Abstract
Context:
Early detection of peri-implant bone defects is highly important to prevent further bone loss and implant failure.
Aims:
This study aimed to assess the diagnostic accuracy of three cone-beam computed tomography (CBCT) systems and periapical radiography for detection of fenestration around dental implants.
Methods:
Thirty-one titanium implants were placed in the bovine ribs, in which peri-implant fenestration were simulated. Using a round fissure bur, fenestration defects were created in the apical-third region of implants. CBCT and PA radiographs were obtained before and after creating the defects. The results were analyzed using Chi-square test; kappa coefficient; Cochran's Q-test; McNemar's test; and sensitivity, specificity, positive predictive value, and negative predictive value; and receiver operating characteristic curve.
Results:
A significant agreement was noted between the two observers in the detection of defect-free samples in all imaging systems (P < 0.05). In detection of samples with defects, a significant agreement was observed between the two observers in use of Cranex three-dimensional and NewTom 3G systems (P < 0.05), but the agreement was not significant for detection of defects in use of Promax 3D (P > 0.05). The results showed no significant difference among the four imaging systems in detection of defect-free samples while the difference was significant among the four groups for detection of defects (P < 0.05). NewTom had the highest sensitivity (75.81%) and specificity (100%) for detection of fenestration.
Conclusions:
Within the limitations of CBCT systems different kVp used by different systems, artifacts and noises that influences image quality, difference in diagnostic value of different CBCT systems is due to the differences in type of detector and voxel size. In terms of the type of detector, our results showed that NewTom 3G, which has a higher (kVP) than other systems and the highest accuracy for detection of fenestration.
Keywords: Cone-beam computed tomography, fenestration, peri-implant defects, periapical radiography
Introduction
Visualization of cortical bone is important, especially for periodontal treatment planning and implant treatment. Knowledge about the quality and quantity of cortical plate in the desired area is important for the success of dental implant treatment because the primary stability of implants and adequate osseointegration depend on the amount of cortical bone surrounding the implant.[1] A minimum of 1 mm of bone around the implant is required for the success of implant treatment, and inadequate amount of bone increases the risk of cortical bone defects such as fenestration and dehiscence.[2]
Other factors causing cortical bone defects include improper placement of implant, applying excessive pressure to implant and peri-implant inflammation due to biofilm accumulation. These defects prevent complete coverage of implant surface by bone and compromise esthetics and periodontal health. Thus, early detection of peri-implant bone defects is highly important to prevent gingival recession, further bone loss and implant failure.[3]
Diagnostic imaging is often used to assess alveolar bone height and presence of bone defects.[4] Conventional and digital intraoral radiography, panoramic radiography, computed tomography (CT), and cone-beam CT (CBCT) are used for this purpose.[5] Long cone intraoral periapical (PA) radiography is a standard technique for longitudinal assessment of dental implants. Low radiation dose, low cost, and high resolution are among the advantages of this imaging technique. It is also highly accurate for postoperative assessment of dental implants. However, it provides two-dimensional (2D) image of a 3D object, and therefore, cannot help in detection of fenestration and dehiscence. It is only suitable for assessment of the level of interproximal bone.[2,4] Furthermore, 2D radiographs often underestimate the bone loss and superimposition of anatomical structures prevents accurate estimation of the actual dimensions of buccal and lingual cortical plates, especially in the presence of intraosseous lesions. Image acquisition is faster in digital imaging systems and they do not require image processing. Patient radiation dose is lower than conventional radiography and these systems also allow image enhancement by the software. However, digital imaging systems are not superior to conventional PA radiography in terms of diagnostic accuracy for bone defects.[5]
Introduction of CT revolutionized diagnosis and treatment planning in medicine. However, its use is rather limited in dentistry due to high cost, large size of equipment, and high dose.[6] CBCT has been suggested as a standard alternative for many diagnostic procedures.[7,8,9,10] Images acquired by CBCT have high quality and accuracy and enable 3D assessment of bone defects from different angles with no distortion.[2,5] Considering the availability of different CBCT systems and their related software programs, it is imperative to assess the capability and accuracy of different systems to find the most efficient system for visualization of cortical plates and bone defects. Search of the literature yielded no previous study comparing the accuracy of three CBCT systems and PA radiography for detection of fenestration and dehiscence around dental implants. Thus, this study aimed to compare the diagnostic accuracy of NewTom 3G, Planmeca and Cranex 3D CBCT systems, and PA radiography for detection of fenestration around dental implants.
