags, documentation, diagnostic imaging, patient-reported outcomes, adverse event reporting, chiropractic treatment frequency and duration standards, tailored approaches to chiropractic care in veteran populations, and clinical presentation of common mental health conditions. Care algorithms outlined chiropractic case management and interprofessional collaboration and referrals between doctors of chiropractic and primary care and mental health providers.
Conclusion
This study offers an integrative care pathway that includes chiropractic care for veterans with low back pain.
Key Indexing Terms: Chiropractic, Veterans, Delivery of Health Care, Interprofessional Relations, Spinal Manipulation
Introduction
Of the 5.7 million patients served annually in Department of Veterans Affairs (VA) facilities, more than half experience chronic pain.1 Much of the chronic pain reported by veterans is musculoskeletal (MSK) pain,2–8 with around 25% consistently reporting low back pain (LBP).7 The prevalence of severe pain is more common in veterans with LBP than in nonveterans.9 Coincident with MSK pain, many veterans are diagnosed with mental health conditions, such as depression, anxiety, posttraumatic stress disorder (PTSD), and substance use disorders.8 Veterans with MSK pain and mental health comorbidity use more VA health care services than veterans without these conditions, including primary care, medical specialty, chronic pain, and behavioral health services.10
The widely accepted biopsychosocial model postulates that physical disease, mental health or illness, and social factors interact and contribute to the patient’s overall suffering and experience of chronic pain.11–14 Clinical practice guidelines (CPGs) and systematic reviews recommend that clinicians incorporate biopsychosocial approaches into the management of patients with LBP, including effective nonpharmacological therapies such as patient education, activity/exercise, yoga, massage, acupuncture, and spinal manipulation.15–18 However, few strategies exist to integrate these complementary therapies with conventional approaches to pain management, and little evidence is available to guide collaborative management among musculoskeletal specialists, primary care providers, and mental health professionals, all of whom are often involved in the management of patients with LBP.19
The Department of Veterans Affairs expanded its delivery of nonpharmacological treatment offerings for LBP when, in 2004, it began providing chiropractic services, including spinal manipulation, both on site at select VA facilities and through purchased care arrangements with private sector providers.20 Previous work indicates that the use of VA chiropractic services has grown substantially since its inception, as currently upward of 46,000 veterans are being served, and that doctors of chiropractic (DCs) working in VA manage LBP through the delivery of evidence-based, nonpharmacological services.21–24 Although the use of chiropractic care in VA has expanded,23 few data exist to inform optimal models of access to and delivery of chiropractic care, in VA or elsewhere.
The implementation of chiropractic services in VA presents a novel opportunity to explore strategies to improve collaborative case management for patients with LBP, including those with mental health comorbidity.24,25 One aim of our research project, Collaborative Care for Veterans with Spine Pain and Mental Health Conditions, was to develop a consensus-based, chiropractic integrated care pathway to guide clinical decision making and improve communication and referral processes between DCs, primary care providers, and mental health professionals who manage veterans with LBP in VA healthcare facilities. Care pathways are health care tools designed to support evidence-based practices, clinical decision making, and the organization of care processes for providers treating patients with well-defined health conditions, such as those with LBP.26
The purpose of this study was to develop a consensus-based, integrated care pathway for DCs, primary care providers, and mental health professionals who manage veterans with LBP, with or without mental health comorbidity, within VA health care facilities.
Methods
Project Overview
This study was part of a funded research project (R34 AT008427) designed to integrate nonpharmacological approaches into the management of pain and comorbid conditions in US military veterans seeking care in VA health care facilities.
Human Participant Considerations
This modified Delphi study was exempted by the Palmer College of Chiropractic Institutional Review Board (Approval No X2016-4-11-G, April 13, 2016) and was determined to not constitute human participant research by the University of Iowa Human Subjects Research Office (notification May 19, 2016). We received written consent and permission to publish names from all participants.
Research Participants
Three groups were integral to the development of the integrative care pathway: the investigative team, external advisors, and consensus panel. The investigative team included 10 experts in the fields of chiropractic, primary care, psychiatry, veterans’ health, clinical and health services research, and modified Delphi process methodology. This team reviewed documents, developed seed statements and algorithms, and identified external advisors and consensus panel participants. Five leaders in evidence-based chiropractic practice served as advisors who provided feedback on the initial and finals draft of the pathway. A multidisciplinary panel of VA clinicians (n = 184) were invited to serve as clinical experts for the modified Delphi process. Initial interest was received from 49 DCs employed in VA facilities throughout the United States and 21 non-DC clinicians who worked in VA health care systems located in Iowa City, Iowa, West Haven, Connecticut, and Minneapolis, Minnesota. Sixty-one potential panelists completed consent forms and submitted demographic forms.
Fifty-eight VA employees served as consensus panelists. Their mean age was 44 years (range: 28–64), the majority being male (n = 41), with a mean of 4.4 years working in VA. Eight panelists were themselves military veterans. Professions represented included chiropractic (n = 41), medicine (n = 9), physical therapy (n = 3), psychology (n = 2), and an advance practice nurse, an occupational therapist, and a dual-trained DC/physical therapist. Seven panelists also were trained in acupuncture. Fifty-six identified as clinicians, and of those, all managed spine-related pain or disability, 10 provided primary care services, and 15 managed mental health conditions. Although all panelists had extensive professional experience (mean: 15.5 years) and reported a mean number of 57 patient visits per week, most had no previous involvement as a Delphi panelist (76%) or in guideline development (59%).
Source Documents and Seed Statements
Our selection of source documents from which to develop our seed statements was based on identifying clinical guidelines and other practice-based initiatives already recommended for use within VA to support pathway integration and uptake by providers. As VA/Department of Defense (DoD) has long recommended the use of a widely accepted CPG for LBP diagnosis and treatment27 in its health care facilities, that guideline served as the source document for this care pathway. This guideline, which recommends spinal manipulative therapy for acute, subacute, and chronic LBP, outlines an algorithm for primary care providers treating LBP patients, but does not specify processes for referral and interdisciplinary communication between primary care and chiropractic clinicians, nor does it provide guidance on chiropractic care management of the LBP patient. The vision, standards, and approach of the DoD/Veterans Health Administration Pain Management Task Force further informed the development of seed statements,28 as did extant chiropractic CPG29 and best practice documents.30,31 Guidance on chiropractic treatment frequency and duration came from previous work of the VA Chiropractic Field Advisory Committee.32 Statements on mental health concerns were derived from VA’s Make the Connection website, an online resource for veterans, active duty military, friends and family, and clinicians on topics such as mental health, daily living, and transition to civilian life (http://maketheconnection.net/; accessed May 26, 2016). As revisions to the primary source document27 were published toward the end of our process,16,17 a review of the updated citations by the investigative team ensured that the care pathway adhered to these new recommendations.
