Lower nutrition literacy predicted poorer weight loss for all participants. For black participants, nutrition literacy indirectly impacted weight loss through quality of self-monitoring.
Keywords: Nutrition literacy, Self-monitoring, Black or African American, Education, Behavioral weight loss
Abstract
Background
Few have examined nutrition literacy (i.e., capacity to process and make informed nutritional decisions) in behavioral weight loss. Nutrition literacy (NL) may impact necessary skills for weight loss, contributing to outcome disparities.
Purpose
The study sets out to identify correlates of NL; evaluate whether NL predicted weight loss, food record completion and quality, and session attendance; and investigate whether the relations of race and education to weight loss were mediated by NL and self-monitoring.
Methods
This is a secondary analysis of 6-month behavioral weight loss program in which overweight/obese adults (N = 320) completed a baseline measure of NL (i.e., Newest Vital Sign). Participants self-monitored caloric intake via food records.
Results
NL was lower for black participants (p < .001) and participants with less education (p = .002). Better NL predicted better 6-month weight loss (b = −.63, p = .04) and food record quality (r = .37, p < .001), but not food record completion or attendance (ps > 0.05). Black participants had lower NL, which was associated with poorer food record quality, which adversely affected weight loss. There was no indirect effect of education on weight loss through NL and food record quality.
Conclusions
Overall, results suggest that lower NL is problematic for weight loss. For black participants, NL may indirectly impact weight loss through quality of self-monitoring. This might be one explanation for poorer behavioral weight loss outcomes among black participants. Additional research should investigate whether addressing these skills through enhanced treatment improves outcomes.
Clinical trial information
Nutrition literacy (NL), defined as an individual’s capacity to obtain, process, and understand information necessary for making appropriate nutrition decisions [1], is an increasingly important concept in health promotion. Previous studies have examined the relation of NL to caloric intake and body mass index (BMI; [2, 3]; however, research is limited in the context of behavioral weight loss outcomes [4]. One of the few studies in this area found that nonresponders had lower nutrition knowledge than those who lost at least five pounds [4]. Research on health literacy, a broader construct that encompasses NL, and behavioral weight loss is also limited [5], but there is an indication that health literacy may be related to intervention outcomes. For example, one study of a worksite wellness program [4] found that health literacy moderated weight loss [6]. The limited research on NL in behavioral weight loss programs warrants a remedy as evidence suggests that NL is a modifiable factor that may affect weight loss success [4]. In fact, interventions to improve NL for individuals with obesity may enhance treatment response [7].
The ways in which lower NL may pose challenges for individuals engaged in behavioral weight loss interventions remain unknown; however, one potential pathway is through skill development. Specifically, NL levels might impact the ability to learn and practice self-monitoring skills necessary to adopt and maintain a low-calorie diet. Preliminary evidence suggests that participants with lower NL have greater challenges in self-monitoring intake [8]; this could compromise behavioral weight loss outcomes since accurate and consistent self-monitoring of calorie intake is a crucial skill for successful weight loss [9, 10]. Previous experience with behavioral weight loss attempts that emphasize meeting calorie goals in conjunction with self-monitoring (i.e., lifestyle modification programs), especially experiences that were more successful from a weight loss perspective, may serve as NL skill-building opportunities. Consistent with previous findings that those who were exposed to dietary counseling gained more nutrition knowledge than those in usual care [11], the literature potentially supports an association between a history of lifestyle dieting and NL.
Lower NL, and associated limitations in self-monitoring caloric intake, may contribute to the suboptimal weight losses that are faced by a substantial portion of participants in behavioral weight-loss interventions [12–14]. In particular, black participants lose approximately half as much weight as white participants in behavioral weight loss [15–17]. Literature also suggests that educational status may impact weight loss [18]. Given the importance of understanding why gaps in treatment outcomes occur, examination of differences in NL according to participant characteristics is warranted.
