Highlights
-
•
Seroma is a common and challenging post-operative complication for both surgeons and patients.
-
•
Doxycycline can be a simple, safe and effective method for resolution of chronic seroma.
-
•
Negative Pressure Wound Therapy System can induce seroma cavity collapse and surface adherence.
Keywords: Seroma, Abdominal wall, Sclerosant, Sclerotherapy, Fluid collection
Abstract
Introduction
Seroma is a common and challenging post-operative complication that surgeons are often faced with after performing procedures in which tissue dead spaces have been created. The management strategies consist of non-operative management, percutaneous drainage, or surgical drainage. Our case report discusses the use of Doxycycline sclerotherapy in the successful resolution of a chronic abdominal wall seroma.
Presentation of case
We present the case of a 50 year old patient with extensive history of multiple abdominal surgeries, including appendectomy, multiple hernia repairs with recurrent mesh replacement as a result of infection followed by post-operative formation of seroma after each repair. Recently, patient underwent panniculecotomy complicated by seroma that was successfully resolved with the use of doxycycline sclerotherapy.
Discussion
Sclerotherapy has been used previously in the surgical field such as thoracic surgery, as a successful use of sclerosants in chronic pleural effusions has been documented. Sclerosants range from talc, tetracycline antibiotics, ethanol, polidocanol, erythromycin, OK-432, fibrin glue, and povidone-iodine, and are largely safe and easily applicable. Doxycycline in particular can be a simple and effective method for resolution of chronic seroma. This case demonstrates the successful use of doxycycline in the resolution of a chronic abdominal wall seroma.
Conclusion
Chronic and recurrent seroma after surgery can be difficult to deal with. Using sclerosants such as Doxycycline would be an effective solution to treat this chronic issue and to prevent its recurrence especially if it is used with a Negative Pressure Wound Therapy System.
1. Introduction
The vascular and lymphatic structures within subcutaneous tissue are at risk for disruption during surgery. This can lead to seroma formation and lymphedema. Seromas are typically self-resolving, but in some cases, they present an uncomfortable problem for physicians and patients [1].
Current treatment options include compression, percutaneous aspiration, and possible additional surgical interventions [1]. Accessing the sterile fluid within the cavity poses the risk for infecting the seroma resulting in an abscess. The use of sclerotherapy in the management of seromas has been reported in small scale studies and case reports, and has shown strong success with minimal complications [2]. Talc and Tetracycline antibiotic are alternative sclerosant agents used in the management of chronic seromas [2].
2. Presentation of case
This is a 50-year-old African American male with history of chronic type 2 DM, HTN and obesity. His previous surgeries included appendectomy in 2007, incisional hernia repair in 2009 followed by a subsequent repair between 2009–2014 due to a short interval hernia recurrence and infection of previously placed polypropylene mesh. Postoperative seroma development followed each repair and was treated with abdominal wall wash out. Patient also had multiple wound debridement and scar excision. The patient developed a chronic abdominal wall infection which persisted for several years. Excision of the abdominal wall infection and associated draining tracts required resection of the involved pannus. His previous hernia repair was an overlay repair with Strattice biological “mesh”. It was neither evident nor removed since it would have already fully integrated into his underlying fascia. A preoperative MRI revealed no Strattice remnants. He has never had a repair with synthetic mesh. Recently in September 2017, patient underwent panniculectomy and was placed on Ceftriaxone. Due to the large defect in a grossly contaminated field, the wound, including skin and subcutaneous space was left open (Fig. 1).
Fig. 1.
Intraoperative image demonstrating area of panniculectomy. Cranial is on the left side of the image. Caudal is on the right side.
Delayed primary closure of the defect was undertaken five days later using an Abra® Surgical Skin Closure System (Ontario, Canada) for progressive reapproximation of the wound (Fig. 2).
Fig. 2.
Post-operative Day #5 demonstrating close re-approximation of the wound with ABRA® device.
Final closure of the skin was achieved approximately two weeks following this procedure using staples and nylon sutures. Bulky dressing was then placed over the skin staple line and an abdominal binder was then placed for further support and compression.
