Abstract
Objective
Few have compared short-term outcomes following knee dislocations with or without concomitant popliteal artery disruption (PAD).
Methods
The Nationwide Inpatient Sample was used to identify 2175 patients admitted for knee dislocation from 2005 to 2013 (concomitant PAD: n = 210/9.7%; without: n = 1965/90.3%).
Results
Patients with PAD were younger, more often male, Black and Hispanic, and with Medicaid (all p ≤ 0.013). PADs were associated with 11.0-times higher odds of increased LOS (95%CI, 6.6–18.4) and 2.8-times higher odds of experiencing any complication (95%CI, 2.03–3.92). Female sex was a protective factor against increased LOS, (OR = 0.65; 95%CI, 0.48–0.88).
Conclusion
High suspicion index should be maintained for concomitant vascular injuries following knee dislocations.
Keywords: Knee dislocation, Popliteal artery disruption, Complications, Length of stay, Charges, Nationwide analysis
1. Introduction
Dislocation of the knee constitutes an orthopaedic emergency that is associated with concomitant soft-tissue and vascular injuries. Dislocation is most often secondary to high-energy “dashboard” injuries in motor vehicle accidents,1, 2, 3, 4 although low-energy falls and athletic injuries can lead to dislocation.2, 3, 4, 5, 6 Upon presentation, patient evaluation includes immediate knee reduction, followed by lower extremity neurovascular examination and imaging studies to assess the reduction and evaluate vascular and soft-tissue integrity.7, 8, 9, 10, 11 Most knee dislocations are managed operatively with external fixation, which has been found to have superior functional outcomes compared to conservative therapy.12, 13, 14 Popliteal artery disruption occurs in an estimated 30% of knee dislocations following high-energy injuries,4, 5, 6, 7,15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27 and prompt diagnosis and treatment is critically important, as a delay in revascularization beyond 8 h27, 28, 29, 30 can potentially lead to limb ischemia, necrosis, and ultimately surgical amputation.27,29
Currently, the data is sparse on short-term outcomes of patients with knee dislocations and concomitant popliteal artery disruption. To address this knowledge gap, we used the Nationwide Inpatient Sample (NIS), a large, nationwide US inpatient database, to identify all knee dislocations in the United States between 2005 and 2013. Specifically, we compared the following metrics among knee dislocation patients with and without popliteal artery disruption: (1) patient factors (incidence and demographics); (2) perioperative factors (medical and surgical complications, length of stay [LOS], and hospital charges).
2. Materials and methods
2.1. Study population
The NIS contains a 20% representative sample of annual hospital admissions in the United States.27 It contains demographic and clinical variables for each admission, including International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) diagnosis and procedure codes. Additionally, a data-weighting variable, which is based on the size and location of the hospital where each admission occurred, allows statistical models to calculate nationwide estimates of patient discharges. The NIS is publicly available to researchers and contains de-identified data. Therefore, this study did not meet human subject research criteria and was exempt from institutional review.
2.2. Patient factors
Utilizing ICD-9-CM diagnosis codes, all patients between 2005 and 2013 who were admitted with a closed knee dislocation (836.5x) were identified. Patients who had a popliteal artery disruption were identified using the ICD-9-CM diagnosis code 904.41. For each patient, data on demographics, as they were recorded, was collected, including age (continuous, in years), sex (male, female), race (White, Black, Hispanic, Asian or Pacific Islander, or Other), insurance (government, private, other), and year of hospital admission (2005–2013). Comorbidities were calculated from diagnosis codes using Charlson and Deyo's method,31 and patients were distributed into comorbidity score categories of 0, 1, and ≥2 points.
2.3. Perioperative factors
For each patient, data on perioperative complications, length of stay, and hospital charges were collected. Perioperative complications were calculated using ICD-9-CM diagnosis codes, as described previously.15 Medical complications included hematoma, altered mental status, acute myocardial infarction (MI), pulmonary distress, pneumonia, gastrointestinal upset, urinary tract infection (UTI), acute renal failure (ARF), sepsis, pulmonary embolism (PE), or deep vein thrombosis (DVT). Surgical complications included wound infection, wound dehiscence, or blood transfusion.
