Abstract
Background
Unicompartmental knee arthroplasty (UKA) originated in the 1950's. There have been many enhancements to the implants and the technique, improving the precision and accuracy of this challenging operation. Specifically for Robotic Arm Interactive Orthopedic System (Rio; Mako Stryker, Fort Lauderdale, FL), there are many studies reporting clinical outcomes, but our search offered nothing regarding patient reported outcomes using validated surveys.
Methods
Patients with onlay tibial components presenting for routine follow-up of robotic-arm assisted UKA performed between May 2009 and September 2013 were invited to participate. Four joints had simultaneous patella femoral resurfacing. Knee Injury and Osteoarthritis Outcomes Score (KOOS) and the 2011 Knee Society Scores were collected. Radiographic evidence of osteoarthritis in the non-operative knee compartments was documented.
Results
Eighty-one patients presented for follow-up and consented to participate. Mean follow up was 54 months. Mean patient reported KOOS activities of daily living and pain scores were each 90. Knee Society 2011 mean objective score was 96 and mean function score 81. There was one revision to total knee at 40 months post-op for pain after injury. Seventy-seven percent reported their knee always felt “Normal”, 20% sometimes, and only 3% reported that it never felt normal.
Conclusion
Literature on UKA failure rates suggests that UKA may be a less forgiving procedure than total knee arthroplasty. Robotic-arm assisted surgery is reported to improve the accuracy of implant placement. Based on our prospectively collected positive patient outcomes, the authors have achieved good results from performing robotic-arm assisted UKA on select patients.
Keywords: Robotic assisted, Unicompartmental knee, MakoPlasty, Unicondylar knee arthroplasty
1. Introduction
The introduction of robotic-arm assisted technology for unicondylar knee arthroplasty (UKA) has revolutionized this challenging procedure. Prior to robotic technology, poor implant positioning was blamed for the high rate of revision in manual UKA procedures.1, 2, 3, 4, 5 The robotic technology allows for precise component placement and ligament balancing that has improved clinical and radiographic outcomes in patients with isolated medial knee arthritis.1, 2, 3, 4, 5, 6, 7, 8, 9, 10
What we do not have is data on how our patients feel about their knees two or more years after surgery. Is there pain? How well can you perform daily activities? Does it feel normal? With the shift toward patient-centered care, it is essential to focus on patient reported outcomes (PRO) as well as clinical results.
2. Materials and methods
One hundred and fifty-three patients underwent robotic-arm assisted UKA with a metal backed onlay tibial component between May 2009 and September 2013. Surgery was performed by authors DAC and TMS. Both surgeons had experience using robotic technology for nine months prior with each performing at least 18 robotic-arm assisted medial unicondylar knee arthroplasties with all-poly inlay tibial components. All patients presenting in clinic for routine follow-up at a minimum two-years after medial unicondylar knee arthroplasty with a metal backed onlay tibial component, were asked to participate in this Institutional Review Board approved study. Patients that were not already scheduled received phone calls, letters, and emails reminding them that their annual follow-up was due. Eighty-four of the 153 possible study participants presented in clinic for routine follow-up. Eighty-one completed the informed consent process and were enrolled in the study. Sixty-nine of the possible participants did not come in for follow-up. Of those 69, 12 were deceased due to causes other than the knee. Twenty-one could not be located. Fifteen did not show up for their appointments and did not reschedule. The ten that returned phone calls said they were doing great, were happy with their knee and would come in only if they had a problem. Five had health issues other than their knee that prevented them from coming in. Five had no insurance and were not willing to pay for a visit but said they were having no issues with their knee. One subject was incarcerated in another state and one had been dismissed from the practice due to substance abuse. Sixteen subjects had bilateral procedures with four performed simultaneously. There were four knees in three patients that had simultaneous patellofemoral arthroplasty.
