Supplemental Digital Content is available in the text
Keywords: cauda equina syndrome, core outcome set, neurology, neurosurgery, orthopedics, outcome domains, outcomes, Prisma, spine surgery, surgery, systematic literature review
Abstract
Study Design.
This is a systematic literature review following the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines.
Objective.
To assess the outcomes reported in trials and observational studies of surgery for cauda equina syndrome (CES), and to inform the development of a core outcome set.
Summary of Background Data.
Scoping searches revealed that there were inconsistencies in which outcomes were reported and how they were measured in research studies for patients who had undergone surgery for CES.
Methods.
Ovid Medline, Embase, CINAHL Plus, and trial registries were searched from January 1, 1990 to September 30, 2016 with the term “cauda equina syndrome.” Inclusion and exclusion criteria were applied according to study design, diagnosis, procedure, publication date, language, and patient age. Data extracted included demographics, study design, the outcomes reported, and their definition. We also assessed variation in the use of terminology for each outcome domain.
Results.
A total of 1873 articles were identified, of which 61 met the inclusion criteria. Of these, 737 outcomes reported verbatim were categorized into 20 core outcome domains and 12 subdomains with a range of 1 to 141 outcomes per outcome domain or subdomain. The most commonly reported outcomes were bladder function (70.5%), motor function (63.9%), and sensation (50.8%). Significant variation in the terms used for each outcome was documented, for example, bladder function outcome domain had 141 different terms.
Conclusion.
There is significant heterogeneity in outcomes reported for studies after surgery for CES patients. This indicates a clear need for the development of a core outcome set, which has been registered as number 824 on the COMET (Core Outcome Measure in Effectiveness Trials) database.
Level of Evidence: 1
Cauda equina syndrome (CES) is mainly caused by compression of the lumbosacral nerve roots below the conus medullaris. Clinically, symptoms and signs include low-back pain, saddle anesthesia, unilateral or bilateral sciatica, and motor weakness of the lower extremities with bladder and bowel dysfunction.1,2 However, CES is a clinical-radiological diagnosis as clinical signs are not particularly sensitive to a CES diagnosis.3,4 A lumbo-sacral magnetic resonance imaging (MRI) is required for diagnosis. Gleave and McFarlane5 stressed the importance of categorizing CES into CES incomplete (CESI) and CES complete with urinary retention (CESR) (Figure 1). It is deemed a surgical emergency and there have been numerous publications and debates relating to the ideal timing for surgery.6–9 It can result in permanent damage to nerve roots resulting in long lasting or permanent disabling symptoms.2
Figure 1.
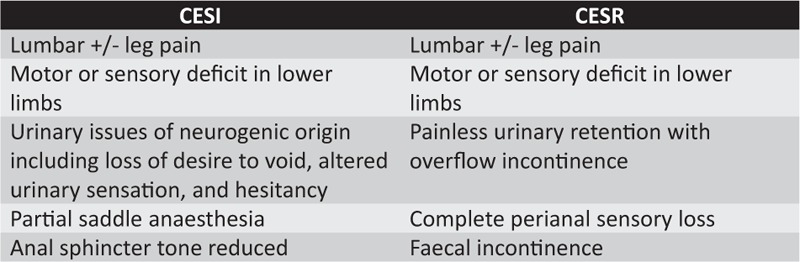
Symptoms relating to CESI and CESR.
There is no consultation with patients in the literature regarding importance of outcomes for CES. In addition, there is little known about the long-term outcomes, which was highlighted by Korse et al,10 who independently decided to focus on outcomes of micturition, defecation, and sexual function. Bias in studies, lack of universal definitions, and incomplete follow-up data were seen in this systematic review.
The problems with not having a core outcome set (COS) includes:
-
(i)
Patients are not included so important outcomes to them may not be measured. This has been witnessed in other healthcare areas such as childhood asthma and esophageal cancer.11–14
-
(ii)
Lack of a consistent approach makes individual studies difficult to interpret and put into context of other studies.
-
(iii)
Possibility for synthesizing evidence in a systematic review and meta-analysis are diminished 15.
-
(iv)
Waste and inefficiency. It is reported that 85% of research funding is wasted across the research cycle with key sources related to outcomes; important outcomes are not assessed, published research fails to set its position when compared with all previous similar research and 50% of planned study outcomes are not reported.16
At present, there is no COS for CES, which is to the detriment of patients and health services. The aim of this systematic literature review is to inform the future development of a COS by identifying all documented outcomes for patients after surgery in CES, identify if they are defined, and to assess what variability there is. The systematic literature review is the first step to inform the development of a COS14 for patients who have undergone surgery for CES to be used in research and in practice.
METHODS
This study has been registered as 824 on the COMET (Core Outcome Measures in Effectiveness Trials) website (http://www.comet-initiative.org/studies/details/824). Table 1 lists the inclusion criteria applied to the search strategy.
TABLE 1.
Inclusion Criteria for the Systematic Literature Review
| Diagnosis of CES |
| Patients have undergone surgery for the pathology causing CES |
| Randomized controlled trials, nonrandomized controlled trials, prospective and retrospective cohort studies, and case series |
| Human studies |
| English language |
| Five or more patients |
| Published between 1990 to September 30, 2016 |
| Adult patients aged 16 years and above |
CES indicates cauda equina syndrome.
Search Strategy
We searched Medline, Embase, and CINAHL Plus (Cumulative Index to Nursing and Allied Health Literature). The search strategy for each database is available in Appendix 1. Online trial registries included Clinical Trials.gov, EU clinical trials registry and the ISRCTN (International Standard Randomized Controlled Trials Number) registry. The trial registries were searched for any completed or ongoing trials in surgery for CES and no relevant studies were found. Only case reports and abstracts were excluded in the initial search term as we wanted studies with five or more patients. We only included studies published after January 1, 1990 to keep investigation (post-MRI era) and surgical management of CES in line with current medical practice. Citations were collated with Endnote X7 referencing program (Thomson Reuters, New York, NY) and duplicates removed.
