Abstract
The surgical treatment of adolescent idiopathic scoliosis (AIS) involves 3-dimensional curve correction with multisegmental pedicle screws attached to contoured bilateral rods. The substantial corrective forces exert a high level of stress on the rods, and the ability of the rod to withstand these forces without undergoing permanent deformation relies on its biomechanical properties. These properties, in turn, are dependent on the material, diameter, and shape of the rod. The surgical treatment of AIS is characterized by the requirement for a special biomechanical profile that may differ substantially from what is needed for adult deformity surgery. This overview summarizes the current knowledge of rod biomechanics in frequently used rod constructs, with a particular focus on translational research between biomechanical studies and clinical applicability in AIS patients.
Keywords: Scoliosis, Surgery, Adolescent, Spinal fusion, Methods
INTRODUCTION
Surgical treatment of adolescent idiopathic scoliosis (AIS) is complex and involves extensive 3-dimensional (3D) correction and fusion of the spine while avoiding intraoperative complications such as pedicle fractures, dural tears, excessive bleeding and neurological deterioration. Standard surgical treatment of AIS patients involves posterior multisegmental pedicle screw insertion in the length of the intended fusion. With pedicle screws connected to dual rods the deformity is corrected using one or multiple different techniques including translation, distraction-compression, rod derotation, direct vertebral derotation, cantilever, in situ bending or vertebral coplanar alignment [1-4]. Before insertion, the rods are bend to the desired sagittal contour to achieve a balanced spine with a natural lordosis/kyphosis profile (Fig. 1). The success of these intraoperative corrective maneuvers is highly dependent on rod biomechanics as they exert high levels of stress on the rods. Corrective forces increase the risk of plastic deformation of the rod and subsequent loss of correction due to the low viscoelasticity of the tissue [5]. A thorough understanding of the stress and strains exerted on the rods due to contouring and the forces and torques applied during correction can ultimate improve clinical results in AIS surgery. Despite extensive research into the potential benefits and side effect of different rod constructs there is no universal agreement as to the optimal biomechanical properties.
Fig. 1.

Rod contouring using a French bender whereby a physiological sagittal profile is mimicked prior to rod insertion.
AIS patients often present with a preoperative hypokyphosis and the restoration of sagittal alignment has received increasing attention in recent years. Several studies have shown that all-pedicle screw constructs may be associated with a failure to restore thoracic kyphosis to a normal range postoperatively [6-8]. Postoperative hypokyphosis can lead to increased risk of adjacent segment disease and poorer quality of life and should be a main concern during surgery [9,10]. The lack of kyphosis restoration has been attributed to the corrective maneuvers [11-15] but has also been associated with the biomechanical properties of the construct (Fig. 2) [16,17].
Fig. 2.
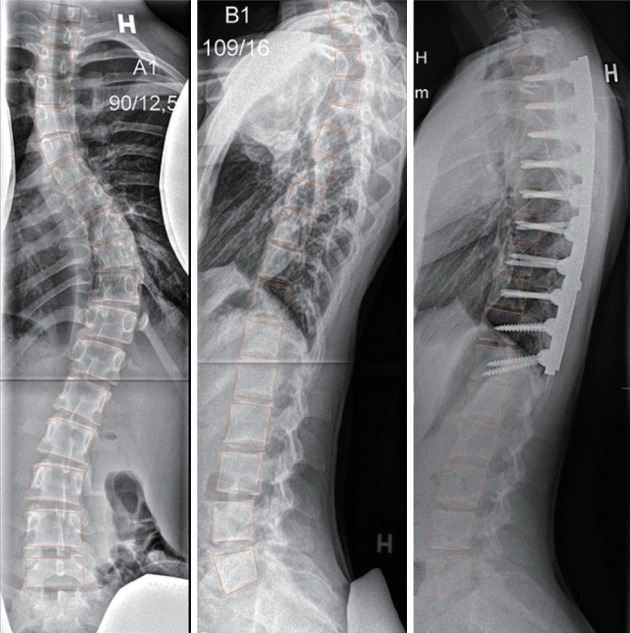
A main thoracic curve with a preoperative severe hypokyphosis (lordosis). The lordosis is only minimally improved after surgery and a proximal junctional kyphosis is developing.
The ultimate goal of AIS surgery is to correct the deformity, ensure a balanced spine with level shoulders, and prevent curve deterioration [18]. The current trend in AIS surgery is to use higher pedicle screw density to increase load sharing and apply stiffer rod constructs to avoid rod deformation and loss of correction in both the coronal, sagittal and axial plane. This development has been largely driven by biomechanical studies suggesting improved sustainability of the correction using this approach. However, increased construct stiffness may have side effects; as implant-bone fixation is increased, a higher proportional load is transferred to the rod, which decreases the physiological stress on the bone. This may impact bone quality long-term although no studies have verified this theory in AIS patients. Furthermore, increased rod stiffness may add to the junctional stress on the levels adjacent to the instrumentation which increase the risk of adjacent segment disease [19] or decompensation above the implant. The biomechanical profile of a rod largely depends on diameter, shape and material properties. This overview aims to describe these concepts and assess the potential advantages and pitfalls of their clinical use in surgical treatment of AIS.