The Knee Injury and Osteoarthritis Outcome Score (KOOS) and the 2011 Knee Society Scoring System were administered using a combination of self-administration followed by live interview to ensure that no questions were missed11,12 The 2011 Knee Society Score was chosen over the 1989 version due to the improved subjective patient reported component. The American Joint Replacement Registry was used as a data receptacle to calculate the scores. Routine annual clinical exam was performed and knee radiographs were obtained. Radiographs were assessed using the Kellgren-Lawrence Classification System to classify disease progression, if any, in the lateral compartment and the patellofemoral compartment in those patients without patellofemoral arthroplasty.13 Pain levels specific to the lateral and patellofemoral compartments were also documented by the physician using a 0 to 10 pain scale with 0 being no pain and 10 being the worst pain. The physician questioned the subject regarding their pain unlike the 2011 Knee Society Score where the pain level was self-reported. Retrospective chart review was performed to collect history and physical findings as well as peri-operative data and length of stay.
Contraindications for UKA vary widely and during the time these surgeries were performed, highly debated.14 Kozinn and Scott (1989) suggested exclusion of patients who weighed greater than 180 pounds, patients younger than age 60, patients who had more than minimal changes in the patellofemoral compartment, patients with anterior knee pain, patients with varus deformity greater than 10°, patients who were physically active or performed heavy labor, had a flexion contracture greater than 15°, inflammatory arthropathy, range of motion less than 90°, and anterior cruciate ligament deficiency.15 This was considered the gold standard by many until Pandit et al. (2011) reported that these outdated contraindications for UKA could be ignored at least for mobile bearing UKA.14 In our series of patients, we took the original gold standard contraindications into consideration but also looked at the individual patient regarding age, activity level, BMI, radiographic assessment, clinical exam, and expectations when making the decision to perform UKA versus TKA. The main reason for not explicitly adhering to the gold standard is that patients are individuals with different expectations and do not always fit into defined categories. As a result, seventy percent of the subjects in this study weighed more than 180 pounds and 38% were less than 60 years of age. More recently, Berend et al. (2015) reported a consensus statement from 6 surgeons with a combined experience of 8000 partial knees. The new gold standard for contraindications to UKA in general, is limited to systemic inflammatory arthropathy and previous high tibial osteotomy.16
2.1. Surgical technique
Stryker's Mako ™ robotic-arm assisted UKA was performed using the following surgical technique: The patient was taken to the operating room and placed in the supine position on the operating table. General anesthesia was then induced. The operative site was then prepped and draped in sterile fashion. A time out procedure was performed confirming operative site, preoperative antibiotics given, and equipment available. Percutaneous incisions were made over the femur and tibia and guide pins were placed using a power drill. Tracking devices for the robotic procedure were then attached to the guide pins. The limb was then taken through a range of motion to determine the hip center of rotation and points were taken of the medial and lateral ankle using the green probe. A longitudinal incision was then performed over the right medial knee from the superior patella to the medial proximal tibia and carried down through skin and subcutaneous tissue. A medial parapatellar arthrotomy was then made with a small extension into the vastus medialis obliqus. Checkpoints were then placed in the femur and tibia. Using a probe, the position of the checkpoints was confirmed. The femur was then registered, followed by the tibia. Osteophytes were then removed around the medial joint. The knee was then taken through a range of motion and applying a corrective force, these points were taken at varying degrees of motion. Next, slight adjustments were made to the preoperative plan to optimize tracking and stability. After confirming registration of the Mako System, the femoral resection was performed, followed by the tibial resection. Additional osteophytes were then removed. Trial components were placed and the knee was taken through a range of motion, comparing the position to the preoperative plan. After noting they were similar, the trials were removed. The checkpoints and guide pins were removed. The knee was irrigated with a pulsatile lavage containing polymyxin B 500,000 units, and the bony surfaces dried. The components were then cemented into place removing excess cement. A trial polyethylene insert was used and compression applied to the joint. After the cement cured, the trial polyethylene was removed and the joint checked for osteophytes and retained cement. The joint was irrigated again, and the definitive polyethylene was locked into place. After a final check of range of motion and stability, the tourniquet was deflated and hemostasis achieved. The capsule and percutaneous incisions were injected with a mixture of 40 ml 0.5% ropivacaine, Epinephrine 1:1000, 30 mg ketorolac, 10 mg morphine, and 80 ml 0.9% injectable NACL and the wounds closed in layers. A sterile dressing was applied. The irrigation solution and peri-articular injection components were considered appropriate at the time of the surgery but have changed since 2013.