Data Extraction
Titles and abstract were initially screened by NS to identify potential studies for inclusion, for which full text articles were obtained for further assessment. Approximately, 10% of included articles were randomly checked for suitability by clinical supervisors and any discussion regarding uncertainty of eligibility criteria applied to the search results was discussed with them (SC, MW, and TM). A data extraction form was used to collect data on study design and location, patient demographics, timing of operation, definition of CES, diagnosis, etiology, surgical procedure, follow-up duration, outcome terminology, outcome definition, and assessment tool.
Terminology
Below are the definitions for the main terms used in the analysis of this systematic literature review.
-
1.
Core outcome domain- The overall category to which similar subdomains and outcomes are listed under. The outcome domains that we have used in this article have been linked to the high level set of outcome categories used for annotation of Cochrane reviews17 (http://linkeddata.cochrane.org/linked-data-project/metadata-and-vocabularies/outcomes) and through discussion with the COMET initiative team. These are listed in bold in Table 3.
-
2.
Subdomain- A subcategory of a Core outcome domain to which similar outcomes are listed under. These are listed in normal script in Table 3.
-
3.
Outcome- An outcome documented in an article after a patient has had an operation for CES. For example, nervous system (core outcome domain)> bladder function (subdomain)> urinary incontinence (outcome).
-
4.
Variations- Variations were also documented, which means the number of different terms used to define a core outcome domain or subdomain. An example of a variation is given in the superscript of Table 4.
-
5.
Outcome definition- this was categorized as “no definition” or “definition present.” If a definition was present it could be subjectively a complete or partial definition but was recorded as “definition present.” “No definition” indicates the outcome domain was mentioned with no accompanying definition in the article or assessment tool. An example of how outcome definition was done is given in the superscript of Table 4.
TABLE 3.
Core Outcome Domains (in Bold) and Subdomains
| Mortality | Role Functioning |
| General Disorders | Social functioning |
| Nervous System Outcomes | Emotional functioning |
| Bladder Function | Global quality of life |
| Motor Function | Hospital use |
| Sensation | Need for intervention |
| General Neurology | Adverse events |
| Lower Back Pain | Infection |
| Leg Pain | Skin and subcutaneous tissue |
| Bowel Function | Vascular |
| Perianal sensation | Outcomes related to neoplasms |
| Perianal Tone | Urological and renal |
| Reflexes | Cardiac |
| Physical Functioning | Blood and lymphatic |
| Sexual Function | Respiratory |
| Walking | Gastrointestinal |
TABLE 4.
Raw Data for Each Outcome Showing How Many Studies Each Outcome is Reported in, the Total Number of Outcomes, the Variations for Each Outcome, if a Definition is Present in the Reported Studies and the Number of Assessment Tools for the Reported Outcomes. Outcomes are Listed in Order of Decreasing Frequency of Reported Studies
| Outcome Domain | Reported 61 Studies, N (%) | Total Number of Outcomes | Number of Variations | Definition Present in Reported Studies (%) | Assessment Tool in Reported Studies (%) |
| Bladder function (nervous system) | 43 (70.5) | 141 | 87* | 25 (58.1)† | 13 (30.2) |
| Motor function (nervous system) | 39 (63.9) | 62 | 36 | 9 (23.1) | 16 (41) |
| Sensation (nervous system) | 31 (50.8) | 53 | 26 | 6 (19.4) | 6 (19.4) |
| Bowel function (nervous system) | 28 (45.9) | 60 | 47 | 7 (25) | 8 (28.6) |
| Leg Pain (nervous system) | 27 (44.3) | 32 | 16 | 5 (18.5) | 7 (25.9) |
| Lower-back pain (nervous system) | 26 (42.6) | 31 | 13 | 4 (15.4) | 9 (34.6) |
| General neurology (nervous system) | 22 (36.1) | 31 | 21 | 3 (13.6) | 8 (36.4) |
| Skin and subcutaneous tissue | 19 (31.1) | 22 | 15 | 5 (26.3) | 0 (0) |
| general disorders | 19 (31.1) | 44 | 36 | 6 (31.6) | 6 (31.6) |
| mortality | 18 (29.5) | 25 | 13 | 6 (33.3) | 0 (0) |
| Perianal sensation (nervous system) | 17 (27.9) | 23 | 16 | 5 (29.4) | 0 (0) |
| Sexual function (physical functioning) | 16 (26.2) | 46 | 41 | 6 (37.5) | 6 (37.5) |
| Walking (physical functioning) | 16 (26.2) | 28 | 25 | 3 (18.8) | 5 (31.3) |
| Adverse events | 12 (19.7) | 16 | 12 | 8 (66.7) | 0 (0) |
| Role functioning | 11 (18) | 20 | 20 | 3 (27.3) | 7 (63.6) |
| Perianal tone (nervous system) | 11 (18) | 16 | 13 | 2 (18.2) | 0 (0) |
| Need for intervention | 10 (16.4) | 13 | 13 | 6 (60) | 0 (0) |
| Infection | 10 (16.4) | 11 | 8 | 1 (10) | 0 (0) |
| Vascular | 8 (13.1) | 13 | 5 | 0 (0) | 0 (0) |
| Hospital use | 5 (8.2) | 8 | 6 | 0 (0) | 0 (0) |
| Global quality of life | 5 (8.2) | 8 | 6 | 3 (60) | 4 (80) |
| Reflexes (nervous system) | 4 (6.6) | 7 | 7 | 0 (0) | 0 (0) |
| Emotional functioning | 4 (6.6) | 7 | 7 | 1 (25) | 3 (75) |
| Respiratory | 4 (6.6) | 4 | 5 | 0 (0) | 0 (0) |
| Outcomes relating to neoplasms | 3 (4.9) | 5 | 3 | 0 (0) | 0 (0) |
| Urological and renal | 3 (4.9) | 3 | 3 | 0 (0) | 0 (0) |
| Cardiac | 3 (4.9) | 3 | 2 | 0 (0) | 0 (0) |
| Social functioning | 2 (3.3) | 2 | 2 | 0 (0) | 2 (100) |
| Blood and lymphatic | 2 (3.3) | 2 | 2 | 0 (0) | 0 (0) |
| Gastrointestinal | 1 (1.6) | 1 | 1 | 0 (0) | 0 (0) |
*An example of analyzing the variation of terminology used for bladder function outcome domain: “urinary incontinence” “bladder dysfunction” and “urinary retention” are 3 variations of the way this outcome domain is described.