The Newest Vital Sign (NVS) is a relatively new measure of NL [19] that has been examined in a limited number of interventions related to weight (i.e., stepped care, weight gain prevention) [7, 20]; no research to date has examined the NVS in relation to weight lost in a behavioral weight loss program. Given that standard behavioral weight loss is considered the first-line treatment for obesity, examining whether the NVS is related to outcome in this context is crucial. Because the NVS is a brief measure that quickly identifies low NL [19], it may provide efficient treatment guidance for those struggling with behavioral weight loss. This is the first article to examine the relation of NVS scores to both weight loss and weight control behaviors in a standard, group-based behavioral weight loss program.
This study aimed to fill the existing gaps in the literature as follows: (a) identify participant characteristics and behavioral factors associated with NL; (b) determine whether NL predicts 6-month (6M) weight change; (c) examine whether NL predicts food record completion, food record quality, and session attendance; and (d) explore whether the relations of race and education to 6M weight change were mediated by NL and self-monitoring. We also planned to conduct exploratory analyses to determine whether demographic variables might have bearing on analyses related to our study aims. Our hypotheses were as follows: (a) black participants and participants with less education would have lower NL; (b) previous exposure to programs emphasizing NL (i.e., lifestyle modification weight loss attempts) would be associated with higher NL; (c) lower baseline NL would predict less 6M weight loss; (d) lower NL would be associated with lower rates of food record completion, lower food record quality, and lower session attendance; and (e) lower NL would result in poorer food records, which would adversely impact 6M weight loss for black participants, and those with less education, respectively.
Methods
Participants and Procedures
Participants were 320 overweight and obese individuals (22% men) who received 16 sessions of a uniform behavioral weight loss intervention over 6M as part of a larger weight loss study before being randomized to one of three weight loss maintenance conditions (NCT02363010). The parent study compared whether following standard behavioral weight loss intervention with physical activity focused treatments, one behavioral and one acceptance based, respectively, would improve weight loss maintenance over continuation of standard behavioral weight loss. This study is a secondary analysis of data from the initial 6M weight loss induction period prior to randomization.
Groups of 10–15 participants were led by doctoral-level clinicians. Content for the initial 6M of treatment was based on the Diabetes Prevention Program and Look AHEAD [21, 22]. Participants’ goals were designed to achieve a 10% weight loss over 6M. Standard physical activity goals were provided, starting at 45 min per week and uniformly progressing to 250 min per week. Additionally, they were asked to complete detailed daily food records to self-monitor their caloric intake and to set specific calorie goals within the ranges provided (i.e., 1200–1500 per day for those <250 lbs. and 1500–1800 per day for those ≥250 lbs.). Since meal planning is a key skill in standard behavioral weight loss, session content included brief education on reading nutrition facts labels, weighing/measuring foods, and portion size estimation. Participants were instructed on how to complete food records, emphasizing the inclusion of calories, timing of meals/snacks, and portion size. Recording of micro and macronutrients was not recommended as participants were free to consume any foods/beverages they wished that fit within calorie goals.
Most participants were white (70%). The remaining were African American/black (25%), multiracial (3%), Asian (2%), and American Indian/Native Alaskan (<1%). The sample was 4% Hispanic/Latino. Educational status was as follows: graduate/professional degree (44%), bachelor’s degree (33%), associate’s degree/some college (18%), and high school/general equivalency diploma (GED) (5%). Few participants (14%) identified their household income as $50,000 a year or less. Others were as follows: $50,000–$125,000 (49%); $125,000–$200,000 (25%); and more than $200,000 (10%).
Participants were recruited over 1.5 years beginning in 2014 from a Mid-Atlantic metropolitan area using newspaper, radio, and direct mail ads. University-affiliated primary care practices also participated in recruitment. Participants were eligible if they had a BMI between 27 and 45 kg/m2, were 18- to 70-years old, and able to participate in physical activity. Participants were excluded if they (a) had previous bariatric surgery and/or acceptance-based therapy; (b) were currently or recently on weight-affecting drugs; (c) had ≥5% weight loss in the last 6M; (d) had significant medical or psychiatric conditions (e.g., eating disorders and psychosis) that might impact participation in treatment; or (e) were nursing, pregnant, or planning to become pregnant. The Institutional Review Board approved this study; all participants gave informed consent.
