Abstract
Background
Few randomised controlled trials (RCTs) have evaluated the different recalling approaches for enhancing adherence to faecal immunochemical test (FIT)-based screening.
Aim
The authors evaluated the effectiveness of two telecommunication strategies on improving adherence to yearly FIT screening.
Design and setting
A randomised, parallel group trial was performed in a primary care screening practice.
Method
The authors recruited 629 asymptomatic individuals aged 40–70 years with a negative FIT in 2015 to a population-based screening programme. On participation, they were invited to repeat their second round of FIT in 2016, 12 months after the first test. Each participant was randomly assigned to either interactive telephone reminder (n = 207), short message service reminder (SMS, n = 212), or control, where no additional interventions were delivered after the findings of their first FIT was communicated to the participants (n = 210). Reminders in the intervention groups were delivered 1 month before subjects’ expected return. Additional telephone reminders were delivered 2 months after the expected return date to all subjects who defaulted specimen return. The outcomes included rates of FIT collection and specimen return up to 6 months after their expected return.
Results
At 6 months, the cumulative FIT collection rate was 95.1%, 90.4%, and 86.5%, respectively, for the telephone, SMS, and control groups (P = 0.010). The corresponding specimen return rate was 94.1%, 90.0%, and 86.0% (P = 0.022). When compared with the control, only subjects in the telephone group were significantly more likely to collect FIT tubes (adjusted odds ratio [AOR] 3.18, 95% confidence interval [CI] = 1.50 to 6.75, P = 0.003) and return completed specimens (AOR = 2.73, 95% CI = 1.35 to 5.53, P = 0.005).
Conclusion
Interactive telephone reminders are effective at securing previously screened subjects to repeat screening 1 year after a negative finding.
Keywords: adherence, colorectal cancer, screening, short message service, telecommunications, telephone reminders
INTRODUCTION
Guidelines recommend annual faecal immunochemical test (FIT) for colorectal cancer (CRC) screening.1,2 Persistent adherence to FIT screening is a crucial determinant of programme success,3 whereas non-adherence to FIT schedules is a significant contributor to CRC mortality.4 However, organised population-based screening programmes in various regions of the world have not achieved optimal uptake rates.5 In the US, for instance, only 60% of adults aged 50–75 years were up-to-date with CRC screening in 2010.6
A recent study3 reviewed the available evidence regarding effective strategies to enhance screening acceptance. The use of personal invitations and reminders sent by primary care practitioners has been highlighted as a priority for interventions that aimed to enhance CRC screening adherence. Previous studies examining the effectiveness of various strategies have, in general, provided encouraging results, both in organised7–20 and opportunistic settings targeted towards the organisation of practices and/or patients for CRC screening.3 One of the principles of improving adherence rates includes influencing behavioural change, using an interplay of predisposing, enabling, and reinforcing factors, based on the PRECEDE-PROCEED model.21 This model provides the rationale or motivation for factors that enable somebody’s decision to be screened, and also for the factors that reinforce and continuously maintain a subject’s decision to participate in screening. Among these strategies, automatic and interactive telephone calls are considered to be potentially cost-effective, practical, and feasible tools.22
Nevertheless, it is not known whether telephone calls and short message services (SMS) are effective at increasing adherence for a sustained period of follow-up, which requires a robust prospective trial. Also, most studies targeted CRC screening participants who were overdue for screening, lending little evidence about those who had previously been adherent to the programme. FIT has been one of the most common screening tests employed for population-based screening, particularly in resource-deprived regions where colonoscopy capacity is limited. Although the authors have previously performed a study comparing the effectiveness of telephone and SMS on adherence to CRC screening, the observation of that trial was limited to 1 year.23 The authors aimed to evaluate the effectiveness of delivering interactive telephone reminders versus SMS messages for improving persistent adherence to FIT screening when compared with usual care. They also examined the effect modifiers of persistent adherence.
How this fits in
Few studies have performed head-to-head comparisons of the various telecommunication strategies for enhancing adherence to faecal immunochemical test (FIT)-based screening in people who have had a previous negative test result. This randomised controlled trial compared the impact of interactive telephone reminders, short message services (SMS), and usual care. The authors found that individuals in the telephone group were significantly more likely than controls to collect FIT tubes and return completed FIT specimens 6 months after their expected return. Practices may consider adopting telephone reminders in FIT-based screening programmes to increase programme effectiveness.
METHOD
Study design
This was a prospective, randomised, parallel group study, the setting of which has been previously described.23–25 To summarise, a community screening centre invited asymptomatic individuals aged >40 years for free CRC screening in Hong Kong through territory-wide media invitations. The eligibility criteria in the first screening round in 2015 included the absence of: self-reported CRC symptoms, any CRC screening tests in the past 5 years, a personal history of colorectal neoplasia or inflammatory bowel disease, and contraindications for colonoscopy. At the time of the present study, there had been no organised, subsidised screening service offered by the government. CRC screening remains opportunistic, and there are no incentives, or particular roles played by primary care. International authorities, including the updated Asia Pacific recommendations, propose that people aged 50–75 years undergo yearly FIT screening,2 and this was the reason for the existing programme of yearly screening, which was subsidised by a charitable body.
