Highlights
-
•
All documented blunt cerebrovascular artery transections have demonstrated a one hundred percent mortality rate to date.
-
•
These injuries occur in patients with coexisting injuries, limiting the ability to attribute a given neurologic outcome to any one injury.
-
•
These injuries must be distinguished from the better-studied blunt carotid artery injuries, as each responds to treatment differently.
Keywords: Vertebral artery injury, Vertebral artery dissection, BCVI, Carotid artery injury, Multiple trauma, Case report
Abstract
Introduction
Blunt vertebral artery injury (BVI) is a potentially catastrophic event associated with a variety of trauma mechanisms, particularly in the setting of cervical spine injury. Early detection and treatment of BVI and blunt carotid artery injury (BCI) – collectively termed blunt cerebrovascular injuries (BCVI) – is a known determinant of favorable outcomes, except in the case of complete transection injuries. The limited existing reports of these injuries demonstrate a 100% mortality rate regardless of the management approach taken, and further investigation is essential in better understanding the nature of the injury and improving patient outcomes.
Presentation of case
A 55 year old previously healthy patient was brought to the Emergency Department following a motor vehicle collision. The patient was alert upon arrival to the ED and complained of neck pain. Initial assessment was significant for open fracture of the left upper extremity, swelling of the anterior neck, and no purposeful movements noted of the lower extremities. Shortly thereafter, the patient showed a sudden decline in mental status and became hemodynamically unstable. Focused Assessment with Sonography for Trauma was positive, and after remaining unstable despite resuscitation efforts, the patient was brought emergently to the operating room.
Discussion
Following exploratory laparotomy for bleeding control and washout of the open fracture, CT angiogram of the head and neck was obtained. This revealed significant C5–C6 dissociation as well as bilateral vertebral artery transection and large prevertebral hematoma. Prior to any further surgical intervention, the patient’s neurologic function continued to decline, and brain CT demonstrated infarcts in the posterior cerebral artery distribution. Brain death was confirmed the next day, and all care was subsequently withdrawn.
Conclusions
Analysis of outcomes in patients with BCVI suggests that BVI should be distinguished from the better-studied CVI. Each injury type has been found to possess its own distinct risk factors, likelihoods of progression, and surgical accessibility, all of which affect management. Data on complete vessel transections remains limited for all BCVIs, with no documented cases of bilateral BVI to date. Our case study supports the 100% mortality rate seen in previously reported BCVI transections. Furthermore, our findings suggest that BVI transections occur in patients with coexisting injuries, which challenges the ability to attribute a single neurologic outcome to any one injury.
1. Introduction
Blunt vertebral artery injury (BVI) is a potentially catastrophic event associated with a variety of trauma mechanisms, particularly in the setting of cervical spine injury. With the implementation of more aggressive screening guidelines, the incidence of BVI appears to be higher than previously thought. Early detection and treatment of BVI is a known determinant of favorable outcomes [1], except in the case of complete transection injuries. Though reports are limited, these injuries have demonstrated a 100% mortality rate regardless of the management approach taken [2], and alternative approaches must be explored. We present a case of bilateral vertebral artery transection and its extensive neurologic sequelae seen in a patient at our institution.
This work has been reported in line with the SCARE criteria [3].
2. Presentation of case
A 55 year old previously healthy patient was brought to the Emergency Department following a motor vehicle collision. The patient was a restrained driver traveling 50 miles per hour when she was struck on the driver’s side by another high-speed vehicle. The patient was trapped inside her vehicle and was extracted upon paramedic arrival to the scene. The patient was alert upon arrival to the ED and complained of neck pain. There was an obvious open fracture of the left upper extremity and swelling of the anterior neck. No purposeful movements were noted of the lower extremities. After initial assessment, the patient showed a sudden decline in mental status and was intubated for airway protection.
The patient was transferred to the nearest trauma facility, and was hemodynamically unstable upon arrival despite aggressive fluid resuscitation. Focused Assessment with Sonography for Trauma was positive in the right upper quadrant, warranting emergent exploratory laparotomy for control of blood loss. Intraoperative findings included a grade one liver laceration, grade one splenic laceration, and small mesenteric hematomas at the distal ileum and proximal transverse mesocolon. Approximately 400 ml of blood was evacuated from the peritoneal cavity. Systolic blood pressure was maintained in the 100 s, which was monitored throughout the operation by arterial line. On post-operative reassessment, pupils were unequal but reactive bilaterally; Eyes opened to stimulation but no movements of the extremities were observed. CT angiogram of the head and neck revealed significant C5–C6 dissociation as well as bilateral vertebral artery injury and large prevertebral hematoma (Fig. 1).
