Abstract
Background
Hospital stays for patients discharged to post-acute care are longer and more costly than routine discharges. Issues disrupting patient flow from hospital to post-acute care facilities are an underrecognized strain on hospital resources. We sought to quantify the burden of medically unnecessary hospital days for inpatients with neurologic illness and planned discharge to post-acute care facilities.
Methods
We conducted a retrospective evaluation of hospital discharge delays for patients with neurologic disease and plans for discharge to post-acute care. We identified 100 sequential hospital admissions to an academic neurology inpatient service that were medically ready for discharge from December 4, 2017, to January 25, 2018. For each patient, we quantified the number of medically unnecessary hospital days, or all days in the hospital following the determination of medical discharge readiness.
Results
Among 100 patients medically ready for discharge with plans for post-acute care disposition (47 female, mean age 72.5 years, mean length of stay 12.3 days), 50 patients were planned for discharge to skilled nursing, 37 to acute rehabilitation, 10 to hospice/palliative care, and 3 to other facilities. There was a total of 1,226 patient-days, and 480 patient-days (39%) occurred following medical readiness for discharge. Medically unnecessary days ranged from 0 to 80 days per patient (mean 4.8, median 2.5, interquartile range 1–5 days).
Conclusion
Unnecessary hospital days represent a large burden for patients with neurologic illness requiring post-acute care on discharge. These discharge delays present an opportunity to improve hospital-wide patient flow.
Discharge to post-acute care is common for patients following hospitalization for neurologic disease. Over one-third of US stroke inpatients are discharged to post-acute care facilities including acute rehabilitation, skilled nursing, and long-term care facilities.1 Patients recovering from neurologic disease who require an inpatient stay, such as those with traumatic brain injury,2 status epilepticus,3 or multiple sclerosis,4 may have similar post-acute care needs to support recovery, improve functional status, or manage chronic illness.
The need for post-acute care is increasing. In 2014, neurologic conditions comprised 13% of Medicare cases within inpatient rehabilitation facilities compared to 5% in 2004.5 Medicare spending on post-acute care facility payments doubled from $20.3 to $41.3 billion from 2001 to 2014,5 and considerably contributes to regional variation in spending.6 The rapid growth and high variability of post-acute care utilization has resulted in an increasingly regulated insurance market for these services,7 including separately bundled skilled nursing facility payments. These policies have the potential to create more selective post-acute care facilities.
Regionalization of neurologic care in the prehospital setting has received considerable attention,8 particularly given the expansion of neurocritical and acute care services.9 Less attention has been paid to post-acute care and discharge patient flow. Hospital stays with discharge to post-acute care are longer and more costly than routine discharges (7.0 vs 3.6 days; $16,900 vs $8,300 on average in 2013).1 While the reasons for these extended stays and increased costs are in part related to more complex medical illness, a portion of hospital stays for these patients may be due to difficulties in facility placement, unrelated to medical illness.10,11
The Institute for Healthcare Improvement characterizes hospital-wide patient flow as providing “the right care, in the right place, at the right time.”12 Hospital discharge planning, with careful consideration of insurance payers and patient eligibility, largely determines to which post-acute care facility a patient is discharged.13 Post-acute care decisions are further driven by the availability of specific settings, convenience to the patient/family, and financial incentives that are not always aligned with clinical needs or cost-effectiveness.7 The complexity encountered when navigating post-acute care facility discharges may lead to delays and disruption in patient flow. The recent Institute for Healthcare Improvement's white paper on achieving patient flow recommends advance planning, coordination, and development of partnerships with skilled nursing and rehabilitation facilities.12 However, in practice, coordination between acute and post-acute care facilities is poor.14
We sought to determine the modern-day burden of medically unnecessary hospital days for inpatients with neurologic illness in our institution, with focus on patients with planned discharge to a post-acute care facility.