The first office visit for follow up was at week three post-op. The wound was found to have an approximately 4 cm area of dehiscence at the staple line with serous drainage from a large underlying seroma. The patient continued to drain approximately 800 ml per day of serosanguinous drainage. Patient denied hot spells, cold spells, fevers or chills. The patient admits to failure of receiving home IV antibiotics for the first 3 weeks post-op as a result of insurance issues. In addition, application of Santyl (collagenase topical ointment) to wound once a day was prescribed. However, 3 days later, the patient presented to the ER for abdominal wound opening and incisional tenderness. Patient stated that abdominal pads were saturated twice a day. He denied any fever, chills, nausea, vomiting, SOB, chest pain, burning at wound site.
On Physical exam, the wound was draining clear serous fluid. There was a 16.5 × 5 cm opening instead of the 4 × 1 cm he had in the office visit, with an estimation of 60% of the wound open. There was granulating tissue with yellow slough present. There was no surrounding erythema noted.
Basic blood work revealed WBC 10.3, hemoglobin 13.3 with normal electrolytes, renal and liver function tests. Because the seroma cavity was draining through a wound defect and was of sufficient size and surface area to produce such large volumes of serous drainage, neither the placement of surgical drains nor surgically re-opening of an almost closed incision was considered appropriate initial approaches.
We decided to proceed with Doxycycline sclerotherapy using a Negative Pressure Wound Therapy System KCI-V.A.C.Ulta™. A low-volume, high-frequency sclerosant infusion technique was employed to contain the sclerosant within the cavity for a sufficient dwell time to be effective. A segment of White Foam placed through the open wound with approximately 3 cm protruding into the seroma cavity. This was covered with Granu Foam and a Veraflo dressing was applied.
Doxycycline, 20 mg/ml, was infused into the wound using the Veraflo therapy capability of the VAC Ulta. The device was programmed to instill into the wound 60 ml of doxycycline, 20 mg/ml every two hours and allowed to dwell for two hours. During which time, the patient was encouraged to ambulate and change positions frequently to facilitate distribution of Doxycycline. Following this, the VAC Ulta was cycled to the negative-pressure mode with aspiration of the remaining sclerosant. This cycle was repeated a total of six times. After completion of sclerosant infusion, the VAC remained in continuous negative-pressure mode to facilitate collapse of the cavity and surface adherence. An abdominal binder was then placed around the patient’s abdomen to reduce the seroma cavity. Dimensions and apposition of surfaces made adherent by the sclerosant (Fig. 3).
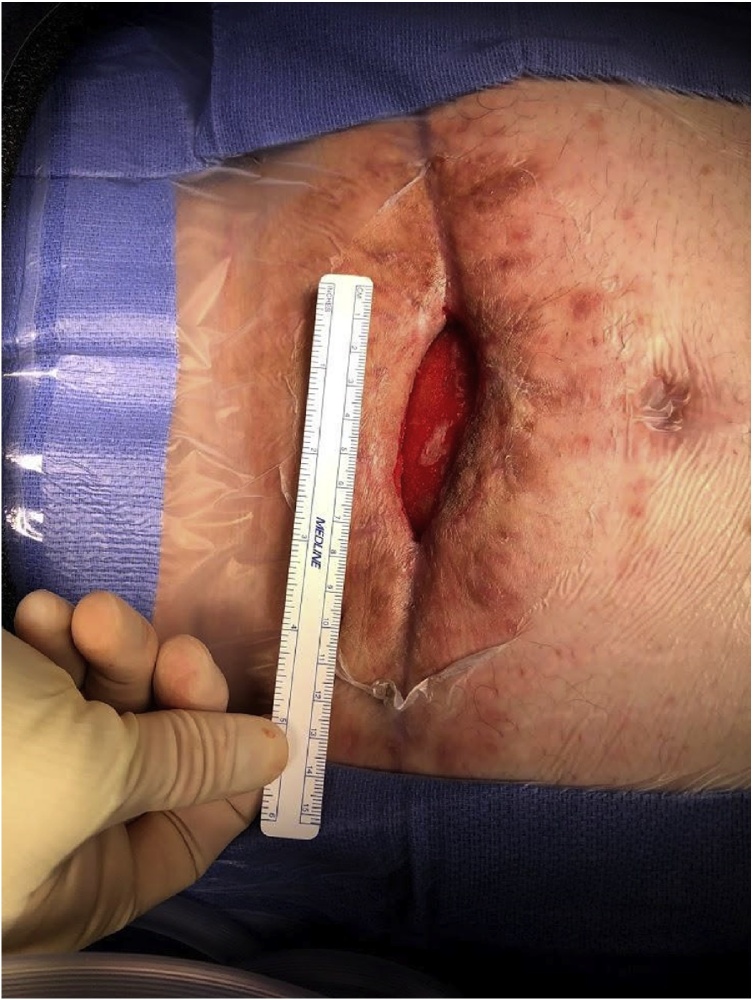
Fig. 3.