BIOMECHANICAL PROPERTIES
Biomechanical properties of spinal rods are typically differentiated by yield strength and stiffness. The yield strength, or yield stress, can be defined as the stress at which permanent deformation occurs. Stiffness, or rigidity, can be defined as the extent to which a rod resists deformation in response to an applied force. This is often reported as Young’s modulus, which is measure of material elasticity (or stiffness) and is also known as the elastic modulus. The difference between yield strength and stiffness can be exemplified by a classic rubber band that requires very little stress to deform (low stiffness) but a much higher stress is needed for permanent deformation (high yield strength). While these material properties can be easily measured in a laboratory setting the theoretical implications cannot necessarily be transferred to the clinical reality. Furthermore, Ayers et al. [20] found that the biomechanical profile of a given rod was very sensitive to differences in production as individual properties varied greatly between manufacturers for the same material. Pienkowski et al. [21] showed that fatigue life of the implant was explained by implant type rather than material further adding to the complexity of understanding rod biomechanics.
ROD MATERIAL
The most frequently reported rod materials used in AIS corrective surgery are stainless steel (SS) or ultrahigh strength stainless steel (UHSS), titanium alloy (Ti), and cobalt chromium (CoCr) (Table 1) [22].
Table 1.
Mechanical properties of 3 main groups of spinal implants in adolescent idiopathic scoliosis surgery [22]
| Biomaterial | Elastic modulus (Young’s modulus) (Gpa) | Yield strength (MPa) | Fatigue strength (MPa) |
|---|---|---|---|
| CoCr alloys | 200–300 | 300–2,000 | 207–950 |
| Titanium alloys | 110–116 | 485–1,034 | 300–389 |
| Stainless steel | 190 | 792 | 241–820 |
CoCr, cobalt chromium.
Generally, Ti is characterized by high yield strength but a lower stiffness compared to SS, UHSS and CoCr. CoCr has only in recent years been introduced in AIS surgery but is characterized by a very high stiffness and low yield strength [23,24]. Ti originally gained popularity in both adult and adolescent spine deformity surgery due to a high biocompatibility, corrosion resistance and magnetic resonance imaging (MRI) compatibility. Scuderi et al. [25] examined the presence of MRI artifacts in an animal model between Ti, SS, and CoCr. Ti rods showed the least amount of artefacts followed by CoCr while SS showed the highest amount. Several studies have verified these finding although Trammell et al. [26] and Ahmad et al. [27] found that the difference in artefacts between Ti and CoCr did not interfere with the evaluation of the spinal canal and surrounding neural elements. It has been reported that Ti compared to SS produce substantially better overall diagnostic quality [28-30] although the clinical implication of this difference has not been established.
Serhan et al. [31] conducted a biomechanical study comparing Ti, CoCr, UHSS, and SS. Rods were contoured with one-plane bending and placed in a synthetic spine model imitating spinal deformity correction. After removal from the construct 90% of Ti rod retained their original shape versus 77%, 63%, and 54% of UHSS, SS and CoCr, respectively, illustrating the lower yield strength of the latter materials. Conversely, when the corrective forces were measured in-construct, UHSS and CoCr were found to have 42% higher corrective forces compared to Ti due to a higher stiffness.
AIS surgery involves rod contouring to mimic the sagittal profile with a lumbar lordosis followed by a thoracic kyphosis within the normal range (Fig. 1). This intraoperative bending of the rod introduces cracks or dents in the material, which can reduce the endurance limit of the rod, also termed the “notch effect”. Slivka et al. [32] found that the endurance limit of CoCr was at least 25% higher than UHSS, SS, or TI in response to repetitive bending whereas Noshchenko et al. [33] showed the highest “springback” (or yield strength) in Ti rods compared to SS. Wedemeyer et al. [34] in a bovine model, confirmed that Tis can withstand higher strains and yield than the relatively brittle SS before failure occurs after bending. However, Lindsey et al. [35] contradicted these results demonstrating a lower fatigue life of Ti compared to SS in response to bending. Burger et al. [36] performed 3-point bending on Ti and SS rods and stored the rods for 8 months at 37°C temperature to mimic a physiological environment. Ti rods lost correction corresponding to 6° per year for a 300-mm rod, which was considerably more than SS rods.