Methods
We conducted a retrospective evaluation of hospital discharge delays for patients admitted to an academic neurology inpatient service with plans for discharge to a post-acute care facility (i.e., skilled nursing, long-term care, acute/inpatient rehabilitation, hospice/palliative care facility, medical group home) deemed medically ready for discharge between December 4, 2017, and January 25, 2018. The study objective was to quantify discharge delays, or the number of medically unnecessary hospital days, for patients with planned discharge to a post-acute care facility.
Standards protocol approvals, registrations, and patient consents
The University of Rochester Research Subjects Review Board approved the study with a waiver of patient consent.
Institution description
The study was performed at an 838-bed primary teaching hospital, designated a comprehensive stroke center, within an academic medical center (University of Rochester Medical Center). Our institution serves patients within an approximate 100-mile radius, and has a local post-acute care network including 2 institution-owned skilled nursing facilities (122 and 145 beds) within a 20-minute drive time, a 20-bed on-campus acute rehabilitation unit, formal relationships with 2 long-term care facilities (362 and 566 beds) within a 10-minute drive-time, and no long-term acute care facilities. In addition to in-network post-acute care facilities, our hospital coordinates with an additional 32 out-of-network rehabilitation and long-term care facilities within 25 miles of the hospital and many more at greater distances.
Patient selection
We examined inpatients admitted to the general or vascular neurology services deemed medically ready for discharge between December 4, 2017, and January 25, 2018. We selected 100 sequential patients deemed medically ready for discharge within the timeframe and with plans for discharge to a post-acute care facility at the time of medical readiness for discharge. Data for patients with a discharge plan for home were not collected for this study. Patients with a plan for discharge to a post-acute facility who were ultimately discharged home due to either improvement or barriers to facility placement were included (n = 10). Patients transferred to another inpatient service were excluded (hospital medicine; n = 2, neurosurgery; n = 2, vascular surgery; n = 1), unless the transfer was for the purpose of care on a dedicated inpatient rehabilitation unit or inpatient palliative care unit. Patient characteristics including demographics, clinical features (diagnosis, length of stay, comfort care status, disposition), and social factors (insurer, prehospital living arrangements, marital status, caregiver availability, primary income source) were extracted directly from the electronic medical record.
Outcome measures
We defined medically ready for discharge based on a set of criteria used by our neurology inpatient team (appendix, links.lww.com/CPJ/A37). These criteria were developed internally but are similar to those used previously.15,16 The classification of medical readiness for discharge was performed by the neurology service on a daily basis and recorded within the physician progress notes or handoff tool within the electronic medical record. Patients are deemed medically ready for discharge if all criteria are met and consensus agreement by the health care team is reached during a multidisciplinary patient review held each weekday morning. On the weekends, the senior resident under the supervision of the attending physician is responsible for reviewing and updating medical readiness for discharge.
Medically unnecessary days were defined as all patient-days spent in the hospital following the determination of medical readiness for discharge and were collected from a retrospective chart review. Days following the development of hospital-acquired complications were counted if the patient was already deemed medically ready for discharge prior to developing the complication. The admission date was defined as hospital day zero. Patient-days were considered equivalent to the number of midnights spent in the hospital.
Hospital-acquired complications were determined by chart review and included health care–associated infections and hospital-acquired delirium. For the purpose of this study, health care–associated infections were defined as any infection acquired while inpatient requiring antibiotics (e.g., pneumonia, urinary tract infection).17 Hospital-acquired delirium was identified as any cognitive disturbance not present on admission that occurred at least 24 hours following admission and prompted the use of restraints or administration of pharmacologic intervention (e.g., quetiapine or haloperidol). These complications were abstracted directly from daily progress notes.
Statistical analysis
Results were reported descriptively. A nonparametric Kruskal-Wallis test was used to assess differences in medically unnecessary days by patient variables. Statistical evaluation was completed using Stata version 14.2 (College Station, TX).
Data availability
Due to the potential for loss of patient confidentiality, complete individualized data cannot be made publicly available; however, anonymized data may be shared at the request of any qualified investigator.