†Two examples of how bladder function outcome domain was classified with definition present: (i) retention of urine – “the inability to pass urine necessitating urinary catheterization.” This study was retrospective and relied upon adequate documentation in the patients’ clinical notes. Residual urine volumes were only available in 11 patients (all greater than 300 mm) whereas 24 patients were documented to be in urinary retention. Urinary retention at follow-up comprised those patients requiring catheterization to enable them to empty their bladder and also those patients who reported incomplete bladder emptying (McCarthy et al,49). (ii) Urine retention diagnosis was clinical (a bladder that required catheterization). (Foruria et al35)
RESULTS
A total of 1873 articles were identified by electronic database searches.
-
1.
Medline (650)
-
2.
Embase (949)
-
3.
CINAHL Plus (239)
-
4.
Registries (35) included Clinical Trials.gov (5), EU clinical trials registry (12) and ISRCTN (International Standard Randomized Controlled Trials Number) registry (18).
The Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) flowchart in Figure 2 shows the process during the systematic literature review. Following inclusion criteria in Table 1 resulted in 1838 articles plus the 35 studies from the online registry search giving a total of 1873 studies. Moreover, 10% of included studies were reviewed by a supervisor (MW and SC) to assess if inclusion criteria had been applied adequately and agreement was achieved after discussion amongst us. Uncertainty regarding eligibility of certain full text articles for inclusion were discussed with the clinical supervisory team (MW, SC, and TM) and settled leading to 61 included articles. Thirty-four articles were excluded after the full text was obtained and the reasons for this were given as in Figure 2.
Figure 2.
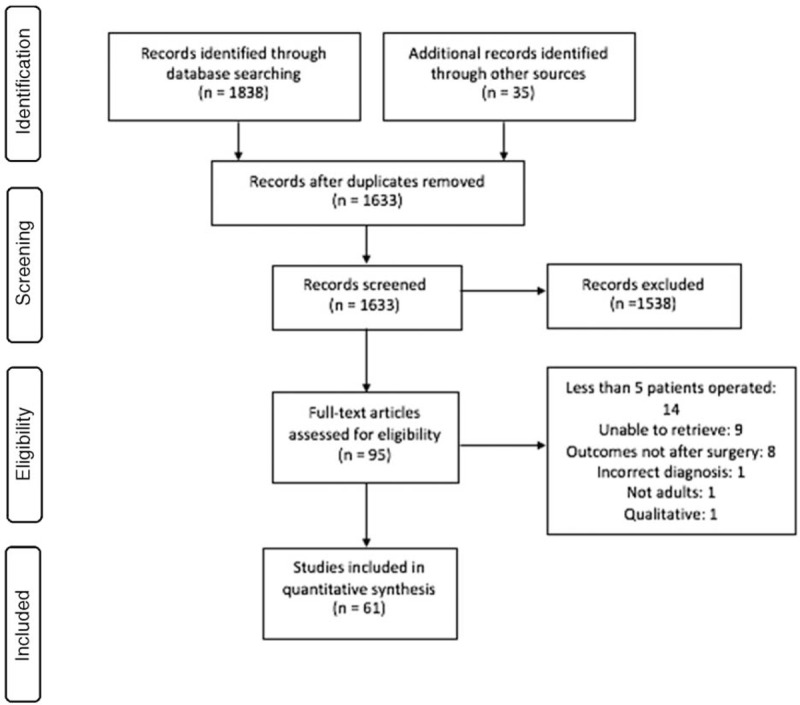
PRISMA flowchart for online databases.
Summary details, patient demographics, and how many studies they were reported in out of the 61 included studies are detailed in Table 2. Most studies (90.2%) were retrospective. CES was not defined in 20 studies (32.8%). Even in the articles where CES is defined there were many differing definitions. The most common definition was CESI and CESR as described in Figure 1.
TABLE 2.
Summary Characteristics and Demographics of Included Studies
| Characteristic (Number of Studies Reported) | Value |
| Study design (61) | |
| Retrospective cohort | 55 |
| Prospective cohort | 6 |
| Location (61) | |
| Europe | 32 |
| North America | 15 |
| South America | 1 |
| Asia | 13 |
| Single center | 57 |
| Year of publication (61) | |
| 1990–1995 | 5 |
| 1996–2000 | 4 |
| 2001–2005 | 10 |
| 2006–2010 | 16 |
| 2011–2016 | 26 |
| Mean follow-up period postsurgery (54) | 8.4 yrs |
| Range | 1–38 yrs |
| Median number of CES patients (61) | 14 |
| Range | 5 to 11,207 |
| Mean age (53) | 45.5 |
| Range | 20.5–70 |
| Median follow up (43) | 31 months |
| Range | postoperative–29 yrs |
| CES definition (61) | |
| Defined | 41 |
| Not defined | 20 |
| Diagnostic main investigation (54) | |
| MRI | 44 |
| CT | 9 |
| Myelogram | 1 |
| Etiology (59) | |
| Disc herniation | 34 |
| Degenerative | 4 |
| Postoperative complication | 3 |
| Trauma | 7 |
| Tumor | 6 |
| Other | 2 |
| Main surgical method (51) | |
| Laminectomy and discectomy | 15 |
| Laminectomy | 14 |
| Laminectomy and instrumentation | 12 |
| Microdiscectomy | 8 |
| Other | 2 |
CES indicates cauda equina syndrome; CT, computed tomography; MRI, magnetic resonance imaging.
