Abstract
Background:
The incidence of cervical cancer in younger women remains high. This is worrisome as it affects future generations. Therefore Malaysia implements human papilloma virus (HPV) vaccination as a national vaccination program. Parents play an important role in determining the success of this HPV vaccination program among school-aged girls by their compliance. Objective: To assess parental knowledge, decision-making and acceptance of HPV vaccination.
Methods:
This cross sectional study was conducted among 280 randomly selected parents of primary school students aged 11 in Kota Bharu using a pre-validated self-administered questionnaire to assess knowledge and decision-making with regard to HPV vaccination.
Results:
Most parents (62%) were shown to have poor knowledge while most decision-making was shared. Age of respondents (adjusted odds ratio ‘AOR’= 1.09; 95% confidence interval ‘CI’= 1.04-1.14; p <0.001) and good knowledge of HPV vaccination (AOR= 16.32; 95% CI= 7.32-36.4; p <0.001) were significantly associated with HPV vaccine acceptance.
conclusion:
The majority of parents exhibited poor knowledge which may affect their decision-making and uptake of HPV vaccination among their children. This highlights the need to better educate parents on HPV vaccination.
Keywords: HPV vaccination, knowledge, decision making, acceptance, parents
Introduction
Cancer is one of the common causes of death in Malaysia. Cervical cancer is ranked second among all cancers in Malaysian women aged 15 to 44 years after breast cancer (ICO Malaysia, 2014). This is a worrisome as it occurs in their prime productive years. In Kelantan, cervical cancer is the 5th leading cancer and ranked 2nd after breast cancer among women for the period of 1999 till 2003 (ICO Malaysia, 2014). Even from 2007 till 2011 cervical cancer was the 10th commonest cancer among female population in Kelantan (Kelantan Cancer Registry, 2012). The ultimate cause of cervical cancer is Human Papilloma Virus infection (CPG Malaysia, 2003; Zaridah, 2014). The most frequent HPV oncogenic types among women with invasive cervical cancer by histology in Malaysia are HPV 16 and HPV 18 (ICO Malaysia, 2014).
Overall, cervical cancer mortality ranks as the 5th leading cause of cancer deaths in women with more than 600 new cervical cancer deaths occur annually in Malaysia (ICO Malaysia, 2014). The majority of cases are squamous cell carcinoma followed by adenocarcinoma (CPG Malaysia, 2003). Most women in developing countries, clinically presented with advanced stages. Although Pap smear is the most widely used screening method for cervical cancer since 1960s, no reduction in cervical cancer prevalence has been documented (Othman, 2002). The National Health and Morbidity Survey of Malaysia revealed that national prevalence of pap smear performed was only 43.7% where only 59.7% done within the last 3 years (NHMS III, 2006). Furthermore Othman et al., (2004) has shown between 2000 and 2006, among cervical cancer who were diagnosed in Malaysian hospitals, 48% reported never had a pap smear and 95% did not have a smear within the past three years. There was an overall low uptake of cervical cancer screening.
In 2006, US Food and Drug Administration (FDA) approved prophylactic vaccine of HPV. Aged between 9 to 26 years are recommended (MMWR Morbidity and mortality weekly report. 2010). The vaccines are made from non-infectious HPV virus-like particles (VLPs). There are two types of vaccine which are licensed by FDA. The bivalent HPV (Cervarix) prevents the 16 and 18 HPV types, which cause 70% of cervical cancers. The quadrivalent vaccine (Gardasil) prevents four HPV types 6, 11, 16, 18, which type 6 and 11 can cause 90% genital warts. Only the quadrivalent vaccine is used for males. Both of the vaccines have no therapeutic effect on HPV-related disease. However both vaccines have shown excellent efficacy and safety. Ideally quadrivalent HPV vaccine is routinely recommended, as 90.7-100% effective in preventing infection of the four HPV types, safe, and halal (Kane et al., 2006).
