Abstract
Background:
The aim of this study was to compare the clinical and radiographic outcomes of partial and complete caries removal (CCR) in permanent teeth with deep carious lesions.
Materials and Methods:
One hundred and forty-three patients of age group 14–54 years with mature permanent molars having deep carious lesions were divided into two groups: partial caries removal (PCR) and CCR. A layer of soft, wet carious dentin was left adjacent to pulpal wall in PCR group, whereas in CCR group, complete infected caries was removed with the help of caries-detector dye. Teeth were restored with composite resin (Tetric N-Ceram; Ivoclar Vivadent), with base of resin-modified glass ionomer cement (RMGIC) and patients were recalled at 1, 3, 6, 12, and 18 months. Success was defined as absence of signs and symptoms of irreversible pulpitis (spontaneous pain, fistula, and swelling) and absence of periapical alterations (radiolucency at furcal or periapical region).
Results:
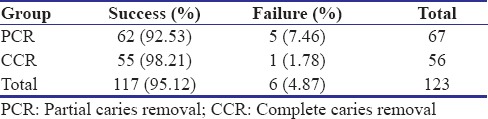
Pulp exposure occurred in 13 (9.55%) cases of CCR group. Statistical significant difference (P = 0.001) in terms of pulp exposure was found between two groups. After 18 months, 123 teeth were evaluated (CCR = 56 and PCR = 67) and the success rate in CCR group (98.21%) and the PCR group (92.53%) did not differ significantly (P = 0.115).
Conclusion:
PCR could be as an elective treatment option for the mature permanent teeth with deep carious lesions.
Keywords: Caries, pulp exposure, vitality
Introduction
Management of deep carious lesions in recent years has been changed from complete caries removal (CCR) to partial caries removal (PCR). PCR has gained importance due to less pulpal exposure, no interference in pulpal vitality, and no postoperative complications.[1,2,3] Vitality of pulp is preserved because it improves survival prognosis, defensive mechanisms, tooth sensitivity, and proprioception.[4,5] Maintaining the vital pulp also helps reduce the occurrence of apical periodontitis by blocking bacterial infections.[6] Thus, from a biological and cost perspective, preservation of healthy portion of the pulp is essential for maintaining its healing ability.
Conventionally, CCR was considered as gold standard, but now, partial caries is evidenced by literature clinically, biochemically, radiographically, microbiologically, and histologically.[7,8,9] PCR is cost-effective, patient-friendly, less technique sensitive, avoids the need of endodontic treatment in case of pulpal exposure, and avoids multivisits of patient to clinic. Clinical trials with long-term follow-up periods have demonstrated that accurate assessment of preoperative pulpal status and proper cavity sealing are extremely important factor for the success of vital pulp therapy, regardless of the material used for protection and induction of the remaining carious dentin.[10,11]
Despite the advantages of partial caries excavation, 70% of dentists and patients prefer complete caries excavation due to fear of progress of remaining dentin caries to the pulp and low restoration survival.[12] A recent systemic review suggested that the need of high-quality randomized controlled trial in future due to high risk of bias, poor randomization, high dropout, and blinding of operators and examiners was not done in the included studies.[13] To our knowledge, only two studies (Orhan et al. and Franzon et al.) compared the success of one step partial and complete caries excavation; both of these studies were conducted in deciduous and young permanent teeth (mean age: 8 years). Till now, no randomized controlled trial has been conducted in mature permanent teeth that compared the clinical and radiographic outcomes of one step partial and complete caries excavation.
Thus, the aim of this study was to compare the clinical and radiographic outcomes of PCR and CCR in permanent teeth with deep carious lesions with regard to pulpal health. Null hypothesis was that there was no difference with regard to pulpal health between two groups.
Materials and Methods
The present study was conducted following approval by the Ethics Committee (PGIDS/IEC/2015/65) of the Postgraduate Institute of Dental Sciences (PGIDS), Rohtak. Study participants were recruited from the pool of patients referred to the Postgraduate Department of Conservative Dentistry and Endodontics of PGIDS, Rohtak.
Mature permanent mandibular molars having deep carious lesions involving half or more of the dentine detected by radiographic examination (occlusal, occlusal with buccal and lingual extension), confirmed as vital teeth using the electric pulp test (Digitest D626D; Parkell Electronics, New York, USA) and the cold test (Endo-Ice, Coltene, Whaledent), and the absence of apical radiolucency were included. Patients were excluded if they presented with signs and symptoms of irreversible pulpitis, swelling, fistula, and mobility. Sample size calculation was based on a difference in the percentage of success of complete 62% (Bjørndal et al.[14]) versus partial removal of caries 92% (Franzon et al.[2]) using a significance level of 5% and power of 80%. A sample size of 33 teeth per group was calculated. Given an expected attrition rate of 20%, we estimated that 43 teeth had to be included in each group.