A total of 737 outcomes were reported in the 61 included articles.9,18–78 For ease of analysis in this study, these reported outcomes have been categorized to one of the 20 core outcome domains (Table 3). The nervous system core outcome domain had 10 subdomains, and the physical functioning has two subdomains (Table 3). The number of different variations in the description of outcomes can be seen in Table 4 linked to the outcome domains.
Figure 3 shows the number of articles in which specific outcomes were reported. Bladder function, motor function, sensation, bowel function, leg pain, and lower-back pain were the most commonly reported in descending order. They are all within the nervous system core outcome domain. Moreover, for each outcome, the number of articles where it is defined and not defined is documented. Figure 3 also shows the number of articles where the reported outcome had an assessment tool or not.
Figure 3.
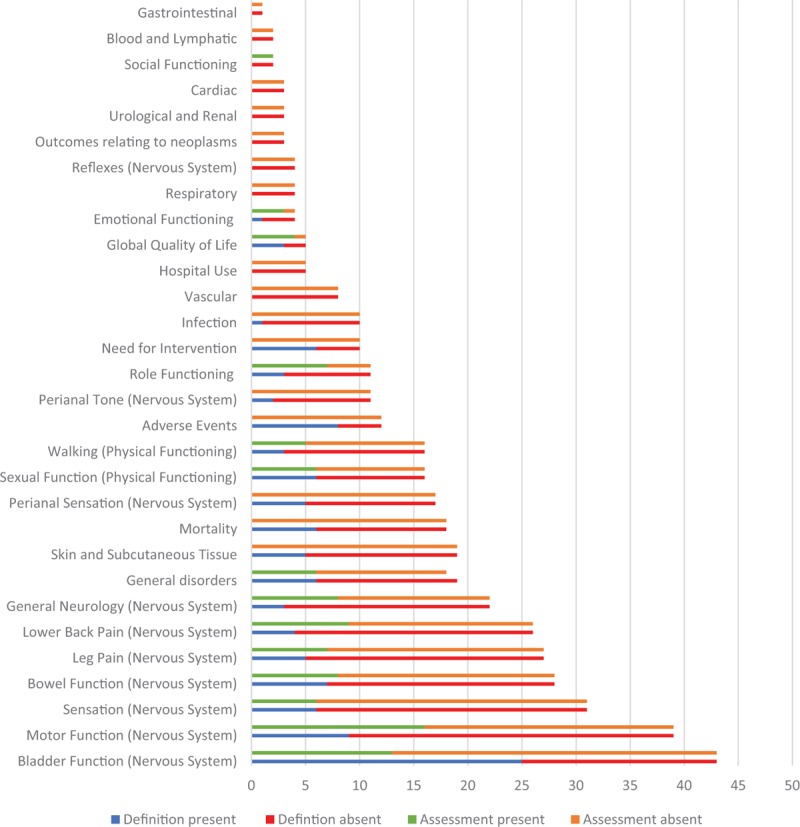
Stacked bar chart showing total number of articles where the outcome was reported and the proportion of those defined (blue) and those not defined (red). Moreover for each outcome the number of articles which have used an assessment tool for a reported outcome (green) and the number that have not (orange). Outcomes are listed from most to least reported.
Table 4 shows the raw data for each outcome showing how many studies each outcome is reported in, the total number of outcomes, the number of variations in the description of the outcome if a definition is present or not in the reported studies, and the number of assessment tools for the reported outcome. Table 5 shows the various assessment tools used for each outcome.
TABLE 5.
Assessment Tools are Listed in Alphabetical Order for the Corresponding Reported Outcomes
| Outcome Domain | Assessment Tools |
| Bladder function (nervous system) | 25-Item questionnaire36/ Bristol female lower urinary tract/ Cystometry/ Functional Independence Measurement/ Gibbon's criteria/ Gleave and McFarland, 1990/ Hannover pelvic scoring system/ International Continence Society male questionnaire/ Japanese Orthopedic Association score / Modified Odom's criteria/ Short-form Incontinence Questionnaire/ Urodynamics |
| Motor function (nervous system) | American Spinal Injury Association Score/ Frankel grading/ Gibbon's criteria / McCormick scale/ MRC grading/ Modified Odom's criteria |
| Sensation (nervous system) | American Spinal Injury Association Score/ Frankel grading/ Gibbon's criteria / McCormick scale/ Modified Odom's criteria/ Nanko evaluation system |
| Bowel function (nervous system) | 25-Item questionnaire36/ Chronic idiopathic constipation index / Fecal incontinence questionnaire (Jorge et al 1993)/ Functional Independence Measurement/ Hannover pelvic scoring system/ Modified Odom's criteria/ Nanko evaluation system/ Short-form Incontinence Questionnaire |
| Leg pain (nervous system) | Benoist et al 1993/ Japanese Orthopedic Association score/ Visual Assessment Score |
| Lower back pain (nervous system) | Low Back Outcome Score/ Oswestry Disability Index/ Short-form Health Survey 36/ Visual Assessment Score |
| General neurology (nervous system) | American Spinal Injury Association Score/ Baba et al, 1995 study questionnaire/ Frankel grading/ Gibbon's criteria/ Japanese Orthopedic Association score/ McCormick's scale |
| General disorders | Epstein & Hood/ Nanko evaluation system/ Prolo economic and functional scale/ Short Form Health Survey 36/ Spengler classification/ Visual Assessment Score |
| Sexual function (physical functioning) | International index of erectile function/ Male sexual health inventory/ McCormick scale/ Modified Odom's criteria/ Nogueira et al 1990/ Sheffield Female pelvic floor questionnaire/ Japanese Orthopedic Association score |
| Walking (physical functioning) | Baba et al 1995/ Functional Independence Measurement/ Japanese Orthopedic Association score/ McCormick scale/ Short-form Health Survey 36 |
| Role functioning | Chronic idiopathic constipation index/ Kirkaldy Willis classification/ Nanko evaluation system/ Oswestry Disability Index/ Prolo economic and functional scale/ Short-form Incontinence Questionnaire |
| Global quality of life | 25-Item questionnaire36/ Oswestry Disability Index/ Short Form Health Survey 36 |
| Emotional functioning | Functional Independence Measurement/ Kelleher et al 1997 questionnaire/ Short-form Health Survey 36 |
| Social functioning | Kelleher et al 1997 questionnaire/ Short-form Health Survey 36 |
DISCUSSION
This systematic review shows that there is significant heterogeneity in the outcomes measured for patients who have undergone surgery for CES with no consensus.