Malaysia is the first country in the Southeast Asia region to implement national HPV immunization programs under the Ministry of Health’s School Health Unit program, which is a free vaccination program on 13 years old girls in government and private schools starting in 2010. This voluntary HPV immunization program, given at 0, 1, and 6 months schedule of a 3-dose program within school calendar year (Saidatul and Rohani, 2010) requires parental written consent. A cross-sectional study among mothers in 2007 showed 65.7% accepted HPV vaccine for their daughters. However, many of mothers (83.9%) were unwilling to vaccinate their children if they had to pay but the acceptability rate increased to 97.8% if it was routine and freely available (Sam et al., 2009).
Since parents play an effective role in determining the HPV vaccine uptake, assessment of the knowledge towards HPV vaccination is important to reduce the risk among future generation. Thus, the aims of this study were to assess parental knowledge, decision making and acceptance of HPV vaccination following the implementation of the vaccination program in the country.
Materials and Methods
Setting and design
This school-based cross sectional study was conducted among parents of standard 5 at 10 primary schools in Kota Bharu.
Sample size
Sample size was calculated using a single proportion formula. The reference proportion of good knowledge of HPV vaccination was based on a previous study done in Thailand which was 20.6% (Archin et al., 2012). Taking the precision of 0.05 with 95% confidence, the minimum required sample size was 255. However, after considering the non-response rate of 30%, the sample size calculated was 330.
Sampling method
In order to achieve the study aim in assessing parents of potential HPV vaccines among school-aged girls, the study respondents (the parents) were chosen by randomly sampling the children who were students in selected schools. Only students who have female siblings aged 9 to 12 were included in order to assess the parents of potential HPV vaccines. A list of 96 primary schools in Kota Bharu was identified and 10 schools were chosen as the primary sampling unit in this two-stage random sampling. The selection of schools was purposely determined by the local authorities based on the administrative ground. The sample units were parents of the Standard 5 students (ages of 11 year old). Standard 6 students were not chosen as Ministry of Education Malaysia does not encourage research to be conducted on students who are taking national exams.
Three classes were selected from all Standard 5 classes in each school by simple random sampling. Eleven students were selected by a systematic random sampling from the list of students in the selected classes. There were 35 to 40 students in each selected class.
Research tools
A self-administered questionnaire was used which has 4 sections: socio-demographic data, knowledge on HPV vaccination, decision-making and acceptance of HPV vaccination.
Socio-demographic data consisted of 8 questions regarding age; gender; race; relationship with student; marital status; education level; employment status and household income. Knowledge on HPV vaccination was a modified questionnaire to assess knowledge of HPV vaccination among parents of primary school students (Archin et al., 2012; Al Dubai et al., 2010). The questionnaire development was done in stages. The first stage involved reviewing the literatures on knowledge on HPV vaccination among parents, students, teachers and women to develop questionnaire items. Then, these items were arranged into domains. In the second stage, several series of discussion were done to get the expert opinions, in order to ensure good content validity and comprehensiveness of the questionnaire. All items were constructed in English and Malay languages.
Acceptance consisted of one question with two options either agree or not agree. Decision-making consisted one question with three options: make own decision, make joint decision with spouse or spouse makes the decision, which needed to be chosen only one answer.
The questionnaire was then pre-tested among 30 parents in Pasir Puteh for face validity (Perneger et al, 2015). Construct validity was assessed using exploratory factor analysis with varimax rotation while reliability was assessed using Cronbach’s alpha among 65 parents from the same district. The overall Cronbach’s alpha was 0.86.
Scoring
Parental knowledge was categorized as poor and good. One mark was given for a correct answer and 0 mark for the wrong and do not know answers. Participants were considered as having good knowledge if the summed scores were more than 70% (Hesham et al., 2011).
Data collection and procedure
The questionnaire was administered between January and May 2015. In order to distribute the questionnaire to the parents, teacher advisor in each school was assigned to enhance cooperation. Before enrollment, study objectives and questionnaire were explained to the teachers. They were also trained on how to distribute the questionnaire using systematic random sampling.