Randomization was developed to eliminate any bias on the part of the investigators and to equalize the number of patients between the two treatment groups. Using an equal proportion randomization allocation ratio, one of the investigators (M. J.) created envelopes containing concealed assignment codes that were assigned sequentially to eligible patients. Informed consent explaining benefits and risks of treatment was taken from patients before participation in the trial.
Clinical procedures
The procedure was performed under local anesthesia and rubber dam isolation. Carious tissue from the lateral walls and dentinoenamel junction was removed completely using low-speed metal burs and/or hand excavator. Superficial necrotic dentin was removed from the pulpal and axial wall using low-speed round bur. A layer of soft, wet carious dentin was left adjacent to pulpal wall [Figure 1] and cavity was cleaned with distilled water and gently dried with air and moist cotton pellet. In CCR, a caries-detector dye (Kurary, Medical Inc, Tokyo, Japan) was applied to dentin for 10 s, followed by washing. This procedure was repeated until the dentin was no longer stained [Figure 2]. Resin-modified glass ionomer cement (RMGIC) (Fuji Lining LC; GC, Tokyo, Japan) was applied to the pulpal wall after conditioning, followed by etching with 37% phosphoric acid for 15 s. All cavities were restored with composite resin (Tetric N-Ceram; Ivoclar Vivadent), using the incremental technique and each increment was polymerized for 40 s. The rubber dam was then removed and occlusion was checked. In cases of pulp exposure direct pulp capping, pulpotomy and root canal treatment was performed.
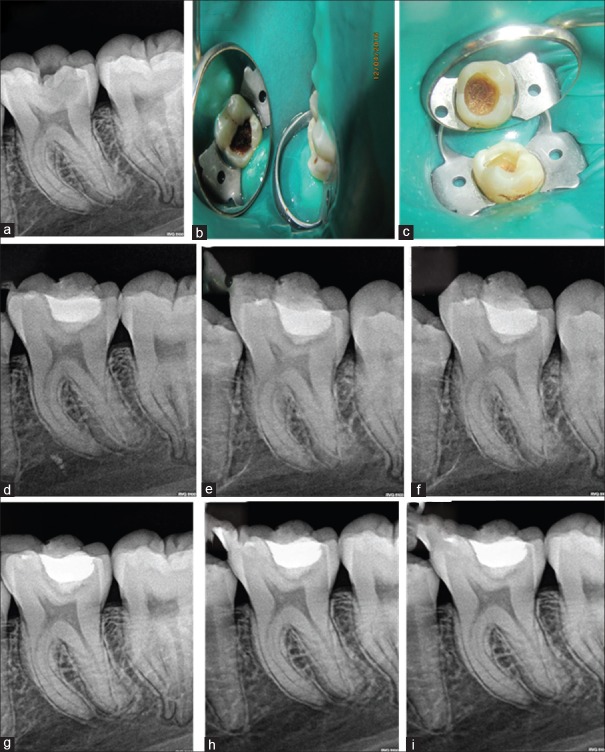
Figure 1.
Partial caries removal case: Preoperative radiograph (a), preoperative photograph (b), photograph after partial caries removal (c), radiograph at baseline after composite restoration (d), radiograph at 1 month (e), radiograph at 3, 6, 12, and 18 months (f-i)
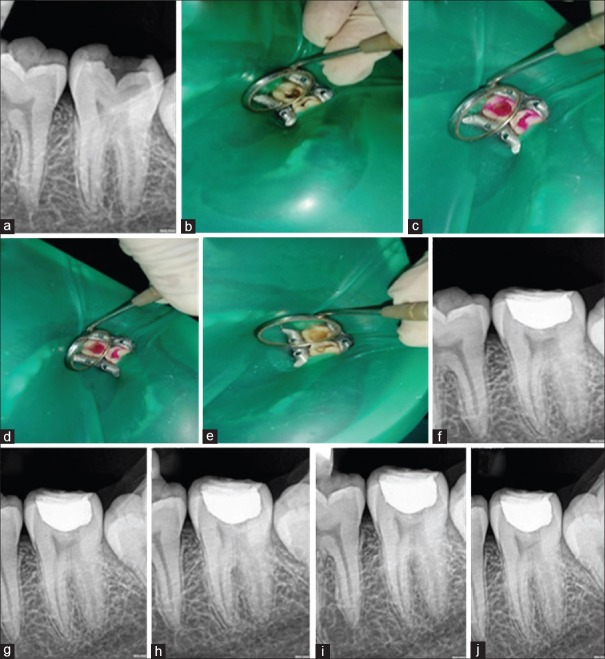
Figure 2.