During visits to the screening practice, each eligible participant completed a self-administered questionnaire on their sociodemographics and clinical history. For the first round of screening, subjects were offered one FIT tube to perform in the same month as their study participation. On study enrolment in 2015, all participants were reminded to return for repeat FIT in the same month of 2016 if their FIT result was negative.
Participant selection
The authors selected subjects who had negative FIT results in their first screening round, from April to September 2015. Subjects who had medical conditions rendering them unable to understand telephone or SMS messages, or who had no mobile phone, were excluded.
Intervention groups
A simple random sampling process was administered using computer-generated numbers, with an allocation ratio of 1:1:1. The usual-care group consisted of subjects whose FIT result was negative in 2015 and who were reminded in the same year to repeat the test by revisiting the centre in 2016 for collection of FIT tubes. They did not receive any additional reminders before the expected dates of return. In the SMS group, participants received a one-way SMS message, sent from the centre to their mobile phone. A generic message about the importance of regular CRC screening, and the time and venue of FIT tube retrieval, was used. In the telephone group, subjects received an interactive telephone call from healthcare professionals at the screening centre with the message content identical to that delivered by SMS, except that the screening participants were able to have a conversation with the healthcare professionals. The healthcare professionals are public health practitioners trained by experienced family physicians and epidemiologists on the accurate expression of the reminder messages and responses to common enquiries made by participants. Up to three telephone calls were made for each participant and, if there was still no response, a voicemail was left. The telephone calls and SMS messages were delivered during office hours 1 month prior to the expected date of participant return. Each telephone call took approximately 5 minutes, delivered by personnel who charged an hourly rate of US$15.
All eligible participants who did not return to the centre in the same calendar month of 2016 as in the previous year received a telephone call 2 months after their expected return, inviting their attendance at the centre. For example, a subject who had negative FIT results in April 2015 was expected to return to the centre for repeat testing in April 2016. If they had not returned by the end of May 2016, a reminder telephone call was made in early June 2016. This is a routine service to ensure a proper duty of care has been delivered to the screening participants who defaulted the programme. Thus, additional telephone reminders were delivered 2 months after the expected return date to subjects in all groups who defaulted specimen return.
Outcome measures
The primary outcomes included FIT collection rate, defined as the proportion of subjects who returned to the centre to collect FIT tubes in the same calendar month of the second year as in the first year of the screening test, and rate of FIT specimen return, defined as the proportion of subjects who successfully returned the completed FIT specimen. The denominators of both outcomes were the total number of analysable subjects in each group. A grace period of 6 months was offered to all subjects to study the sustained impact of the interventions. For example, a subject who was expected to return the FIT specimen to the centre in April 2016, but instead returned the completed specimen on or before 30 October 2016, was considered a ‘successful specimen return’. The outcome variables were measured 6 months after their expected return date. There were no changes to methods or trial outcome after the trial commenced.
Sample size
The minimum sample size required was 600, with 200 subjects in each of the three groups. A power calculation indicates that a sample of 200 participants in each group would provide 80% power (at the 5% level) to detect an increase of 11% in the interactive phone call and automated SMS message groups, versus no increase in the control group, which is assumed to have a baseline return rate of FIT specimens of approximately 70%. This is supported by results from the authors’ prospective cohort study on persistent adherence with yearly FIT screening programme in the same setting.26
Data analysis
The baseline characteristics of the three groups were presented. The associations between the study groups and the outcome variables were examined by backward stepwise, binary logistic regression analyses. The covariates included age, sex, marital status, household income, and educational level, while the control group was used as the reference group. Subgroup analysis according to these covariates was performed, because previous studies identified these variables as potential effect modifiers.5 In addition, the authors performed two separate binary logistic regression analyses to explore the possible effect modifiers. P<0.05 was interpreted as statistically significant.