2.4. Statistical analysis
Patients were stratified into two groups, those with vascular injury and those without (the reference group). To compare differences in demographics between patients who had vascular injury and the reference group, regression modeling was employed to predict the chance that a patient had a vascular injury based on each demographic variable. To compare the risk of complication between patients who had a vascular injury and the reference group, logistic regression was utilized to calculate the Odds Ratio (OR) of having a perioperative (any, medical, surgical) complication. To compare differences in length of stay, length of stay was dichotomized by defining an increased length of stay as greater than 0.5 standard deviations (SD) from the mean. Subsequently, a logistic regression was used to calculate the OR as previously described. All regression models included the following covariates: age, sex, race, and Deyo comorbidity score.
Weighting variables were utilized in all analyses to simulate nationwide United States rates of admission for knee dislocation. All analyses were performed with SPSS version 24 (IBM Corp., Armonk, New York). Figures were created with Microsoft Excel 2010 (Microsoft Corporation, Redmond, Washington). An alpha level of 0.05 was selected as the threshold for statistical significance.
3. Results
3.1. Patient factors
The analysis identified 2,175 patients who had a knee dislocation between 2005 and 2013 in the United States. A diagnosis of popliteal artery injury was documented for 210 (9.7%) patients, while the other 1,965 (90.3%) patients did not have an arterial injury. Patients with popliteal artery disruptions were younger (35 vs. 44 years, p < 0.001) and were more often male relative to patients without vascular injury (72.9% vs. 56.2% male, p < 0.001). Patients with popliteal artery disruption were more often Black and Hispanic, with an increased frequency of Medicaid, private insurance, and self-pay as the primary payer (all p ≤ 0.013) (Table 1).
Table 1.
Demographic information for patients with and without popliteal artery injury from the Nationwide Inpatient Sample (NIS) between 2005 and 2013.
| Patients (n) | No Disruption |
Disruption |
p Value |
|
|---|---|---|---|---|
| 1,965 | 210 | – | ||
| Age (years) | 44 | 35 | 0.001 | |
| Sex (%) | Male | 56.20 | 72.90 | 0.001 |
| Female | 43.80 | 27.10 | ||
| Primary Payer (%) | Medicare | 20.50 | 5.70 | 0.001 |
| Medicaid | 13.30 | 18.70 | ||
| Private Insurance | 42.70 | 44.00 | ||
| Self-Pay | 11.90 | 12.90 | ||
| No-Charge | 1.30 | 2.40 | ||
| Other | 10.30 | 16.30 | ||
| Race (%) | White | 63.70 | 52.20 | 0.013 |
| Black | 18.20 | 24.40 | ||
| Hispanic | 12.10 | 17.80 | ||
| Asian or Pacific Islander | 1.30 | 0.00 | ||
| Native American | 1.20 | 2.20 | ||
| Other | 3.50 | 3.30 | ||
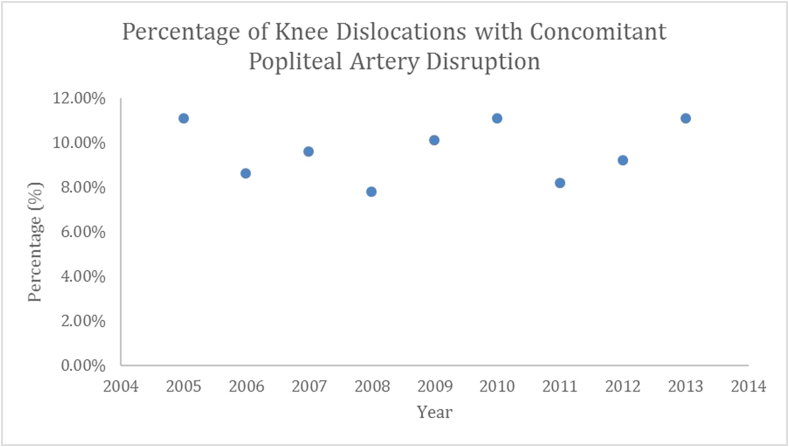
Chi-square analysis revealed that the percentage of popliteal artery disruptions in patients with knee dislocations did not vary significantly from 2005 to 2013 (Fig. 1). The rate of vascular injury fluctuated between 7.8 and 11.1%.
Fig. 1.