2.2. Statistical analysis
Pearson's and Spearman's correlation coefficients were calculated to assess the link and the degree of relation between variables BMI, ASA scores, age, gender, and length of follow-up, with the KOOS, and Knee Society Scores. The correlation coefficient was considered very weak if smaller than 0.19, weak if 0.20 to 0.39, moderate from 0.40 to 0.59, strong from 0.60 to 0.79 and very strong if higher than 0.80. All statistical tests were considered significant at the 0.05 threshold. Implant survivorship was calculated and plotted using the Kaplan Meier Estimator.
3. Results/discussion
There were 47 (58%) females and 34 (42%) males. The mean age at surgery was 62 ± 10 (range 38–81) with a body mass index of 31.7 ± 4.8 (range 21.12–45.35). Mean length of symptoms prior to surgical intervention was 2.73 years (range 0.25–15 years). Mean follow-up was 54 months (range 24–85). Mean tourniquet time was 81 min (range 60–167) and the mean length of stay was 1.5 days (range 1.8–3.4). The American Society of Anesthesiology Classification (ASA) as determined by the anesthesiologist, was a 2 for 48% of the subjects, 46% were classified as a 3, and 6% were classified as a 4.
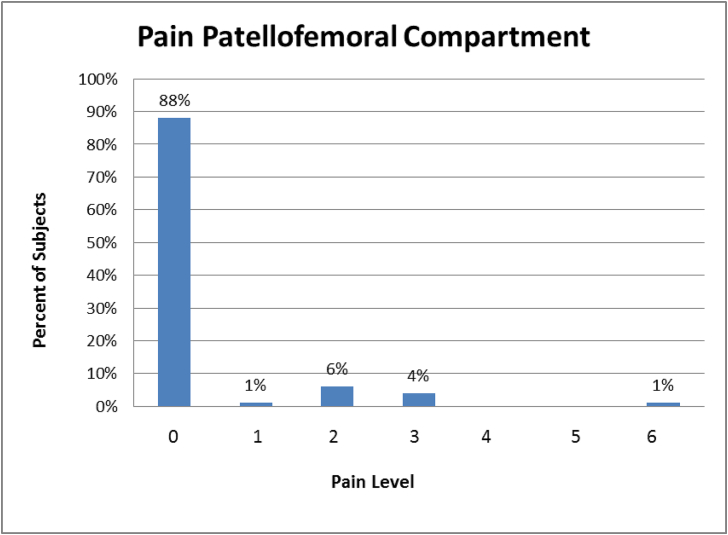
Radiographic assessment was performed at last follow-up on 80 subjects since one subject refused x-rays. The Kellgren–Lawrence Classification (Table 1) revealed no evidence of osteoarthritis (OA) in the lateral compartment in 44% of the cases, 29% had grade 1, 20% had grade 2, 7% had grade 3, and no subjects had grade 4. Only 15% reported pain specific to the lateral compartment (Fig. 1). In the patellofemoral compartment, 21% had no evidence of OA, 34% had grade 1, 34% had grade 2, 9% had grade 3, and 2% had grade 4. Only 12% of subjects reported pain specific to the patella-femoral compartment (Fig. 2).
Table 1.
Kellgren-Lawrence classification non-operative compartments.
| Kellgren-Lawrence Classification System | Lateral Compartment | Patellofemoral | |
|---|---|---|---|
| 0 | No radiographic features of OA | 44% (n = 35) | 21% (n = 17) |
| 1 | Possible joint space narrowing and osteophyte formation | 29% (n = 23) | 34% (n = 27) |
| 2 | Definite osteophyte formation with possible joint space narrowing | 20% (n = 16) | 34% (n = 27) |
| 3 | Multiple osteophytes, definite joint space narrowing, sclerosis and possible bony deformity | 7% (n = 6) | 9% (n = 7) |
| 4 | Large osteophytes, marked joint space narrowing, severe sclerosis and definite bony deformity | 0% (n = 0) | 2% (n = 2) |
Fig. 1.