Methods
In this in vitro, experimental study (Res. Proj. 16/35/1/5310), fresh bovine ribs with similar width to human mandibular bone were used due to high similarity to the alveolar bone. Ribs with defects and very thicker or thinner width are excluded. Red dental wax was used to create boxes simulating the mandible. Sample size was calculated to be 62 (31 before creating defects and 31 after creating defects) assuming the mean difference of 4, 90% study power and alpha = 0.05.
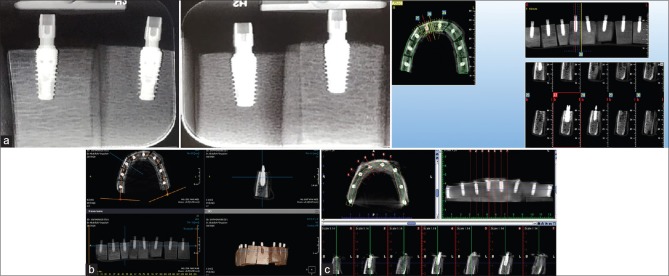
Using a saw, the ribs were divided into segments and placed in the boxes. A total of 31 titanium implants measuring 11 mm × 4.5 mm (SIC Invent AG, Switzerland) were placed in the ribs by an experienced maxillofacial surgeon. Using a trimmer (Doppelscheiben Modelltrimmer, Dentaurum, Germany), cortical bone was sectioned such that the distance between the implant and the bone surface was 2 mm [Figure 1]. Images of the control group (no fenestration) were immediately captured using three different CBCT systems [Figure 2].
Figure 1.
(a and b) The ribs were divided into segments. (c and d) Titanium implants were placed in the ribs by an experienced maxillofacial surgeon. (e) The distance between the implant and the buccal bone surface was 2 mm
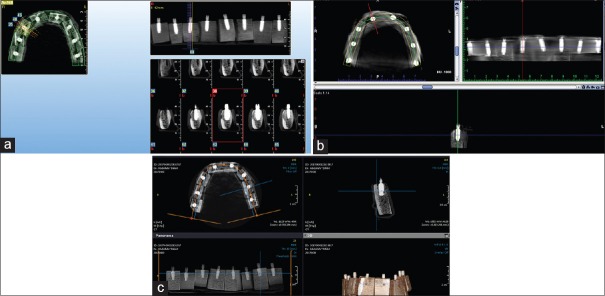
Figure 2.
Images captured by NewTom (a), Cranex 3D (b), and Planmeca (c) cone-beam computed tomography systems of samples without fenestration defects. (NewTom: Without defect, Cranex 3D: Without defect, Planmeca: Without defect)
PA radiographs were obtained with digital intraoral X-ray unit (Minray; Soredex, Tuusula, Finland) with the exposure settings of 7 mA, 0.25 s, and 60 kVp using the paralleling technique and size 2 photostimulable phosphor plate (PSP) detector. To maintain the geometry and for the purpose of reproducibility, an intraoral film holder was adjusted at 5 mm distance from the healing abutment screwed into the implant. The X-ray tube was fixed to the film holder using putty impression material.
CBCT images were taken with the following exposure settings:
Cranex 3D (Soredex, Tuusula, Finland): 4 mA, 6.1 s time, 90 kVp, FOV: 6-inch
NewTom 3G (Quantitative Radiology, Verona, Italy): 10.65 mAs, 110 kVp, FOV: 6-inch
Promax 3D (Planmeca, Helsinki, Finland): 14 mA, 12 s time, 84 kVp, FOV: 8-inch
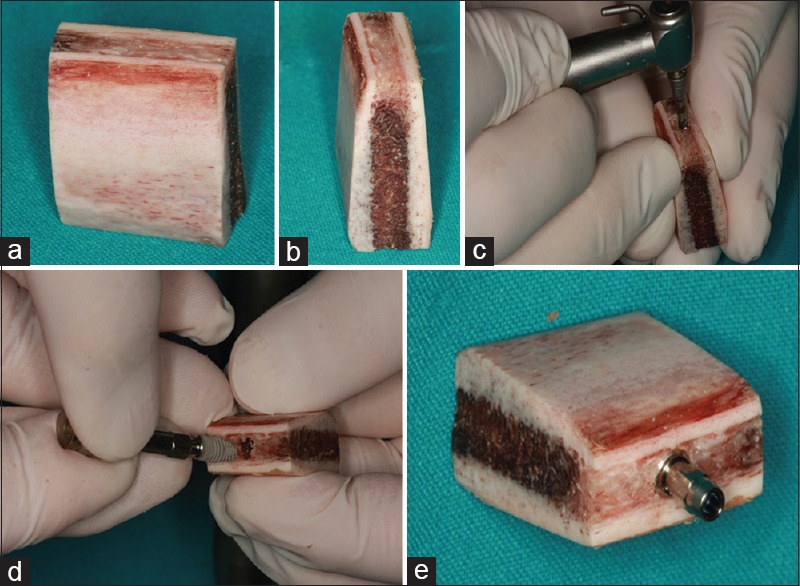
Using ½ and ¼ round burs (Teeskavan, Tehran, Iran), fenestration defects were created in the apical third of implants placed in the bone. For this purpose, the bone was removed in a semilunar fashion incrementally such that the shape of defects highly simulated the defects in the clinical setting. The fenestration defects were extended 0.5 mm beyond the anterior and posterior implant borders, and CBCT and PA radiographs were captured again using the aforementioned exposure settings [Figure 3].