Percentage of knee dislocations with concomitant popliteal artery disruptions from 2005 to 2013.
3.2. Perioperative factors
Among medical complications, patients with popliteal disruptions had significantly higher rates of hematoma, UTI, ARF, PE, DVT (p ≤ 0.049). Among surgical complications, the popliteal disruption population had significantly higher rates of wound infection and blood transfusion when compared to patients with knee dislocations without popliteal disruption (p < 0.001). Furthermore, LOS and total charges were increased in the popliteal disruption patients (p < 0.001.) (Table 2).
Table 2.
Medical and surgical complication rates, length of stay, and total hospital charges in knee dislocation patients with and without popliteal artery disruption.
| No Disruption | Disruption | P-value | |
|---|---|---|---|
| Length of Stay (days) | 6.84 | 13.94 | 0.001 |
| Total Charges (US Dollars) | $70,756 | $147,425 | 0.001 |
| Medical Complications (%) | |||
| Hematoma | 0.90 | 4.30 | 0.001 |
| Altered Mental Status | 0.20 | 0 | 0.513 |
| Acute Myocardial Infarction | 0.30 | 0 | 0.423 |
| Pulmonary Distress | 1.20 | 1.40 | 0.744 |
| Pneumonia | 1.90 | 1.40 | 0.609 |
| Gastrointestinal Complications | 0.20 | 0.50 | 0.298 |
| Urinary Tract Infection | 0.40 | 1.40 | 0.047 |
| Acute Renal Failure | 2.00 | 4.30 | 0.037 |
| Sepsis | 0.70 | 1.90 | 0.052 |
| Pulmonary Embolism | 0.90 | 2.40 | 0.049 |
| Deep Vein Thrombosis | 2.40 | 5.20 | 0.018 |
| Surgical Complications (%) | |||
| Transfusion of Blood | 10.80 | 19.00 | 0.001 |
| Wound Infection | 3.50 | 8.60 | 0.001 |
| Wound Dehiscence | 0.80 | 1.90 | 0.116 |
After adjusting for the potential confounding effects (covariates) of race, sex, age, and Deyo Index, binary logistic regression revealed that the odds of developing at least one medical or surgical complication was 2.8 times higher (95% CI, 2.03–3.92, p < 0.001) among patients with popliteal artery disruption compared to the reference group. Similarly, the odds of having an increased length of stay was 11.0 times higher (95% CI, 6.6–18.4, p < 0.001) in patients with popliteal artery disruption, while female sex was associated with a 0.65 lower odds (95% CI, 0.48–0.88, p = 0.005) (Table 3).
Table 3.
Logistic Regression of Factors Independently Associated with the occurrence of Any Medical or Surgical Complication, or a Length of Stay (LOS) 0.5 SD greater than the mean.
| Odds Ratio | 95% Confidence Interval | p-value | |||
|---|---|---|---|---|---|
|
Any Complication |
Popliteal Disruption | 2.819 | 2.030 | 3.915 | 0.001 |
| Female Sex | 0.841 | 0.666 | 1.061 | 0.144 | |
| African American | 1.005 | 0.744 | 1.360 | 0.972 | |
| Hispanic | 1.240 | 0.888 | 1.731 | 0.207 | |
| Asian or Pacific Islander | 1.079 | 0.387 | 3.008 | 0.885 | |
| Native American | 1.495 | 0.598 | 3.740 | 0.390 | |
| Other | 1.179 | 0.649 | 2.144 | 0.589 | |
| Deyo Index | 1.073 | 0.947 | 1.215 | 0.268 | |
|
Age in years at admission |
1.016 |
1.010 |
1.022 |
0.001 |
|
|
Odds Ratio |
95% Confidence Interval |
p-value |
|||
| Increased Length of Stay ( > 0.5 SD) | Popliteal Disruption | 11.040 | 6.622 | 18.404 | 0.001 |
| Female Sex | 0.650 | 0.480 | 0.881 | 0.005 | |
| African American | 1.006 | 0.685 | 1.478 | 0.976 | |
| Hispanic | 1.330 | 0.857 | 2.062 | 0.203 | |
| Asian or Pacific Islander | 1.267 | 0.383 | 4.194 | 0.698 | |
| Native American | 1.185 | 0.374 | 3.758 | 0.773 | |
| Other | 1.182 | 0.586 | 2.383 | 0.640 | |
| Deyo Index | 0.902 | 0.717 | 1.135 | 0.380 | |
| Age in years at admission | 1.004 | 0.996 | 1.013 | 0.326 | |
4. Discussion
Although knee dislocations are considered rare injuries, they are surgical emergencies due to the potential neurovascular complications.32 This study utilized the NIS database to assess the risks and burdens associated with knee dislocation and analyzed frequency trends over time, stratified by age, sex, race, and Deyo comorbidity index, to determine the incidence of knee dislocations and the associated complications. In knee dislocation patients, popliteal artery injury occurred in 7.8–11.1% of cases. Specifically, knee dislocation patients with concomitant vascular injury were found to be younger and more often male. Additionally, race may have a role in the rate of vascular injury, as Black and Hispanic patients more often incurred a vascular complication rather than a purely anatomical dislocation. Furthermore, vascular injury patients were more likely to experience secondary medical and surgical complications, including hematoma, UTI, ARF, PE, DVT, and wound infection and were also more likely to experience an increased length and cost of stay. Of note, patient comorbidities did not significantly influence the rate of vascular complications following knee dislocation (p = 0.268).