A few clinical studies have investigated the importance of rod material in AIS patients. Lamerain et al. [37] compared SS with CoCr rods in 90 AIS patients and found significantly better coronal curve correction, reduced loss of correction and a better kyphosis restoration using CoCr rods. Angelliaume et al. [38] using hybrid constructs found that coronal curve correction was similar for Ti and CoCr constructs but that a better kyphosis restoration was seen in the CoCr group. Cidambi et al. [39] using 5.5-mm UHSS found that the rod on the concave side of the curve flattened by 21° 4–6 weeks postoperatively, which was similar to the results from Salmingo et al. [40] showing 16° deformation of Ti rods. Le Navéaux et al. [41] showed that even in stiff 5.5-mm CoCr constructs some postoperative 3D rod deformation can be expected.
ROD DIAMETER AND PROFILE
Surgeons may choose rods of different diameters to achieve the desired biomechanics in any given case. An increase in radius alters stiffness to the 4th power of the change in radius. Consequently, the bending stiffness increases from 5.17 EI (Nm2) for a rod diameter of 5.5 to 9.18 EI (Nm2) for a rod diameter of 6.35 mm. A change in rod diameter is therefore bound to result in a stiffer construct but whether this is beneficial to AIS patients is a crucial point of interest.
Huang et al. [42] compared 5.5-mm vs. 6.35-mm Ti rods in 93 AIS patient and found no difference in curve correction, loss of correction or coronal global balance. Liu et al. [43] also reported similar coronal curve correction of single thoracic curves, however the authors found a significantly better kyphosis restoration with the 6.35-mm rods. Abul-Kasim [44] made a similar observation in 116 AIS patients reporting a better kyphosis restoration and derotation with higher diameter rods but with no difference in coronal correction. Fletcher et al. [45] reported 2-year follow-up on 214 AIS patients and found that 72% vs. 47% had a normal kyphosis in the 6.35 and 5.5 mm groups, respectively. In contrast to these studies Prince et al reported on a national database of 163 pediatric scoliosis patients and found the 5.5 mm group to have a significantly better curve correction 2 years postoperatively compared to 6.35-mm rods. Rod diameter was not found to be predictive of sagittal plane correction. The analysis, however, did not adjust for rod material and the cohort included non-AIS patients.
In recent years, a few studies have examined the potential benefits of using a noncircular rod. In a biomechanical simulation Cui et al. [46] found that for a given cross-sectional area, the axial stiffness rises by about 2.5% and the maximum stress drops by up to 22% when the section is square compared to when it is circular. Gehrchen et al. [16] reported the immediate curve correction comparing circular and “beam-like” rods in 129 AIS patients. Coronal curve correction was found to be 9% higher in the beam-like group. A failure to restore thoracic kyphosis was seen but with no significant difference between the 2 groups.
HYBRID RODS OR CONSTRUCTS
Proximal junctional kyphosis (PJK) is an abnormal kyphosis that develops at the upper instrumented vertebra in response to fusion. It is a relatively common finding after AIS deformity surgery and is universally considered a unsatisfactory outcome [47-49]. Multiple factors have been associated with PJK including disruption of posterior ligaments and poor postoperative sagittal alignment or the use of all-pedicle screw constructs. It has also been suggested that a high construct rigidity can lead to increased junctional stress at the adjacent upper segment leading to forward decompensation and ultimately PJK. Han et al. [50] found that increasing the rigidity of the construct using multiple-rod CoCr vs. 2-rod Ti significantly increased the rate of PJK. In a subsequent study, Han et al. [51] found that patients operated with CoCr rods compared to Ti more frequently developed PJK. It should be noted that these studies were conducted on adult deformity patients who differ in a number of ways from AIS patients.
Whether a gradual stress reduction at the proximal level of the construct could reduce the rate of PJK has been the focus of several studies. Lange et al. [52] investigated the effect of using cerclage wires at the proximal segment of a short lumbar fusion. At the proximal transition segment rigidity was reduced by about 60% compared to an all-pedicle screw construct. Facchinello et al. [53] and Thawrani et al. [54] reported similar results using proximal hooks showing lower stiffness at the upper instrumented level which applied less force on the anchors. Cahill et al. [55] using computer simulation showed that the use of a transition rod with a proximal decrease in diameter leads to less disc angulation compared to a standard construct. Maximum implant stress was theoretically reduced by up to 60%. This concept was applied in a clinical setting by Ohrt-Nissen et al. [56] who showed that the use of double transition rods in AIS corrective surgery resulted in an improved kyphosis restoration compared to a standard construct. However, whether this new rod concept can reduce the rate of PJK is not yet known.