Most of the evidence regarding outcomes for CES patients after surgery is derived from level 4 evidence, namely, single centre retrospective cohort review studies. The average data collection period was over 8 years with a median number of 14 patients per study, which highlights the rare nature of the condition and difficulty in collecting meaningful data retrospectively. This feeling is also echoed by Todd and Dickson, 2016.79 Since 1990, the number of publications analyzing outcomes after an operation for CES have increased with the most being produced in the last 5-year period (43.5%). Median follow up was at 31 months reflecting the deficiency in the literature for any long-term outcomes.
The main investigation is MRI, which reflects the systematic literature review focusing on studies from 1990 onwards. Before this there may have been a reliance on myelography and CT to radiologically identify CES compression. The main etiology is disc herniation. There are no studies in the literature documenting the exact distribution of CES aetiology but the most common cause is believed to be because of disc herniation.
Poor definition of CES has been previously highlighted in a systematic review of the literature.80 Twenty studies (32.8%) did not define this and of the 41 studies where a definition was present, there was significant heterogeneity in the definitions. The most common definition for CES in this review was CESI and CESR.5 If a study fails to define CES then we are unsure of the condition to which the outcomes of the study belong to.
Most common surgical method in studies was a laminectomy and discectomy as seen in Table 2 but there were other studies that predominantly performed surgery via a microdiscectomy. Laminectomy alone, or with instrumentation was also mentioned for CES patients. In fact, now there is an increase in the popularity of endoscopic lumbar discectomy procedure 45 that adds to the range of procedures available when dealing with CES secondary to disc herniation. There is no consensus in the literature as to a specific decompressive procedure to be used for CES secondary to compressive pathology. This is also another factor that may affect outcomes for these patients.
In total, there were 737 outcomes reported verbatim and categorized into 20 core outcome domains and 12 subdomains. Instead of the same term being used for each outcome, there exists 507 variations in terminology (Table 4). In addition, most of the outcomes in the included articles have no definition. Except bladder function, adverse events, need for intervention, and global quality of life, all other outcomes had “no definition” in the majority of the included articles (Figure 3). This highlights that there is significant heterogeneity in not only the outcome terminology used but the level to which it is defined in the literature. Except global quality of life, emotional functioning, role functioning, and social functioning, most outcomes did not have an assessment tool in most of the articles (Figure 3). Fourteen of the outcome domains/subdomains we categorized had multiple different assessment tools used for each of them as seen in Table 5. There is a lack of uniformity over which assessment tool is best suited for each outcome in the literature. If outcomes are being measured with different scales, scoring systems, and questionnaires then it would be difficult to synthesize these results for meaningful analyses.
There is significant heterogeneity of the outcomes for patients who have undergone an operation for CES, how they are defined and measured in the literature. Bladder function, motor function, sensation, bowel function, leg pain and lower-back pain outcomes are the most reported. They are all physiological core domains, which have been prioritized in the literature over the other core domains that relate to life impact, mortality, resource use, and adverse events. However, there has not been consultation with key stakeholders regarding what outcomes are the most important to be justifying this practice. Involvement of key stakeholders through an iterative process has been employed in Rheumatology through OMERACT (Outcome MEasures in Rheumatology) and in Women's Health through the CROWN (CoRe Outcomes in Women's and Newborns health) initiative 81,82 (http://www.omeract.org/; http://www.crown-initiative.org). They have come a long way from developing COS to achieving a level of homogeneity among similar studies to increase the quality and yield of their research. This needs to be achieved for patients who have undergone surgery for CES.
LIMITATIONS
The systematic literature review was carried out by the main author (NS). Uncertainties and discrepancies were discussed with the research team (PRW, TM, MW, SC, and AN). Only English language articles were included. It would have been beneficial to have another independent group conduct the search strategy and data extract independently and to compare the results achieved. Because of the limitation of resources this was not performed.
CONCLUSION
There is significant heterogeneity in outcomes reported for studies after surgery for CES patients and the methods by which they are measured. This indicates a clear need for the development of a COS and the results of this systematic literature will be combined with the results of outcomes sourced from CES patients in qualitative interviews. All outcomes will then be prioritized through a Delphi process and consensus meeting to develop a core list of outcomes determined to be of most importance by key stakeholders.
Key Points
For patients who have had an operation for CES there are inconsistencies in the outcomes reported, defined, and assessed between studies.
Because of the heterogeneity of outcomes reported, defined, and assessed we are unable to synthesize the results for a meta-analysis.
The outcomes have not been validated in the literature by key stakeholders as being important to them.
Supplementary Material
Footnotes
The manuscript submitted does not contain information about medical device(s)/drug(s).
No funds were received in support of this work.
Relevant financial activities outside the submitted work: grants.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website (www.spinejournal.com).