Four investigators prepared the first round of seed statements in areas of their clinical and research expertise based on these source documents. Seed statements were refined through an iterative process involving the rest of the investigative team, and then organized into thematic headings. Algorithms were prepared based on those published in a recent revision of a CPG on chiropractic care for LBP29 and the clinical expertise of the investigators who were VA-based DCs. We distributed this initial draft to the external advisors, who reviewed each statement and algorithm to refine or clarify recommendations and processes. The investigative team finalized these revisions and approved this final draft for distribution to the panelists.
Modified Delphi Consensus Process
As the current VA guideline for LBP offered few details on interdisciplinary care processes that include chiropractic care for veterans with LBP conditions, we chose to conduct a modified Delphi process study to seek consensus among clinicians who work in real-world VA settings on best practices for establishing interprofessional collaboration and communication for this patient group.33 We used a modification of the RAND Corporation/University of California, Los Angeles (UCLA) consensus methodology to conduct this modified Delphi study.34 Data collection was conducted electronically, by email, with the external advisors and panelists. The chiropractic profession has used the e-Delphi process previously to develop CPGs35 and best practice documents.29–31 Nominees received an invitational e-mail that included an overview of the research grant, purpose of the care pathway, introduction to the Delphi process, and research responsibilities, including time commitment. Interested persons submitted a written consent, background form, and curriculum vitae. Investigators reviewed these materials to ensure a diverse, cross-disciplinary panel. Two mental health professionals were added when original mental health panelists withdrew because of time constraints.
During each round, panelists received a rating sheet that included the seed statements and clinical algorithms. Panelists rated the appropriateness of the content of each seed statement, with “appropriateness” defined as the expected health benefit is greater to the patient than any expected negative consequences.34 Ratings used an ordinal scale of 1 to 9 (scores 1–3 described as “highly inappropriate” and scores 7–9 as “highly appropriate”). Panelists provided a reason for any “inappropriate” ratings and supplied citations from refereed literature to facilitate revisions. Text fields were available for each seed statement to allow written comments.
Numerical responses were entered into a spreadsheet and tabulated. Verbatim comments were de-identified and entered into a word processing program. Agreement (consensus) on appropriateness was reached if a minimum of 80% of panelists rated a statement as 7, 8, or 9 and the median response score was at least 7. Investigators revised statements for which consensus was not reached and recirculated the results to the panelists until a consensus of 80% was reached. Panelists received the revised seed statements, the level of consensus achieved on the statement during the previous round, and submitted comments with rating score in a de-identified document.
The consensus process occurred between July and December 2016. Round 1 ran for 10 weeks from August to October 2016 and consisted of 43 seed statements and 3 algorithms. Round 2 was completed over 3 weeks in October 2016 and included 2 revised statements, suggestions for the deletion of 1 algorithm and revisions to a second, and a new seed statement to replace the deleted algorithm. Investigators distributed the final draft of the care pathway in December 2016, with no substantive feedback received from the panelists or external advisors. Fifty-eight panelists reviewed the pathway during round 1, and 56 panelists completed round 2.
Results
Consensus Statements: Chiropractic Integrative Care Pathway for Veterans
For patients with LBP, primary care providers may consider the use of nonpharmacological therapies with proven benefits along with other treatment options.16 Clinical practice guidelines recommend the use of spinal manipulation for adults with LBP.16 In VA, chiropractic care, including spinal manipulation, is a tier 1 integrative pain treatment modality that may be incorporated into a veteran’s patient-centered plan of care.28
The purpose of this chiropractic integrated care pathway is to define the parameters of an appropriate approach incorporating mental health and chiropractic considerations in the primary management of patients with LBP presenting for care at VA health care facilities. Mental health conditions are common among VA patients. During the course of care, DCs may identify changes in a patient’s mental health status that may require additional follow-up. Although this care pathway focuses on LBP management, it also includes an overview of common mental health comorbidities, and referral algorithms for primary care providers, mental health specialists, and chiropractors in VA settings.
Informed Consent for Clinical Care
Informed consent is the process of proactive communication between a patient and provider resulting in the patient's authorization or agreement to undergo a specific health care intervention.
Informed consent includes information about the suggested treatment approach, its potential benefits, possible risks, and availability of other treatment options.
Obtain informed consent from the patient, either verbally or in writing, within local and/or regional standards of practice.
History and Examination
Before using any intervention such as exercise, joint manipulation, or other manual therapy, obtain, at a minimum, an appropriate history and perform a regional examination of the area to be treated. These efforts must be sufficient to reach a working diagnosis, rule out probable or suspected underlying conditions that may contraindicate any intended treatment, and provide the clinical rationale for reasonable and appropriate evaluation and treatment.
- Obtain a problem-focused health history of the musculoskeletal chief complaint and any associated conditions and confirm documentation of such pertinent health information in the clinical record, including but not limited to:
-
○Symptom history
-
○Injury history, as applicable
-
○Past medical and surgical history, including response to treatment
-
○Past manual therapy history (chiropractic, osteopathic or other spinal manipulation, physical therapy, acupuncture, etc), including response to treatment
-
○Use of active care and other self-management strategies
-
○Medication review (over-the-counter and prescription medication, including opioids/narcotics)
-
○Substance use history (alcohol, tobacco, recreational drugs, prescription drug misuse)
-
○Family health and social history
-
○Review of systems
-
○
Review clinical record for information on VA disability status, service connection, non-VA disability-related claims, and designated disability rating for spine disorders and related health conditions.