RESULTS
Recruitment and characteristics of study participants
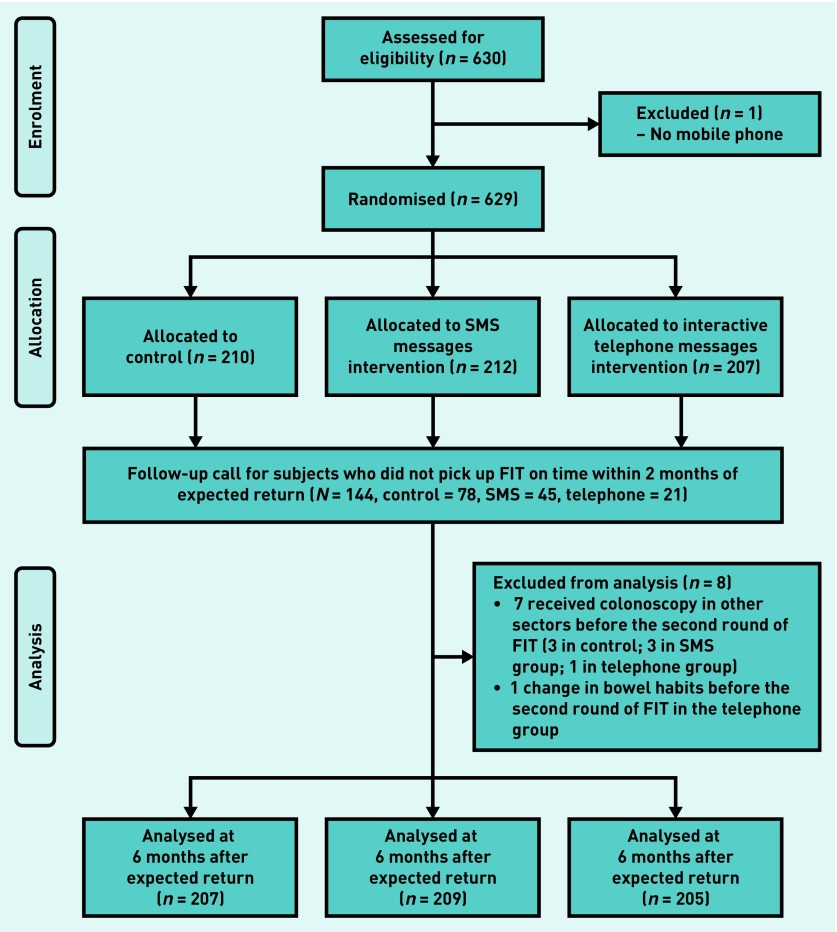
A total of 630 subjects joined the screening programme from April to September 2015. One subject did not have a mobile phone and was not eligible, and all participants were able to understand SMS message and telephone reminders. Among them, 210, 212, and 207 subjects were randomised into the control, SMS, and interactive telephone groups, respectively (Figure 1). Of 212 subjects in the SMS group, text messages were successfully delivered to 190 participants (89.6%), and all read the SMS messages. Of 207 subjects in the telephone group, 191 (92.3%) received the interactive phone calls within three telephone attempts, and 11 subjects (5.3%) did not respond to telephone calls but listened to the voice message left after three failed telephone contact attempts. Five subjects (2.4%) could not be contacted via phone. The average age of the study participants was 57.5 years, and 63.4% were male (Table 1). Prior to the 2-month reminders, the respective FIT collection rate was 62.3%, 78.5%, and 89.8% for subjects in the control, SMS, and telephone groups, respectively. The corresponding proportions for the rate of FIT return were 69.1%, 82.8%, and 91.2%, respectively.23
Figure 1.
Flow diagram of subject recruitment. FIT = faecal immunochemical test.
Table 1.
Baseline characteristics of study participants in the first screening round
| SMS, n= 212 (%) | Telephone, n= 207 (%) | Control, n= 210 (%) | |
|---|---|---|---|
| FIT positivity ratea | 9/188 (4.8) | 11/193 (5.7) | 8/178 (4.5) |
|
| |||
| Age at baseline, mean (SD) | 57.2 (7.0) | 57.5 (6.9) | 57.8 (7.1) |
|
| |||
| Male | 132 (62.3) | 127 (61.4) | 140 (66.7) |
|
| |||
| Educational level | |||
| Primary or below | 47 (22.2) | 35 (16.9) | 43 (20.5) |
| Secondary | 131 (61.8) | 134 (64.7) | 138 (65.7) |
| Tertiary or above | 34 (16.0) | 38 (18.4) | 29 (13.8) |
|
| |||
| Monthly household income | |||
| ≤HK$10 000, or not reported | 70 (33.0) | 64 (30.9) | 77 (36.7) |
| HK$10 001–HK$20 000 | 83 (39.2) | 77 (37.2) | 78 (37.1) |
| >HK$20 000 | 59 (27.8) | 66 (31.9) | 55 (26.2) |
|
| |||
| Work status | |||
| Unemployed/retired/housewife | 103 (48.6) | 97 (46.9) | 105 (50.0) |
| Part-time | 29 (13.7) | 22 (10.6) | 23 (11.0) |
| Full-time | 80 (37.7) | 88 (42.5) | 82 (39.0) |
|
| |||
| Marital status | |||
| Married | 169 (79.7) | 159 (76.8) | 164 (78.1) |
| Other | 43 (20.3) | 48 (23.2) | 46 (21.9) |
|
| |||
| Weight, kg, mean (SD) | 64.3 (10.8) | 65.3 (11.5) | 65.3 (11.2) |
|
| |||
| Height, cm, mean (SD) | 164.4 (8.3) | 164.4 (8.0) | 164.9 (8.0) |
|
| |||
| BMI, mean (SD) | 23.8 (3.4) | 24.1 (3.2) | 23.9 (3.1) |
|
| |||
| Waist circumference, cm, mean (SD) | 82.4 (9.7) | 82.9 (10.3) | 82.8 (9.7) |
|
| |||
| Family history of CRC in a FDR | 124 (58.5) | 118 (57.0) | 121 (57.6) |
|
| |||
| Asia Pacific Colorectal Screening (APCS) score | |||
| Average/moderate risk | 28 (13.2) | 20 (9.7) | 20 (9.5) |
| High risk | 184 (86.8) | 187 (90.3) | 190 (90.5) |
|
| |||
| Smoking status | |||
| Current | 39 (18.4) | 37 (17.9) | 37 (17.6) |
| Never | 108 (50.9) | 99 (47.8) | 98 (46.7) |
| Past | 65 (30.7) | 71 (34.3) | 75 (35.7) |
|
| |||
| Alcohol drinker | 42 (19.8) | 45 (21.7) | 51 (24.3) |
|
| |||
| Comorbidities | |||
| Diabetes | 19 (9.0) | 25 (12.1) | 21 (10.0) |
| Fatty liver | 17 (8.0) | 8 (3.9) | 13 (6.2) |
| Obesity (BMI ≥25) | 74 (34.9) | 74 (35.7) | 80 (38.1) |
| Hypertension | 57 (26.9) | 59 (28.5) | 45 (21.4) |
| Heart disease | 1 (0.5) | 1 (0.5) | 1 (0.5) |
| Chronic lung disease | 2 (0.9) | 3 (1.4) | 0 (0) |
| Stroke | 0 (0) | 1 (0.5) | 3 (1.4) |
| Gastro-oesophageal reflux disease | 16 (7.5) | 19 (9.2) | 23 (11.0) |