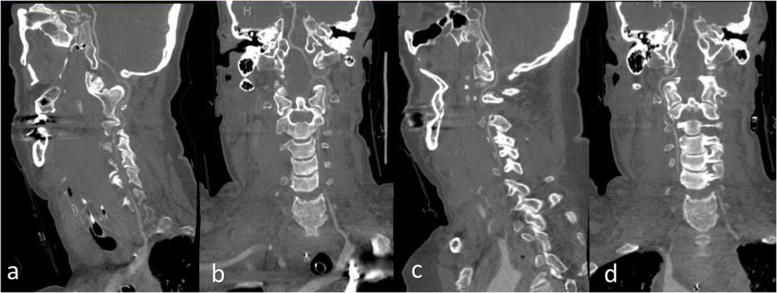
Fig. 1.
CTA cervical spine. Sagittal (a) and Coronal (b) views of right vertebral artery demonstrating lack of visualization of mid-cervical segment at C4–C5 levels. Sagittal (c) and Coronal (d) views of left vertebral artery demonstrating lack of visualization beyond the origin, as well as at C2–C4 and a small segment at C1–C2 level. Prominent vasospasm versus dissection. Fracture dislocation with distraction at C5–C6.
Neurosurgery placed patient in a Halo tongue. Fluoroscopy revealed a very unstable cervical spine, but given the extent of vascular injuries, surgical stabilization was deemed inappropriate at this time. MRI and CT of cervical spine re-demonstrated complete dissociation at C5–C6 with bilateral vertebral artery transections and large prevertebral hematoma, as well as spinal cord contusion extending from C2–C7, with significant stenosis (Fig. 2). Head MRI and CT revealed infarcts in the posterior circulation distribution. Given the complexity of findings, neurosurgery recommended transfer to a tertiary care hospital for stabilization. The patient’s neurologic function showed no signs of improvement. Cerebral perfusion scan confirmed brain death, at which time all care was withdrawn and the patient expired.
Fig. 2.
CT cervical spine without contrast, sagittal (a) and coronal (b) views. Avulsion fracture off the anterior, inferior endplate of C5 with disc space widening, consistent with anterior longitudinal ligament injury. Significant retropharyngeal soft tissue swelling.
3. Discussion
In light of recent literature suggesting an increasing prevalence of BVI, the best modalities of screening and treatment for these injuries is of ongoing debate. Despite continued efforts to identify risk factors and early signs of BVI, the vast array of presentations seen in these patients poses a challenge in formulating diagnostic and treatment guidelines.
Blunt vertebral and carotid artery injuries (BCI), collectively termed blunt cerebrovascular injuries (BCVI), can be classified using a grading system based on angiographic appearance [4]. Developed by Biffl et al., this grading scale (Table 1) was initially formulated on the supposition that different vessel injury types had distinct responses to therapy, patterns which ultimately could help standardize management. However, while BCI demonstrated a linear relationship between injury grade and stroke risk (with higher injury grades associated with higher incidence of stroke), this relationship was not observed in BVI [5]. Furthermore, Biffl et al. saw no difference in mortality among grades I-IV BCVI, while reporting a 100% mortality rate for carotid artery transections (grade V). No vertebral artery transections were reported in this 2001 study, which is likely attributable to the difficulty in identifying the injury in patients prior to its rapidly fatal consequences (Table 2).
Table 1.
Biffl scale for blunt cerebrovascular injury.
| Injury grade | Description |
|---|---|
| 1 | Luminal irregularity or dissection with <25% luminal narrowing |
| 2 | Dissection of intramural hematoma with >25% luminal narrowing, intraluminal |
| 3 | Pseudoaneurysm |
| 4 | Occlusion |
| 5 | Transection with free extravasation, hemodynamically significant arteriovenous fistulae |
Table 2.
BCI, blunt carotid artery injury; BVI, blunt vertebral artery injury.
| BCI |
BVI |
|||
|---|---|---|---|---|
| Worst injury grade | Total | Stroke | Total | Stroke |
| I | 50 | 4 (8%) | 33 | 2 (6%) |
| II | 14 | 2 (14%) | 13 | 5 (38%) |
| III | 35 | 9 (26%) | 15 | 4 (27%) |
| IV | 8 | 4 (50%) | 18 | 5 (28%) |
| V | 7 | 7 (100%) | – | – |
Since that time, there still are no BCVI studies which include patients with grade V BVI injuries, as was sustained in our patient. Maloney et al. [4] published a series of four blunt vertebral artery transection cases, all of which had fatal outcomes. The patients in these cases each developed signs of neurologic damage similar to that seen in our patient, however none survived long enough for specific assessment of cerebral ischemia. They concluded that the morbidity and mortality seen across all BCVI transections is not solely attributable to the vessel injury itself, but also to the severe coexisting and distraction injuries. In another recent case of fatal BVI transection with associated intraspinal hematoma, Shiban and Meyer discussed the dilemma faced in managing these injuries among patients with additional life-threatening injuries [6]. Ultimately, they concluded that their ideal management approach would entail immediate endovascular treatment followed by limited surgery addressing cervical instability, prior to spinal decompression surgery or any other repair.
Consistent with findings from previous reports, our case of vertebral artery transection maintains a 100% mortality rate of grade V BCVI. We partially attribute this prognosis to the many confounding variables involved in such traumas. Our particular case involved bilateral BVI, which has been documented in up to one fourth of all BVI cases. While unilateral injuries have the potential to remain asymptomatic due to extensive recruitment of collateral blood supply, bilateral BVI have demonstrated greater neurologic sequelae. There is however no data suggesting how this impacts management.