The questionnaires were distributed to students by teacher advisor of each school. The selected students were given clear instructions regarding self-administered questionnaire that need to be filled up by parents and submission within a week to respective teacher. Written consent was obtained from the parents and they were given written information about the conduct of the study enclosed with the questionnaire form. The questionnaire set was sealed in the envelope. For those, who did not return the questionnaire within a week, the advisor teacher would call the parents. No response is considered if the parents fail to return the questionnaire within next 3 days.
Data analysis
Statistical Package for Social Sciences Inc, Chicago Illinois (SPSS) version 22 was used for data entry, exploration, cleaning and statistical analysis. Categorical variables were expressed using percentage and numerical variables were expressed using mean (standard deviation). Descriptive statistics was used to describe proportion of parental knowledge, acceptance and decision-making pattern on HPV vaccination. Multiple logistic regressions were used to identify the associated factors for acceptance of HPV vaccination.
Ethical consideration
Permission was obtained from the Research and Ethics Committee (Human), School of Medical Sciences, Universiti Sains Malaysia on 23rd September 2014 (Ref: USM/JEPeM/1404160) and the local education authorities. A written consent was obtained from the parents prior to answering questionnaire. Participation was strictly voluntary and anonymity of the participants was assured.
Results
Overall 330 subjects were enrolled in the study however, 280 subjects completed the questionnaire of the study. Fifty of the subjects were withdrawn from the study. These are due to 18 of them were not completely filled the questionnaire and 15 were not consented. Meanwhile 17 did not return the questionnaire. Due to these events, the response rate was 84.8%.
All of the parents were married. By ethnicity, all of them were Malays. The mean (SD) age of the participants was 42.5 (6.22) years old. Men represented 21.8% of the participants. Thus women were in the majority representing 78.2% of participants. Majority of the participants received tertiary education (64.3%). More than half (56.1%) of parents were working as government servant. Meanwhile household income of the majority (42.5%) was less than RM3000.
Table 2 shows the knowledge on HPV vaccination among the parents. Overall, the findings shows most parents (62%) exhibited poor knowledge. Some specific knowledge items that were shown to be low include questions on “HPV is transmitted by sexual intercourse” with only 32.8% correct answer; “HPV vaccination protects against cervical cancer” (31.8%); “HPV vaccine is halal” (44.6%); and male can be infected by HPV (35.4%).
Table 1.
Socio- Demographic Characteristic of the Parents
| Characteristic | n (%) | Mean (SD) |
|---|---|---|
| Age (years) | 42.5 (6.22) | |
| Gender | ||
| Male | 61 (21.8) | |
| Female | 219 (78.2) | |
| Education level | ||
| Primary | 9 (3.2) | |
| Secondary | 91 (32.5) | |
| Tertiary | 180 (64.3) | |
| Employment status | ||
| Government | 157 (56.1) | |
| Non-government | 34 (12.1) | |
| Self-employed | 33 (11.8) | |
| Unemployed | 56 (20.0) | |
| Household income | ||
| Low <RM3,000 | 119 (42.5) | |
| Mid RM3,000-8,000 | 103 (36.8) | |
| High >RM8,000 | 58 (20.7) |
*RM, Ringgit Malaysia
Table 2.
Number (%) of Parents Who Gave Correct Answers about HPV Vaccination
| Questions | Parents | Total 280 n (%) | |
|---|---|---|---|
| Mother (n=219) n (%) | Father (n=61) n (%) | ||
| 1. HPV causes cervical cancer | 190 (86.8) | 48 (78.7) | 238 (85.0) |
| 2. HPV is transmitted by sexual intercourse | 71 (32.4) | 21 (34.4) | 92 (32.8) |
| 3. HPV causes genital warts | 199 (90.9) | 52 (85.2) | 251 (89.6) |
| 4. HPV vaccination protects against cervical cancer | 68 (31.0) | 21 (34.4) | 89 (31.8) |
| 5. Vaccine can be offered to female child aged 9 and above | 186 (84.9) | 48 (78.7) | 234 (83.6) |
| 6. Vaccine requires three injections | 153 (69.9) | 34 (55.7) | 187 (66.8) |
| 7. HPV vaccine is halal | 101 (46.1) | 24 (39.3) | 125 (44.6) |
| 8. Vaccine is only for women who have had multiple sexual partners | 144 (65.8) | 46 (75.4) | 190 (67.9) |
| 9. Vaccine only for those has family history of cervical cancer | 164 (74.9) | 46 (75.4) | 210 (75) |
| 10. Male can be infected by HPV | 77 (35.2) | 22 (36.1) | 99 (35.4) |
| 11. Female who got the HPV vaccine, also need to get cervical cancer screening (Pap smears) | 171 (78.1) | 35 (57.4) | 206 (73.6) |
| 12. HPV vaccine can promotes risky sexual behaviors among teenagers | 148 (67.6) | 41 (67.2) | 189 (67.5) |
| 13. HPV vaccine is safe | 159 (72.6) | 38 (62.3) | 197 (70.4) |
Table 3.