- Conduct initial examination to provide diagnostic information for preliminary or differential diagnoses. Problem-focused examination may include, but is not limited to:
-
○Regional musculoskeletal and neurological exam, including symptom severity and functional deficits
-
○Cognitive status examination, including level of alertness, ability to understand and follow instructions
-
○Review of existing laboratory or other diagnostic testing
-
○Order or request the appropriate clinician order, any pertinent laboratory, or other diagnostic testing, when indicated
-
○
- The initial history and examination for patients presenting for chiropractic evaluation screens for serious pathology, or red flags, related to spine pain. Signs or symptoms leading to a clinical suspicion of serious pathology are evaluated through additional office procedures or advanced diagnostic testing (see statements on diagnostic imaging) or referred to their primary care provider for evaluation or treatment. Examples of serious pathology include, but are not limited to acute or progressing conditions such as:
-
○Progressive neurological disorders
-
○Cauda equina syndrome
-
○Malignancy
-
○Spinal infection
-
○Abdominal aortic aneurysm
-
○Fracture
-
○Articular derangements/instability
-
○Cerebral ischemic symptoms
-
○Inflammatory arthropathy (rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, etc)
-
○
Review clinical records for past or current treatment of mental health disorders; trauma-related conditions, including traumatic brain injury, PTSD, and military sexual trauma (MST); neurological conditions with behavioral components; and risk of suicide including previous suicidal attempts.
Confirm presence of psychosocial risk factors for chronic disabling LBP, such as depression, anxiety, fear-avoidance behaviors, catastrophization, somatization, pain expectations, work-related stressors, and passive coping.
Patient-Reported Outcomes
Assess patient-reported outcomes with appropriate, standardized, condition-specific, VA-approved instruments at the initial evaluation, at other treatment visits as indicated, and during formal evaluations to determine the need for continued chiropractic management.
Patient-reported outcomes for LBP may include measures of pain, condition-related disability, activities of daily living, physical and mental health function, quality of life, work capacity, and other key domains, as indicated.
Diagnostic Imaging
Routine imaging or other advanced diagnostic tests are not recommended for initial evaluation of patients with uncomplicated LBP of musculoskeletal origin. Imaging and other diagnostic tests may be indicated when patients with LBP experience severe and/or progressive neurologic deficits or if the history and/or examination cause suspicion of serious underlying pathology.
Consider imaging or other diagnostic testing when patients with LBP fail to improve following a reasonable course of care.
Coordinate ordering of diagnostic tests with the patient’s primary care provider or other referral mechanism.
Patients with persistent LBP and/or lumbar radiculopathy who may be candidates for interventional pain medicine procedures or surgery should be evaluated with magnetic resonance imaging (preferred) or computed tomography.
Case Management
Document an individualized plan of care reflective of an evidence-based treatment approach consistent with the patient’s clinical presentation, diagnosis, and any concurrent or collaborative care, which should be supported by health history and examination findings.
The management plan should include outcome assessments, case management decisions, and documentation of therapeutic interventions.
Appropriate documentation includes notation of the anatomical region(s) treated in sufficient detail to ensure that another provider with similar training would understand how to replicate the procedure(s). Detailed documentation includes, but is not limited to type of exercise, rehabilitation procedure, and manipulative or other manual therapy intervention delivered.
Provide patients with evidence-based information on their musculoskeletal complaint, such as LBP, with regard to the expected course for their specific condition, advice to remain active as appropriate, condition-specific exercises, and effective self-management options.
Encourage self-care activities that promote optimal pain management and mental health such as physical activity, regular healthy meals, good sleep quality, relaxation techniques, deep breathing, and involvement in social activities and hobbies.
Adverse Events and Side Effects
Initiate timely and appropriate follow-up, referral, or transfer to a suitable health care setting for a patient in the event of a serious adverse event following treatment or in another medical emergency.
A serious adverse event is defined as one resulting in death, life-threatening symptoms, hospitalization, or disability or requiring intervention to prevent permanent impairment or damage.
Evaluate and document side effects (such as increased pain, muscle stiffness or soreness, headache, dizziness, radiating symptoms, paresthesia, and fatigue) or adverse events from any intervention delivered including manipulation, manual therapies, and exercise at each treatment visit.
Interprofessional Communication
Frequent, ongoing communication between health care providers is a necessary feature of interprofessional collaboration for VA patients. Such interprofessional communication may occur through electronic health records, other VA-approved electronic communication systems, telephone calls, or face-to-face meetings.
If the patient’s condition is not appropriate for chiropractic management, notify primary care provider, suggest referral to other services, and provide the patient with appropriate self-management instructions, as indicated.
If significant pain or functional deficits remain after the maximum therapeutic benefit is reached with chiropractic care, consult with and/or refer patient to an appropriate provider.
Consult with or refer the patient to an appropriate provider if co-management is indicated, such as a patient who has comorbidities requiring evaluation or treatment outside the chiropractic scope of practice.
Mental Health Concerns
At any point during a course of care, patients presenting with a new, suspected, or change in a mental health condition should be assessed for the need for immediate referral to the psychiatric emergency department (concern that he or she may harm self or others, or other emergent circumstances).
Communicate with a patient’s mental health professional and/or primary care provider whenever a patient has a change in a previously diagnosed mental health problem or other comorbid condition, which may require a modification of his or her current treatment plan.
Signs and symptoms of depression: feeling sad or hopeless; loss of interest in daily activities; weight changes; sleep changes; feelings of restlessness or tiredness; feelings of unworthiness or guilt; difficulty with focus or decision making; feeling nervous or worried; drinking more alcohol or caffeine; taking more prescription or over-the-counter medications; smoking or using tobacco more. Depression may be present if a patient experiences these symptoms nearly every day for at least 2 weeks. Refer to mental health or primary care provider, as indicated.
Signs and symptoms of anxiety disorders: pounding or racing heart; feeling restless, on edge, or jumpy; trembling or shaking; difficulty breathing; feeling of fullness in throat or chest; dizziness or lightheadedness; stomachaches or nausea; trouble sleeping; feeling angry or irritable; difficulty concentrating; distraction; drinking or using drugs to numb feelings. Refer to mental health or primary care provider if patient reports a new onset or worsening of symptoms.
Signs and symptoms of PTSD: feeling upset by things that remind the patient of the trauma; nightmares; flashbacks; feeling numb or emotionally cut off from persons or things that interested them; feeling on guard, being jumpy or easily startled; feeling irritated or angry; difficulty sleeping; difficulty concentrating; drinking or using drugs to numb feelings. Refer patients with PTSD symptoms to their primary care or mental health provider.
Some signs and symptoms of bipolar disorder may overlap with and be distinguished from those of clinical depression: manic episode symptoms such as doing things one might later regret (spending lots of money, gambling, arguments, reckless sexual activity), problems with focus, racing thoughts, talking faster than usual, appearing high even if no drugs were taken, taking risks or getting into unsafe situations; and depressed episode symptoms such as feeling hopeless or sad, low energy, difficulty remembering things or making decisions, changes in eating or sleeping (more or less than usual), not enjoying life or usual activities. If symptoms are present, refer to the appropriate provider.