References
- 1.Kostuik JP. Controversies in cauda equina syndrome and lumbar disk herniation. Curr Opin Orthop 1993; 4:125–128. [Google Scholar]
- 2.Gardner A, Gardner E, Morley T. Cauda equina syndrome: a review of the current clinical and medico-legal position. Eur Spine J 2011; 20:690–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Balasubramanian K, Kalsi P, Greenough CG, et al. Reliability of clinical assessment in diagnosing cauda equina syndrome. Br J Neurosurg 2010; 24:383–386. [DOI] [PubMed] [Google Scholar]
- 4.Bell D, Collie D, Statham P. Cauda equina syndrome: what is the correlation between clinical assessment and MRI scanning? Br J Neurosurg 2007; 21:201–203. [DOI] [PubMed] [Google Scholar]
- 5.Gleave J, Macfarlane R. Cauda equina syndrome: what is the relationship between timing of surgery and outcome? Br J Neurosurg 2002; 16:325–328. [DOI] [PubMed] [Google Scholar]
- 6.Ahn UM, Ahn NU, Buchowski JM, et al. Cauda equina syndrome secondary to lumbar disc herniation: a meta-analysis of surgical outcomes. Spine (Phila Pa 1976) 2000; 25:1515–1522. [DOI] [PubMed] [Google Scholar]
- 7.Kohles SS, Kohles DA, Karp AP, et al. Time-dependent surgical outcomes following cauda equina syndrome diagnosis: comments on a meta-analysis. Spine (Phila Pa 1976) 2004; 29:1281–1287. [DOI] [PubMed] [Google Scholar]
- 8.Todd N. Cauda equina syndrome: the timing of surgery probably does influence outcome. Br J Neurosurg 2005; 19:301–306. [DOI] [PubMed] [Google Scholar]
- 9.Srikandarajah N, Boissaud-Cooke MA, Clark S, et al. Does early surgical decompression in cauda equina syndrome improve bladder outcome? Spine (Phila Pa 1976) 2015; 40:580–583. [DOI] [PubMed] [Google Scholar]
- 10.Korse N, Jacobs W, Elzevier H, et al. Complaints of micturition, defecation and sexual function in cauda equina syndrome due to lumbar disk herniation: a systematic review. Eur Spine J 2013; 22:1019–1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sinha IP, Williamson PR, Smyth RL. Outcomes in clinical trials of inhaled corticosteroids for children with asthma are narrowly focussed on short term disease activity. PLoS One 2009; 4:e6276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sinha IP, Smyth RL, Williamson PR. Using the Delphi technique to determine which outcomes to measure in clinical trials: recommendations for the future based on a systematic review of existing studies. PLoS Med 2011; 8:e1000393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Avery K, Chalmers K, Whale K, et al. The importance of stakeholder selection in core outcome set development: how surveying different health professionals may influence outcome selection. Trials 2015; 16:47.25887033 [Google Scholar]
- 14.Williamson PR, Altman DG, Blazeby JM, et al. Developing core outcome sets for clinical trials: issues to consider. Trials 2012; 13:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jones J, Hunter D. Consensus methods for medical and health services research. BMJ 1995; 311:376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chalmers I, Glasziou P. Avoidable waste in the production and reporting of research evidence. Obstet Gynecol 2009; 114:1341–1345. [DOI] [PubMed] [Google Scholar]
- 17.Davey J, Turner RM, Clarke MJ, et al. Characteristics of meta-analyses and their component studies in the Cochrane Database of Systematic Reviews: a cross-sectional, descriptive analysis. BMC Med Res Methodol 2011; 11:160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Akbar A, Mahar A. Lumbar disc prolapse: management and outcome analysis of 96 surgically treated patients. J Pak Med Assoc 2002; 52:62–65. [PubMed] [Google Scholar]
- 19.Allegretti L, Mavilio N, Fiaschi P, et al. Intra-operative vertebroplasty combined with posterior cord decompression a report of twelve cases. Interv Neuroradiol 2014; 20:583–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aly TA, Aboramadan MO. Efficacy of delayed decompression of lumbar disk herniation causing cauda equina syndrome. Orthopedics 2014; 37:e153–e156. [DOI] [PubMed] [Google Scholar]
- 21.Arrigo RT, Kalanithi P, Boakye M. Is cauda equina syndrome being treated within the recommended time frame? Neurosurgery 2011; 68:1520–1526. [DOI] [PubMed] [Google Scholar]
- 22.Ayoub MA. Displaced spinopelvic dissociation with sacral cauda equina syndrome: outcome of surgical decompression with a preliminary management algorithm. Eur Spine J 2012; 21:1815–1825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baba H, Maezawa Y, Furusawa N, et al. The role of calcium deposition in the ligamentum flavum causing a cauda equina syndrome and lumbar radiculopathy. Paraplegia 1995; 33:219–223. [DOI] [PubMed] [Google Scholar]
- 24.Beculic H, Skomorac R, Jusic A, et al. Impact of timing on surgical outcome in patients with cauda equina syndrome caused by lumbar disc herniation. Med Glas (Zenica) 2016; 13:136–141. [DOI] [PubMed] [Google Scholar]
- 25.Bejia I, Younes M, Zrour S, et al. Factors predicting outcomes of mechanical sciatica: a review of 1092 cases. Joint Bone Spine 2004; 71:567–571. [DOI] [PubMed] [Google Scholar]
- 26.Bellabarba C, Schildhauer TA, Vaccaro AR, et al. Complications associated with surgical stabilization of high-grade sacral fracture dislocations with spino-pelvic instability. Spine (Phila Pa 1976) 2006; 31 (11S):S80–S88. [DOI] [PubMed] [Google Scholar]
- 27.Božić B, Kogler A, Negovetić L, et al. Sequestred extrusion of lumbar disc: experimental model, clinical picture, diagnosis and treatment. Acta Clin Croat 2003; 42:213. [Google Scholar]