Factors Associated with Acceptance (Agree) of HPV Vaccination by Simple Logistic Regression Analyses
| Variables | Regression coefficient (b) | Crude OR (95%CI) | Wald statistic (df) | p value |
|---|---|---|---|---|
| Age (years) | 0.08 | 1.080 (1.04, 1.13) | 13.219 | <0.001 |
| Gender | ||||
| Female | - | 1 | ||
| Male | 0.36 | 1.436 (0.81, 2.55) | 1.513 | 0.219 |
| Education level | ||||
| Primary | 1.02 | 2.768 (0.72, 10.7) | 2.18 | 0.14 |
| Secondary | 0.729 | 2.073 (1.24, 3.48) | 7.6 | 0.006 |
| Tertiary | - | 1 | 8.799 | 0.012 |
| Employment status | ||||
| Government | - | 1 | 4.24 | 0.237 |
| Non-government | 0.495 | 1.641 (0.77, 3.49) | 1.653 | 0.199 |
| Self-employed | 0.301 | 1.351 (0.62, 2.93) | 0.58 | 0.446 |
| Unemployed | 0.589 | 1.801 (0.97, 3.36) | 3.435 | 0.064 |
| Household income | ||||
| Low <RM3,000 | - | 1 | 4.4 | 0.111 |
| Mid RM3,000-8,000 | -0.488 | 0.614 (0.36,1.06) | 3.06 | 0.08 |
| High >RM8,000 | -0.579 | 0.56 (0.289, 1.09) | 2.93 | 0.087 |
| Knowledge level | ||||
| Poor | - | 1 | ||
| Good | 2.736 | 15.43(7.07,33.67) | 47.243 | <0.001 |
| Decision making | ||||
| Husband | - | 1 | 6.332 | 0.042 |
| Wife | -0.804 | 0.447 (0.18, 1.12) | 2.96 | 0.085 |
| Shared | -0.962 | 0.382 (0.19, 0.81) | 6.331 | 0.64 |
The proportion of acceptance of HPV vaccine was 63%. Most decision regarding vaccination was a shared decision (72%). Meanwhile 16% of the decision was by the husband while another 12% by the wife. Wives (62.2%) were found more likely to agree with HPV vaccine while husbands were more likely not to agree (57.6%). Our findings showed that majority (65.8%) responded that decision to agree on HPV vaccination was shared by both parents (Figure 1).
Figure 1.
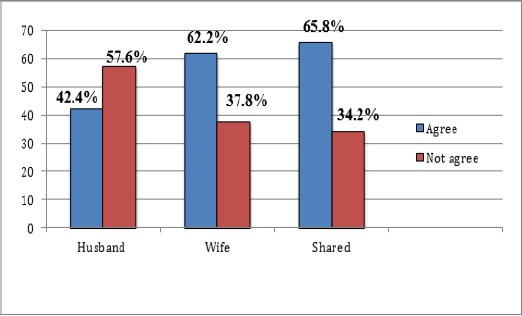
Acceptance of HPV Vaccine among Parents of Primary School Students in Kota Bharu
Table 4.