Survivors of MST may be female, male, or transgender persons. Be aware of the mental health difficulties survivors of MST may experience: strong emotions (depression, anger, irritability), sudden emotional responses, feeling emotionally flat or numb, trouble feeling love or happiness, trouble sleeping including nightmares, trouble with attention and concentration, problems with alcohol or drugs, troubles with reminders of sexual trauma, problems trusting others or in relationships, sexual issues, chronic pain, weight or eating problems, stomach or bowel problems. Modify treatment visits as outlined above. Refer patients with a new onset or worsening of these concerns to an appropriate provider, as indicated.
Ask patient about the use of alcohol, tobacco, marijuana, prescription pain medications including opioids, and illicit/street drugs as strategies to manage pain or cope with mental health problems, and determine if the patient is willing to accept a referral for substance abuse or tobacco cessation treatment. Refer patients who are receptive to the appropriate provider or clinic, as indicated.
Patients with acute or chronic pain may experience insomnia or difficulty sleeping. If patient reports problem with sleep that is not improved following chiropractic treatments for their pain, consider referral to primary care or mental health provider, as indicated.
Offer patients VA-sponsored online resources for additional information about managing their pain and mental health, at the initial visit or as indicated.
Document mental health history findings if indicated. Communicate with and/or refer to primary care or mental health provider, if indicated.
Chiropractic Treatment Frequency and Duration
Recommended chiropractic treatment frequency and duration for VA patients with spine-related symptoms as outlined in Table 1.
Table 1.
Chiropractic Treatment Frequency and Duration
| Recommended Chiropractic Treatment Frequency and Duration for VA Patients With Spine-Related Symptoms | |||
|---|---|---|---|
|
| |||
| Type of Case | Maximum Visits to Reach Initial Minimum Clinically Important Improvement |
Subsequent Visits to Reach Additional Clinically Important Improvement |
No Further Improvement (Resolved or Patient Plateaus With Residual Symptomsa) |
| Acute episode, uncomplicated | ≤6 visits within 3 wkb | ≤4 visits within 3 wk | Endpoint of trial of chiropractic care |
| Acute episode, complicated | ≤6 visits within 3 wkb | ≤6 visits within 3 wk | Endpoint of trial of chiropractic care |
| Chronic condition | ≤8 visits within 6 wk | ≤4 visits within 4 wk | Endpoint of trial of chiropractic care |
|
| |||
| Definitions | |||
| Minimum clinically important improvement: The threshold of a beneficial patient-oriented change that can be ascribed to treatment effects. Objective measures of such are a decrease of ≥2 points on the NPRS, and/or a decrease in ≥10 points on the Oswestry Disability Questionnaire, and/or similar improvement on other comparable outcome measures. | |||
| Complicated case: Presence of one or more of the following: severe pain (8, 9, or 10 on NPRS); history of ≥4 prior episodes; pain duration N8 days; structural pathology/anomaly; relevant comorbid conditions. | |||
| Chronic condition: Condition that has been present for >3 mo and typically has failed other treatment approaches. | |||
Source. Chiropractic Field Advisory Committee, 2013.32
NPRS, numerical pain rating scale; VA, Department of Veterans Affairs.
Additional chiropractic manipulative therapy or other palliative/supportive care for pain management may be indicated for patients with chronic conditions whose function decreases and/or pain increases after a withdrawal of chiropractic care. This added course of chiropractic management may be appropriate for patients engaged in active care strategies, if other indicated medical and psychosocial treatment options have been considered and/or included in the overall VA pain management plan.
If there has been no reasonable benefit within the initial treatment plan period, continuation of chiropractic manipulative therapy requires a substantial change in treatment plan
Modifying Manual Therapy Procedures
Patients with musculoskeletal pain, including those with or without a history of PTSD, MST, or other exposure to interpersonal violence, may have varying reactions to unexpected touch, have difficulty relaxing, and/or exhibit guarding behaviors.
Patients also may be startled easily or feel unsafe in situations that remind them of past trauma. Chiropractic treatments and other manual therapy procedures may require modification to address these concerns.
Describe any touch-based interactions before initiating, especially those that occur outside the patient’s visual field, and ask for permission to enter a patient’s personal space.
Inform patients of any sounds or activities (eg, table drops or instrument sounds) that might be startling during the office visit.
Carefully consider person positioning within the examination or treatment room, as well as the patient’s positioning during both examination and treatment to afford the patient the ability to maintain a sense of control and safety at all times during a visit.
Consider the possibility of including or allowing a chaperone/support person to accompany the patient during the visit.