Figure 3.
Images captured by NewTom (a), Planmeca (b), and Cranex 3D (c) cone-beam computed tomography systems of samples with fenestration defects. (New Tom: with defect, Planmeca: With defect, Cranex 3D: With defect)
Images were interpreted by two experienced maxillofacial radiologists (5 years of experience) blinded to the group allocation of images. Images were observed on a 20-inch monitor (LG, Seoul, Korea) in a semi-dark room. The observers were allowed to enhance the density and contrast of images or use magnification using a software.
The observers reported the presence or absence of defects in a checklist. The images were viewed again by the two observers after 2 weeks to assess the intra-observer agreement. Inter-observer agreement was also calculated using the kappa coefficient.
Data were analyzed using SPSS version 18 (SPSS Inc., IL, USA). Quantitative data were reported as mean and standard deviation and qualitative data were reported as number and percentage. Data were analyzed using Chi-square test, Fisher's exact test, McNemar's test, and Cochran's Q-test. The mean values were analyzed using one-way ANOVA. Level of significance was set at P = 0.05.
Results
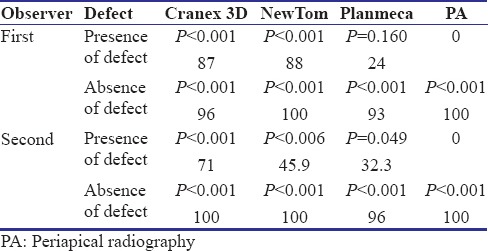
Table 1 shows the intra-observer agreement in the use of each imaging system using Cohen's kappa. As shown, the intra-observer agreement was significant for all imaging modalities (P < 0.001).
Table 1.
Intra-observer agreement in use of each imaging system for detection of defects using Cohen's kappa
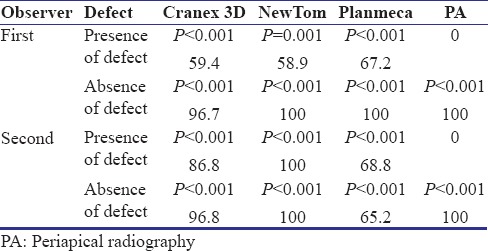
Table 2 shows the interobserver agreement for each imaging system using Cohen's kappa. As shown, the interobserver agreement was significant for all samples with no defects in all imaging systems and samples with bone defects in the use of Cranex 3D and NewTom systems. However, the interobserver agreement for detection of bone defects in the use of Planmeca CBCT system was not significant.
Table 2.
Interobserver agreement for each imaging system using Cohen's kappa
Using Cochran's Q-test, no significant difference was noted among the four imaging modalities for detection of the absence of defect (P = 0.3). However, this difference was significant in the presence of defects (P < 0.001). The results in this respect are presented in Table 3.
Table 3.
Comparison of the four imaging systems for detection of the presence/absence of defect using Cochran's Q-test
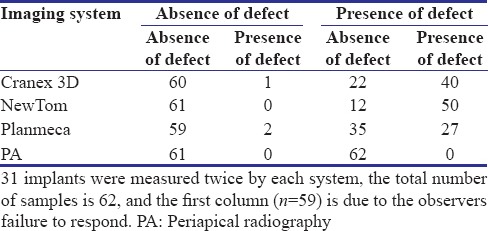
Thirty-one implants were measured twice by each system, the total number of samples is 62, and the first column (n = 59) is due to the observers failure to respond.