Associated Factors of Acceptance (Agree) of HPV Vaccination by Multiple Logistic Regression Model
| Variables | Crude ORa (95% CI) | Adjusted ORb (95% CI) | Wald statisticb (df) | p valueb |
|---|---|---|---|---|
| Age | 1.08 (1.04, 1.13) | 1.09 (1.04, 1.14) | 12.302 | <0.001 |
| Knowledge level | ||||
| Poor | 1 | 1 | ||
| Good | 15.43 (7.07,33.7) | 16.32 (7.32,36.4) | 46.569 | <0.001 |
, Simple Logistic Regression,
, Multiple Logistic Regression;
, Forward LR Multiple Logistic Regression model was applied; There were no interaction and multicollinearity problem; Hosmer Lemeshow test, (p=0.957), classification table (overall correctly classified percentage = 72.5%) and area under the ROC curve (80.8%) were applied to check the model fitness.
Age of respondents (AOR= 1.09; 95% CI= 1.04-1.14; p <0.001) and good knowledge (AOR= 16.32; 95% CI= 7.32-36.4; p <0.001) showed significant association with acceptance of HPV vaccination by multiple logistic regression analysis
Discussion
All study respondents were of Malay ethnicity, which reflects the distribution of the Kelantan population where Malays are the majority ethnic group (Kelantan Cancer Registry, 2012). Thus, generalization of the study findings should be done to this particular ethnic group. Most of parents (62%) in this study were shown to have poor knowledge of HPV vaccination regardless of their social status and acceptability on HPV vaccination. Malaysia government has promoted communication strategies intensively since 2010 in order to gain public support and increase parental awareness on voluntary HPV vaccination program. With media campaign, public access to interactive information and leading to establishment of religious ruling on HPV vaccination for the Muslim, it is hoped that the proportion of good knowledge is high. However our study revealed the proportion of good knowledge was low.
Nearly all parents (85%) knew that HPV cause cervical cancer. This is contradictory to similar study by Al-Dubai et al., (2010), which showed low knowledge about risk factors of cervical cancer was HPV (22%). It was expected since implementation of HPV vaccine in 2010 as national immunization program created many action plans and cancer awareness campaigns. However, there was a need to educate community on the prevention aspects since knowledge regarding the mode of HPV transmission was poor. This finding consistent with previous study done among Malaysian women in 2009 that showed about 20% answered correctly regarding the mode of HPV transmission (Al-Dubai et al., 2010). Mothers were shown to have better knowledge as compared to fathers about cervical cancer screening. This is most possibly due to the exposure with campaigns and counseling during pre-pregnancy care and postnatal period.
Almost 70% parents reported that vaccine was not only for women with multiple sexual partners. This is contradictory to the study among women in Selangor which showed only 23.3% (Al-Dubai et al., 2010). This poor knowledge is possibly due to they perceived themselves not to be at risk. Wong et al., (2008) also reported that women preferred to delay HPV vaccination as they felt they were not sexually active. With that, it highlights parents in our study aware of the risk of HPV infection.
This study revealed just one-third of parents reported that male could be infected by HPV. The finding is in parallel with the study done by Sharifa et al., (2013) in which they could not imagine the infection are being transmitted by the male. With respect to this, possibly due to unawareness, as HPV vaccination program in our country was to all female aged 13. This could act as a barrier for HPV vaccine acceptance if it is to be implemented in the future among boys in Malaysia. However interestingly to note that Seven et al., (2015) revealed that parents in Turkey tend to be more willing to vaccinate their sons than daughters.
Almost all parents knew that HPV vaccine could be delivered to their daughters as early as 9 years old. This highlights the success of education to parents about the importance of vaccination before initiation of sexual activity. Brabin et al., (2007) also reported that parents willing to vaccinate their daughters before 13 years old. But this finding was contrary with a study in China where majority of parents believed the best age to vaccinate their daughters was 19 years old and above (Wei et al., 2014). In consistent with a study in India, the parents believed that their daughters were unlikely to become sexually active before marriage (Madhivanan et al., 2009). This may reflect the reason for acceptance of HPV vaccination among parents in those studies.