SHAPE-MEMORY METAL RODS
Some authors have argued that the stiffness of the implant is not of clinical relevance as most available implant has a stiffness that far exceeds the need for stabile fusion. Some have advocated for the use of dynamic flexible rods to avoid predisposing the patients to PJK and adjacent disc degeneration by reducing the peak stress on the screw anchors during correction [19,57]. The shape-memory metal (SMM) Nitinol (a nickel-Ti) is characterized by an ability to recover from considerable deformation and return to a preconditioned shape when heated above its transformation temperature [58,59] (e.g., body temperature). This may be beneficial because the recovery properties of the rod apply a progressive and constant correction force, which would more gradually counteract the low viscoelasticity of the tissue that is responsible for rod flattening. A few clinical studies have described the use of SMM rods in scoliosis surgery. Wang et al. [60,61] showed satisfactory results using a SMM rod as a temporary rod during surgery to correct the deformity before replacing it with a rigid rod. A recent controlled randomized clinical pilot trial described the use of SMM rods as definitive treatment in AIS patients [62]. The authors found no difference in coronal or sagittal parameters compared to standard rods at 5-year follow-up and concluded that the SMM rods were safe and efficient for AIS corrective surgery.
DISCUSSION
The final outcome of AIS surgery relies not only on choice of rods but also patient characteristics (e.g., skeletal maturity, body mass index), curve type and surgical strategy. Surgical treatment of AIS is substantially different from adult deformity surgery and as such the desirable biomechanical properties of the rods are different. The literature is abundant with biomechanical studies on various implant types but there is a lack of high-quality clinical studies in AIS patients comparing implants. AIS corrective surgery is characterized by a high fusion rate compared to adult deformity patients and revision surgery is a rare event [63,64]. As such, long-term durability of a rod material may have limited clinical applicability. While the higher yield strength of Ti theoretically reduces the risk of rod fracture this complication is almost nonexistent in AIS patients and should not be a main priority in choice of rod. Huang et al. [42] discussed the theoretical disadvantage of using high-stiffness rods when considering the 20–30 fold lower Young Modulus of bone. This mismatch could decrease the stress on the bone-implant interface (stress shielding), which can lead to bone resorption and poor osteointegration. While this theory may apply in an elderly population it has not been shown to have any clinical relevance in AIS surgery.
It seems that the primary objectives of curve correction and sagittal restoration would be best achieved using a stiffer construct, which is minimally weakened by intraoperative contouring. This is likely the reason for the increasing popularity of CoCr and higher-diameter rods. However, high-quality studies on this topic are needed for any firm conclusions to be drawn. Furthermore, we encourage future studies to assess the efficacy of individually tailored rod that are bend at the manufacturing stage to minimize rod weakening during intraoperative contouring.
CONCLUSION
Clinical studies comparing biomechanical differences between rod constructs are generally of poor methodological quality with a high risk of bias. While curve correction does not seem to be substantially different between rod types there is some evidence to suggest that the sagittal profile may be more efficiently restored using stiffer rod constructs. The use of transition rods or shape memory rods may decrease junctional stress but the clinical applicability of these newer designs has not yet been firmly established.
Footnotes
SO, MG, and BD received an institutional research grant from K2M outside the submitted work. MG and BD received an institutional research grant from Medtronic outside the submitted work
REFERENCES
- 1.Hwang SW, Samdani AF, Cahill PJ. The impact of segmental and en bloc derotati on maneuvers on scoliosis correction and rib prominence in adolescent idiopathic scoliosis. J Neurosurg Spine. 2012;16:345–50. doi: 10.3171/2011.11.SPINE11277. [DOI] [PubMed] [Google Scholar]