Patient reported pain level in the lateral compartment of the knee.
Fig. 2.
Patient reported pain level in the patellofemoral compartment of the knee.
Charnley Functional Classification was assigned to each subject according to the definitions listed in the 2011 Knee Society Scoring System.12 At the last follow-up, 42% of subjects had a total knee or UKA performed on the contralateral knee and were classified as B2 and 20% classified as C2 had a medical condition other than their knee that affected ambulation (Table 2).
Table 2.
Charnley classification.
| Charnley Functional Classification at last follow-up | |
|---|---|
| Class | Subjects |
| A Unilateral Knee Arthritis | 26% (N = 21) |
| B1 Unilateral TKA opposite knee arthritic | 11% (N = 9) |
| B2 Bilateral TKA | 42% (N = 34) |
| C1 TKA, but remote arthritis affecting ambulation | 1% (N = 1) |
| C2 TKR, but medical condition affecting ambulation | 20% (N = 16) |
| C3 Unilateral or Bilateral TKA with Unilateral or Bilateral THA | 0% (N = 0) |
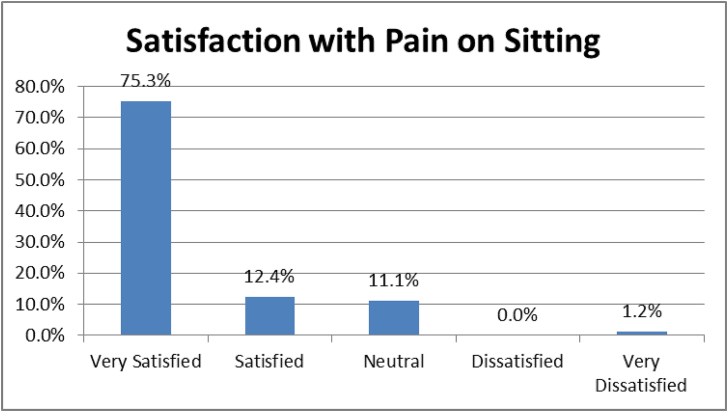
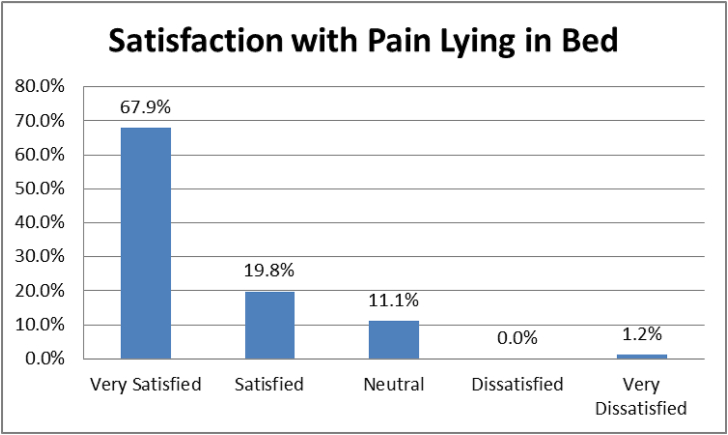
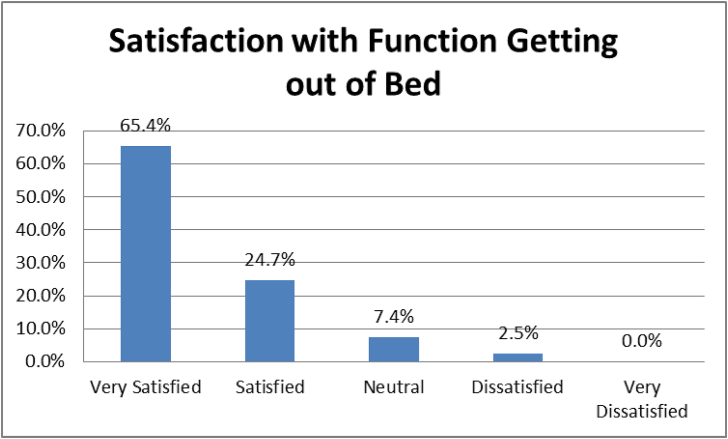
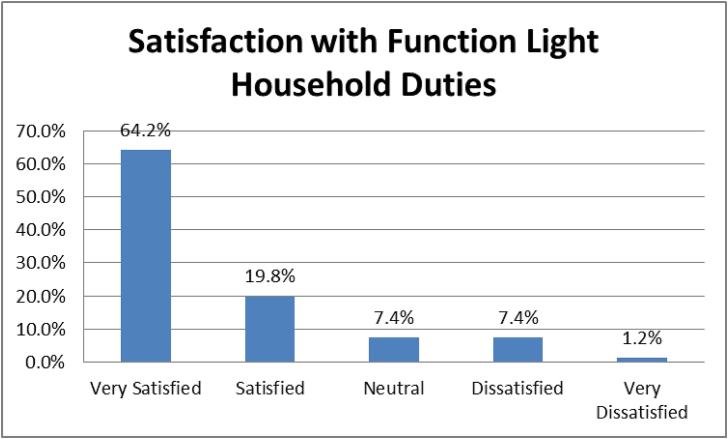
The post-operative 2011 Knee Society Score collected at last follow-up indicated good overall scores for all four components (Table 3). Unfortunately, we did not have preoperative scores for comparison. Patients were satisfied with their pain levels, activities of daily living, sports and leisure. The 2011 Knee Society Score patient satisfaction component revealed that 87.7% of the subjects were either very satisfied or satisfied with their pain level and 81.4% were either very satisfied or satisfied with their knee function while performing leisure recreational activities. Eighty-four