Fortunately most parents (67.5%) in this study believed that the vaccine would not promote risky sexual behaviors among teenagers, similar to previous studies by Al-Dubai et al and Archin et al. Thus it may also explain the reason why high proportion of acceptance in their studies (Al-Dubai et al., 2010; Archin et al., 2012).
This study revealed proportion of acceptance of HPV vaccination among parents was 63%. Acceptance was more common among mother, 141 (80.6%) than father, 34 (19.4%). Although this figure was similar to previous study conducted among mothers in UMMC, Kuala Lumpur in 2007 showed 65.7% acceptance rate but it was before implementation as national program (Sam et al., 2009). Besides, higher acceptance rates were also found in India and Indonesia (Madhivanan et al., 2009; Jasper et al., 2011). Even Marlow et al and Brabin et al also reported high acceptability in UK, 75-81% of parents would like to vaccinate their daughters (Marlow et al., 2007, Brabin et al., 2006).
As the majority refused HPV vaccination was among fathers in our study, possibly due to concern about halal and efficacy as only 24 fathers (8.6%) knew that ‘HPV vaccine is halal’ and only 21 fathers (7.5%) knew about ‘HPV vaccine protects against cervical cancer’. Consistent findings reported by Wong, the major concerns for the study participants to oppose HPV vaccine were the newness of the vaccine, safety, and efficacy (Wong, 2008). In addition to ‘halal’, we should take note that majority of parents in Kota Bharu are Muslim, which should be of concern because of the low uptake of HPV vaccine. Wong did a study on HPV vaccine among 47 mothers in 2007, which reported, the halal issue of HPV vaccine was an important factor for acceptance on HPV vaccine among Muslim mothers (Wong, 2009). Again, with reference to the results, the promotion of the HPV vaccine should be supported with information about the vaccine ingredients, ‘halal’ status, possible side effects and efficacy.
High acceptability in this study does not reflect good knowledge on HPV vaccination among parents. Similar study done in China also showed an acceptance rate of 88% with knowledge deficiency on HPV vaccination (Kwan et al., 2009). This will be a challenge to the success in educating our parents.
Our study showed the increasing proportion of acceptance was occurring more amongst older age groups of parents. Better exposures and higher awareness were assumed to be two contributing factors among older parents. This finding was contrary with previous study of Shao et al, age showed no significant association with acceptability (Shao et al., 2013).
Our findings demonstrated a significant association between good knowledge and acceptance. This study was also supported by other studies, which demonstrated the better knowledge had positive association with vaccine acceptance (Oh et al., 2010; Hsu et al., 2009). On this point in accordance to Gamble et al (2010), acceptance might increase if participants are educated regarding HPV vaccine and infection.
It is hoped that changes over time and intervention reflected an improvement of knowledge among parents together with acceptance of HPV vaccination.
Funding statement
This research did not receive any grant.
Acknowledgements
A very special gratitude to Ministry of Education of Malaysia, State Education Department of Kelantan and all schools in Kota Bharu for helping and providing the opportunity to work in your facilities. We would like to thank to all teachers, parents and students for the encouragement.
References
- 1.Al-Dubai S, Alshagga MA, Al-Naggar RA, et al. Knowledge, attitudes and barriers for human papilloma virus (HPV) vaccines among Malaysian women. Asian Pac J Cancer Prev. 2010;11:887–92. [PubMed] [Google Scholar]
- 2.April MW, Richard AC, Kathleen SJ, et al. HPV vaccine acceptability among women in the Philippines. Asian Pac J Cancer Prev. 2010;11:1781–7. [PubMed] [Google Scholar]
- 3.Archin S, Punnee P, Jaranit K, et al. Knowledge, attitudes, and acceptability of a Human Papilloma Virus vaccine among students, parents and teachers in Thailand. Southeast Asian J Trop Med Public Health. 2012;43:340–53. [PubMed] [Google Scholar]
- 4.Brabin L, Roberts SA, Farzaneh F, Kitchener HC. Future acceptance of adolescent human papillomavirus vaccination:A survey of parental attitudes. Vaccine. 2006;24:3087–94. doi: 10.1016/j.vaccine.2006.01.048. [DOI] [PubMed] [Google Scholar]
- 5.Brabin L, Roberts SA, Kitchener HC. A semi-qualitative study of attitudes to vaccinating adolescents against human papillomavirus without parental consent. BMC Public Health. 2007;7:1–7. doi: 10.1186/1471-2458-7-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clinical Practice Guidelines (CPG) Management of cancer cervix, Malaysia. 2003. Available from http://www.moh.gov.my/index.php/pages/view/148 .