Algorithms for Chiropractic Care in Veterans Affairs Healthcare Facilities
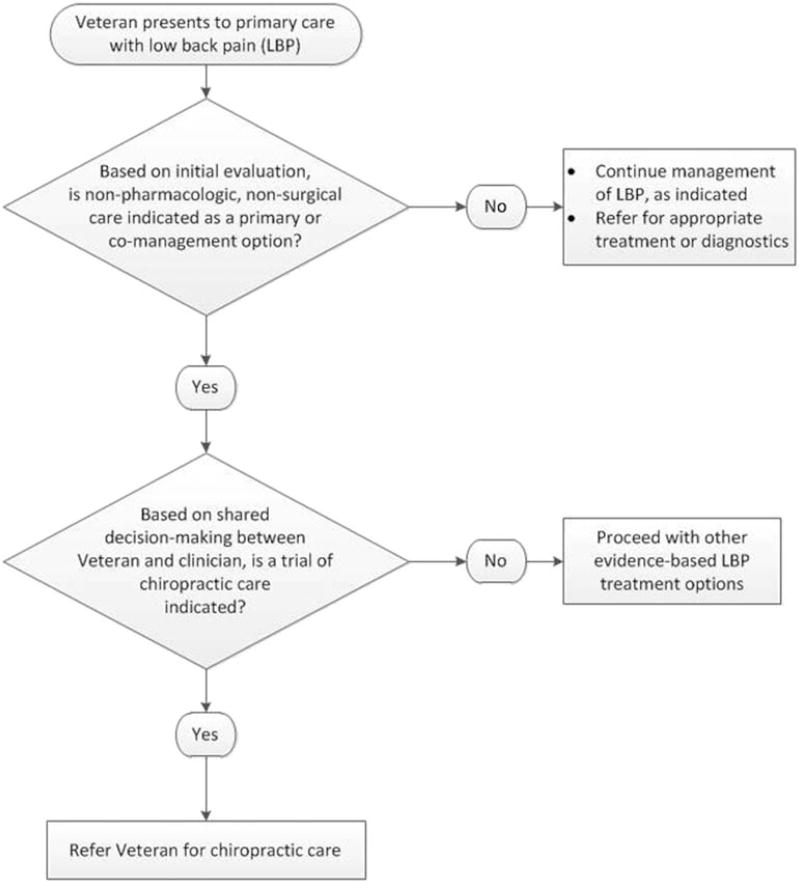
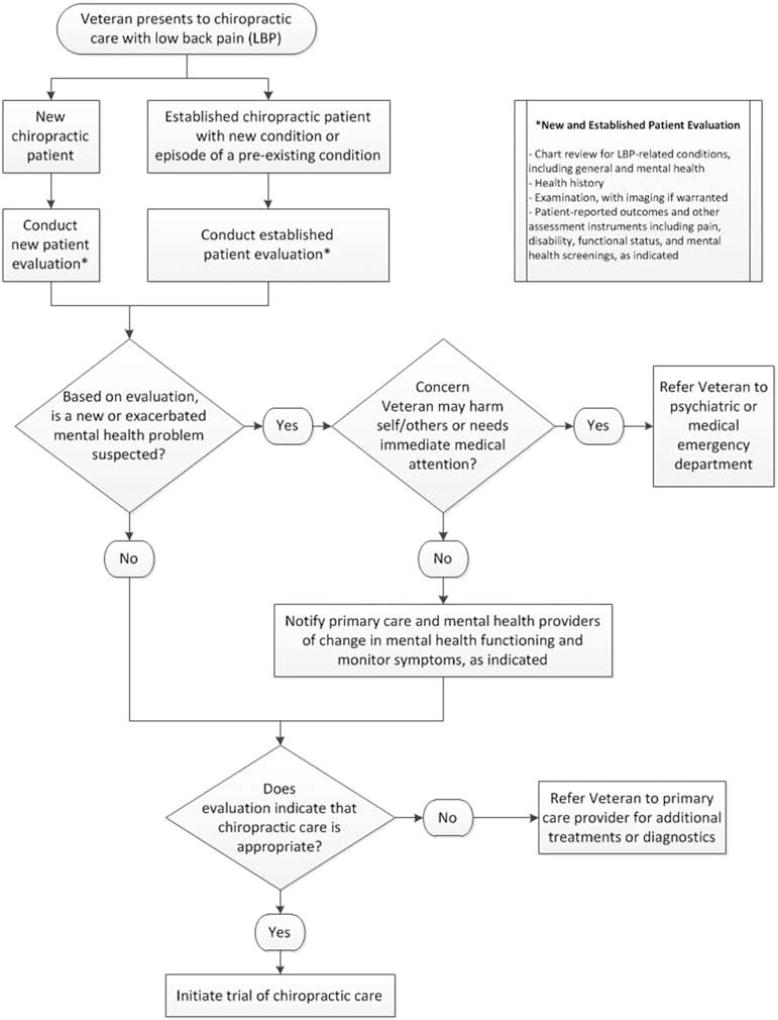
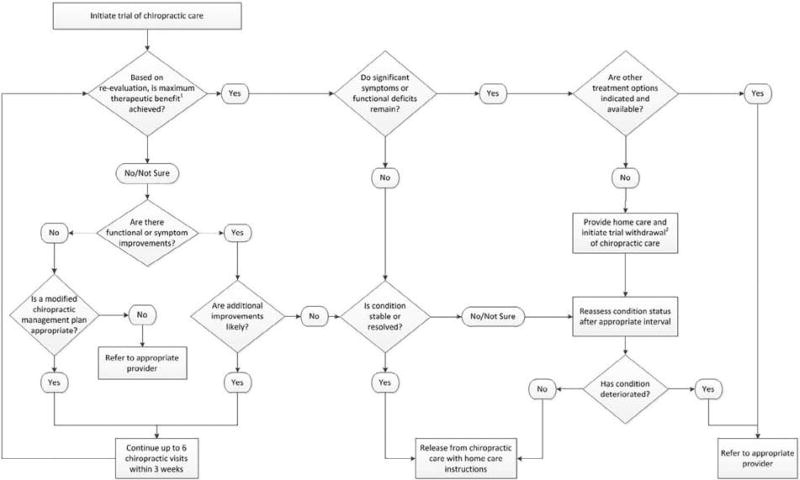
An algorithm for primary care referrals to chiropractic care for veterans with LBP is outlined in Figure 1. The algorithm for the initiation of chiropractic care is outlined in Figure 2. The algorithm for chiropractic case management, applicable to both acute and chronic LBP, is outlined in Figure 3. Initial dosing should be guided by the information provided in Table 1.
Fig 1.
Algorithm for primary care referrals to chiropractic care for veterans with low back pain.
Fig 2.
Algorithm for the initiation of chiropractic care.
Fig. 3.
Algorithm for chiropractic case management, applicable to both acute and chronic low back pain. Chiropractic Case Management Algorithm Notes: 1Maximum therapeutic benefit: Further improvement in symptoms or condition cannot be reasonably expected and treatment is not considered necessary to prevent an immediate decline in status. 2Trial withdrawal may be necessary when a patient reaches maximum therapeutic benefit to determine if condition recovery is stable. If condition deteriorates after the trial, then ongoing care may be necessary to maintain function and minimize symptoms. The therapeutic withdrawal can be gradual, where the patient’s care is reduced through tapered visits. It can also be rapid, with the patient instructed to return for care or evaluation only if symptoms recur or worsen. The patient can be scheduled for an evaluation at a later date to evaluate for signs of regression.
Discussion
To our knowledge, this is the first chiropractic integrated care pathway for veterans with LBP, with or without comorbid mental illness, that proposes a standardized approach to interdisciplinary referral to chiropractic services and for chiropractic case management in VA health care settings. This care pathway is based on available LBP clinical practice guidelines,16,27 existing VA care processes and pain management initiatives,28 expert opinion, and achieved consensus among our consensus panelists. This pathway includes spinal manipulation, a central component of chiropractic care, which is congruent with the findings of a widely cited systematic review.36 Clinicians may use the pathway to guide clinical decision making and improve communication and referral processes, particularly between primary care providers, mental health professionals, and DCs who are involved in treating veterans with LBP. Because interprofessional collaboration among all health care providers is challenging37 and the degree of chiropractic integration varies by facility,20 this pathway also may be useful to health care administrators in VA or other multidisciplinary clinical settings seeking to integrate chiropractic care into their offered services.