McNemar's test was applied for pairwise comparison of the groups with defects and the results are presented in Table 4.
Table 4.
Pairwise comparison of the groups with defects using McNemar's test (n=62)
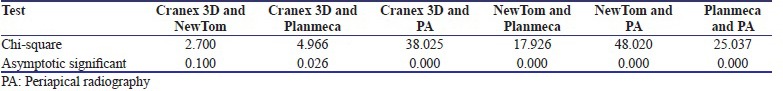
All pairwise comparisons were statistically significant (P < 0.05) except for the comparison of Cranex 3D and NewTom (P = 0.100). Using Cronbach's alpha, the intraclass correlation for the four imaging systems was found to be 0.438 (P = 0.012) and 0.510 (P = 0.002) for the first observer in the absence and presence of defects, respectively. These values were 0.350 (P = 0.044) and 0.464 (P = 0.006) for the second observer in the absence and presence of defects, respectively. Table 5 shows the sensitivity, specificity, positive predictive value, and negative predictive value of the four imaging systems.
Table 5.
Sensitivity, specificity, positive predictive value, and negative predictive value of the four imaging systems
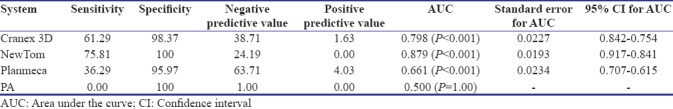
Figure 4 shows the area under the receiver operating characteristic (ROC) curve for the four systems. Since the area under the ROC curve was greater for NewTom, its diagnostic accuracy was higher than that of three other systems.
Figure 4.
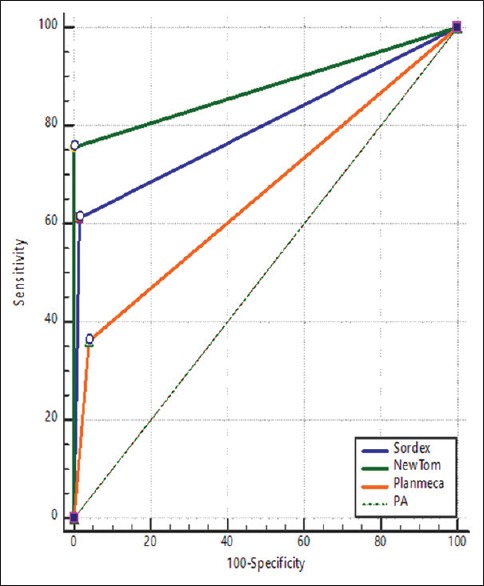
Area under the receiver operating characteristic curve for the four systems
Discussion
Dental implants are used to replace the lost teeth and provide optimal esthetics and function with no adverse effects on the adjacent soft and hard tissues. Success of dental implant treatment depends on the quality and quantity of bone. Inadequate cortical bone may lead to fenestration and dehiscence.
PA radiography is commonly used for the postoperative assessment of dental implants.[11,12] However, this modality cannot well visualize the buccal and lingual defects due to superimposition of anatomical structures. CBCT systems were introduced to overcome the shortcomings of conventional radiography. However, different types of CBCT systems are available, which are different in terms of diagnostic accuracy.
This study assessed the diagnostic accuracy of three CBCT systems and PA radiography for detection of fenestration around dental implants. The results showed a strong agreement between CBCT and reality for the first observer in the absence of defects. The kappa coefficient for Cranex 3D, NewTom 3G, and Planmeca was found to be 96.7, 100, and 100, respectively. These values were 96.8, 100, and 65.2 for the second observer, respectively. The agreement of PA radiography with reality was 100 and 100 for the first and second observers, respectively.
Kappa coefficient showed a strong agreement between Cranex 3D (86.8%) and NewTom 3G (100%) and reality for the second observer in the presence of defects. Thus, NewTom 3G CBCT system showed high agreement with reality. However, it should be noted that the difference in diagnostic accuracy of the three CBCT systems was not significant.