- 7.Control CfD Prevention. FDA licensure of bivalent human papillomavirus vaccine (HPV2, Cervarix) for use in females and updated HPV vaccination recommendations from the Advisory Committee on Immunization Practices (ACIP) MMWR Morb Mortal Wkly Rep. 2010;59:626. [PubMed] [Google Scholar]
- 8.Erdin I, Aygen C, Berna H, Elif U, Ahmet M. Women's knowledge of Pap smear test and human papillomavirus:Acceptance of HPV vaccination to themselves and their daughters in an Islamic society. Int J Gynecol Cancer. 2010;6:1058–62. doi: 10.1111/IGC.0b013e3181dda2b9. [DOI] [PubMed] [Google Scholar]
- 9.Gamble HL, Klosky JL, Parra GR, Randolph ME. Factors influencing familial decision-making regarding human papillomavirus vaccination. J Pediatr Psychol. 2010;35:704–15. doi: 10.1093/jpepsy/jsp108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hesham R, Syarif HL, Kiat AN. Knowledge of cervical cancer and acceptance of HPV vaccination among secondary school students in Sarawak, Malaysia. Asian Pac J Cancer Prev. 2011;12:1837–41. [PubMed] [Google Scholar]
- 11.Hsu YY, Fetzer SJ, Hsu KF, et al. Intention to obtain human papillomavirus vaccination among Taiwanese undergraduate women. Sex Transm Dis. 2009;36:686–92. doi: 10.1097/OLQ.0b013e3181ad28d3. [DOI] [PubMed] [Google Scholar]
- 12.Hyunjin O. Knowledge about HPV and the attitudes toward HPV vaccination among adult women in Asian Countries:A literature review. J Korean Oncol Nurs. 2011;11:171–8. [Google Scholar]
- 13.ICO information centre on HPV and cancer, Malaysia. 2014. Available from http://www.hpvcentre.net/statistics/reports/MYS_FS.pdf .
- 14.Jaspers L, Budiningsih S, Wolterbeek R, Henderson F, Peters A. Parental acceptance of human papillomavirus (HPV) vaccination in Indonesia:A cross-sectional study. Vaccine. 2011;29:7785–93. doi: 10.1016/j.vaccine.2011.07.107. [DOI] [PubMed] [Google Scholar]
- 15.Kelantan cancer registry report 2007-2011. Malaysia: Kelantan state health department; 2012. [Google Scholar]
- 16.Kwan TTC, Chan KKL, Yip AMW, et al. Acceptability of human papillomavirus vaccination among Chinese women:concerns and implications. Int J Gynaecol Obstet. 2009;116:501–10. doi: 10.1111/j.1471-0528.2008.01988.x. [DOI] [PubMed] [Google Scholar]
- 17.Madhivanan P, Krupp K, Yashodha M, et al. Attitudes toward HPV vaccination among parents of adolescent girls in Mysore, India. Vaccine. 2009;27:5203–8. doi: 10.1016/j.vaccine.2009.06.073. [DOI] [PubMed] [Google Scholar]
- 18.Marlow LA, Waller J, Wardle J. Parental attitudes to pre-pubertal HPV vaccination. Vaccine. 2007;25:1945–52. doi: 10.1016/j.vaccine.2007.01.059. [DOI] [PubMed] [Google Scholar]
- 19.Seven M, Guvenc G, Sahin E, Akyuz A. Attitudes to HPV vaccination among parents of children aged 10 to 13 years. J Pediatr Adolesc Gynecol. 2015;28:382–6. doi: 10.1016/j.jpag.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 20.Ministry of Health Malaysia (MOH) Third national health and morbidity survey (NHMS III) Kuala Lumpur: Institute for public health; 2006. [Google Scholar]