- 2.Clement JL, Chau E, Geoffray A, et al. Restoration of thoracic kyphosis by simultaneous translation on two rods for adolescent idiopathic scoliosis. Eur Spine J. 2014;23 Suppl 4:S438–45. doi: 10.1007/s00586-014-3340-9. [DOI] [PubMed] [Google Scholar]
- 3.Charles YP, Bouchaïb J, Walter A, et al. Sagittal balance correction of idiopathic scoliosis using the in situ contouring technique. Eur Spine J. 2012;21:1950–6. doi: 10.1007/s00586-012-2356-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tang X, Zhao J, Zhang Y. Radiographic, clinical, and patients’ assessment of segmental direct vertebral body derotation versus simple rod derotation in main thoracic adolescent idiopathic scoliosis: a prospective, comparative cohort study. Eur Spine J. 2015;24:298–305. doi: 10.1007/s00586-014-3650-y. [DOI] [PubMed] [Google Scholar]
- 5.Wang X, Aubin CE, Labelle H, et al. Biomechanical analysis of corrective forces in spinal instrumentation for scoliosis treatment. Spine (Phila Pa 1976) 2012;37:E1479–87. doi: 10.1097/BRS.0b013e3182706745. [DOI] [PubMed] [Google Scholar]
- 6.Yilmaz G, Borkhuu B, Dhawale AA, et al. Comparative analysis of hook, hybrid, and pedicle screw instrumentation in the posterior treatment of adolescent idiopathic scoliosis. J Pediatr Orthop. 2012;32:490–9. doi: 10.1097/BPO.0b013e318250c629. [DOI] [PubMed] [Google Scholar]
- 7.Lowenstein JE, Matsumoto H, Vitale MG, et al. Coronal and sagittal plane correction in adolescent idiopathic scoliosis: a comparison between all pedicle screw versus hybrid thoracic hook lumbar screw constructs. Spine (Phila Pa 1976) 2007;32:448–52. doi: 10.1097/01.brs.0000255030.78293.fd. [DOI] [PubMed] [Google Scholar]
- 8.Ohrt-Nissen S, Hallager DW, Karbo T, et al. Radiographic and functional outcome in adolescent idiopathic scoliosis operated with hook/hybrid versus all-pedicle screw instrumentation-a retrospective study in 149 patients. Spine Deform. 2017;5:401–8. doi: 10.1016/j.jspd.2017.05.002. [DOI] [PubMed] [Google Scholar]
- 9.Ilharreborde B, Morel E, Mazda K, et al. Adjacent segment disease after instrumented fusion for idiopathic scoliosis: review of current trends and controversies. J Spinal Disord Tech. 2009;22:530–9. doi: 10.1097/BSD.0b013e31818d64b7. [DOI] [PubMed] [Google Scholar]
- 10.Hwang SW, Samdani AF, Tantorski M, et al. Cervical sagittal plane decompensation after surgery for adolescent idiopathic scoliosis: an effect imparted by postoperative thoracic hypokyphosis. J Neurosurg Spine. 2011;15:491–6. doi: 10.3171/2011.6.SPINE1012. [DOI] [PubMed] [Google Scholar]
- 11.Mladenov KV, Vaeterlein C, Stuecker R. Selective posterior thoracic fusion by means of direct vertebral derotation in adolescent idiopathic scoliosis: effects on the sagittal alignment. Eur Spine J. 2011;20:1114–7. doi: 10.1007/s00586-011-1740-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Watanabe K, Nakamura T, Iwanami A, et al. Vertebral derotation in adolescent idiopathic scoliosis causes hypokyphosis of the thoracic spine. BMC Musculoskelet Disord. 2012;13:99. doi: 10.1186/1471-2474-13-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mattila M, Jalanko T, Helenius I. En bloc vertebral column derotation provides spinal derotation but no additional effect on thoracic rib hump correction as compared with no derotation in adolescents undergoing surgery for idiopathic scoliosis with total pedicle screw instrumentation. Spine (Phila Pa 1976) 2013;38:1576–83. doi: 10.1097/BRS.0b013e31829a6d37. [DOI] [PubMed] [Google Scholar]
- 14.Newton PO, Yaszay B, Upasani VV, et al. Preservation of thoracic kyphosis is critical to maintain lumbar lordosis in the surgical treatment of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2010;35:1365–70. doi: 10.1097/BRS.0b013e3181dccd63. [DOI] [PubMed] [Google Scholar]
- 15.Potter BK, Lenke LG, Kuklo TR. Prevention and management of iatrogenic flatback deformity. J Bone Joint Surg Am. 2004;86-A:1793–808. doi: 10.2106/00004623-200408000-00027. [DOI] [PubMed] [Google Scholar]
- 16.Gehrchen M, Ohrt-Nissen S, Hallager DW, et al. A uniquely shaped rod improves curve correction in surgical treatment of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2016;41:1139–45. doi: 10.1097/BRS.0000000000001504. [DOI] [PubMed] [Google Scholar]