| Other | 35 (16.5) | 41 (19.8) | 49 (23.3) |
|
| |||
| Use of medications | |||
| NSAIDs | 14 (6.6) | 11 (5.3) | 11 (5.2) |
| Calcium supplements | 25 (11.8) | 30 (14.5) | 30 (9.5) |
| Folate supplements | 8 (3.8) | 6 (2.9) | 3 (1.4) |
| Statins | 32 (15.1) | 35 (16.9) | 29 (13.8) |
| Gastroprotective agents | 11 (5.2) | 13 (6.3) | 12 (5.7) |
| Steroids or immunosuppressants | 2 (0.9) | 2 (1.0) | 2 (1.0) |
FIT positivity rate was calculated among those who returned completed FIT samples. BMI = body mass index. CRC = colorectal cancer. FDR = first-degree relative. FIT = faecal immunochemical test. NSAIDs = non-steroidal anti-inflammatory drugs. SD = standard deviation. SMS = short message service.
At 2 months after their expected return, 78, 45, and 21 extra telephone calls were made to the subjects who did not return to the centre in the control, SMS, and telephone groups, respectively. After excluding three, three, and two subjects, respectively, who were not eligible for the second round of FIT screening (Figure 1), there were 28, 20, and 10 subjects in the corresponding three groups who did not return to the centre for FIT collection at 6 months. Hence the yield of the extra telephone reminder was 47 (59.6%), 22 (48.9%), and nine (42.9%) subjects, respectively.
Cost of the intervention strategies
The total cost incurred for the telephone group was US$375, with an average of 1.45 calls made per person. For the SMS group, the total cost was US$8.03, with an average of one message sent per person. Therefore, the study cost required to engage one additional person to screen subjects was US$1.81, as compared with the cost in the literature (US$40 per additional member of staff).
Effectiveness of intervention on adherence rates
The rate of FIT collection within the scheduled month was 86.5%, 90.4%, and 95.1% for the control, SMS, and telephone groups, respectively (P = 0.010). The corresponding specimen return rate within 6 months of the scheduled return date was 86.0%, 90.0%, and 94.1% (P = 0.022). When compared with the control group, the collection rate was significantly higher in the telephone group (adjusted odds ratio [AOR] 3.18, 95% confidence interval [CI] = 1.50 to 6.75, P = 0.003, Table 2). Similarly, the return rate of completed FIT specimens was also higher in the telephone group (AOR 2.73, 95% CI = 1.35 to 5.53, P = 0.005) compared with the control group. All subjects with positive FIT subsequently attended an appointment arranged for diagnostic colonoscopies.
Table 2.
The effectiveness of telephone reminders and short message service (SMS) on rate of faecal test collection and return, within 6 months of their expected returna
| FIT collection | FIT return | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N b | n /%b | AD | NNT | 95% CI | AOR | 95% CI | P-value | n /% b | AD | NNT | 95% CI | AOR | 95% CI | P-value | |
| No reminders | 207 | 179/86.5 | – | – | – | 1.0 | Reference | – | 178/86.0 | – | – | – | 1.0 | Reference | – |
| SMS group | 209 | 189/90.4 | 3.9% | 25 | 24 to 27 | 1.53 | 0.83 to 2.83 | 0.173 | 188/90.0 | 4.0% | 25 | 24.0 to 27.1 | 1.51 | 0.83 to 27.6 | 0.179 |
| Telephone group | 205 | 195/95.1 | 8.6% | 12 | 11 to 12 | 3.18 | 1.50 to 6.75 | 0.003 | 193/94.1 | 8.1% | 12 | 12 to 13 | 2.73 | 1.35 to 5.53 | 0.005 |
AOR was controlled for age, sex, marital status, household income, and educational level. In the SMS group, only one SMS message highlighting the importance of compliance with FIT screening and the expected date of re-attendance was delivered. In the telephone group, a message similar to that of SMS was delivered via an interactive telephone conversation between the study participant and the healthcare providers.