This care pathway presents chiropractic treatment schedules for uncomplicated acute LBP (≤6–10 visits over 6 weeks), complicated acute LBP (≤6–12 visits over 6 weeks), and chronic LBP (≤12 visits over 10 weeks) based on expert clinical opinion and achieved consensus among our consensus panelists.32 These treatment recommendations are of different frequency dosages than those producing clinically important outcomes for chronic LBP (12–18 weekly visits) in randomized controlled trials conducted outside VA settings.38,39 The typical chiropractic visit in VA is 30 minutes in duration, compared with 15 minutes in the large published trial.39 Thus, further research is needed to determine the optimal dose of chiropractic care to manage LBP and other MSK complaints in veteran populations, whose physical health and mental well-being may differ from those of community-based chiropractic patients.
This pathway addressed multimodal chiropractic care, rather than focusing on spinal manipulation as an isolated treatment modality. However, recommendations for specific elements of multimodal chiropractic care (eg, patient education, manual techniques, exercise) were beyond the scope of this project.
We did not address the use of specific clinical assessment tools, including instruments designed to determine the risk of delayed recovery or persistent disability from LBP, as many such tools have not yet been validated in veteran populations. We also did not address the use of patient-reported experience measures, such as patient expectations and satisfaction with care, again because of the lack of standardized, validated instruments for use in VA patients seeking chiropractic care. The DoD/Veterans Health Administration Pain Management Task Force guidance28 does recommend some specific instrumentation for pain assessment as outlined in this clinical pathway; however, many measures currently in use in VA settings are those preferred by individual providers or instituted by clinical departments.
Strengths and Limitations
One strength of this study was our interdisciplinary research team, which included several members who are practicing VA chiropractors or who, along with our advisory committee members, have developed clinical practice guidelines in the past. In addition, we convened a large, interdisciplinary panel of VA clinicians, including more than 40 DCs, who have varied and diverse expertise in the care of veterans with musculoskeletal conditions and mental health concerns to serve as consensus panelists. This panel came to consensus on seed statements and algorithms that we based on established clinical guidelines and educational modules approved for use in VA settings.
Although we used these multidisciplinary CPGs as source documents, some seed statements and aspects of the clinical algorithms developed during this study were based on our knowledge of existing VA care processes and expert opinion on the appropriateness of these processes, neither of which has been evaluated in experimental studies. As our process was to base seed statements on CPGs currently in use in VA settings, we used a nonstructured search strategy to locate such documents on VA/DoD clinical practice guideline and educational sites and did not assess the quality of these sources with independent assessors using validated tools. Other potentially informative documents might have been uncovered with the use of different search strategies.
There also may be important limitations when implementing the pathway in different VA contexts. This pathway is limited to care provided on station at VA facilities where DCs are integrated into team-based management. Generalizability beyond these settings is unknown. Doctor of chiropractic representation on the panel was geographically diverse, although input from other health professionals was reserved to staff members of 3 VA facilities. Research on the process of implementing chiropractic,20 evidence-based guidelines,40 patient-centered medical homes,41 and other care processes42 within VA has been observed to vary at the institutional level. Therefore, VA providers may find they need to tailor this care pathway for their facility. Our team planned to solicit feedback from VA patients on the pathway during its development, but patient recruitment was not possible in the study time frame. We will seek input from veterans during a pilot trial that will investigate the feasibility and acceptability of this pathway for guiding chiropractic treatments for VA patients.
Conclusions
This article offers an integrated care pathway for chiropractic management of veterans with LBP, with or without mental health comorbidity. The pathway was developed by VA-based DCs, primary care providers, mental health professionals, and clinical experts in the field of veterans’ health. The pathway provides a reasonable approach to multidisciplinary care for veterans with acute and chronic LBP.
Practical Applications.
This care pathway provides an evidence-based approach to chiropractic management of low back pain in veterans with or without mental health comorbidity.
The pathway offers a framework for interprofessional communication and referral between doctors of chiropractic, primary care providers, and mental health professionals caring for veterans.
Acknowledgments
We thank Virginia Smith, MS, for coordinating the Delphi process. We also thank our external advisory committee members for their expert feedback on this study: Scott Haldeman, DC, MD, PhD, Michael Schneider, DC, PhD, Donald Murphy, DC, Wayne Whalen, DC, and Anthony Hamm, DC. The feedback from the many Delphi panelists who participated in this study was both essential to its successful completion and an exemplar to the dedicated service these health professionals provide to veterans. The Delphi panelists were Michael Anderson, DC, MS, Anthony Battaglia, DC, Keith E. Biggs, DC, Gina M. Bonavito-Larragoite, DC, Kimberly S. Brown, DC, MA, Glenn A. Bub, DC, Nathan Campbell, DC, Michael Clay, DC, MPH, Ramon Cuevas-Trisan, MD, Clinton Daniels, DC, MS, Ryan Diana, DC, Amanda Dluzniewski, DC, Paul Dougherty, DC, Stephen C. Ezeji-Okoye, MD, Lance Formolo, DC, MS, Richard S. Forrette, DC, Ryan Furniss, DC, Jason L. Gibson, DC, Jordan Gliedt, DC, Justin Goehl, DC, MS, Derek J. Golley, DC, MS, Kelly Grover, PhD, Paul Heideman, PhD, Nathan A. Hinkeldey, DC, Benjamin Kligler, MD, MPH, Katherine Krivan, DC, JoEllen Kubik, MSN, ARNP, Molly J. Lahn, PhD, DPT, Ralph Magnuson, PT, Lindsay A. Marth, MA, OT, Kevin S. Mathers, DC, DPT, Timothy Mellin, DC, Jason Napuli, DC, MBA, Michele Neal, DC, MA, Casey Okamoto, DC, Juli L. Olson, DC, MA, David Paris, DC, Rachel Perrucci, DC, Christopher Pierson, DC, Lindsay Rae, DC, Henri J. Roca, MD, Cassandra Rosenberg, MD, Gary Rubenstein, DC, Todd S. Rubley, DC, Michael Saenger, MD, Kerry Sarnowski, DC, Christopher R. Sherman, DC, MPH, Kevin Stemple, PT, MBA, William Tellin, DC, Christopher C. Toney, DC, Pamela Wakefield, DC, Robert Walsh, DC, Jeffrey Warner, DC, MPH, Susan Wenberg, DC, MA, Clint Williamson, DC, and Bradley Zupancich, DC.