percent were very satisfied or satisfied with their knee function while performing light household duties and 90.1% were very satisfied or satisfied with their knee function while getting out of bed (Fig. 3, Fig. 4, Fig. 5, Fig. 6, Fig. 7). Twenty-percent of the subjects with a Charnley Classification of C2 could explain the lower satisfaction scores with function performing recreational activities. Knee Society 2011 mean objective score completed by the surgeon was 96. The Knee Society 2011 function score was patient reported with a mean score of 81.
Table 3.
Mean 2011 knee society scores.
| Objective Knee Score Maximum Score 100 | Patient Satisfaction Maximum Score 40 | Patient Expectations Maximum Score 15 | Functional Knee Score Maximum Score 100 |
|---|---|---|---|
| 96.08 ± 5.03 | 34.81 ± 7.58 | 11.32 ± 3.05 | 80.72 ± 16.73 |
Fig. 3.
Patient satisfaction with knee pain while sitting.
Fig. 4.
Patient satisfaction with knee pain with lying in bed.
Fig. 5.
Patient satisfaction with knee function while getting out of bed.
Fig. 6.
Patient satisfaction with knee function while performing light household duties.
Fig. 7.
Patient satisfaction with knee function while performing leisure recreational activities.
The mean KOOS Score for pain was 90, for symptoms it was 88, activities of daily living score was 90, quality of life was 79, and sports and recreation was 71 (Table 4). The sports and recreation questions addressed kneeling, squatting, running, jumping, and pivoting on the affected knee. Only 26% had a Charnley category of A, meaning unilateral arthritis, leaving 74% with arthritis elsewhere, or having another replacement or condition affecting ambulation. This would account for the lower KOOS score for sports and recreation.
Table 4.