N represents the total number of analysable subjects. n/% denotes the number and proportion of subjects, respectively, who attended for FIT collection and returned completed FIT specimens. AD = absolute difference compared with the first group. AOR = adjusted odds ratio. CI = confidence interval. FIT = faecal immunochemical test. NNT = number needed to treat.
Reasons for non-response
All subjects who did not collect the FIT tubes or return the faecal specimens at 6 months were contacted by telephone (Table 3). The major reasons included a loss of interest in continued screening (43.1%) (for example, because of a perception that the incremental benefits conferred by screening were minimal given a previous negative screening, or a perception of the futility of being re-screened), being busy at the expected time of return (31.0%), and having forgotten to return to the centre (24.2%).
Table 3.
Reasons for not collecting FIT tubes 6 months within the expected return
| Reason | No collection of FIT tubes 6 months within the expected month, n (%) | |||
|---|---|---|---|---|
| Control (n= 28) | SMS (n= 20) | Telephone (n= 10) | All subjects (n= 58) | |
| Not interested to continue | 13 (46.4) | 9 (45.0) | 3 (30.0) | 25 (43.1) |
| Busy | 7 (25.0) | 5 (25.0) | 6 (60.0) | 18 (31.0) |
| Forgotten | 8 (28.6) | 5 (25.0) | 1 (10.0) | 14 (24.2) |
| Refuse to disclose | 0 (0) | 1 (5.0) | 0 (0) | 1 (1.7) |
FIT = faecal immunochemical test. SMS = short message service.
Variation was observed in reasons for non-response among groups. ‘Forgotten’ was stated more frequently by subjects in the control (28.6%) and SMS (25.0%) arms, while being ‘busy’ was more commonly reported in the telephone arm (60.0%). Likewise, a lower proportion of subjects reported that they were ‘not interested to continue’ in the telephone arm (30.0%), with higher levels in the control (46.4%) and SMS (45.0%) groups.
Subgroup analysis
Subgroup analysis was performed by stratifying subjects according to sex, educational level (primary versus secondary or above), median household income (≤HK$10 000 versus >HK$10 000), and marital status (married versus others). It was found that the higher adjusted odds of participants in the telephone group remained significant in these subgroups.
Effect modifiers of the outcomes
Sex was found to be an effect modifier for FIT collection (male versus female: 92.4% versus 87.6%, AOR 2.96, 95% CI = 1.13 to 7.75, P = 0.027) and FIT specimen return (male versus female: 91.9% versus 86.7%, AOR 3.68, 95% CI = 1.40 to 9.71, P = 0.008). Smoking status was also found to be an effect modifier (Table 4).
Table 4.
Factors associated with collection of FIT tube and return of completed FIT specimens within 6 months of expected pickup or returna
| Nb (%) | FIT collection | FIT return | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| n | % | AOR (95% CI) | P-value | n | % | AOR (95% CI) | P-value | ||
| Sex | |||||||||
| Female | 225 (36.2) | 197 | 87.6 | 1.0 (Reference) | 195 | 86.7 | 1.0 (Reference) | ||
| Male | 396 (63.8) | 366 | 92.4 | 2.96 (1.13 to 7.75) | 0.027 | 364 | 91.9 | 3.68 (1.40 to 9.71) | 0.008 |
|
| |||||||||
| Smoking status | |||||||||
| Current | 115 (18.5) | 96 | 83.5 | 1.0 (Reference) | <0.001 | 95 | 82.6 | 1.0 (Reference) | <0.001 |
| Never | 295 (47.5) | 265 | 89.8 | 4.09 (1.47 to 11.34) | 264 | 89.5 | 5.04 (1.79 to 14.19) | ||
| Past | 211 (34.0) | 202 | 95.7 | 4.63 (2.01 to 10.65) | 200 | 94.8 | 4.04 (1.85 to 8.84) | ||
Age, sex, educational level, household income, work status, marital status, BMI, family history of colorectal cancer, smoking, alcohol, intervention group, and number of comorbidities were covariate in the regression model. Only significant variables were presented.
N represents the total number of analysable subjects. n denotes the number of subjects who attended for FIT collection and returned completed FIT specimens. AOR = adjusted odds ratio. BMI = body mass index. CI = confidence interval. FIT = faecal immunochemical test.
Age, educational level, household income, work status, marital status, body mass index (BMI), family history of CRC, alcohol drinking, and number of comorbidities were not significantly associated with the outcomes.
DISCUSSION
Summary
This randomised trial found that the use of interactive telephone messages was significantly more effective than no reminders at enhancing adherence to annual FIT-based CRC screening among subjects who were previously enrolled, as it conferred a 3.2 and 2.7-fold higher odds of FIT collection and FIT specimen return, respectively. These findings are robust when tested in different subgroups.
A study from Mandel et al 27 found that a faecal test could reduce CRC-related mortality by 33%, where 69% of all participants completed ≥75% of the planned tests; and, as was also found in a previous study,28 the adherence rates to FIT screening in the SMS (90.4%) and interactive telephone (95.1%) groups were much higher than the range achieved by Mandel et al, in which a faecal test was shown to decrease CRC mortality.