While the grading system developed by Biffl et al. has in fact guided treatment recommendations, there are no level I studies comparing treatment approaches in BCVI, thus management remains controversial [7]. Unless surgically accessible, the accepted standard of treatment in BCVI grades I–IV is systemic antithrombotic therapy, which has reduced the incidence of neurologic complications in retrospective studies [8,9]. Not surprisingly, however, as many as one third of patients are not candidates for this therapy due to traumatic brain injury, hemorrhage, or solid organ injury as was encountered in our patient. Endovascular therapy including stenting and embolization are accepted alternatives, with open surgery reserved as last resort. Vertebral artery transection is in fact the only definitive indication for open surgery, though the associated mortality risk remains extremely high [10].
4. Conclusion
The recent improvements in BVI detection and treatment has improved patient outcomes in certain injury types. Analysis of these trends suggests that BVI should be distinguished from the better-studied CVI; Each injury type possesses its own distinct risk factors, likelihoods of progression, and surgical accessibility, all of which affect management. Data on complete vessel transections remains limited for all BCVIs, with our case study supporting the 100% mortality rate seen in previously reported grade V BCVI. Furthermore, our findings suggest that BVI transections occur in patients with coexisting injuries, challenging the ability to attribute a single neurologic outcome to any one injury.
Conflict of interest
There are no conflicts of interest.
Funding
There are no funding sources for this paper.
Ethical approval
The study is exempt from ethical approval at our institution.
Consent
Verbal informed consent was obtained from the patient’s next of kin for publication of this case report and accompanying images. All items on our institution’s consent form were read and explained to the next of kin, and verbal consent was obtained. Extensive efforts were made to obtain written consent from the patient’s next of kin, however due to the next of kin’s distant location and physical limitations, written consent was not obtainable. A copy of the form containing the information read to the next of kin is available for review by the Editor-in-Chief of this journal on request.
The head of our medical team takes responsibility that exhaustive attempts have been made to contact the family and that the paper has been sufficiently anonymised not to cause harm to the patient or their family. The document stating these terms has been included in this submission.
Author contributions
Theresa Elder performed data collection and analysis and wrote this paper. Faiz Tuma was heavily involved in decision-making regarding the care of this patient, operated on the patient, and reviewed this paper.
Registration of research studies
No research involving human participants was conducted in this case report.
Guarantor
Theresa Elder.
References
- 1.Parks N. Use of computed tomography in the emergency room to evaluate blunt cerebrovascular injury. Adv. Surg. 2012;46(1):205–217. doi: 10.1016/j.yasu.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 2.Maloney E. Vertebral artery transection in nonpenetrating trauma: a series of 4 patients. Ann. Vasc. Surg. 2015;29(7):1450. doi: 10.1016/j.avsg.2015.03.061. e11-6. [DOI] [PubMed] [Google Scholar]
- 3.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., for the SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 4.Biffl W.L., Moore E.E., Offner P.J., Brega K.E., Franciose R.J., Burch J.M. Blunt carotid arterial injuries: implications of a new grading scale. J. Trauma. 1999;47(November (5)):845–853. doi: 10.1097/00005373-199911000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Biffl W.L., Moore E.E., Burch J.M. Blunt carotid and vertebral artery injuries. World J. Surg. 2001;25:1036. doi: 10.1007/s00268-001-0056-x. [DOI] [PubMed] [Google Scholar]
- 6.Shiban E., Meyer B. Traumatic vertebral artery rupture causing intraspinal hematoma and progressive neurologic symptoms. Acta Neurochir. 2018;160(2):249–251. doi: 10.1007/s00701-017-3407-6. [DOI] [PubMed] [Google Scholar]
- 7.Shafafy R., Suresh S., Afolayan J.O., Vaccaro A.R., Panchmatia J.R. Blunt vertebral vascular injury in trauma patients: ATLS® recommendations and review of current evidence. J. Spine Surg. 2017;3(2):217–225. doi: 10.21037/jss.2017.05.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stein D.M., Boswell S., Sliker C.W., Lui F.Y., Scalea T.M. Blunt cerebrovascular injuries: does treatment always matter? J. Trauma. 2009;66(1):132. doi: 10.1097/TA.0b013e318142d146. [DOI] [PubMed] [Google Scholar]
- 9.Acharya V., Chandrasekaran S., Nair S. An interesting case report of vertebral artery dissection following polytrauma. Int. J. Surg. Case Rep. 2016;28:196–199. doi: 10.1016/j.ijscr.2016.09.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.deSouza R.M., Crocker M.J., Haliasos N., Rennie A., Saxena A. Blunt traumatic vertebral artery injury: a clinical review. Eur. Spine J. 2011;20(9):1405–1416. doi: 10.1007/s00586-011-1862-y. [DOI] [PMC free article] [PubMed] [Google Scholar]