- 17.Cao Y, Xiong W, Li F. Pedicle screw versus hybrid construct instrumentation in adolescent idiopathic scoliosis: meta-analysis of thoracic kyphosis. Spine (Phila Pa 1976) 2014;39:E800–10. doi: 10.1097/BRS.0000000000000342. [DOI] [PubMed] [Google Scholar]
- 18.de Kleuver M, Lewis SJ, Germscheid NM, et al. Optimal surgical care for adolescent idiopathic scoliosis: an international consensus. Eur Spine J. 2014;23:2603–18. doi: 10.1007/s00586-014-3356-1. [DOI] [PubMed] [Google Scholar]
- 19.Pan A, Hai Y, Yang J, et al. Adjacent segment degeneration after lumbar spinal fusion compared with motion-preservation procedures: a meta-analysis. Eur Spine J. 2016;25:1522–32. doi: 10.1007/s00586-016-4415-6. [DOI] [PubMed] [Google Scholar]
- 20.Ayers R, Hayne M, Burger E. Spine rod straightening as a possible cause for revision. J Mater Sci Mater Med. 2017;28:123. doi: 10.1007/s10856-017-5935-2. [DOI] [PubMed] [Google Scholar]
- 21.Pienkowski D, Stephens GC, Doers TM, et al. Multicycle mechanical performance of titanium and stainless steel transpedicular spine implants. Spine (Phila Pa 1976) 1998;23:782–8. doi: 10.1097/00007632-199804010-00008. [DOI] [PubMed] [Google Scholar]
- 22.Ratner BD, Hoffman AS, Schoen FJ, et al. Biomaterials science: an introduction to materials in medicine. 2nd ed. Boston: Elsevier Science; 2004. [Google Scholar]
- 23.Scheer JK, Tang JA, Deviren V, et al. Biomechanical analysis of cervicothoracic junction osteotomy in cadaveric model of ankylosing spondylitis: effect of rod material and diameter. J Neurosurg Spine. 2011;14:330–5. doi: 10.3171/2010.10.SPINE1059. [DOI] [PubMed] [Google Scholar]
- 24.Demura S, Murakami H, Hayashi H, et al. Influence of rod contouring on rod strength and stiffness in spine surgery. Orthopedics. 2015;38:e520–3. doi: 10.3928/01477447-20150603-61. [DOI] [PubMed] [Google Scholar]
- 25.Scuderi GJ, Greenberg SS, Cohen DS, et al. A biomechanical evaluation of magnetic resonance imaging-compatible wire in cervical spine fixation. Spine (Phila Pa 1976) 1993;18:1991–4. doi: 10.1097/00007632-199310001-00011. [DOI] [PubMed] [Google Scholar]
- 26.Trammell TR, Flint K, Ramsey CJ. A comparison of MRI and CT imaging clarity of titanium alloy and titanium alloy with cobalt-chromium-alloy pedicle screw and rod implants in the lumbar spine. J Bone Joint Surg Am. 2012;94:1479–83. doi: 10.2106/JBJS.K.01470. [DOI] [PubMed] [Google Scholar]
- 27.Ahmad FU, Sidani C, Fourzali R, et al. Postoperative magnetic resonance imaging artifact with cobalt-chromium versus titanium spinal instrumentation: presented at the 2013 Joint Spine Section Meeting. Clinical article. J Neurosurg Spine. 2013;19:629–36. doi: 10.3171/2013.7.SPINE1359. [DOI] [PubMed] [Google Scholar]
- 28.Knott PT, Mardjetko SM, Kim RH, et al. A comparison of magnetic and radiographic imaging artifact after using three types of metal rods: stainless steel, titanium, and vitallium. Spine J. 2010;10:789–94. doi: 10.1016/j.spinee.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 29.Rupp R, Ebraheim NA, Savolaine ER, et al. Magnetic resonance imaging evaluation of the spine with metal implants. General safety and superior imaging with titanium. Spine (Phila Pa 1976) 1993;18:379–85. [PubMed] [Google Scholar]
- 30.Rudisch A, Kremser C, Peer S, et al. Metallic artifacts in magnetic resonance imaging of patients with spinal fusion. A comparison of implant materials and imaging sequences. Spine (Phila Pa 1976) 1998;23:692–9. doi: 10.1097/00007632-199803150-00009. [DOI] [PubMed] [Google Scholar]
- 31.Serhan H, Mhatre D, Newton P, et al. Would CoCr rods provide better correctional forces than stainless steel or titanium for rigid scoliosis curves? J Spinal Disord Tech. 2013;26:E70–4. doi: 10.1097/BSD.0b013e31826a0f19. [DOI] [PubMed] [Google Scholar]
- 32.Slivka MA, Fan YK, Eck JC. The effect of contouring on fatigue strength of spinal rods: is it okay to re-bend and which materials are best? Spine Deform. 2013;1:395–400. doi: 10.1016/j.jspd.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 33.Noshchenko A, Xianfeng Y, Armour GA, et al. Evaluation of spinal instrumentation rod bending characteristics for insitu contouring. J Biomed Mater Res B Appl Biomater. 2011;98:192–200. doi: 10.1002/jbm.b.31837. [DOI] [PubMed] [Google Scholar]