Measures
Demographic characteristics
Participants self-reported age, gender, race, ethnicity, education, and annual household income at baseline via online or paper survey.
Nutrition literacy
NL was assessed using the NVS [19] at baseline. Participants interpret and utilize information on a standard Food and Drug Administration-approved nutrition label, with one point awarded for each correct answer out of a maximum of 6. Standard administration protocol was used; staff asked questions verbally and scored responses on an answer sheet. Higher scores indicate greater NL; scores ≥4 indicate adequate NL. It has shown good internal consistency (Cronbach’s a = 0.76) and criterion validity (r = .59, p < .001) [19].
Previous lifestyle dieting attempts
At baseline, participants completed the Weight and Lifestyle Inventory [23], which assesses history of lifestyle dieting attempts and pounds lost.
Food records
Participants’ weekly food records of caloric intake at Sessions 2, 8, and 14 were coded for quality by a clinical staff member. Since 2 weeks of food records were collected at Session 14, we sampled 28 days of food record data. Participants were not made aware of which weeks’ records would be coded. Participants were free to choose their format for food records (e.g., paper and mobile app); those who used an electronic method provided a print out. Quality coding was based on the extent to which key elements were included throughout the food record using criteria operationalized for this study (e.g., timing of meals/snacks, portion size, and calories). Staff also tallied the number of days food records were completed for the three sessions above. A subsample of records also received coding from a second staff member. Agreement among coders was good (Krippendorff alpha = 0.83). Means for completion and quality were calculated across the three sessions to represent average levels across treatment for analyses and ranged from 0% to 100%. Anchors were specified for quality to aid in operationalization (e.g., 75% quality indicated ≥75% of calorie and portion size information was present, with at least half of timing of meals/snacks allowed to be missing). Higher means indicated higher completion and quality.
Weight
Participants were weighed in light clothing on a digital scale (Tanita model WB-3000) at baseline and 6M. Weight loss was calculated as the percentage lost at 6M from baseline.
Attendance
Attendance at each of the 16 group sessions was recorded by staff and summed.
Analytic Plan
Data were analyzed with SPSS version 23 [24]. Descriptive statistics were computed using means, standard deviations, and frequencies. Correlations identified the relation of NL to participant characteristics and behavioral factors; ANOVAs evaluated differences in NL for categorical variables. We examined whether NL predicted weight change with a regression analysis using last observation carried forward to minimize potential bias due to missing 6M weight data, controlling for relevant participant characteristics that were significantly related to NVS, as identified through the analyses performed in Aim 1. Preliminary evaluations of the relations of NL to food record completion, food record quality, and session attendance were performed via correlations. Additional evaluations of the relation between NL, food record quality, and weight change were conducted using separate serial mediation analyses for race and education, controlling for relevant participant characteristics as above, using Hayes’ PROCESS model [25]. We screened for potential multicollinearity via variance inflation factor (VIF) and did not find cause for concern in our models (all VIF values <1.3). Because black and white participants comprised 95% of our sample and dichotomization would facilitate interpretation of differences, we excluded the 5% of participants of other races from further analyses. To also aid interpretation, education was dichotomized to reflect differences in NVS between those with high-school degrees and those with college degrees or higher. Given that NL was hypothesized to impact subsequent skill development for recording food, our models were ordered with NVS as the first mediator, affecting food record quality.
Results
Descriptive Information
Table 1 displays the means and standard deviations for NL, age, baseline BMI, the number of previous lifestyle diet attempts, weight loss from previous lifestyle diets, food record completion, food record quality, and treatment session attendance. Overall, the sample had relatively high NL (M = 5.13, SD = 1.15). Approximately 10% (n = 32) of participants had total NVS scores below the adequate NL range.
Table 1.