Patel et al.[13] compared the diagnostic accuracy of PA radiography and CBCT for detection of root resorption defects while Stavropoulos et al.[14] compared the diagnostic accuracy of PA radiography and CBCT for detection of PA lesions in pig jaws. Both studies showed that despite the differences in size and nature of lesions evaluated, the sensitivity of intraoral radiography was less than that of CBCT, irrespective of the size of lesions. However, in the study by Patel et al.,[13] ROC curve showed that although the diagnostic accuracy of PA radiography was acceptable, it was lower than that of CBCT. Furthermore, the intra- and inter-observer agreements in the use of CBCT were higher than those in use of PA radiography. These results were in agreement with ours.[13]
Stavropoulos et al.[14] evaluated that the sensitivity, diagnostic accuracy, and false negative and false positive of NewTom were significantly higher than those of digital and conventional PA radiography, but the specificity of all three systems was the same. Their results were in agreement with ours regarding higher sensitivity and diagnostic accuracy of NewTom CBCT and its equal specificity to that of PA radiography. Bagis et al.[4] and Dehghani et al.[15] compared the diagnostic accuracy of CBCT with PA radiography for detection of tunnel, fenestration, and dehiscence bone defects and showed higher diagnostic accuracy of CBCT than PA radiography.
Takeshita et al.[5] compared PA radiography and CBCT for detection and quantification of bone loss and indicated that the diagnostic accuracy of CBCT and the accuracy of measurements made on CBCT scans were both higher than PA radiography, which was in agreement with our results. Saati et al.[16] compared the diagnostic accuracy of NewTom 3G, Soredex, and Planmeca for detection of anatomical landmarks of dry human mandibles. In contrast to our results, they showed that Crane × 3D had the highest diagnostic accuracy followed by Planmeca and NewTom 3G. In their study, similar to ours, the voltage (kVp) of NewTom 3G CBCT system was higher than that of other systems, which would result in greater beam scattering and noise and eventually more difficult detection of anatomical landmarks, especially finer structures. Kasraei et al.[17] compared the diagnostic accuracy of several imaging modalities for detection of recurrent caries under composite restorations. Contrary to our findings, they demonstrated that Cranex 3D was superior to NewTom 3G for this purpose. Difference between our findings and the results of the abovementioned studies may be attributed to the absence of metal structures (which would create artifact) in the aforementioned two studies, since metal artifacts can significantly compromise the diagnostic accuracy of imaging and also with increasing kV, the artifact decreases and the defects are better detected.
The quality of CBCT images is influenced by artifacts, noise, and lower contrast of soft tissue covering the hard tissue. When a defect is adjacent to a dental implant, a radiolucent area is formed. This can also occur due to beam hardening, complicating accurate detection of defects. Metal artifacts also decrease the sensitivity of diagnostic modalities. Thus, the presence of amalgam restorations and metal crowns also lower the diagnostic accuracy. Our study had an in vitro design and there was no metal restoration to compromise the accuracy of results. This is far from the situation in the clinical setting and should be taken into account when interpreting the results. Wax was used in our study to simulate peri-implant soft tissue as in some previous studies.[4,16] However, data regarding the effect of soft-tissue simulation on CBCT image quality are limited and further studies are required to better simulate the clinical setting. Also, since artificially created lesions have a distinct border, it is recommended to use acid for the creation of defects with irregular borders to better simulate the clinical setting. Furthermore, the study should be done on a larger sample sizes and taking live patients into consideration in order to gain more valuable results.