- 34.Wedemeyer M, Parent S, Mahar A, et al. Titanium versus stainless steel for anterior spinal fusions: an analysis of rod stress as a predictor of rod breakage during physiologic loading in a bovine model. Spine (Phila Pa 1976) 2007;32:42–8. doi: 10.1097/01.brs.0000251036.99413.20. [DOI] [PubMed] [Google Scholar]
- 35.Lindsey C, Deviren V, Xu Z, et al. The effects of rod contouring on spinal construct fatigue strength. Spine (Phila Pa 1976) 2006;31:1680–7. doi: 10.1097/01.brs.0000224177.97846.00. [DOI] [PubMed] [Google Scholar]
- 36.Burger EL, Baratta RV, King AG, et al. The memory properties of cold-worked titanium rods in scoliosis constructs. Spine (Phila Pa 1976) 2005;30:375–9. doi: 10.1097/01.brs.0000153343.16140.1b. [DOI] [PubMed] [Google Scholar]
- 37.Lamerain M, Bachy M, Delpont M, et al. CoCr rods provide better frontal correction of adolescent idiopathic scoliosis treated by all-pedicle screw fixation. Eur Spine J. 2014;23:1190–6. doi: 10.1007/s00586-014-3168-3. [DOI] [PubMed] [Google Scholar]
- 38.Angelliaume A, Ferrero E, Mazda K, et al. Titanium vs cobalt chromium: what is the best rod material to enhance adolescent idiopathic scoliosis correction with sublaminar bands? Eur Spine J. 2017;26:1732–8. doi: 10.1007/s00586-016-4838-0. [DOI] [PubMed] [Google Scholar]
- 39.Cidambi KR, Glaser DA, Bastrom TP, et al. Postoperative changes in spinal rod contour in adolescent idiopathic scoliosis: an in vivo deformation study. Spine (Phila Pa 1976) 2012;37:1566–72. doi: 10.1097/BRS.0b013e318252ccbe. [DOI] [PubMed] [Google Scholar]
- 40.Salmingo RA, Tadano S, Abe Y, et al. Influence of implant rod curvature on sagittal correction of scoliosis deformity. Spine J. 2014;14:1432–9. doi: 10.1016/j.spinee.2013.08.042. [DOI] [PubMed] [Google Scholar]
- 41.Le Navéaux F, Aubin CE, Parent S, et al. 3D rod shape changes in adolescent idiopathic scoliosis instrumentation: how much does it impact correction? Eur Spine J. 2017;26:1676–83. doi: 10.1007/s00586-017-4958-1. [DOI] [PubMed] [Google Scholar]
- 42.Huang TH, Ma HL, Wang ST, et al. Does the size of the rod affect the surgical results in adolescent idiopathic scoliosis? 5.5-mm versus 6.35-mm rod. Spine J. 2014;14:1545–50. doi: 10.1016/j.spinee.2013.09.026. [DOI] [PubMed] [Google Scholar]
- 43.Liu H, Li Z, Li S, et al. Main thoracic curve adolescent idiopathic scoliosis: association of higher rod stiffness and concave-side pedicle screw density with improvement in sagittal thoracic kyphosis restoration. J Neurosurg Spine. 2015;22:259–66. doi: 10.3171/2014.10.SPINE1496. [DOI] [PubMed] [Google Scholar]
- 44.Abul-Kasim K, Karlsson MK, Ohlin A. Increased rod stiffness improves the degree of deformity correction by segmental pedicle screw fixation in adolescent idiopathic scoliosis. Scoliosis. 2011;6:13. doi: 10.1186/1748-7161-6-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fletcher ND, Jeffrey H, Anna M, et al. Residual thoracic hypokyphosis after posterior spinal fusion and instrumentation in adolescent idiopathic scoliosis: risk factors and clinical ramifications. Spine (Phila Pa 1976) 2012;37:200–6. doi: 10.1097/BRS.0b013e318216106c. [DOI] [PubMed] [Google Scholar]
- 46.Cui Y, Lewis G, Qi G. Numerical analysis of models of the standard TSRH spinal instrumentation: effect of rod crosssectional shape. Comput Methods Biomech Biomed Engin. 2002;5:75–80. doi: 10.1080/10255840290008097. [DOI] [PubMed] [Google Scholar]
- 47.Helgeson MD, Shah SA, Newton PO, et al. Evaluation of proximal junctional kyphosis in adolescent idiopathic scoliosis following pedicle screw, hook, or hybrid instrumentation. Spine (Phila Pa 1976) 2010;35:177–81. doi: 10.1097/BRS.0b013e3181c77f8c. [DOI] [PubMed] [Google Scholar]
- 48.Kim YJ, Bridwell KH, Lenke LG, et al. Proximal junctional kyphosis in adolescent idiopathic scoliosis following segmental posterior spinal instrumentation and fusion: minimum 5-year follow-up. Spine (Phila Pa 1976) 2005;30:2045–50. doi: 10.1097/01.brs.0000179084.45839.ad. [DOI] [PubMed] [Google Scholar]
- 49.Kim YJ, Lenke LG, Bridwell KH, et al. Proximal junctional kyphosis in adolescent idiopathic scoliosis after 3 different types of posterior segmental spinal instrumentation and fusions: incidence and risk factor analysis of 410 cases. Spine (Phila Pa 1976) 2007;32:2731–8. doi: 10.1097/BRS.0b013e31815a7ead. [DOI] [PubMed] [Google Scholar]