The findings from this study were in agreement with other works with regards to the incidence of vascular injury following knee dislocation. A multicenter prospective study by Boisrenoult et al.33 found that of the 67 knee dislocation patients, 12% incurred a vascular injury. Similarly, Medina et al.34 showed that of 826 patients with a knee dislocation, 171 (18%) experienced vascular complications. This investigation produced similar results to the aforementioned studies and highlight that, while knee dislocations may be rare, there were high enough rates of vascular complications following knee dislocation emphasize the need for careful examination.
However, while this study pointed to a high incidence of vascular injury following knee dislocation, other studies have reported different injury rates. In a national 14-year prospective study conducted in Finland by Sillanpää et al.,35 of the 837 patients included in the study, only 13 (1.6%) experienced vascular injury. Likewise, using a large private insurance database, Natsuhara et al.36 reported that among the 8050 limbs reviewed, only 267 (3.3%) experienced a vascular injury. Several factors may account for the differences found between these studies and the present one. Different patient populations may alter study results. Specifically, as there is a higher incidence of traffic accidents in the USA compared with most other countries,37,38 and since high-energy mechanisms are more likely to be associated with vascular injuries,17 this can potentially impact incidence rates. Likewise, the use of a private insurance database may potentially limit variations in the patient population included in the study. Moreover, patient body mass index (BMI) might influence injury biomechanics and alter patient presentation. In a retrospective cohort study, Johnson et al.39 reported a slightly lower vascular injury rate of 5.63% following knee dislocation compared to our results. However, their rate increased to 7.2% in obese patients and 11.3% among morbidly obese patients, indicating that BMI may influence the rates of vascular injury. The importance of these findings becomes apparent when considering the role that angiography plays in detecting vascular injury. Angiography is an invasive and expensive modality with the potential for allergic reactions, renal damage, and vascular injury.25 If the rates of vascular injury are in fact lower than what is presented in the current study, more stringent patient selection criteria for angiography is justified.
There were several limitations to the current study. Performing retrospective analysis with the use of large administrative encompasses inherit limitations. As databases were not maintained by study personnel, there exists the potential to introduce bias with data entry and errors in reporting diagnosis codes. Additionally, as hospitals operate under various regulations, the reporting of vascular injury may be reported under different codes depending on that particular institute's reporting protocol. As such, the true incidence of vascular injury may be either over or underestimated. Despite these limitations, we believe that the results of the present study are significant and valid.
5. Conclusions
It is critical to accurately diagnose and assess knee dislocations, as they are associated with significant patient morbidity. This study reported on a significant proportion of patients that incurred popliteal artery injury following a knee dislocation. Importantly, these patients with concomitant popliteal injury were also more likely to experience secondary complications, experience longer hospital stays, and incur greater healthcare costs. Diagnostic diligence is vital, as a proper neurovascular and ligamentous examination may accurately identify soft tissue and neurovascular complications and may decrease patient morbidity.