Within the limitations of CBCT systems (different kVp used by different systems, artifacts, and noises that influences image quality), the results showed that CBCT systems were more efficient than PA radiography for correct diagnosis of the presence or absence of fenestration around dental implants. Among the three CBCT systems evaluated in this study, NewTom 3G showed the highest diagnostic accuracy for detection of fenestration around dental implants.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Lekholm U, Zarb G. Patient selection and preparation. DMFR. 2013;14:40–58. [Google Scholar]
- 2.de-Azevedo-Vaz SL, Vasconcelos Kde F, Neves FS, Melo SL, Campos PS, Haiter-Neto F, et al. Detection of periimplant fenestration and dehiscence with the use of two scan modes and the smallest voxel sizes of a cone-beam computed tomography device. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115:121–7. doi: 10.1016/j.oooo.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 3.Haghgoo JM, Shokri A, Khodadoustan A, Khoshhal M, Rabienejad N, Farhadian M. Comparison the accuracy of the cone-beam computed tomography with digital direct intraoral radiography, in assessment of periodontal osseous lesions. Avicenna J Dent Res. 2014;6:1–6. [Google Scholar]
- 4.Bagis N, Kolsuz ME, Kursun S, Orhan K. Comparison of intraoral radiography and cone-beam computed tomography for the detection of periodontal defects: An in vitro study. BMC Oral Health. 2015;15:64. doi: 10.1186/s12903-015-0046-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Takeshita WM, Vessoni Iwaki LC, Da Silva MC, Tonin RH. Evaluation of diagnostic accuracy of conventional and digital periapical radiography, panoramic radiography, and cone-beam computed tomography in the assessment of alveolar bone loss. Contemp Clin Dent. 2014;5:318–23. doi: 10.4103/0976-237X.137930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Razavi T, Palmer RM, Davies J, Wilson R, Palmer PJ. Accuracy of measuring the cortical bone thickness adjacent to dental implants using cone beam computed tomography. Clin Oral Implants Res. 2010;21:718–25. doi: 10.1111/j.1600-0501.2009.01905.x. [DOI] [PubMed] [Google Scholar]
- 7.Eskandarloo A, Mirshekari A, Poorolajal J, Mohammadi Z, Shokri A. Comparison of cone-beam computed tomography with intraoral photostimulable phosphor imaging plate for diagnosis of endodontic complications: A simulation study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114:e54–61. doi: 10.1016/j.oooo.2012.05.026. [DOI] [PubMed] [Google Scholar]
- 8.Shokri A, Eskandarloo A, Noruzi-Gangachin M, Khajeh S. Detection of root perforations using conventional and digital intraoral radiography, multidetector computed tomography and cone beam computed tomography. Restor Dent Endod. 2015;40:58–67. doi: 10.5395/rde.2015.40.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shokri A, Mortazavi H, Salemi F, Javadian A, Bakhtiari H, Matlabi H, et al. Diagnosis of simulated external root resorption using conventional intraoral film radiography, CCD, PSP, and CBCT: A comparison study. Biomed J. 2013;36:18–22. doi: 10.4103/2319-4170.107156. [DOI] [PubMed] [Google Scholar]
- 10.Shokri A, Khajeh S, Khavid A. Evaluation of the accuracy of linear measurements on lateral cephalograms obtained from cone-beam computed tomography scans with digital lateral cephalometric radiography: An in vitro study. J Craniofac Surg. 2014;25:1710–3. doi: 10.1097/SCS.0000000000000908. [DOI] [PubMed] [Google Scholar]
- 11.De Smet E, Jacobs R, Gijbels F, Naert I. The accuracy and reliability of radiographic methods for the assessment of marginal bone level around oral implants. Dentomaxillofac Radiol. 2002;31:176–81. doi: 10.1038/sj/dmfr/4600694. [DOI] [PubMed] [Google Scholar]
- 12.Wakoh M, Harada T, Otonari T, Otonari-Yamamoto M, Ohkubo M, Kousuge Y, et al. Reliability of linear distance measurement for dental implant length with standardized periapical radiographs. Bull Tokyo Dent Coll. 2006;47:105–15. doi: 10.2209/tdcpublication.47.105. [DOI] [PubMed] [Google Scholar]
- 13.Patel S, Kanagasingam S, Mannocci F. Cone beam computed tomography (CBCT) in endodontics. Dent Update. 2010;37:373–9. doi: 10.12968/denu.2010.37.6.373. [DOI] [PubMed] [Google Scholar]
- 14.Stavropoulos A, Wenzel A. Accuracy of cone beam dental CT, intraoral digital and conventional film radiography for the detection of periapical lesions. An ex vivo study in pig jaws. Clin Oral Investig. 2007;11:101–6. doi: 10.1007/s00784-006-0078-8. [DOI] [PubMed] [Google Scholar]
- 15.Dehghani M, Montazer Lotf Elahi H. Comparing the accuracy of cone beam computed tomography, digital intraoral radiography and conventional intraoral radiography in the measurement of periodontal bone defects. J Res Dent Maxillofac Sci. 2015;1:123–32. [Google Scholar]
- 16.Saati S, Kaveh F, Yarmohammadi S. Comparison of cone beam computed tomography and multi slice computed tomography image quality of human dried mandible using 10 anatomical landmarks. J Clin Diagn Res. 2017;11:ZC13–6. doi: 10.7860/JCDR/2017/20637.9253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kasraei S, Shokri A, Poorolajal J, Khajeh S, Rahmani H. Comparison of cone-beam computed tomography and intraoral radiography in detection of recurrent caries under composite restorations. Braz Dent J. 2017;28:85–91. doi: 10.1590/0103-6440201701248. [DOI] [PubMed] [Google Scholar]