Mean KOOS Score (Maximum Score 100 for each category).
| KOOS Pain Score | KOOS Symptoms | KOOS Activities of Daily Living | KOOS Sports/Recreation | KOOS Quality of Life |
|---|---|---|---|---|
| 90.19 ± 15.25 | 87.83 ± 14.08 | 89.62 ± 14.22 | 70.78 ± 27.36 | 78.55 ± 21.24 |
The mean patient reported pain level while walking was 0.59 on a scale of 0–10. One subject with a history of DVT and PE reported a pain level of 8 at the four-year follow-up. An ultrasound performed that day was positive for DVT. Another subject with a history of Sjogren's syndrome reported their pain levels as a 5. On47e bilateral bicompartmental subject reported a pain level of 6 specific to lateral compartment in one knee only with certain movements and pain level of 2 on the other. Radiographic assessment of both lateral compartments revealed a Kellgren-Lawrence Classification of 3 on both knees. This subject had been quad strengthening with biking and running. Pain had not yet interfered enough for surgical intervention. The mean pain level for walking was 0.59 and 1.30 for stairs.
There was one UKA revised to a total knee at 40 months post-op resulting in a 1.2% revision rate for this series. This subject presented with persistent pain after a twisting injury. The last annual follow-up was at 36 months with a self reported pain level of 2 with level walking and a 3 with inclines and stairs. However, when asked by the physician, if there was pain specific to the lateral or patellofemoral compartments, the answer was no. This subject weighed 274 pounds at the time of UKA surgery and 255 pounds at time of revision. Radionuclide bone scan revealed nonspecific uptake within the medial knee adjacent to the prosthesis. At surgery, the implants did not appear to be loose and the intraoperative cultures were negative. Our revision rate is similar to, but with a longer mean follow-up than a larger series of robotic-assisted UKA by by Coon et al., reporting 1.2% at an average of 29.6 months.17, 18, 19 We reported a two-year minimum follow-up, but the mean was 54 months. The literature reports higher revision rates using a manual technique for performing UKA. The mean follow-up was slightly longer in most of the manual technique studies. Vorlat (2006) reported 16 revisions (10.7%) in 149 cases with a mean follow-up of 67 months in a mobile bearing UKA.20 Pandit et al. (2011) reported a 2.9% implant related re-operation rate using manual technique for mobile bearing implants at a mean follow-up of 67 months.21 Lim (2012) reported 3.5% revision rate at a mean follow-up of 62 month.22 Hamilton (2014) reported fixed-bearing revision rate of 2.9% within 2 years and 6% within 6 years.23 The low revision rate for our series supports our decision to use robotic-arm assisted UKA and also supports the method we used in selecting candidates. A method more similar to the current consensus statement than the literature at the time of surgery.15,16
Pearson's and Spearman's correlation coefficient between the ASA and the Knee Society expectations score, gender and the Knee Society function score, and the length of stay, with the KOOS scores was significant, (P < 0.05), but the correlations were weak. There was also a weak correlation between the lateral compartment Kellgren-Lawrence Classification and length of follow-up that was not significant.
Three subjects (one bilateral) who were included in the results of the total cohort had simultaneous patellofemoral arthroplasty. The mean age of 49 years was less than the mean for the total cohort which was 62. BMI was similar. Mean follow-up was 52 months. The mean patient reported pain levels were 0.75 for walking and 3.75 for stairs. They were satisfied with their function while sitting, lying and performing household duties, but dissatisfied with function during sports and recreational activities. All four knees felt “normal” at least some of the time.
4. Conclusions
Revision rates in a community hospital setting compare with earlier multi-center studies of UKA using robotic-arm assist.17, 18, 19 This series of patients reported a high level of satisfaction with their pain level, KOOS and 2011 Knee Society Scores. All outcome scores indicated that patients were doing very well with the exception of sports and recreation. This category had the lowest percentage of patients that were satisfied. Our UKA patients are counseled to only perform low-impact activities. For subjects that were previously runners or performed other high-impact sports, this limitation on activity could certainly have a negative effect on their satisfaction level. We had positive results from the most important question, “Does your knee feel normal?” This question is most important since it reflects the subjects overall sense of how their knee feels. With 81 subjects, only 3.7% (3) reported that their knee never felt “Normal” (Fig. 8).