Acknowledgments
We thank the Healthcare Cost and Utilization Project (HCUP) Data Partners who contribute annually to the NIS. A full listing of participants can be found at <http://www.hcup-us.ahrq.gov/hcupdatapartners.jsp>.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jor.2018.08.006.
Funding
This study was performed without any external funding.
Conflicts of interest
There are no relationships or conflicts of interest directly related to this paper or that could influence or bias this work. The authors have the following financial relationships to disclose: Naziri — nothing to disclose; Beyer — nothing to disclose; Shah — nothing to disclose; Solow — nothing to disclose; Hayden — nothing to disclose; Nadarajah — nothing to disclose; Ho – nothing to disclose; Newman – nothing to disclose; Boylan — nothing to disclose; Basu — nothing to disclose; Zikria — Vericel - paid speaker or presenter; Urban — nothing to disclose.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Clarke H., Scott W., Insall J., Al E. Anatomy. In: Insall J., Scott W., editors. Surgery of the Knee. third ed. Churchill Livingstone; New York, NY: 2001. pp. 13–76. [Google Scholar]
- 2.Borden P., Johnson D. Initial assessment of the acute and chronic multiple ligament-injured knee. Sports Med Arthrosc. 2001;9(3):178–184. [Google Scholar]
- 3.Bratt H.D., Newman A.P. Complete dislocation of the knee without disruption of both cruciate ligaments. J Trauma. 1993;34(3):383–389. doi: 10.1097/00005373-199303000-00013. http://www.ncbi.nlm.nih.gov/pubmed/8483179 [DOI] [PubMed] [Google Scholar]
- 4.Stannard J., Schenck R., Fanelli G. Rockwood and Green's Fractures in Adults. seventh ed. Lippincott, Williams & Wilkins; Philadelphia, PA: 2010. Knee dislocations and fracture-dislocations. [Google Scholar]
- 5.Twaddle B.C., Bidwell T.A., Chapman J.R. Knee dislocations: where are the lesions? A prospective evaluation of surgical findings in 63 cases. J Orthop Trauma. 2003;17(3):198–202. doi: 10.1097/00005131-200303000-00008. http://www.ncbi.nlm.nih.gov/pubmed/12621261 [DOI] [PubMed] [Google Scholar]
- 6.Helgeson M.D., Lehman R.A., Murphy K.P. Initial evaluation of the acute and chronic multiple ligament injured knee. J Knee Surg. 2005;18(3):213–219. doi: 10.1055/s-0030-1248185. http://www.ncbi.nlm.nih.gov/pubmed/16152871 [DOI] [PubMed] [Google Scholar]
- 7.Merritt A.L., Wahl C. Initial assessment of the acute and chronic multiple-ligament injured (dislocated) knee. Sports Med Arthrosc. 2011;19(2):93–103. doi: 10.1097/JSA.0b013e3182191a7e. [DOI] [PubMed] [Google Scholar]
- 8.Hirschmann M.T., Iranpour F., Müller W., Friederich N.F. Surgical treatment of complex bicruciate knee ligament injuries in elite athletes: what long-term outcome can we expect? Am J Sports Med. 2010;38(6):1103–1109. doi: 10.1177/0363546509356978. [DOI] [PubMed] [Google Scholar]
- 9.Shelbourne K.D., Klootwyk T.E. Low-velocity knee dislocation with sports injuries. Treatment principles. Clin Sports Med. 2000;19(3):443–456. doi: 10.1016/s0278-5919(05)70217-9. http://www.ncbi.nlm.nih.gov/pubmed/10918959 [DOI] [PubMed] [Google Scholar]
- 10.Azar F.M., Brandt J.C., Miller R.H., Phillips B.B. Ultra-low-velocity knee dislocations. Am J Sports Med. 2011;39(10):2170–2174. doi: 10.1177/0363546511414855. [DOI] [PubMed] [Google Scholar]
- 11.Peltola E.K., Lindahl J., Hietaranta H., Koskinen S.K. Knee dislocation in overweight patients. AJR Am J Roentgenol. 2009;192(1):101–106. doi: 10.2214/AJR.07.3593. [DOI] [PubMed] [Google Scholar]