Complete caries removal case: Preoperative radiograph (a), preoperative photograph (b), photograph after apple of caries detector dye (c), photograph after wash of dye (d), photograph after complete removal of caries (e), radiograph at 1 month (f), radiograph at 3, 6, 12, and 18 months of follow-up (g-j)
Outcome
Two blinded examiners assessed the clinical and radiographic outcomes of test and control treatments at 1, 3, 6, 12, and 18 months after treatment. Success was defined as positive response to cold and electric pulp test, absence of signs and symptoms of irreversible pulpitis (spontaneous pain, fistula, and swelling) and absence of periapical alterations (radiolucency at furcal or periapical region) (combined outcome). Digital radiographs were taken with standardized exposure parameters (70 kvp, 3.5 mAs, and 0.2 s) by a single operator according to a standardized procedure by placement of film holders (XCP-DS Carestream) in paralleling technique. All radiographs were obtained by the same digital imaging system (Kodak RVG 5200; Carestream Dental).
Statistical analysis
Categorical variables were compared using Chi-square test. Statistical analyses were performed using SPSS version 20.0 (Statistical Package for the Social Science) software (Armonk, NY: IBM Corp). The statistical significance of the data were determined at P ≤ 0.05.
Results
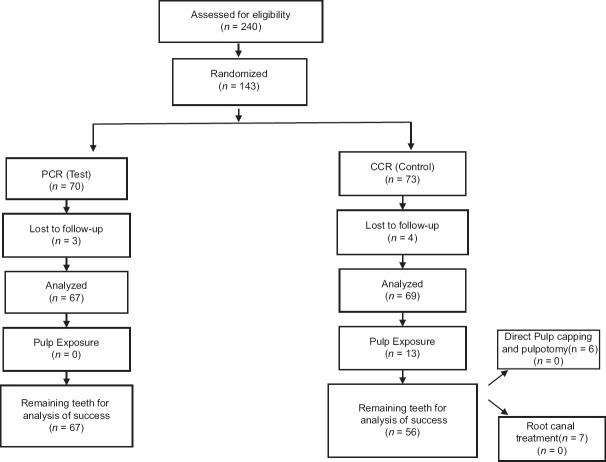
Of the 143 treatments performed, 70 received pretreatment PCR and 73 received CCR. The patients' ages ranged from 14 to 54 years (maximum: 54 years, minimum: 14 years, and mean age: 25.19 years). Due to loss of contact, there was loss of 7 patients (PCR: 3 and CCR: 4) [Figure 3]. Of 136 treatments left, 79 (58. 08%) were first molar and 57 (41.91%) were second molar. There was no significant difference between the two groups with respect to baseline characteristics such as age, gender, type of tooth, and site of lesion [Table 1]. Among 136 teeth, total pulp exposure occurred in 13 (9.55%), and these cases belong to CCR group. Statistically significant difference (P = 0.001) in terms of pulp exposure was found between two groups. No significant difference in pulp exposure in relation to site was found [Table 2]. The overall clinical and radiographic success rate after excluding teeth with pulp exposure was 95.12% after 18 months. Success rate in CCR group after excluding teeth with pulp exposure (98.21%) and the PCR group (92.53%) did not differ significantly (P = 0.115) [Table 3]. All failures detected were evaluated histologically; three cases showed completely necrotic pulp chamber at the 4th month, two with liquefactive necrosis and one with reversible pulpitis with moderate inflammation. The four cases of direct pulp capping and pulpotomy were followed separately and no clinical and radiographic failure was evaluated after 18 months.
Figure 3.
Study design
Table 1.
Demographics of patients participating in the study
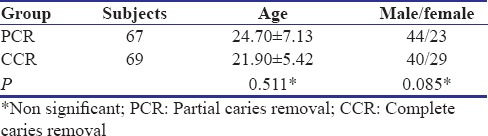
Table 2.
Comparison of pulp exposure occurrence
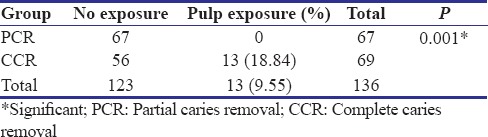
Table 3.