Means, Standard Deviations (SD), and Bivariate Correlations Among Variables of Interest
| Mean (SD) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Nutrition literacy | 5.13 (1.15) | 1 | −.12* | −.06 | −.16** | .11 | .18 | .03 | .15** | .10 |
| 2. 6M weight loss (%) | −9.17 (5.69) | 1 | −.01 | −.14** | .04 | −.06 | −.21*** | −.40*** | −.46*** | |
| 3. BL BMI (kg/m2) | 35.09 (4.74) | 1 | −.17** | −.08 | .10 | .02 | −.05 | −.13* | ||
| 4. Age (years) | 52.74 (10.32) | 1 | .01 | .01 | −.02 | .04 | .14* | |||
| 5. Number of previous lifestyle diet attempts | 0.70 (1.22) | 1 | .62*** | −.01 | .02 | −.09 | ||||
| 6. Total weight loss during previous lifestyle diets (lbs.) | 39.89 (32.31) | 1 | .00 | .03 | −.18 | |||||
| 7. Food record completion (%) | 89.73 (17.05) | 1 | .64*** | .28*** | ||||||
| 8. Food record quality (%) | 72.78 (19.40) | 1 | .37*** | |||||||
| 9. Sessions attended (out of 16) | 13.10 (2.84) | 1 |
6M 6 month, BL baseline, BMI body mass index.
*p < .05; **p < .01; ***p < .001.
Participant Characteristics and Behavioral Factors Associated With NL
An ANOVA indicated significant differences in NL by race (F (3, 315) = 7.64, p < .001, R2 = .07); however, a Bonferroni post-hoc test revealed that the only group difference was between white (M = 5.32, SD = 0.99) and black participants (M = 4.64, SD = 1.33; p < .001). There were significant differences in NL by education level (F (3, 316) = 4.95, p = .002, R2 = .05), between those with a high-school diploma/GED (M = 4.35, SD = 1.46) differing from those with bachelor’s degrees (M = 5.25, SD = 1.16, p = .02) and those with graduate/professional degrees (M = 5.25, SD = 1.03, p = .01). There were no differences in NL by gender, ethnicity, or income, and NL was not correlated with baseline BMI (all ps > .05). It was significantly negatively correlated with age, marginally positively correlated with previous lifestyle diet attempts (p = .05), and weight loss from previous lifestyle diets (p = .06; Table 1).
Relation of NL to Weight Change
A regression analysis examining whether baseline NL predicted 6M percent weight loss, controlling for age, education, and race, was significant (F (4, 300) = 4.06, p = .003, R2 = .05). Baseline NL significantly predicted (b = −.63, t (300) = −2.06, p = .04) 6M percent weight loss, such that weight loss was 0.63% better for every point higher in NVS scores. Since the NVS has a 6-point score range, this suggests that weight loss could differ by 3.78% between those with the lowest and highest possible scores.
Relation of NL to Food Record Completion, Food Record Quality, and Session Attendance
NL significantly positively predicted food record quality, but not completion. There was a marginal positive correlation between NL and session attendance (p = .07; Table 1).
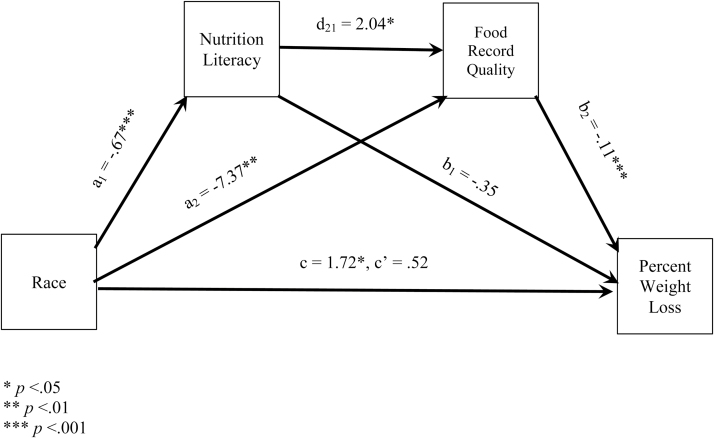
Relations of Race and Education to Weight Change as Mediated by NL and Self-monitoring
Exploratory analyses were conducted based on differences observed in NL by race and education. First, we examined the direct and indirect effects of race on 6M percent weight loss through NL and food record quality operating in serial as mediators. The model (Fig. 1) containing race, NL, and food record quality (F (5, 297) = 13.27, p < .001, R2 = .18) indicated that the total effect of race on weight loss was significant (b = 1.72, t (299) = 2.34, p = .02; path c, see Fig. 1), with a significant total indirect effect of race on weight loss (b = 1.2, SE = 0.37, 95% CI: 0.5 to, 2.00; sum of all indirect effects not depicted in Fig. 1). The indirect serial mediation effect was also significant, such that black participants had lower NL, which negatively affected food record quality, which in turn adversely affected weight loss (b = .15, SE = 0.09, 95% CI: 0.01 to 0.39; path a1d1b2, not depicted in Fig. 1). The model did not support an indirect effect of race on weight loss through NL alone (b = .23, SE = 0.19, 95% CI: −0.08 to 0.68; path a1b1; not depicted in Fig. 1).