- 12.Sharma H., Singh G.K., Gupta M., Moss M. Type IIIB tibial intercondylar eminence fracture associated with a complex knee dislocation in a grossly obese adult. Knee Surg Sports Traumatol Arthrosc. 2005;13(4):313–316. doi: 10.1007/s00167-004-0520-x. [DOI] [PubMed] [Google Scholar]
- 13.Shetty R.R., Mostofi S.B., Housden P.L. Knee dislocation of a morbidly obese patient: a case report. J Orthop Surg. 2005;13(1):76–78. doi: 10.1177/230949900501300114. [DOI] [PubMed] [Google Scholar]
- 14.Hamblin T., Curtis S.H., D'Astous J., Aoki S.K. Childhood obesity and low-velocity knee dislocation in a fifteen-year-old girl: a case report. J Bone Joint Surg Am. 2010;92(12):2216–2219. doi: 10.2106/JBJS.J.00115. [DOI] [PubMed] [Google Scholar]
- 15.Kaufman S.L., Martin L.G. Arterial injuries associated with complete dislocation of the knee. Radiology. 1992;184(1):153–155. doi: 10.1148/radiology.184.1.1609074. [DOI] [PubMed] [Google Scholar]
- 16.Varnell R.M., Coldwell D.M., Sangeorzan B.J., Johansen K.H. Arterial injury complicating knee disruption. Third place winner: conrad Jobst award. Am Surg. 1989;55(12):699–704. http://www.ncbi.nlm.nih.gov/pubmed/2596766 [PubMed] [Google Scholar]
- 17.Wascher D.C. High-velocity knee dislocation with vascular injury. Treatment principles. Clin Sports Med. 2000;19(3):457–477. doi: 10.1016/s0278-5919(05)70218-0. http://www.ncbi.nlm.nih.gov/pubmed/10918960 [DOI] [PubMed] [Google Scholar]
- 18.Kendall R.W., Taylor D.C., Salvian A.J., O'Brien P.J. The role of arteriography in assessing vascular injuries associated with dislocations of the knee. J Trauma. 1993;35(6):875–878. doi: 10.1097/00005373-199312000-00013. http://www.ncbi.nlm.nih.gov/pubmed/8263986 [DOI] [PubMed] [Google Scholar]
- 19.Sisto D.J., Warren R.F. Complete knee dislocation. A follow-up study of operative treatment. Clin Orthop Relat Res. 1985;198:94–101. http://www.ncbi.nlm.nih.gov/pubmed/4028570 [PubMed] [Google Scholar]
- 20.Treiman G.S., Yellin A.E., Weaver F.A. Examination of the patient with a knee dislocation. The case for selective arteriography. Arch Surg. 1992;127(9):1056–1062. doi: 10.1001/archsurg.1992.01420090060009. http://www.ncbi.nlm.nih.gov/pubmed/1514907 discussion 1062-3. [DOI] [PubMed] [Google Scholar]
- 21.Hoover N.W. Injuries of the popliteal artery associated with fractures and dislocations. Surg Clin. 1961;41:1099–1112. doi: 10.1016/s0039-6109(16)36451-9. http://www.ncbi.nlm.nih.gov/pubmed/13715729 [DOI] [PubMed] [Google Scholar]
- 22.Stannard J.P., Sheils T.M., Lopez-Ben R.R., McGwin G., Robinson J.T., Volgas D.A. Vascular injuries in knee dislocations: the role of physical examination in determining the need for arteriography. J Bone Joint Surg Am. 2004;86-A(5):910–915. http://www.ncbi.nlm.nih.gov/pubmed/15118031 [PubMed] [Google Scholar]
- 23.Wascher D.C., Dvirnak P.C., DeCoster T.A. Knee dislocation: initial assessment and implications for treatment. J Orthop Trauma. 1997;11(7):525–529. doi: 10.1097/00005131-199710000-00011. http://www.ncbi.nlm.nih.gov/pubmed/9334955 [DOI] [PubMed] [Google Scholar]
- 24.Levy B.A., Fanelli G.C., Whelan D.B. Controversies in the treatment of knee dislocations and multiligament reconstruction. J Am Acad Orthop Surg. 2009;17(4):197–206. doi: 10.5435/00124635-200904000-00001. http://www.ncbi.nlm.nih.gov/pubmed/19307669 [DOI] [PubMed] [Google Scholar]