Comparison of clinical and radiographic success
Discussion
Indirect pulp treatment is a conservative treatment modality to save pulp for the management of deep carious lesions. However, there is no precise conclusion as to whether it should be performed in single, double sitting, or complete removal of caries in single sitting. Lack of studies comparing clinical and radiographic outcomes in permanent teeth inspired us to carry out this study.
The findings of this study showed statistically significant difference in pulp exposure between partial and CCR with low proportion of exposure in PCR. In our excavation trial, fewer pulp exposure (18.88%) occurred in CCR group than previous studies of Leksell et al.[15] (40%), Franzon et al.[2] (27%), and Orhan et al.[3] (22%). This may be due to minimally invasive caries excavation procedure carried out in this study, performed by a single operator as compared to multiple operators in previous studies. Second, we included teeth with >50% of caries depth as compared to 75% of dentin depth included in other studies.
The high clinical and radiographic success rate in PCR after 18 months suggests that PCR may be as effective as CCR in permanent teeth with additional advantage of reduction of pulp exposures. The observed success rate of PCR coincides with clinical studies of Maltz et al. (99% at 18 months), Franzon et al. in primary teeth (92% at 24 months), and Orhan et al. in young permanent teeth (100% at 1-year follow-up). The higher success rate in PCR could be attributed to proper sealing, reduction of exogenous nutrient supply, and stabilization of remaining carious dentine by adhesive resin restoration.[8,10,16]
There is also no clear recommendation on which depth caries needs to be removed. Some studies removed just enamel, others recommended removal of affected enamel and some dentin, leaving soft and moist carious on the floor.[8,16,17] The protocol followed in our study was complete removal of carious tissue from cavity walls but limited removal from the pulpal floor and axial wall. Dye was used in the other group to reduce visual and tactile subjectivity; however, it is less caries specific, results in excessive removal of totally sound tooth structure and increased likelihood of mechanical pulp exposures. Hence, should be used judiciously and with caution.
RMGIC was used as base due to less moisture sensitivity, higher shear bond strength to composites than conventional GIC.[18,19] In contrast to the studies of Franzon et al. and Orhan et al., calcium hydroxide was not used due to its high solubility and hydrolyze over time that reduces the area for bonding, low compression resistance, and no adherence to dental substrates.
Histological evaluation of failure cases showed that clinically vital pulp may histologically undergo pulp necrosis. Unfortunately, still, there is no reliable instrument to accurately assess the preoperative condition of pulp. Hence, preoperative diagnosis should be made precisely with proper patient history, signs and symptoms, radiographs, and pulp sensibility tests. Randomization, less attrition of follow-up, single operator, standardized treatment protocol, and histological evaluation of failure cases were the strengths of this study attributed to high level of evidence in this study. Major limitations of this study were that randomization was performed before caries excavation that may cause bias in the study.
Conclusion
Within the limitations of the study, the findings of the study showed positive clinical and radiographic outcomes, suggesting partial caries excavation as an elective treatment option in management of deep carious lesions in everyday practice to maintain pulp vitality.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Maltz M, Jardim JJ, Mestrinho HD, Yamaguti PM, Podestá K, Moura MS, et al. Partial removal of carious dentine: A multicenter randomized controlled trial and 18-month follow-up results. Caries Res. 2013;47:103–9. doi: 10.1159/000344013. [DOI] [PubMed] [Google Scholar]
- 2.Franzon R, Guimarães LF, Magalhães CE, Haas AN, Araujo FB. Outcomes of one-step incomplete and complete excavation in primary teeth: A 24-month randomized controlled trial. Caries Res. 2014;48:376–83. doi: 10.1159/000357628. [DOI] [PubMed] [Google Scholar]