Day 4 post doxycycline wound VAC application. This image shows four retention sutures on both sides of open abdominal wound present; staples present on lateral edges of incision; open wound approximately 16.5 × 5 cm – beefy red with no purulent drainage; site of point tenderness proximal to open wound; bowel sounds present.
After 10 days of applying Doxycycline as a sclerosant, the seroma resolved completely, that allowed us for abdominal wall closure and application of Prevena wound vac®. One week later, the patient was discharged home with this wound vac. After 2 weeks of home discharge, the patient was seen at the hospital for wound debridement and JP drain implementation. Physical exam showed a 60% of wound healing and minimal to no serous drainage. The open wound had reduced dramatically from 16.5 cm × 5 cm in the ER visit to 7 cm × 1 cm (Fig. 4).
Fig. 4.
Shows wound size reduced dramatically from 16.5 cm × 5 cm to 7 cm × 1 cm in the office visit after one month of the ER visit.
The last office visit five months after the first Doxycycline sclerotherapy showed substantial wound healing (Fig. 5).
Fig. 5.
Substantial wound healing five months after the first Doxycycline sclerotherapy.
3. Discussion
The prevalence of post-operative seroma is particularly high after hernia repair, abdominoplasty, liposuction and Morel-Lavallée (closed soft-tissue de-gloving) lesions [1,[3], [4], [5]]. Incidence rates as high as 60% after mastectomy [6]. The disruption of lymphatic channels and blood vessels in each of these procedures is believed to play a central role in the accumulation of exudative fluid that results in seroma [2,6]. In particular, hernia repair with mesh placement can trigger a local inflammatory reaction that appears to play an additional role in seroma formation [7]. The accumulation of lymph, inflammatory and exudative fluids in surgically or traumatically created dead-space prevents the apposition and adhesion of tissue surfaces [2]. Over time, the cavities of these fluid collections will become lined by fibrous tissue without epithelium, and form pseudocysts [8].
Preventative measures include elimination of surgical dead-space through progressive tension sutures, closed suction drains, compression as well as the use of moderate electrocautery [3,4,6,9]. Expectant management which is the preferred initial treatment of seroma, is often sufficient as most seromas are asymptomatic and resolve within weeks [10]. Some seromas require further management. Fluid aspiration can be used but carries a risk of recurrence as well as a risk of infection. In particular, the use of aspiration in patients who have had hernia repair with mesh placement is risky as infection can be highly detrimental in the presence of mesh [7].
In one systematic review, Talc was found to promote resolution within 2 weeks for 10 of 13 patients, with most needing only one treatment [2]. Tetracycline antibiotics were used to achieve successful resolution in a similar amount of time, in all cases reviewed, with follow up application required in only a few lower extremity cases [2]. Similar rates of resolution and typical use of only one session were seen in case reports on Ethanol, polidocanol, erythromycin, OK-432 and fibrin glue [2]. All sclerosing agents were found to have a low risk of complication including pain, tightness or discomfort of treated area, and infection [2]. The use of Percutaneous Transcatheter Ethanol Sclerotherapy (PTES) for postoperative pelvic lymphocele treatment showed a 94% success rate with an average of 11.8 days (1–60 days) of catheter use. There was a mean of 25.8 months (2–64 months) of follow up time [11]. Sclerotherapy was cost-effective for improving quality of life for patients with Venous Malformations [12]. However, there are not enough literature about the cost effectiveness of sclerotherapy in treating seromas.