Fig. 1.
Serial mediation model examining the effects of race, nutrition literacy, and food record quality on 6-month percent weight loss. *p < .05; **p < .01; ***p < .001.
Next, we used a similar approach to examine the direct and indirect effects of education on 6M percent weight loss through NL and food record quality operating in serial. Although the overall model was significant (F (3, 244) = 3.48, p = .02, R2 = .04), the total effect of education on weight loss (b = .96, t (244) = 0.66, p = .51), including the total indirect effect of education (b = .36, SE = 0.55, 95% CI: −0.65 to 1.51), was not significant.
Discussion
This study aimed to (a) identify participant characteristics and behavioral factors associated with NL; (b) determine whether NL predicts 6M weight change; (c) examine whether NL predicts food record completion, food record quality, and session attendance; and (d) explore whether the relations of race and education to 6M weight change were mediated by NL and self-monitoring.
Consistent with prior research, NL differed by race, age, and education in this behavioral weight loss sample [7, 26–29]; however, we failed to find significant differences in NL by baseline BMI, as reported elsewhere [6, 7, 26]. Regarding dieting history, lower NL was marginally associated with fewer prior weight loss attempts and less weight lost during past attempts. Although previous research has found that exposure to nutritional counseling is associated with greater gains in nutritional knowledge [11], others have found that NL is not associated with engagement in lifestyle modification or weight change [7]. Future research examining the relation of dieting history and NL may identify if low NL is characteristic of treatment for nonresponders.
We found that lower NL predicted poorer weight losses at 6M after controlling for relevant covariates. Given that only 5% of the variance in weight loss was explained by baseline NL, controlling for age, education, and race, the clinical significance of the overall model evaluating NL may be somewhat low. Nonetheless, this finding is particularly concerning given that clinically significant weight loss is associated with numerous health benefits that smaller weight losses may not confer [30]. Previous research has demonstrated that NL can improve with intervention [4]; therefore, it may be useful to investigate whether targeted NL training improves weight loss. Our study provided some training in nutritional skills in early intervention sessions (e.g., nutrition facts label reading tutorial); however, the impact of this intervention component is unknown. Additional research is needed to determine essential nutritional skills for weight loss (e.g., portion size estimation) along with their optimal timing and dose. Ongoing assessment of nutritional skills via questionnaires could help identify and remedy individualized gaps in nutritional skills that may interfere with weight loss.
Food record completion and session attendance were not associated with NL. It is possible that these behaviors may be more strongly related to motivation than to knowledge or skill [31]. NL was, however, positively associated with food record quality, such that individuals with higher NL had higher quality food records. Since the average food record completion and attendance rates were generally high, it may be quality of the self-monitoring and synthesis of session content into the practice of behavior change in daily life that conferred an advantage to individuals with higher NL.
Race, which is associated with NL, may be indirectly related to weight loss through food record quality. Specifically, compared with white participants, black participants tended to have disproportionately lower NL, which was associated with poorer food record quality, which was in turn related to less weight loss. These findings may help explain the suboptimal weight loss seen in black participants across behavioral weight loss studies [16, 32–35] and suggest that better understanding of NL among blacks may be important to improving behavioral weight loss outcomes. Specifically, our findings support prior literature suggesting that black participants have lower NL than whites [3, 18] and provide new evidence suggesting that lower NL may pose a challenge for developing and practicing accurate self-monitoring of caloric intake. Overall, although race did not demonstrate an indirect effect through NL alone on weight loss in this sample, it was associated with a weight control behavior (i.e., food record quality) that was related to weight loss outcomes. Taken together, these findings may help to understand some of the racial discrepancies in the effectiveness of behavioral weight loss programs.