- 25.Nicandri G.T., Chamberlain A.M., Wahl C.J. Practical management of knee dislocations: a selective angiography protocol to detect limb-threatening vascular injuries. Clin J Sport Med. 2009;19(2):125–129. doi: 10.1097/JSM.0b013e31819cd37a. [DOI] [PubMed] [Google Scholar]
- 26.Fanelli G.C., Stannard J.P., Stuart M.J. Management of complex knee ligament injuries. Instr Course Lect. 2011;60:523–535. http://www.ncbi.nlm.nih.gov/pubmed/21553795 [PubMed] [Google Scholar]
- 27.Green N.E., Allen B.L. Vascular injuries associated with dislocation of the knee. J Bone Joint Surg Am. 1977;59(2):236–239. http://www.ncbi.nlm.nih.gov/pubmed/845209 [PubMed] [Google Scholar]
- 28.McCoy G.F., Hannon D.G., Barr R.J., Templeton J. Vascular injury associated with low-velocity dislocations of the knee. J Bone Joint Surg Br. 1987;69(2):285–287. doi: 10.1302/0301-620X.69B2.3818761. http://www.ncbi.nlm.nih.gov/pubmed/3818761 [DOI] [PubMed] [Google Scholar]
- 29.Miller H.H., Welch C.S. Quantitative studies on the time factor in arterial injuries. Ann Surg. 1949;130(3):428–438. http://www.ncbi.nlm.nih.gov/pubmed/17859442 [PMC free article] [PubMed] [Google Scholar]
- 30.O'Donnell T.F., Brewster D.C., Darling R.C., Veen H., Waltman A.A. Arterial injuries associated with fractures and/or dislocations of the knee. J Trauma. 1977;17(10):775–784. doi: 10.1097/00005373-197710000-00005. http://www.ncbi.nlm.nih.gov/pubmed/909119 [DOI] [PubMed] [Google Scholar]
- 31.Deyo R.A., Cherkin D.C., Ciol M.A. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 32.Rihn J.A., Groff Y.J., Harner C.D., Cha P.S. The acutely dislocated knee: evaluation and management. J Am Acad Orthop Surg. 2004;12(5):334–346. doi: 10.5435/00124635-200409000-00008. http://www.ncbi.nlm.nih.gov/pubmed/15469228 [DOI] [PubMed] [Google Scholar]
- 33.Boisrenoult P., Lustig S., Bonneviale P. Vascular lesions associated with bicruciate and knee dislocation ligamentous injury. Orthop Traumatol Surg Res. 2009;95(8):621–626. doi: 10.1016/j.otsr.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 34.Medina O., Arom G.A., Yeranosian M.G., Petrigliano F.A., McAllister D.R. Vascular and nerve injury after knee dislocation: a systematic review. Clin Orthop Relat Res. 2014;472(9):2621–2629. doi: 10.1007/s11999-014-3511-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sillanpää P.J., Kannus P., Niemi S.T., Rolf C., Felländer-Tsai L., Mattila V.M. Incidence of knee dislocation and concomitant vascular injury requiring surgery: a nationwide study. J Trauma Acute Care Surg. 2014;76(3):715–719. doi: 10.1097/TA.0000000000000136. [DOI] [PubMed] [Google Scholar]
- 36.Natsuhara K.M., Yeranosian M.G., Cohen J.R., Wang J.C., McAllister D.R., Petrigliano F.A. What is the frequency of vascular injury after knee dislocation? Clin Orthop Relat Res. 2014;472(9):2615–2620. doi: 10.1007/s11999-014-3566-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Evans L. Traffic fatality reductions: United States compared with 25 other countries. Am J Publ Health. 2014;104(8):1501–1507. doi: 10.2105/AJPH.2014.301922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Luoma J., Sivak M. University of Michigan Transportation Research Institute; 1992 Aug. Traffic Accidents in Finland and the U.S.A.: a Cross-cultural Comparison of Associated Factors. UMTRI-92-96:1-29. [Google Scholar]
- 39.Johnson J.P., Kleiner J., Klinge S.A., McClure P.K., Hayda R.A., Born C.T. Increased incidence of vascular injury in obese patients with knee dislocations. J Orthop Trauma. 2018;32(2):82–87. doi: 10.1097/BOT.0000000000001027. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.