Doxycycline as a sclerosant has been used successfully in pleurodesis, lymphocele obliteration and pericardial effusion [5,13]. Its use has been proposed for the management of chronic seroma due to its low cost, relative safety, ease of use and accessibility [2]. Bansal et all presented a series of 16 patients with thigh, gluteal and trunk seromas who were treated with 500 mg of doxycycline wash and pressure dressings and saw resolution time of 4 weeks in thigh lesions, 8 weeks in anterior abdominal wall lesions, and 16 weeks in a patient who had difficulty with compliance [5].
In our case, the use of Doxycycline solution in a KCI Negative Pressure Wound Therapy System has shown a resolution of the chronic abdominal wall seroma within 10 days of implementing this sclerosant. The patient had this recurrent abdominal wall seroma for long time that different treatments other than the doxycycline sclerotherapy have been used without successful resolution of this seroma. The resolution of the seroma had helped the wound closure as it helped in reducing the open wound dramatically. The presence of this recurrent seroma would have impacted the closure of this wide open wound if left untreated. This work has been reported in line with the SCARE criteria [14].
4. Conclusion
Doxycycline sclerotherapy in the treatment of chronic abdominal wall seroma can be used as an effective and safe treatment. The use of a Negative Pressure Wound Therapy System KCI-V.A.C.Ulta™ can help induce collapse of the seroma cavity by removing the serous fluids as well as facilitating adherence of the cavity surface and making it sticky by using the sclerosant. This can be an initial treatment especially if the wound overlying the seroma has a small dehiscence and the seroma size is large or has a collapsed cavity and drains almost 800 cc per day.
Conflict of interest statement
None. This work has been reported in line with the SCARE criteria.
Source of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
Ethical approval is not required by our institution.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request”.
Author contribution
Fadi Al Daoud. MD. MPH: First author. Coordinated the design of this study, performed literature reviews, contributed in data collection from the preoperative, intraoperative and postoperative periods. Helped in writing the manuscript and provided proofreading of the report and gave its final form for submission.
Angelyn Thayer RN-BSN. MS3: Co-author. Did literature reviews and contributed in collection of data from the preoperative, intraoperative and postoperative periods. Helped in writing the manuscript.
Gul Sachwani Daswani. DO: Co-author. Provided feedback and proofreading for this case, and he approved it for submission.
Tareq Maraqa. MD: Co-Author. Assisted in the surgery and provided proofreading.
Vinu Perinjelil. MD: Co-Author. She Provided proofreading for this case.
Leo Mercer. MD: Co-author. Is the chief operating surgeon in this case. Provided feedback and proofreading for this case, and he approved it for submission.
All the authors had read and approved the final report.
Registration of research studies
This is a case report not a research or a study, so Registration of Research Studies is not required.
Guarantor
Dr. Leo Mercer.
Footnotes
The work took place in the trauma surgery research department at Hurley Medical Center, 1 Hurley plaza, 7 B trauma services, Flint, Michigan 48503, USA. Hurley Medical Center is a level 1 trauma center with 442 beds. It is affiliated with Michigan State University as a teaching and training hospital.
Contributor Information
Fadi Al Daoud, Email: FAldaou1@hurleymc.com.
Angelyn Thayer, Email: angelyn.thayer@msrj.chm.msu.edu.
Gul Sachwani Daswani, Email: GSachwa1@hurleymc.com.
Tareq Maraqa, Email: tmaraqa1@hurleymc.com.
Vinu Perinjelil, Email: VPerinj1@hurleymc.com.
Leo Mercer, Jr., Email: lmercer1@hurleymc.com.