- 3.Orhan AI, Oz FT, Orhan K. Pulp exposure occurrence and outcomes after 1- or 2-visit indirect pulp therapy vs.complete caries removal in primary and permanent molars. Pediatr Dent. 2010;32:347–55. [PubMed] [Google Scholar]
- 4.Caplan DJ, Cai J, Yin G, White BA. Root canal filled versus non-root canal filled teeth: A retrospective comparison of survival times. J Public Health Dent. 2005;65:90–6. doi: 10.1111/j.1752-7325.2005.tb02792.x. [DOI] [PubMed] [Google Scholar]
- 5.Ou KL, Chang CC, Chang WJ, Lin CT, Chang KJ, Huang HM, et al. Effect of damping properties on fracture resistance of root filled premolar teeth: A dynamic finite element analysis. Int Endod J. 2009;42:694–704. doi: 10.1111/j.1365-2591.2009.01570.x. [DOI] [PubMed] [Google Scholar]
- 6.Gesi A, Hakeberg M, Warfvinge J, Bergenholtz G. Incidence of periapical lesions and clinical symptoms after pulpectomy – A clinical and radiographic evaluation of 1- versus 2-session treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:379–88. doi: 10.1016/j.tripleo.2005.05.073. [DOI] [PubMed] [Google Scholar]
- 7.Maltz M, de Oliveira EF, Fontanella V, Bianchi R. A clinical, microbiologic, and radiographic study of deep caries lesions after incomplete caries removal. Quintessence Int. 2002;33:151–9. [PubMed] [Google Scholar]
- 8.Lula EC, Monteiro-Neto V, Alves CM, Ribeiro CC. Microbiological analysis after complete or partial removal of carious dentin in primary teeth: A randomized clinical trial. Caries Res. 2009;43:354–8. doi: 10.1159/000231572. [DOI] [PubMed] [Google Scholar]
- 9.Maltz M, Henz SL, de Oliveira EF, Jardim JJ. Conventional caries removal and sealed caries in permanent teeth: A microbiological evaluation. J Dent. 2012;40:776–82. doi: 10.1016/j.jdent.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 10.Corralo DJ, Maltz M. Clinical and ultrastructural effects of different liners/restorative materials on deep carious dentin: A randomized clinical trial. Caries Res. 2013;47:243–50. doi: 10.1159/000345648. [DOI] [PubMed] [Google Scholar]
- 11.Pinto AS, de Araújo FB, Franzon R, Figueiredo MC, Henz S, García-Godoy F, et al. Clinical and microbiological effect of calcium hydroxide protection in indirect pulp capping in primary teeth. Am J Dent. 2006;19:382–6. [PubMed] [Google Scholar]
- 12.Oen KT, Thompson VP, Vena D, Caufield PW, Curro F, Dasanayake A, et al. Attitudes and expectations of treating deep caries: A PEARL network survey. Gen Dent. 2007;55:197–203. [PubMed] [Google Scholar]
- 13.Schwendicke F, Dörfer CE, Paris S. Incomplete caries removal: A systematic review and meta-analysis. J Dent Res. 2013;92:306–14. doi: 10.1177/0022034513477425. [DOI] [PubMed] [Google Scholar]
- 14.Bjørndal L, Reit C, Bruun G, Markvart M, Kjaeldgaard M, Näsman P, et al. Treatment of deep caries lesions in adults: randomized clinical trials comparing stepwise vs. direct complete excavation, and direct pulp capping vs. partial pulpotomy. Eur J Oral Sci. 2010;118:290–7. doi: 10.1111/j.1600-0722.2010.00731.x. [DOI] [PubMed] [Google Scholar]
- 15.Leksell E, Ridell K, Cvek M, Mejàre I. Pulp exposure after stepwise versus direct complete excavation of deep carious lesions in young posterior permanent teeth. Endod Dent Traumatol. 1996;12:192–6. doi: 10.1111/j.1600-9657.1996.tb00513.x. [DOI] [PubMed] [Google Scholar]
- 16.Ribeiro CC, Baratieri LN, Perdigão J, Baratieri NM, Ritter AV. A clinical, radiographic, and scanning electron microscopic evaluation of adhesive restorations on carious dentin in primary teeth. Quintessence Int. 1999;30:591–9. [PubMed] [Google Scholar]
- 17.Mertz-Fairhurst EJ, Curtis JW, Jr, Ergle JW, Rueggeberg FA, Adair SM. Ultraconservative and cariostatic sealed restorations: Results at year 10. J Am Dent Assoc. 1998;129:55–66. doi: 10.14219/jada.archive.1998.0022. [DOI] [PubMed] [Google Scholar]
- 18.Palma-Dibb RG, de Castro CG, Ramos RP, Chimello DT, Chinelatti MA. Bond strength of glass-ionomer cements to caries-affected dentin. J Adhes Dent. 2003;5:57–62. [PubMed] [Google Scholar]
- 19.Sidhu SK. Glass-ionomer cement restorative materials: A sticky subject? Aust Dent J. 2011;56(Suppl 1):23–30. doi: 10.1111/j.1834-7819.2010.01293.x. [DOI] [PubMed] [Google Scholar]