Fig. 8.
Does this knee feel normal? Patient responses.
There were limitations to this study. One of them was the number of participants. Only 54% of the possible participants presented for follow-up and consented to participate. Patients were consented and enrolled at the time of routine annual follow–up and therefore we could not enroll any patients that did not show up and did not reschedule their appointment. Forty-six percent were of working age 65 and under which we agree contributed to poor follow-up compliance. Close proximity to military base may explain the high number lost to follow-up as this population tends to move frequently making it difficult to keep up with contact information. We were the first facility in the region to offer this technique and many patients came from out-of-state, hence making it difficult for them to return to clinic. Unfortunately, we did not have a consecutive series and therefore introduced selection bias. There were no outcome scores collected or consistency in the documented pain or function levels preoperatively therefore, we had no baseline for comparison to the follow-up scores.
Funding
This work was supported by Stryker Corporation.
Acknowledgements
We would like to acknowledge the Statistical Consulting Center, UGA System, Inc. 101 Cedar Street, Athens, GA, 30602 USA for their contribution and The American Joint Replacement Registry, 9400 W Higgins Rd #210, Rosemont, IL 60018 USA for their support with instrument scoring.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jor.2018.08.018.
Contributor Information
J. Melvin Deese, Email: mdeese@me.com.
Gwen Gratto-Cox, Email: ggratto@sghs.org.
Denny A. Carter, Email: dcarter@sghs.org.
Thomas M. Sasser, Jr., Email: tsasser@sghs.org.
Karah L. Brown, Email: kbrown4@sghs.org.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Dunbar N.J., Roche M.W., Park B.H. Accuracy of dynamic tactile-guided unicompartmental knee arthroplasty. J Arthroplasty. 2012;27(e1):803–808. doi: 10.1016/j.arth.2011.09.021. [DOI] [PubMed] [Google Scholar]
- 2.Jacofsky D.J., Allen M. Robotics in arthroplasty: a comprehensive review. J Arthroplasty. October 2016;31(Issue 10):2353–2363. doi: 10.1016/j.arth.2016.05.026. [DOI] [PubMed] [Google Scholar]
- 3.Citak M., Suero E.M., Citak M. Unicompartmental knee arthroplasty: is robotic technology more accurate than conventional technique? Knee. 2013;20:268–271. doi: 10.1016/j.knee.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 4.Lonner J.H., John T.K., Conditt M.A. Robotic arm-assisted UKA improves tibial component alignment: a pilot study. Clin Orthop Relat Res. 2010;468:141–146. doi: 10.1007/s11999-009-0977-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mofidi A., Plate J., Jinnah R. Assessment of accuracy of robotically assisted unicompartmental arthroplasty. Knee Surg Sports Traumatol Arthrosc. August 2014;22(8):1918–1925. doi: 10.1007/s00167-014-2969-6. [serial online] [DOI] [PubMed] [Google Scholar]
- 6.Pearle A.D., O'Loughlin P.F., Kendoff D.O. Robot-assisted unicompartmental knee arthroplasty. J Arthroplasty. 2010;25:230–237. doi: 10.1016/j.arth.2008.09.024. [DOI] [PubMed] [Google Scholar]
- 7.Plate J.F., Mofidi A., Mannava S. Achieving accurate ligament balancing using robotic-assisted unicompartmental knee arthroplasty. Adv Orthop. 2013;2013 doi: 10.1155/2013/837167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roche M. Robotic-assisted unicompartmental knee arthroplasty: the MAKO experience. Orthop Clin N Am. 2015;46:125–131. doi: 10.1016/j.ocl.2014.09.008. [DOI] [PubMed] [Google Scholar]
- 9.Bell, SW, Anthony I, Jones B, et al Improved Accuracy of Component Positioning with Robotic-assisted Unicompartmental Knee Arthroplasty. [DOI] [PubMed]