References
- 1.Janis J.E., Khansa L., Khansa I. Strategies for postoperative seroma prevention: a systematic review. Plast. Reconstr. Surg. 2016;138:240–252. doi: 10.1097/PRS.0000000000002245. [DOI] [PubMed] [Google Scholar]
- 2.Sood A., Kotamarti V.S., Therattil P.J., Lee E.S. Sclerotherapy for the management of seromas: a systematic review. Eplasty. 2017;17:e25. [PMC free article] [PubMed] [Google Scholar]
- 3.Vidal P., Berner J.E., Will P.A. Managing complications in abdominoplasty: a literature review. Arch. Plast. Surg. 2017;44(5):457–468. doi: 10.5999/aps.2017.44.5.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rice D.C., Morris S.M., Sarr M.G., Farnell M.B., van Heerden J.A., Grant C.S., Rowland C.M., Ilstrup D.M., Donohue J.H. Intraoperative topical tetracycline sclerotherapy following mastectomy: a prospective, randomized trial. J. Surg. Oncol. 2000;73:224–227. doi: 10.1002/(sici)1096-9098(200004)73:4<224::aid-jso7>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 5.Bansal Abhishek, Bhatia Naval, Singh Archana, Singh Ashwani Kumar. Doxycycline sclerodesis as a treatment option for persistent Morel-Lavallée lesions. Injury. 2013;44(1):66–69. doi: 10.1016/j.injury.2011.11.024. ISSN 0020-1383. [DOI] [PubMed] [Google Scholar]
- 6.Woodworth Philip A., McBoyle Marilee F., Helmer Stephen D., Beamer R. Larry. Am. Surg. Atlanta. 2000;66(May (5)):444–450. discussion 450-1. [PubMed] [Google Scholar]
- 7.Vasilakis V., Cook K., Wilson D. Surgical resection and scarification for chronic seroma post-ventral hernia mesh repair. Am. J. Case Rep. 2014;15:526–529. doi: 10.12659/AJCR.891346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Throckmorton A.D., Askegard-Giesmann J., Hoskin T.L. Sclerotherapy for the treatment of postmastectomy seroma. Am. J. Surg. 2008;196:541–544. doi: 10.1016/j.amjsurg.2008.06.020. [DOI] [PubMed] [Google Scholar]
- 9.Agrawal A., Ayantunde A.A., Cheung K.L. Concepts of seroma formation and prevention in breast cancer surgery. ANZ J. Surg. 2006;76:1088–1095. doi: 10.1111/j.1445-2197.2006.03949.x. [DOI] [PubMed] [Google Scholar]
- 10.Lopez-Monclus J., Garcia-Ureña M.A., Blázquez L.A., Melero D.A., Jiménez-Ceinos C. Persistent inguinal seroma managed with sprinkling of talcum powder: a case report. J. Med. Case Rep. 2012;6(391) doi: 10.1186/1752-1947-6-391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Okan O., Karcaaltincaba M., Ozmen M.N., Akinci D., Karcaaltincaba D., Ayhan A. Percutaneous transcatheter ethanol sclerotherapy and catheter drainage of postoperative Pelvic Lymphoceles. Cardiovasc. Intervent. Radiol. 2007;30(2):237–240. doi: 10.1007/s00270-006-0180-y. April. [DOI] [PubMed] [Google Scholar]
- 12.Ono Y., Osuga K., Takura T., Nakamura M., Shibamoto K., Yamamoto A., Fujiwara H., Mimura H., Tomiyama N. Cost-effectiveness analysis of percutaneous sclerotherapy for venous malformations. J. Vasc. Interv. Radiol. 2016;(June) doi: 10.1016/j.jvir.2015.12.019. [DOI] [PubMed] [Google Scholar]
- 13.Caliendo Mark V., Lee David E., Queiroz Rodolfo, Waldman David L. Sclerotherapy with use of doxycycline after percutaneous drainage of postoperative lymphoceles. J. Vasc. Interv. Radiol. 2001;12(1):73–77. doi: 10.1016/s1051-0443(07)61407-9. ISSN 1051-0443. [DOI] [PubMed] [Google Scholar]
- 14.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., the S.C.A.R.E. Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]