- 28.Buchner M, Schiltenwolf M. Cauda equina syndrome caused by intervertebral lumbar disk prolapse: mid-term results of 22 patients and literature review. Orthopedics 2002; 25:727–731. [DOI] [PubMed] [Google Scholar]
- 29.Busse JW, Bhandari M, Schnittker JB, et al. Delayed presentation of cauda equina syndrome secondary to lumbar disc herniation: functional outcomes and health-related quality of life. CJEM 2001; 3:285–291. [DOI] [PubMed] [Google Scholar]
- 30.Crocker M, Fraser G, Boyd E, et al. The value of interhospital transfer and emergency MRI for suspected cauda equina syndrome: a 2-year retrospective study. Ann R Coll Surg Engl 2008; 90:513–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dhatt S, Tahasildar N, Tripathy SK, et al. Outcome of spinal decompression in cauda equina syndrome presenting late in developing countries: case series of 50 cases. Eur Spine J 2011; 20:2235–2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Domen P, Hofman P, Van Santbrink H, et al. Predictive value of clinical characteristics in patients with suspected cauda equina syndrome. Eur J Neurol 2009; 16:416–419. [DOI] [PubMed] [Google Scholar]
- 33.Duncan JW, Bailey RA. Cauda equina syndrome following decompression for spinal stenosis. Global Spine J 2011; 1:15–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ea H-K, Lioté F, Lot G, et al. Cauda equina syndrome in ankylosing spondylitis: successful treatment with lumboperitoneal shunting. Spine (Phila Pa 1976) 2010; 35:E1423–E1429. [DOI] [PubMed] [Google Scholar]
- 35.Foruria X, de Gopegui KR, García-Sánchez I, et al. Cauda equina syndrome secondary to lumbar disc herniation: Surgical delay and its relationship with prognosis. Rev Esp Cir Ortop Traumatol 2016; 60:153–159. [DOI] [PubMed] [Google Scholar]
- 36.Fukui J, Ohotsuka K, Asagai Y. Improved symptoms and lifestyle more than 20 years after untethering surgery for primary tethered cord syndrome. Neurourol Urodyn 2011; 30:1333–1337. [DOI] [PubMed] [Google Scholar]
- 37.Fuso FAF, Dias ALN, Letaif OB, et al. Epidemiological study of cauda equina syndrome. Acta Ortop Bras 2013; 21:159–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Galasko C. Spinal instability secondary to metastatic cancer. J Bone Joint Surg Br 1991; 73:104–108. [DOI] [PubMed] [Google Scholar]
- 39.Galvin J, Freedman B, Schoenfeld A, et al. Morbidity of early spine surgery in the multiply injured patient. Arch Orthop Trauma Surg 2014; 134:1211–1217. [DOI] [PubMed] [Google Scholar]
- 40.Gooding BW, Higgins MA, Calthorpe DA. Does rectal examination have any value in the clinical diagnosis of cauda equina syndrome? Br J Neurosurg 2013; 27:156–159. [DOI] [PubMed] [Google Scholar]
- 41.Henriques T, Olerud C, Petren-Mallmin M, et al. Cauda equina syndrome as a postoperative complication in five patients operated for lumbar disc herniation. Spine (Phila Pa 1976) 2001; 26:293–297. [DOI] [PubMed] [Google Scholar]
- 42.Hussain S, Gullan R, Chitnavis B. Cauda equina syndrome: outcome and implications for management. Br J Neurosurg 2003; 17:164–167. [DOI] [PubMed] [Google Scholar]
- 43.Kennedy JG, Soffe KE, McGrath A, et al. Predictors of outcome in cauda equina syndrome. Eur Spine J 1999; 8:317–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.KOTİL K, ERAS M, AKÇETİN M, et al. Do the spinal pathologies that accompany lumbar disc disease affect surgical prognosis? Turkish Neurosurg 2006; 16: 4. [Google Scholar]
- 45.Li X, Dou Q, Hu S, et al. Treatment of cauda equina syndrome caused by lumbar disc herniation with percutaneous endoscopic lumbar discectomy. Acta Neurol Belg 2016; 116:185–190. [DOI] [PubMed] [Google Scholar]
- 46.Lich Ng LC, Tafazal S, Longworth S, et al. Cauda equina syndrome: an audit. can we do better? J Orthop Med 2004; 26:98–101. [Google Scholar]
- 47.Lyons MK, Atkinson JL, Wharen RE, et al. Surgical evaluation and management of lumbar synovial cysts: the Mayo Clinic experience. J Neurosurg 2000; 93:53–57. [DOI] [PubMed] [Google Scholar]
- 48.Marascalchi BJ, Passias PG, Goz V, et al. Comparative analysis of patients with cauda equina syndrome versus an unaffected population undergoing spinal surgery. Spine (Phila Pa 1976) 2014; 39:482–490. [DOI] [PubMed] [Google Scholar]
- 49.McCarthy MJH, Aylott CEW, Grevitt MP, et al. Cauda equina syndrome: factors affecting long-term functional and sphincteric outcome. Spine (Phila Pa 1976) 2007; 32:207–216. [DOI] [PubMed] [Google Scholar]
- 50.McKinley WO, Tellis AA, Cifu DX, et al. Rehabilitation outcome of individuals with nontraumatic myelopathy resulting from spinal stenosis. J Spinal Cord Med 1998; 21:131–136. [DOI] [PubMed] [Google Scholar]
- 51.Morita M, Miyauchi A, Okuda S, et al. Intraspinal epidermoid tumor of the cauda equina region: seven cases and a review of the literature. J Spinal Disord Tech 2012; 25:292–298. [DOI] [PubMed] [Google Scholar]
- 52.Lich Ng LC, Tafazal S, Longworth S, et al. Cauda equina syndrome: an audit. Can we do better? J Orthop Med 2004; 26:98–101. [Google Scholar]
- 53.Ökten AI, Özsoy KM, Gezercan Y, et al. Analysis of clinical and surgical outcomes of upper lumbar disk herniations. Neurosurg Q 2015; 25:349–354. [Google Scholar]
- 54.Olivero WC, Wang HA, Hanigan WC, et al. Cauda equina syndrome (CES) from lumbar disc herniations. J Spinal Disord Tech 2009; 22:202–206. [DOI] [PubMed] [Google Scholar]