The authors of the present study also found that male participants and non-smokers or ex-smokers were effect modifiers to FIT tube collection and specimen return.
Strengths and limitations
This is the first study to compare two telecommunication reminder strategies that could enhance screening adherence in future population-based programmes. Nevertheless, there are several limitations that should be addressed. First, the trial was conducted in a single centre, and the subjects were almost exclusively ethnic Chinese. Therefore, its generalisability to other population groups needs to be further tested. In addition, the participants were observed for 18 months only, and follow-up of these subjects to assess the longer-term sustainability of these strategies is warranted. In Hong Kong, CRC screening is opportunistic, and an organised screening programme was not yet available at the time the participants joined the study. In underprivileged regions and screening practices, where participants did not commonly use mobile telephones, alternatives measures — such as the postal system as used in the UK — to enhance adherence will need to be further explored. Another important group of service recipients in the CRC screening programme includes individuals who do not opt for screening in the first place. These require more intensive investigations into the predisposing factors that enhance awareness and knowledge of the cancer and its screening, and into the perceptions and psychological factors that impede CRC screening, as well as exploration and acknowledgement of their health beliefs.3
Furthermore, this study included self-referred subjects who joined a free screening programme. The findings need to be interpreted with caution, as the results were gathered in opportunistic screening practices.
Finally, the study population was a highly selected group of previously adherent individuals. The mean age is relatively young, with a higher proportion of males than females, as compared with non-responders. The difference in response to screening according to age and sex is not clearly understood, and findings in existing literature are inconclusive in terms of determinants of screening. Future studies should evaluate the reasons for adherence in different population groups.
A vast majority of the study participants had valid mobile phones, which may be due to their common use in the area in which the study was conducted. Besides, all subjects understood SMS messages and telephone reminders. This is because screening participants who enrolled in the programme in year 1 were contacted via their mobile phones, and hence represented a selected group of subjects who could comprehend SMS and telephone messages well. In addition, the authors’ messages in both groups were designed and tailored to the local population, using the simplest language comprehensible by the general public.
It was also found that the yield from the extra telephone reminder was the highest for subjects in the control group, and lowest for subjects in the telephone group. This demonstrates the effectiveness of interactive telephone reminders among individuals who have not received any additional reminders, and shows that the add-on value of an extra telephone reminder among those who have already received a similar telephone call is modest.
Comparison with existing literature
Few studies have examined the impact of telephone reminders on CRC screening adherence. One study compared the effectiveness of a multifaceted intervention among 450 underserved subjects who had prior negative faecal test results, mostly Latinos in US community health centres.28 The intervention consists of a mailed reminder letter, a free FIT with low-literacy instructions, a postage-paid return envelope, an automated telephone and text reminder, and personal telephone outreach. The intervention achieved a FIT completion rate of 82.2% compared with the control group (37.3%).
Another study examined the influence of an interactive voice response to encourage CRC screening among subjects aged 50–81 years who were not adherent to screening, in a managed care organisation in the US.29 The rate of any CRC screening was slightly higher than that of the control group (16.6% versus 14.1%) at 12 months. Yet another trial in primary care practices in the US studied subjects aged ≥50 years with no personal or family history of CRC, and who were overdue for screening. They received health counselling involving a phone call from a trained interventionist, and the rate of any CRC screening was 2.2-fold (23.8% versus 11.8%) higher than that of the control group.30
There are several differences in subject characteristics between these trials and the present study. This study enrolled self-referred subjects who were already engaged in a CRC screening programme, a relatively novel health assessment programme in Hong Kong. The study participants were arguably more health conscious, and the programme is also free. In addition, these subjects may represent a highly selected group of screening participants who encountered no difficulties in terms of accessibility to the screening service, because they had successfully completed previous screening tests in the same centre. This explains the overall higher rates of adherence with the FIT-based programme in this study.
It is speculated that interactive telephone reminders are effective at reminding subjects who were not interested in continuing to participate in the screening programme, or who were forgetful of their scheduled screening appointments. In the current study, ‘not interested to continue’ was more commonly reported in subjects in the telephone group, suggesting that telephone reminders are effective at enhancing subjects’ interests in participation. The reminders also enable individuals to plan their attendance at their screening appointments.3 The intervention consists of a simple telephone conversation highlighting the importance of CRC screening, acting on the predisposing and reinforcing factor components of the PRECEDE-PROCEED model.21 Interactive telephone messages from healthcare practitioners delivered added advantages by offering a ‘personal reminder’ element that is absent from the SMS messages. This implies that screening participants might value a one-to-one conversation delivered by healthcare professionals who allow questions to be addressed directly via phone conversations.
From the literature,3 it is widely recognised that automated telephone calls were highly cost-effective (US$40 per additional member of staff employed to perform the screening). Therefore, telephone reminders may potentially represent an operationally feasible and practical approach to enhance screening adherence in clinical practice. Because most subjects who did not return FIT specimens had not collected FIT tubes in the first place, interventions that enhance collection rates represent important strategies.