Education level did not affect weight loss either directly or indirectly. This finding is perhaps unsurprising given that data on the relation between education and weight loss in behavioral weight loss programs remain mixed with some studies reporting that individuals with lower levels of education have poorer weight outcomes [36], others finding the opposite [37], and still others finding no relation between education and weight loss [38]. Our findings further suggest that, although level of education and NL are related, it is NL rather than education that has important associations with weight control behaviors and outcomes.
This study had several strengths, including that it is the first study to our knowledge to examine the relation between the NVS and weight outcome in a behavioral weight loss sample. Additionally, our sample was large and racially diverse, allowing us to examine racial differences and increasing the generalizability of our findings. Despite these strengths, certain limitations should be noted. In our sample, NVS scores and food record completion were high on average, both of which may have contributed to ceiling effects. It is possible that different findings might emerge in samples containing individuals with more variabilities in NL and food record completion. Some aspects of the socioeconomic status of our sample may limit generalizability to other groups, such as those with less education, lower income, and lower NL. Additionally, to limit assessment burden, we sampled food record data from three sessions rather than analyzing across all 16. Although participants were not aware that the selected sessions were being sampled, it is possible that these weeks were not fully reflective of the full 6M of treatment. Further, we could not evaluate whether behavioral weight loss treatment improved NVS scores. Finally, this was an observational study within a large behavioral weight loss trial and, as such, could not assess for causal relationships among NL and other factors.
Future research should further explore the role of NL in a behavioral weight loss program. Some participants may benefit from targeted NL training, perhaps even prior to beginning a formal behavioral weight loss program. Additional research to evaluate differences in participant characteristics and behavioral factors among those with low NL may be helpful to better understand those who may benefit most from an NL-based intervention. Given a heightened risk for obesity development in black individuals, it is particularly important to identify barriers to weight loss and to develop treatments that improve outcomes for black participants [39]. Thus, determining whether additional NL training improves food record quality and, in turn, weight loss, in black participants warrants study. While there are likely many factors that contribute to the gap in the effectiveness of behavioral weight loss interventions between black and white participants, future research should continue to explore whether adjunctive or tailored interventions aimed toward improving NL and self-monitoring help to decrease the racial disparity in traditional behavioral weight loss programs.
Acknowledgement
This research was funded by the National Institutes of Health (R01DK100345-01A1).
Compliance with Ethical Standards
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standard Authors Diane L. Rosenbaum, Margaret H. Clark, Alexandra D. Convertino, Christine C. Call, Evan M. Forman, and Meghan L. Butryn declare that they have no conflict of interest.
Authors' Contributions Diane L. Rosenbaum, Meghan L. Butryn, and Margaret H. Clark conceived of the idea for this manuscript. Meghan L. Butryn and Evan M. Forman led the parent study from which data collection occurred. Diane L. Rosenbaum carried out the statistical analyses. Diane L. Rosenbaum, Margaret H. Clark, Alexandra D. Convertino, and Christine C. Call wrote the manuscript, with additional critical feedback provided by Meghan L. Butryn and Evan M. Forman. All authors reviewed and discussed the results and contributed to the final manuscript.
Ethical Approval All procedures, including the informed consent process, were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Informed Consent Informed consent was obtained from all individual participants included in the study.