- 21.Oh JK, Lim MK, Yun EH, et al. Awareness of and attitude towards human papillomavirus infection and vaccination for cervical cancer prevention among adults males and females in Korea:a nationwide interview survey. Vaccine. 2010;28:1854–60. doi: 10.1016/j.vaccine.2009.11.079. [DOI] [PubMed] [Google Scholar]
- 22.Othman NH. Cancer of the cervix –from bleak past to bright future. A review, with an emphasis on cancer of the cervix in Malaysia. Malays J Med Sci. 2002;9:13–26. [PMC free article] [PubMed] [Google Scholar]
- 23.Othman NH, Devi BC, Halimah Y. Cervical cancer screening:patients'understanding in major hospitals in Malaysia. Asian Pac J Cancer Prev. 2009;10:569–74. [PubMed] [Google Scholar]
- 24.Perneger TV, Courvoisier DS, Hudelson PM, Gayet-Ageron A. Sample size for pre-tests of questionnaires. Qual Life Res. 2015;24:147–51. doi: 10.1007/s11136-014-0752-2. [DOI] [PubMed] [Google Scholar]
- 25.Saidatul NB, Rohani J. Introduction of national HPV immunisation program:Sharing Malaysia's Experience. Vol. 2010. New York: Health P; 2010. [Google Scholar]
- 26.Sam I, Wong LP, Rampal S, et al. Maternal acceptance of human papillomavirus vaccine in Malaysia. J Adolesc Health. 2009;44:610–2. doi: 10.1016/j.jadohealth.2008.11.014. [DOI] [PubMed] [Google Scholar]
- 27.Shao KZ, Xiong FP, Shiou MW, et al. Perceptions and acceptability of HPV vaccination among parents of young adolescents:A multicenter national survey in China. Vaccine. 2013;31:3244–9. doi: 10.1016/j.vaccine.2013.05.046. [DOI] [PubMed] [Google Scholar]
- 28.Sharifa WPE, Rozita H, Jamsiah M, et al. National HPV immunisation programme:knowledge and acceptance of mothers attending an obstetrics clinic at a teaching hospital, Kuala Lumpur. Asian Pac J Cancer Prev. 2013;141:2991–9. doi: 10.7314/apjcp.2013.14.5.2991. [DOI] [PubMed] [Google Scholar]
- 29.Sun KT, Hextan YSN, Tang YC, Annie NYC, Eng HT. Epidemiology of human papillomavirus infection and cervical cancer and future perspectives in Hong Kong, Singapore and Taiwan. Vaccine. 2008;26:60–70. doi: 10.1016/j.vaccine.2008.05.042. [DOI] [PubMed] [Google Scholar]
- 30.Tay SK, Tesalona KC, Rashid NM, et al. Vaccine misconceptions and low HPV vaccination take –up rates in Singapore. Asian Pac J Cancer Prev. 2015;16:5119–24. doi: 10.7314/apjcp.2015.16.12.5119. [DOI] [PubMed] [Google Scholar]
- 31.Wei W, Yuanyuan M, Xia W, et al. Acceptability of human papillomavirus vaccine among parents of junior middle school students in Jinan, China. Vaccine. 2015;30 doi: 10.1016/j.vaccine.2015.04.010. [DOI] [PubMed] [Google Scholar]
- 32.Wong LP. Preventing cervical cancer through human papillomavirus vaccination:Perspective from focus groups. American society for colposcopy and cervical pathology. J Low Genit Tract Dis. 2009;13:85–93. doi: 10.1097/LGT.0b013e3181865f44. [DOI] [PubMed] [Google Scholar]
- 33.Wong LP. Young multiethnic women's attitudes toward the HPV vaccine and HPV vaccination. Int J Gynecol Obstet. 2008;103:131–5. doi: 10.1016/j.ijgo.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 34.Zaridah S. A review of cervical cancer research in Malaysia. Med J Malaysia. 2014;69:33–41. [PubMed] [Google Scholar]