Funding Sources
The Collaborative Care for Veterans with Spine Pain and Mental Health Conditions study was funded by Grant R34AT008427 from the National Institutes of Health, National Center for Complementary and Integrative Health. Drs. Salsbury, Hawk, Vining, Wallace, Long, and Goertz report grant support from NIH/NCCIH for the work reported in this article. Dr. Goertz reports receipt of personal fees from the PCORI Board of Governors and the American Chiropractic Association for activities outside the submitted work.
Footnotes
Conflicts of Interest
Drs. Lisi, Branson, and Burgo-Black reported nothing to disclose.
Contributorship Information
Concept development (provided idea for the research): S.A.S., C.M.G.
Design (planned the methods to generate the results): A.J.L., S.A.S., C.H., R.D.V., C.M.G.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): A.J.L., S.A.S., C.H., R.D.V., C.M.G.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): A.J.L., S.A.S., C.H., R.D.V., R.B.W., R.B., C.R.L., A.L.B.-B., C.M.G.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): A.J.L., S.A.S., C.H., R.D.V., C.R.L., C.M.G.
Literature search (performed the literature search): A.J.L., S.A.S., C.H., R.D.V.
Writing (responsible for writing a substantive part of the manuscript): A.J.L., S.A.S., C.H., R.D.V.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): A.J.L., S.A.S., C.H., R.D.V., R.B.W., R.B., C.R.L., A.L.B.-B., C.M.G.
References
- 1.US House of Representatives. Between Peril and Promise: Facing the Dangers of VA’s Skyrocketing Use of Prescription Painkillers to Treat Veterans. Washington, DC: House Committee on Veterans’ Affairs, Subcommittee on Health; 2013. [Google Scholar]
- 2.Higgins DM, Kerns RD, Brandt CA, et al. Persistent pain and comorbidity among Operation Enduring Freedom/Operation Iraqi Freedom/Operation New Dawn veterans. Pain Med. 2014;15(5):782–790. doi: 10.1111/pme.12388. [DOI] [PubMed] [Google Scholar]
- 3.Barry LC, Guo Z, Kerns RD, Duong BD, Reid MC. Functional self-efficacy and pain-related disability among older veterans with chronic pain in a primary care setting. Pain. 2003;104(1–2):131–137. doi: 10.1016/s0304-3959(02)00471-2. [DOI] [PubMed] [Google Scholar]
- 4.Kerns RD, Otis J, Rosenberg R, Reid MC. Veterans’ reports of pain and associations with ratings of health, health-risk behaviors, affective distress, and use of the healthcare system. J Rehabil Res Dev. 2003;40(5):371–379. doi: 10.1682/jrrd.2003.09.0371. [DOI] [PubMed] [Google Scholar]
- 5.Lew HL, Otis JD, Tun C, Kerns RD, Clark ME, Cifu DX. Prevalence of chronic pain, posttraumatic stress disorder, and persistent postconcussive symptoms in OIF/OEF veterans: polytrauma clinical triad. J Rehabil Res Dev. 2009;46(6):697–702. doi: 10.1682/jrrd.2009.01.0006. [DOI] [PubMed] [Google Scholar]
- 6.Gironda RJ, Clark ME, Massengale JP, Walker RL. Pain among Veterans of Operations Enduring Freedom and Iraqi Freedom. Pain Med. 2006;7(4):339–343. doi: 10.1111/j.1526-4637.2006.00146.x. [DOI] [PubMed] [Google Scholar]
- 7.Goulet JL, Kerns RD, Bair M, et al. The musculoskeletal diagnosis cohort: examining pain and pain care among veterans. Pain. 2016;157(8):1696–1703. doi: 10.1097/j.pain.0000000000000567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kelsall HL, McKenzie DP, Forbes AB, Roberts MH, Urquhart DM, Sim MR. Pain-related musculoskeletal disorders, psychological comorbidity, and the relationship with physical and mental well-being in Gulf War veterans. Pain. 2014;155(4):685–692. doi: 10.1016/j.pain.2013.12.025. [DOI] [PubMed] [Google Scholar]
- 9.Nahin RL. Severe pain in veterans: the effect of age and sex comparisons with the general population. J Pain. 2017;18(3):247–254. doi: 10.1016/j.jpain.2016.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beehler GP, Rodrigues AE, Mercurio-Riley D, Dunn AS. Primary care utilization among veterans with chronic musculoskeletal pain: a retrospective chart review. Pain Med. 2013;14(7):1021–1031. doi: 10.1111/pme.12126. [DOI] [PubMed] [Google Scholar]
- 11.Outcalt SD, Kroenke K, Krebs EE, et al. Chronic pain and comorbid mental health conditions: independent associations of posttraumatic stress disorder and depression with pain, disability, and quality of life. J Behav Med. 2015;38(3):535–543. doi: 10.1007/s10865-015-9628-3. [DOI] [PubMed] [Google Scholar]
- 12.Waddell G. 1987 Volvo award in clinical sciences. A new clinical model for the treatment of low-back pain. Spine (Phila Pa 1976) 1987;12(7):632–644. doi: 10.1097/00007632-198709000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Kroenke K, Wu J, Bair MJ, Krebs EE, Damush TM, Tu W. Reciprocal relationship between pain and depression: a 12-month longitudinal analysis in primary care. J Pain. 2011;12(9):964–973. doi: 10.1016/j.jpain.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gliedt JA, Schneider MJ, Evans MW, King J, Eubanks JE., Jr The biopsychosocial model and chiropractic: a commentary with recommendations for the chiropractic profession. Chiropr Man Therap. 2017;25:16. doi: 10.1186/s12998-017-0147-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wong JJ, Côté P, Sutton DA, et al. Clinical practice guidelines for the noninvasive management of low back pain: a systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Eur J Pain. 2017;21(2):201–216. doi: 10.1002/ejp.931. [DOI] [PubMed] [Google Scholar]
- 16.Chou R, Deyo R, Friedly J, et al. Nonpharmacologic therapies for low back pain: a systematic review for an American College of Physicians clinical practice guideline. Ann Intern Med. 2017;166(7):493–505. doi: 10.7326/M16-2459. [DOI] [PubMed] [Google Scholar]
- 17.Qaseem A, Wilt TJ, McLean RM, Forciea MA. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166(7):514–530. doi: 10.7326/M16-2367. [DOI] [PubMed] [Google Scholar]