References
- 1. Krause C, Sommerhalder K, Beer-Borst S, Abel T. Just a subtle difference? Findings from a systematic review on definitions of nutrition literacy and food literacy. Health Promot Int. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Huizinga MM, Beech BM, Cavanaugh KL, Elasy TA, Rothman RL. Low numeracy skills are associated with higher BMI. Obesity (Silver Spring). 2008; 16(8): 1966–1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zoellner J, You W, Connell C, et al. . Health literacy is associated with healthy eating index scores and sugar-sweetened beverage intake: Findings from the rural Lower Mississippi Delta. j Am Diet Assoc. 2011; 111(7): 1012–1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Klohe-Lehman DM, Freeland-Graves J, Anderson ER, et al. . Nutrition knowledge is associated with greater weight loss in obese and overweight low-income mothers. j Am Diet Assoc. 2006; 106(1): 65–75; quiz 76. [DOI] [PubMed] [Google Scholar]
- 5. Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: An updated systematic review. Ann Intern Med. 2011; 155(2): 97–107. [DOI] [PubMed] [Google Scholar]
- 6. Zoellner J, You W, Almeida F, et al. . The influence of health literacy on reach, retention, and success in a Worksite Weight Loss Program. Am j Health Promot. 2016; 30(4): 279–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lanpher MG, Askew S, Bennett GG. Health literacy and weight change in a digital health intervention for women: A randomized controlled trial in primary care practice. j Health Commun. 2016; 21 (suppl 1): 34–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Porter K, Chen Y, Estabrooks P, Noel L, Bailey A, Zoellner J. Using teach-back to understand participant behavioral self-monitoring skills across health literacy level and behavioral condition. j Nutr Educ Behav. 2016; 48(1): 20–26.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: A systematic review of the literature. j Am Diet Assoc. 2011; 111(1): 92–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wing RR. Behavioral approaches to the treatment of obesity. In: Bray G, Bouchard C, James W, eds. Handbook of Obesity. New York, NY: Marcel Dekker; 1998: 855–877. [Google Scholar]
- 11. Rhodes KS, Bookstein LC, Aaronson LS, Mercer NM, Orringer CE. Intensive nutrition counseling enhances outcomes of National Cholesterol Education Program dietary therapy. j Am Diet Assoc. 1996; 96(10): 1003–1010; quiz 1011. [DOI] [PubMed] [Google Scholar]
- 12. Lundgren JD, Malcolm R, Binks M, O’Neil PM. Remission of metabolic syndrome following a 15-week low-calorie lifestyle change program for weight loss. Int j Obes (Lond). 2009; 33(1): 144–150. [DOI] [PubMed] [Google Scholar]
- 13. Jakicic JM, Tate DF, Lang W, et al. . Effect of a stepped-care intervention approach on weight loss in adults: A randomized clinical trial. JAMA. 2012; 307(24): 2617–2626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Knowler WC, Barrett-Connor E, Fowler SE, et al. ; Diabetes Prevention Program Research Group Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. n Engl j Med. 2002; 346(6): 393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lewis KH, Edwards-Hampton SA, Ard JD. Disparities in treatment uptake and outcomes of patients with obesity in the USA. Curr Obes Rep. 2016; 5(2): 282–290. [DOI] [PubMed] [Google Scholar]
- 16. West DS, Elaine Prewitt T, Bursac Z, Felix HC. Weight loss of black, white, and Hispanic men and women in the Diabetes Prevention Program. Obesity (Silver Spring). 2008; 16(6): 1413–1420. [DOI] [PubMed] [Google Scholar]
- 17. Cox TL, Krukowski R, Love SJ, et al. . Stress management-augmented behavioral weight loss intervention for African American women: A pilot, randomized controlled trial. Health Educ Behav. 2013; 40(1): 78–87. [DOI] [PubMed] [Google Scholar]
- 18. Kuczmarski MF, et al. . Health literacy and education predict nutrient quality of diet of socioeconomically diverse, urban adults. J Epid Prev Med. 2016; 2: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Weiss BD, Mays MZ, Martz W, et al. . Quick assessment of literacy in primary care: The newest vital sign. Ann Fam Med. 2005; 3(6): 514–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Carels RA, Selensky JC, Rossi J, Solar C, Hlavka R. A novel stepped-care approach to weight loss: The role of self-monitoring and health literacy in treatment outcomes. Eat Behav. 2017; 26: 76–82. [DOI] [PubMed] [Google Scholar]