- 10.van der List J.P., Chawla H., Joskowicz L. Current state of computer navigation and robotics in unicompartmental and total knee arthroplasty: a systematic review with meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2016 doi: 10.1007/s00167-016-4305-9. DOI: 10.1007/s00167-016-4305-9. [DOI] [PubMed] [Google Scholar]
- 11.Collins N.J., Misra D., Felson D.T., Crossley K.M., Roos E.M. Measures of knee function: international knee documentation committee (IKDC) subjective knee evaluation form, knee injury and osteoarthritis outcome score (KOOS), knee injury and osteoarthritis outcome score physical function short form (KOOS-PS), knee outcome survey activities of daily living scale (KOS-ADL), lysholm knee scoring scale, Oxford knee score (OKS), Western Ontario and McMaster. Arthritis Care Res. 2011;63(supplement 11):S208–S228. doi: 10.1002/acr.20632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Noble P.C., Scuderi G.R., Brekke A.C. Development of a new knee society scoring system. Clin Orthop Relat Res. 2012;470(1):20–32. doi: 10.1007/s11999-011-2152-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kellgren J.H., Lawrence J.S. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 2000;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pandit H., Jenkins C., Gill H.S. Unnecessary contraindications for mobile-bearing Unicompartmental replacement. J Bone Joint Surg Br. 2011;93(5):622–628. doi: 10.1302/0301-620X.93B5.26214. [DOI] [PubMed] [Google Scholar]
- 15.Kozinn S.C., Scott R.D. Unicondylar knee arthroplasty: current concepts review. J Bone Joint Surg Am. 1989;71:145–150. [PubMed] [Google Scholar]
- 16.Berend K.R., Berend M.E., Dalury D.F., Argenson J.N., Dodd C.A., Scott R.D. Consensus statement on indications and contraindications for medial unicompartmental knee arthroplasty. J Surg Orthop Adv. 2015 Winter;24(4):252–256. [PubMed] [Google Scholar]
- 17.Coon T., Roche M., Pearle A., Dounchis J., Borus T., Buechel F., Jr. ISTA 27th Annual Congress, Sept. 24-27. 2014. Short to mid term survivorship of robotically assisted UKA: a multicenter study. (Kyoto, Japan) [Google Scholar]
- 18.Coon T., Roche M., Pearle A., Dounchis J., Borus T., Buechel F., Jr. ISTA 26th Annual Congress, Oct. 16-19. 2013. Short to mid term survivorship of robotically assisted UKA: a multicenter study. (Palm Beach, FL) [Google Scholar]
- 19.Pearle A.D., van der list J.P., Lee L., Coon T.M., Borus T.A., Roche M.W. Survivorship and patient satisfaction of robotic-assisted medial unicompartmental knee arthroplasty at a minimum two-year follow-up. Knee. 2017;24(Issue 2):419–428. doi: 10.1016/j.knee.2016.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vorlat P., Putzeys G., Cottenie D. The Oxford unicompartmental knee prosthesis: an independent 10-year survival analysis. Knee Surg Sports Traumatol Arthrosc. 2006;14:40–45. doi: 10.1007/s00167-005-0621-1. [DOI] [PubMed] [Google Scholar]
- 21.Pandit H., Jenkins C., Gill H.S., Barker K., Dodd C.A., Murray D.W. Minimally invasive Oxford phase 3 unicompartmental knee replacement: results of 1000 cases. J Bone Joint Surg Br. 2011;93:198–204. doi: 10.1302/0301-620X.93B2.25767. [DOI] [PubMed] [Google Scholar]
- 22.Lim H.C., Bae J.H., Song S.H., Kim S.J. Oxford phase 3 unicompartmental knee replacement in Korean patients. J Bone Joint Surg Br. 2012;94:1071–1076. doi: 10.1302/0301-620X.94B8.29372. [DOI] [PubMed] [Google Scholar]
- 23.Hamilton W.G., Ammeen D.J., Hopper R.H. Mid-term survivorship of minimally invasive unicompartmental arthroplasty with a fixed-bearing implant: revision rate and mechanisms of failure. J Arthroplasty. 2014;29:989–992. doi: 10.1016/j.arth.2013.10.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.