- 18.Kamper SJ, Apeldoorn AT, Chiarotto A, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: Cochrane systematic review and meta-analysis. BMJ. 2015;350:h444. doi: 10.1136/bmj.h444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cosio D, Lin EH. Effects of a pain education program in complementary and alternative medicine treatment utilization at a VA medical center. Complement Ther Med. 2015;23(3):413–422. doi: 10.1016/j.ctim.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 20.Lisi AJ, Khorsan R, Smith MM, Mittman BS. Variations in the implementation and characteristics of chiropractic services in VA. Med Care. 2014;52(12 suppl 5):S97–S104. doi: 10.1097/MLR.0000000000000235. [DOI] [PubMed] [Google Scholar]
- 21.Dunn AS, Passmore SR. Consultation request patterns, patient characteristics, and utilization of services within a Veterans Affairs medical center chiropractic clinic. Mil Med. 2008;173(6):599–603. doi: 10.7205/milmed.173.6.599. [DOI] [PubMed] [Google Scholar]
- 22.Lisi AJ, Goertz C, Lawrence DJ, Satyanarayana P. Characteristics of Veterans Health Administration chiropractors and chiropractic clinics. J Rehabil Res Dev. 2009;46(8):997–1002. doi: 10.1682/jrrd.2009.01.0002. [DOI] [PubMed] [Google Scholar]
- 23.Lisi AJ, Brandt CA. Trends in the use and characteristics of chiropractic services in the Department of Veterans Affairs. J Manipulative Physiol Ther. 2016;39(5):381–386. doi: 10.1016/j.jmpt.2016.04.005. [DOI] [PubMed] [Google Scholar]
- 24.Green BN, Johnson CD, Daniels CJ, Napuli JG, Gliedt JA, Paris DJ. Integration of chiropractic services in military and veteran health care facilities: a systematic review of the literature. J Evid Based Complement Altern Med. 2016;21(2):115–130. doi: 10.1177/2156587215621461. [DOI] [PubMed] [Google Scholar]
- 25.Dunn AS, Green BN, Gilford S. An analysis of the integration of chiropractic services within the United States military and veterans’ health care systems. J Manipulative Physiol Ther. 2009;32(9):749–757. doi: 10.1016/j.jmpt.2009.10.009. [DOI] [PubMed] [Google Scholar]
- 26.Schrijvers G, van Hoorn A, Huiskes N. The care pathway: concepts and theories: an introduction. Integr Care. 2012;12:e192. doi: 10.5334/ijic.812. (Spec Ed Integrated Care Pathways) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147(7):478–491. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 28.Office of the Army Surgeon General. Pain Management Task Force, Final Report. Falls Church, VA: Office of the Surgeon General; 2010. [Google Scholar]
- 29.Globe G, Farabaugh RJ, Hawk C, et al. Clinical practice guideline: chiropractic care for low back pain. J Manipulative Physiol Ther. 2016;39(1):1–22. doi: 10.1016/j.jmpt.2015.10.006. [DOI] [PubMed] [Google Scholar]
- 30.Hawk C, Schneider M, Dougherty P, Gleberzon BJ, Killinger LZ. Best practices recommendations for chiropractic care for older adults: results of a consensus process. J Manipulative Physiol Ther. 2010;33(6):464–473. doi: 10.1016/j.jmpt.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 31.Hawk C, Schneider M, Evans MW, Jr, Redwood D. Consensus process to develop a best-practice document on the role of chiropractic care in health promotion, disease prevention, and wellness. J Manipulative Physiol Ther. 2012;35(7):556–567. doi: 10.1016/j.jmpt.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 32.VHA Chiropractic Field Advisory Committee. General Guidance on Chiropractic Treatment Frequency and Duration. West Haven, CT: Veterans Health Administration Chiropractic Program Office; 2013. [Google Scholar]
- 33.Hsu CC, Sandford BA. The Delphi technique: making sense of consensus. Pract Assess Res Eval. 2007;12(10):1–8. [Google Scholar]
- 34.Fitch K, Bernstein SJ, Aguilar MD, et al. The RAND/UCLA Appropriateness Method User’s Manual. Santa Monica, CA: RAND Corporation; 2001. [Google Scholar]
- 35.Bussières AE, Peterson C, Taylor JA. Diagnostic imaging practice guidelines for musculoskeletal complaints in adults - an evidence-based approach: introduction. J Manipulative Physiol Ther. 2007;30(9):617–683. doi: 10.1016/j.jmpt.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 36.Paige NM, Miake-Lye IM, Booth M, et al. Association of spinal manipulative therapy with clinical benefit and harm for acute low back pain: systematic review and meta-analysis. JAMA. 2017;317(14):1451–1460. doi: 10.1001/jama.2017.3086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Koenig CJ, Maguen S, Daley A, Cohen G, Seal KH. Passing the baton: a grounded practical theory of handoff communication between multidisciplinary providers in two Department of Veterans Affairs outpatient settings. J Gen Intern Med. 2013;28(1):41–50. doi: 10.1007/s11606-012-2167-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Haas M, Groupp E, Kraemer DF. Dose-response for chiropractic care of chronic low back pain. Spine J. 2004;4(5):574–583. doi: 10.1016/j.spinee.2004.02.008. [DOI] [PubMed] [Google Scholar]
- 39.Haas M, Vavrek D, Peterson D, Polissar N, Neradilek MB. Dose-response and efficacy of spinal manipulation for care of chronic low back pain: a randomized controlled trial. Spine J. 2014;14(7):1106–1116. doi: 10.1016/j.spinee.2013.07.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lyons SS, Tripp-Reimer T, Sorofman BA, et al. VA QUERI informatics paper: information technology for clinical guideline implementation: perceptions of multidisciplinary stakeholders. J Am Med Inform Assoc. 2005;12(1):64–71. doi: 10.1197/jamia.M1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nelson KM, Helfrich C, Sun H, et al. Implementation of the patient-centered medical home in the Veterans Health Administration: associations with patient satisfaction, quality of care, staff burnout, and hospital and emergency department use. JAMA Intern Med. 2014;174(8):1350–1358. doi: 10.1001/jamainternmed.2014.2488. [DOI] [PubMed] [Google Scholar]
- 42.Im JJ, Shachter RD, Oliva EM, Henderson PT, Paik MC, Trafton JA. Association of care practices with suicide attempts in US veterans prescribed opioid medications for chronic pain management. J Gen Intern Med. 2015;30(7):979–999. doi: 10.1007/s11606-015-3220-y. [DOI] [PMC free article] [PubMed] [Google Scholar]