- 55.Podnar S. Cauda equina lesions as a complication of spinal surgery. Eur Spine J 2010; 19:451–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Qureshi A, Sell P. Cauda equina syndrome treated by surgical decompression: the influence of timing on surgical outcome. Eur Spine J 2007; 16:2143–2151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Raj D, Coleman N. Cauda Equina Syndrome secondary to lumbar disc herniation. Acta Orthop Belg 2008; 74:522–527. [PubMed] [Google Scholar]
- 58.Ronen J, Goldin D, Itzkovich M, et al. Outcomes in patients admitted for rehabilitation with spinal cord or cauda equina lesions following degenerative spinal stenosis. Disabil Rehabil 2005; 27:884–889. [DOI] [PubMed] [Google Scholar]
- 59.Sakai Y, Matsuyama Y, Katayama Y, et al. Spinal myxopapillary ependymoma: neurological deterioration in patients treated with surgery. Spine (Phila Pa 1976) 2009; 34:1619–1624. [DOI] [PubMed] [Google Scholar]
- 60.Sapkas GS, Mavrogenis AF, Papagelopoulos PJ. Transverse sacral fractures with anterior displacement. Eur Spine J 2008; 17:342–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Schebesch K-M, Albert R, Brawanski A, et al. Urgent discectomy: clinical features and neurological outcome. Surg Neurol Int 2016; 2016:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Schildhauer TA, Bellabarba C, Nork SE, et al. Decompression and lumbopelvic fixation for sacral fracture-dislocations with spino-pelvic dissociation. J Orthop Trauma 2006; 20:447–457. [DOI] [PubMed] [Google Scholar]
- 63.Sengoz A, Kotil K, Tasdemiroglu E. Posterior epidural migration of herniated lumbar disc fragment Clinical article. J Neurosurg Spine 2011; 14:313–317. [DOI] [PubMed] [Google Scholar]
- 64.Shapiro S. Cauda equina syndrome secondary to lumbar disc herniation. Neurosurgery 1993; 32:743–747. [DOI] [PubMed] [Google Scholar]
- 65.Shapiro S. Medical realities of cauda equina syndrome secondary to lumbar disc herniation. Spine (Phila Pa 1976) 2000; 25:348–351. [DOI] [PubMed] [Google Scholar]
- 66.Shen L, Fang L, Qiu Y, et al. Study on different surgical approaches for acute lumber disk protrusion combined with Cauda Equina Syndrome. Int J Clin Exp Pathol 2014; 7:8875. [PMC free article] [PubMed] [Google Scholar]
- 67.Shi JG, Jia LS, Yuan W, et al. Clinical classification of cauda equina syndrome for proper treatment: a retrospective analysis of 39 patients. Acta Orthop 2010; 81:391–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Smith MD, Bohlman H. Spondylolisthesis treated by a single-stage operation combining decompression with in situ posterolateral and anterior fusion. An analysis of eleven patients who had long-term follow-up. J Bone Joint Surg Am 1990; 72:415–421. [PubMed] [Google Scholar]
- 69.Sokolowski MJ, Garvey TA, Perl J, et al. Postoperative lumbar epidural hematoma: does size really matter? Spine (Phila Pa 1976) 2008; 33:114–119. [DOI] [PubMed] [Google Scholar]
- 70.Sun T, Liu Z, Liu S, et al. The clinical study of repairing cauda equina fibres with fibrin glue after lumbar fracture and dislocation. Spinal Cord 2010; 48:633–637. [DOI] [PubMed] [Google Scholar]
- 71.Szövérfi Z, Lazary A, Bozsódi Á, et al. Primary Spinal Tumor Mortality Score (PSTMS): a novel scoring system for predicting poor survival. Spine J 2014; 14:2691–2700. [DOI] [PubMed] [Google Scholar]
- 72.Takahashi T, Hanakita J, Kawaoka T, et al. Indication for partial vertebral osteotomy and realignment in posterior spinal fixation for osteoporotic thoracolumbar vertebral collapse with neurological deficits. Neurol Med Chir (Tokyo) 2016; 56:485–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tamburrelli F, Genitiempo M, Bochicchio M, et al. Cauda equina syndrome: evaluation of the clinical outcome. Eur Rev Med Pharmacol Sci 2014; 18:1098–1105. [PubMed] [Google Scholar]
- 74.Tan G-q, He J-l, Fu B-s, et al. Lumbopelvic fixation for multiplanar sacral fractures with spinopelvic instability. Injury 2012; 43:1318–1325. [DOI] [PubMed] [Google Scholar]
- 75.Todd NV. Causes and outcomes of cauda equina syndrome in medico-legal practice: a single neurosurgical experience of 40 consecutive cases. Br J Neurosurg 2011; 25:503–508. [DOI] [PubMed] [Google Scholar]
- 76.Walker JL, Schulak D, Murtagh R. Midline disk herniations of the lumbar spine. South Med J 1993; 86:13–17. [DOI] [PubMed] [Google Scholar]
- 77.Wostrack M, Shiban E, Obermueller T, et al. Conus medullaris and cauda equina tumors: clinical presentation, prognosis, and outcome after surgical treatment. Clinical article. J Neurosurg Spine 2014; 20:335–343. [DOI] [PubMed] [Google Scholar]
- 78.Yamanishi T, Yasuda K, Yuki T, et al. Urodynamic evaluation of surgical outcome in patients with urinary retention due to central lumbar disc prolapse. Neurourol Urodyn 2003; 22:670–675. [DOI] [PubMed] [Google Scholar]
- 79.Todd N, Dickson R. Standards of care in cauda equina syndrome. Br J Neurosurg 2016; 30:518–522. [DOI] [PubMed] [Google Scholar]
- 80.Fraser S, Roberts L, Murphy E. Cauda equina syndrome: a literature review of its definition and clinical presentation. Arch Phys Med Rehabil 2009; 90:1964–1968. [DOI] [PubMed] [Google Scholar]
- 81.Kirkham JJ, Gargon E, Clarke M, et al. Can a core outcome set improve the quality of systematic reviews? A survey of the Co-ordinating Editors of Cochrane Review Groups. Trials 2013; 14:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tugwell P, Boers M, Brooks P, et al. OMERACT: an international initiative to improve outcome measurement in rheumatology. Trials 2007; 8:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