Implications for research and practice
Practices may consider telephone-based strategies as a service component due to their sustained significant impact. The authors recommend further research to examine the impact of these strategies in other population groups and practice settings. The acceptability of various intervention strategies, and the satisfaction of study participants, could be further explored by a nested qualitative study. The feasibility and consistency of intervention strategies with a health prevention agenda should be evaluated in this population, similar to a previous study performed in Scottish general practices.31 Given that continuous adherence over repeated rounds of screening represents an important impact indicator, the effectiveness of these reminders on a longer-term adherence to FIT-based screening should be further evaluated.
Acknowledgments
The authors would like to thank the study participants for joining the screening programme.
Funding
Funding for the study was received from the Hong Kong Jockey Club Charities Trust (reference number: 2013/0018).
Ethical approval
This study was approved by the Clinical Research and Ethics Committee of the Chinese University of Hong Kong (protocol CREC 2016.023), which also waived consent from participants for inclusion in this study and randomisation into different groups.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Bibbins-Domingo K, Grossman DC, Curry SJ, et al. Screening for colorectal cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2016;315(23):2564–2575. doi: 10.1001/jama.2016.5989. [DOI] [PubMed] [Google Scholar]
- 2.Sung JJ, Ng SC, Chan FK, et al. An updated Asia Pacific Consensus Recommendations on colorectal cancer screening. Gut. 2015;64(1):121–132. doi: 10.1136/gutjnl-2013-306503. [DOI] [PubMed] [Google Scholar]
- 3.Senore C, Inadomi J, Segnan N, et al. Optimising colorectal cancer screening acceptance: a review. Gut. 2015;64(7):1158–1177. doi: 10.1136/gutjnl-2014-308081. [DOI] [PubMed] [Google Scholar]
- 4.Ries LA, Wingo PA, Miller DS, et al. The annual report to the nation on the status of cancer, 1973–1997, with a special section on colorectal cancer. Cancer. 2000;88(10):2398–2424. doi: 10.1002/(sici)1097-0142(20000515)88:10<2398::aid-cncr26>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 5.Power E, Miles A, von Wagner C, et al. Uptake of colorectal cancer screening: system, provider, and individual factors and strategies to improve participation. Future Oncol. 2009;5(9):1371–1388. doi: 10.2217/fon.09.134. [DOI] [PubMed] [Google Scholar]
- 6.Liss DT, Baker DW. Understanding current racial/ethnic disparities in colorectal cancer screening in the United States: the contribution of socioeconomic status and access to care. Am J Prev Med. 2014;46(3):228–236. doi: 10.1016/j.amepre.2013.10.023. [DOI] [PubMed] [Google Scholar]
- 7.Tinmouth J, Patel J, Austin PC, et al. Increasing participation in colorectal cancer screening: results from a cluster randomized trial of directly mailed gFOBT kits to previous non-responders. Int J Cancer. 2015;136(6):E697–E703. doi: 10.1002/ijc.29191. [DOI] [PubMed] [Google Scholar]
- 8.Van Roosbroeck S, Hoeck S, Van Hal G. Population-based screening for colorectal cancer using an immunochemical faecal occult blood test: a comparison of two invitation strategies. Cancer Epidemiol. 2012;36(5):e317–e324. doi: 10.1016/j.canep.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 9.Giorgi Rossi P, Grazzini G, Anti M, et al. Direct mailing of faecal occult blood tests for colorectal cancer screening: a randomized population study from Central Italy. J Med Screen. 2011;18(3):121–127. doi: 10.1258/jms.2011.011009. [DOI] [PubMed] [Google Scholar]
- 10.Federici A, Giorgi Rossi P, Bartolozzi F, et al. The role of GPs in increasing compliance to colorectal cancer screening: a randomised controlled trial (Italy). Cancer Causes Control. 2006;17(1):45–52. doi: 10.1007/s10552-005-0380-9. [DOI] [PubMed] [Google Scholar]
- 11.Segnan N, Senore C, Andreoni B, et al. Randomized trial of different screening strategies for colorectal cancer: patient response and detection rates. J Natl Cancer Inst. 2005;97(5):347–357. doi: 10.1093/jnci/dji050. [DOI] [PubMed] [Google Scholar]
- 12.Senore C, Ederle A, DePretis G, et al. Invitation strategies for colorectal cancer screening programmes: the impact of an advance notification letter. Prev Med. 2015;73:106–111. doi: 10.1016/j.ypmed.2015.01.005. [DOI] [PubMed] [Google Scholar]
- 13.Libby G, Bray J, Champion J, et al. Pre-notification increases uptake of colorectal cancer screening in all demographic groups: a randomized controlled trial. J Med Screen. 2011;18(1):24–29. doi: 10.1258/jms.2011.011002. [DOI] [PubMed] [Google Scholar]