- 50.Han S, Hyun SJ, Kim KJ, et al. Rod stiffness as a risk factor of proximal junctional kyphosis after adult spinal deformity surgery: comparative study between cobalt chrome multiple-rod constructs and titanium alloy two-rod constructs. Spine J. 2017;17:962–8. doi: 10.1016/j.spinee.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 51.Han S, Hyun SJ, Kim KJ, et al. Comparative study between cobalt chrome and titanium alloy rods for multilevel spinal fusion: proximal junctional kyphosis more frequently occurred in patients having cobalt chrome rods. World Neurosurg. 2017;103:404–9. doi: 10.1016/j.wneu.2017.04.031. [DOI] [PubMed] [Google Scholar]
- 52.Lange T, Schmoelz W, Gosheger G, et al. Is a gradual reduction of stiffness on top of posterior instrumentation possible with a suitable proximal implant? A biomechanical study. Spine J. 2017;17:1148–55. doi: 10.1016/j.spinee.2017.03.021. [DOI] [PubMed] [Google Scholar]
- 53.Facchinello Y, Brailovski V, Petit Y, et al. Biomechanical assessment of the stabilization capacity of monolithic spinal rods with different flexural stiffness and anchoring arrangement. Clin Biomech (Bristol, Avon) 2015;30:1026–35. doi: 10.1016/j.clinbiomech.2015.09.011. [DOI] [PubMed] [Google Scholar]
- 54.Thawrani DP, Glos DL, Coombs MT, et al. Transverse process hooks at upper instrumented vertebra provide more gradual motion transition than pedicle screws. Spine (Phila Pa 1976) 2014;39:E826–32. doi: 10.1097/BRS.0000000000000367. [DOI] [PubMed] [Google Scholar]
- 55.Cahill PJ, Wang W, Asghar J, et al. The use of a transition rod may prevent proximal junctional kyphosis in the thoracic spine after scoliosis surgery: a finite element analysis. Spine (Phila Pa 1976) 2012;37:E687–95. doi: 10.1097/BRS.0b013e318246d4f2. [DOI] [PubMed] [Google Scholar]
- 56.Ohrt-Nissen S, Dragsted CR, Dahl B, et al. A rod construct with differentiated rigidity improves the restoration of thoracic kyphosis in surgical treatment of adolescent idiopathic scoliosis. doi: 10.3171/2017.7.FOCUS17351. Neurosurg Focus Forthcoming 2017. [DOI] [PubMed] [Google Scholar]
- 57.Highsmith JM, Tumialán LM, Rodts GE., Jr Flexible rods and the case for dynamic stabilization. Neurosurg Focus. 2007;22:E11. doi: 10.3171/foc.2007.22.1.11. [DOI] [PubMed] [Google Scholar]
- 58.Sanders JO, Sanders AE, More R, et al. A preliminary investigation of shape memory alloys in the surgical correction of scoliosis. Spine (Phila Pa 1976) 1993;18:1640–6. doi: 10.1097/00007632-199309000-00012. [DOI] [PubMed] [Google Scholar]
- 59.Wever DJ, Elstrodt JA, Veldhuizen AG, et al. Scoliosis correction with shape-memory metal: results of an experimental study. Eur Spine J. 2002;11:100–6. doi: 10.1007/s005860100347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wang Y, Zheng G, Zhang X, et al. Comparative analysis between shape memory alloy-based correction and traditional correction technique in pedicle screws constructs for treating severe scoliosis. Eur Spine J. 2010;19:394–9. doi: 10.1007/s00586-009-1207-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wang Y, Zheng G, Zhang X, et al. Temporary use of shape memory spinal rod in the treatment of scoliosis. Eur Spine J. 2011;20:118–22. doi: 10.1007/s00586-010-1514-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cheung JPY, Samartzis D, Yeung K, et al. A randomized double-blinded clinical trial to evaluate the safety and efficacy of a novel superelastic nickel-titanium spinal rod in adolescent idiopathic scoliosis: 5-year follow-up. Eur Spine J. 2018;27:327–39. doi: 10.1007/s00586-017-5245-x. [DOI] [PubMed] [Google Scholar]
- 63.Benli IT, Ates B, Akalin S, et al. Minimum 10 years followup surgical results of adolescent idiopathic scoliosis patients treated with TSRH instrumentation. Eur Spine J. 2007;16:381–91. doi: 10.1007/s00586-006-0147-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Scaramuzzo L, Giudici F, Bongetta D, et al. Thoraco-lumbar selective fusion in adolescent idiopathic scoliosis with Lenke C modifier curves: clinical and radiographic analysis at 10-year follow-up. Eur Spine J. 2017;26(Suppl 4):514–23. doi: 10.1007/s00586-017-5152-1. [DOI] [PubMed] [Google Scholar]