- 21. The Diabetes Prevention Program Research Group. The Diabetes Prevention Program (DPP): Description of lifestyle intervention. Diabetes Care. 2002; 25: 2165–2171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. The Look AHEAD Research Group. The Look AHEAD Study. A description of the lifestyle intervention and the evidence supporting it. Obesity. 2006; 14: 737–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wadden TA, Foster GD. Weight and lifestyle inventory. Obesity. 2006; 14: 99S–118S. [DOI] [PubMed] [Google Scholar]
- 24. IBM Corporation. IBM SPSS Statistics for Windows, Version 23.Armonk, NY: IBM Corp; 2014. [Google Scholar]
- 25. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York, NY: Guilford Press; 2013. [Google Scholar]
- 26. Speirs KE, Messina LA, Munger AL, Grutzmacher SK. Health literacy and nutrition behaviors among low-income adults. j Health Care Poor Underserved. 2012; 23(3): 1082–1091. [DOI] [PubMed] [Google Scholar]
- 27. Baker DW, Gazmararian JA, Sudano J, Patterson M. The association between age and health literacy among elderly persons. j Gerontol b Psychol Sci Soc Sci. 2000; 55(6): S368–S374. [DOI] [PubMed] [Google Scholar]
- 28. Kobayashi LC, Smith SG, O’Conor R, et al. . The role of cognitive function in the relationship between age and health literacy: A cross-sectional analysis of older adults in Chicago, USA. bmj Open. 2015; 5(4): e007222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wu JR, Moser DK, DeWalt DA, Rayens MK, Dracup K. Health literacy mediates the relationship between age and health outcomes in patients with heart failure. Circ Heart Fail. 2016; 9(1): e002250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wing RR, Lang W, Wadden TA, et al. ; Look AHEAD Research Group Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011; 34(7): 1481–1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Webber KH, Tate DF, Ward DS, Bowling JM. Motivation and its relationship to adherence to self-monitoring and weight loss in a 16-week Internet behavioral weight loss intervention. j Nutr Educ Behav. 2010; 42(3): 161–167. [DOI] [PubMed] [Google Scholar]
- 32. West DS, DiLillo V, Bursac Z, Gore SA, Greene PG. Motivational interviewing improves weight loss in women with type 2 diabetes. Diabetes Care. 2007; 30(5): 1081–1087. [DOI] [PubMed] [Google Scholar]
- 33. Kumanyika SK, Espeland MA, Bahnson JL, et al. ; TONE Cooperative Research Group Ethnic comparison of weight loss in the Trial of Nonpharmacologic Interventions in the Elderly. Obes Res. 2002; 10(2): 96–106. [DOI] [PubMed] [Google Scholar]
- 34. Fitzgibbon ML, Tussing-Humphreys LM, Porter JS, Martin IK, Odoms-Young A, Sharp LK. Weight loss and African-American women: A systematic review of the behavioural weight loss intervention literature. Obes Rev. 2012; 13(3): 193–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Samuel-Hodge CD, Johnson CM, Braxton DF, Lackey M. Effectiveness of diabetes prevention program translations among African Americans. Obes Rev. 2014; 15 (suppl 4): 107–124. [DOI] [PubMed] [Google Scholar]
- 36. Rautio N, Jokelainen J, Saaristo T, et al. ; FIN-D2D Writing Group Predictors of success of a lifestyle intervention in relation to weight loss and improvement in glucose tolerance among individuals at high risk for type 2 diabetes: The FIN-D2D project. j Prim Care Community Health. 2013; 4(1): 59–66. [DOI] [PubMed] [Google Scholar]
- 37. Gurka MJ, Wolf AM, Conaway MR, Crowther JQ, Nadler JL, Bovbjerg VE. Lifestyle intervention in obese patients with type 2 diabetes: Impact of the patient’s educational background. Obesity (Silver Spring). 2006; 14(6): 1085–1092. [DOI] [PubMed] [Google Scholar]
- 38. Rautio N, Jokelainen J, Oksa H, et al. ; FIN-D2D Study Group Socioeconomic position and effectiveness of lifestyle intervention in prevention of type 2 diabetes: One-year follow-up of the FIN-D2D project. Scand j Public Health. 2011; 39(6): 561–570. [DOI] [PubMed] [Google Scholar]
- 39. Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016; 315(21): 2284–2291. [DOI] [PMC free article] [PubMed] [Google Scholar]