- 14.van Roon AH, Hol L, Wilschut JA, et al. Advance notification letters increase adherence in colorectal cancer screening: a population-based randomized trial. Prev Med. 2011;52(6):448–451. doi: 10.1016/j.ypmed.2011.01.032. [DOI] [PubMed] [Google Scholar]
- 15.Lo SH, Good A, Sheeran P, et al. Preformulated implementation intentions to promote colorectal cancer screening: a cluster-randomized trial. Health Psychol. 2014;33(9):998–1002. doi: 10.1037/a0033507. [DOI] [PubMed] [Google Scholar]
- 16.Denters MJ, Deutekom M, Bossuyt PM, et al. A feces collection paper does not enhance participation in a fecal immunochemical test-based colorectal cancer screening program: randomized clinical trial. Eur J Cancer Prev. 2013;22(4):299–304. doi: 10.1097/CEJ.0b013e32835b3882. [DOI] [PubMed] [Google Scholar]
- 17.Hewitson P, Ward AM, Heneghan C, et al. Primary care endorsement letter and a patient leaflet to improve participation in colorectal cancer screening: results of a factorial randomised trial. Br J Cancer. 2011;105(4):475–480. doi: 10.1038/bjc.2011.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cole SR, Smith A, Wilson C, et al. An advance notification letter increases participation in colorectal cancer screening. J Med Screen. 2007;14(2):73–75. doi: 10.1258/096914107781261927. [DOI] [PubMed] [Google Scholar]
- 19.Wardle J, Williamson S, McCaffery K, et al. Increasing attendance at colorectal cancer screening: testing the efficacy of a mailed, psychoeducational intervention in a community sample of older adults. Health Psychol. 2003;22(1):99–105. doi: 10.1037//0278-6133.22.1.99. [DOI] [PubMed] [Google Scholar]
- 20.Cole SR, Young GP, Byrne D, et al. Participation in screening for colorectal cancer based on a faecal occult blood test is improved by endorsement by the primary care practitioner. J Med Screen. 2002;9(4):147–152. doi: 10.1136/jms.9.4.147. [DOI] [PubMed] [Google Scholar]
- 21.Green LW, Kreuter MW, editors. Ecological and educational diagnosis Health program planning: an educational and ecological approach. 4th edn. New York, NY: McGraw-Hill Higher Education; 2005. [Google Scholar]
- 22.Smith DH, Feldstein AC, Perrin N, et al. Automated telephone calls to enhance colorectal cancer screening: economic analysis. Am J Manag Care. 2012;18(11):691–699. [PMC free article] [PubMed] [Google Scholar]
- 23.Wong MC, Ching JY, Lam TY, et al. Association of interactive reminders and automated messages with persistent adherence to colorectal cancer screening — a randomized clinical trial. JAMA Oncol. 2017;3(9):1281–1283. doi: 10.1001/jamaoncol.2017.1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wong MC, Lam TY, Tsoi KK, et al. A validated tool to predict colorectal neoplasia and inform screening choice for asymptomatic subjects. Gut. 2014;63(7):1130–1136. doi: 10.1136/gutjnl-2013-305639. [DOI] [PubMed] [Google Scholar]
- 25.Wong MC, Lam TY, Tsoi KK, et al. Predictors of advanced colorectal neoplasia for colorectal cancer screening. Am J Prev Med. 2014;46(5):433–439. doi: 10.1016/j.amepre.2013.12.008. [DOI] [PubMed] [Google Scholar]
- 26.Wong MC, Ching JY, Lam TY, et al. Prospective cohort study of compliance with faecal immunochemical tests for colorectal cancer screening in Hong Kong. Prev Med. 2013;57(3):227–231. doi: 10.1016/j.ypmed.2013.05.017. [DOI] [PubMed] [Google Scholar]
- 27.Mandel JS, Church TR, Bond JH, et al. The effect of fecal occult-blood screening on the incidence of colorectal cancer. N Engl J Med. 2000;343(22):1603–1607. doi: 10.1056/NEJM200011303432203. [DOI] [PubMed] [Google Scholar]
- 28.Baker DW, Brown T, Buchanan DR, et al. Comparative effectiveness of a multifaceted intervention to improve adherence to annual colorectal cancer screening in community health centers: a randomized clinical trial. JAMA Intern Med. 2014;174(8):1235–1241. doi: 10.1001/jamainternmed.2014.2352. [DOI] [PubMed] [Google Scholar]
- 29.Cohen-Cline H, Wernli KJ, Bradford SC, et al. Use of interactive voice response to improve colorectal cancer screening. Med Care. 2014;52(6):496–499. doi: 10.1097/MLR.0000000000000116. [DOI] [PubMed] [Google Scholar]
- 30.Menon U, Belue R, Wahab S, et al. A randomized trial comparing the effect of two phone-based interventions on colorectal cancer screening adherence. Ann Behav Med. 2011;42(3):294–303. doi: 10.1007/s12160-011-9291-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Calanzani N, Cavers D, Vojt G, et al. Is an opportunistic primary care-based intervention for non-responders to bowel screening feasible and acceptable? A mixed-methods feasibility study in Scotland. BMJ Open. 2017;7(10):e016307. doi: 10.1136/bmjopen-2017-016307. [DOI] [PMC free article] [PubMed] [Google Scholar]