Results
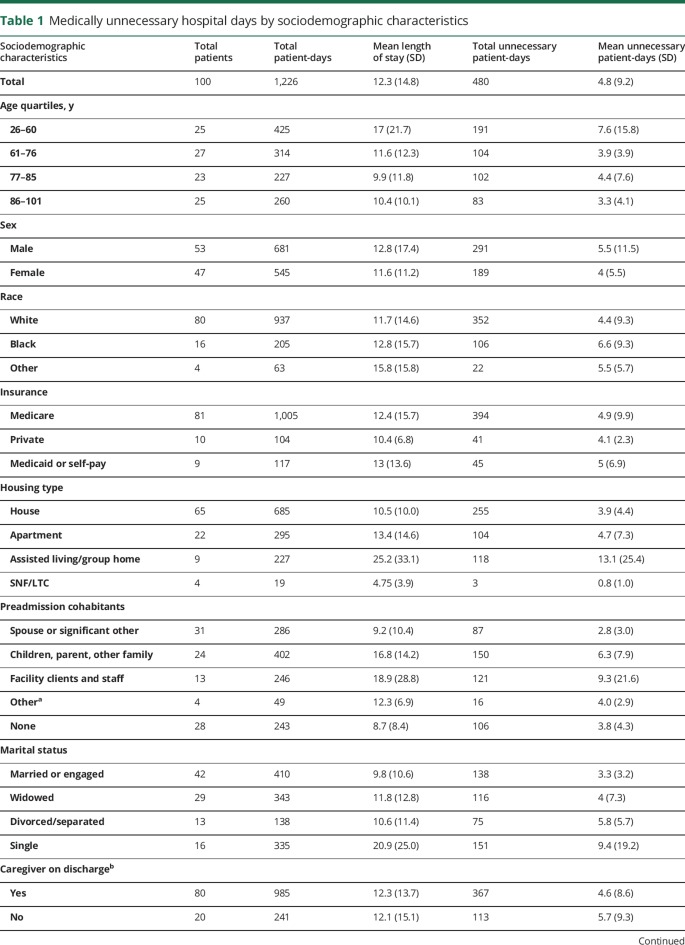
We identified 100 patients admitted to our acute care neurology services with mean age 73 years (SD 16.4) determined to be medically ready for discharge between December 4, 2017, and January 25, 2018, with plans for discharge to a post-acute care facility at the time of medical readiness for discharge. Most patients included in the study were male (n = 53), white (n = 80), and insured by Medicare (n = 81), with a primary source of income from social security retirement (n = 65) (table 1). Many patients included were married (n = 42), the majority lived in a house prior to admission (n = 65), and most lived with their spouse/significant other or family (n = 55). In total, 80 patients or their families were able to identify a caregiver who could assist the patient at least part time on discharge.
Table 1.
Medically unnecessary hospital days by sociodemographic characteristics
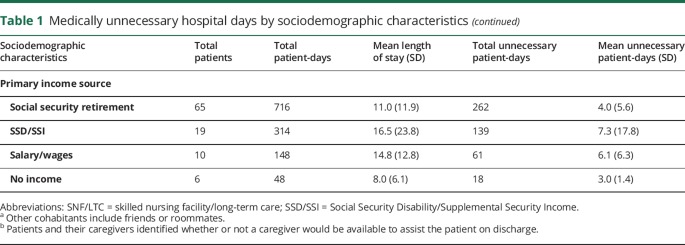
There were 65 patients with a diagnosis of ischemic stroke or intracerebral hemorrhage. Fifty were planned for discharge to skilled nursing, 37 to acute rehabilitation, and 10 to hospice/palliative care facility (table 2). Length of stay ranged from 1 to 106 days (mean 12.3, median 8, interquartile range [IQR] 4.5–12.5 days) and was greatest for nonstroke patients (mean 9.1 vs 18.2 days; p = 0.04). While awaiting placement, 5 patients developed hospital-acquired complications (urinary infection, n = 1; pneumonia, n = 2; delirium, n = 2) and 1 required intensive care services.
Table 2.
Medically unnecessary hospital days by clinical characteristics
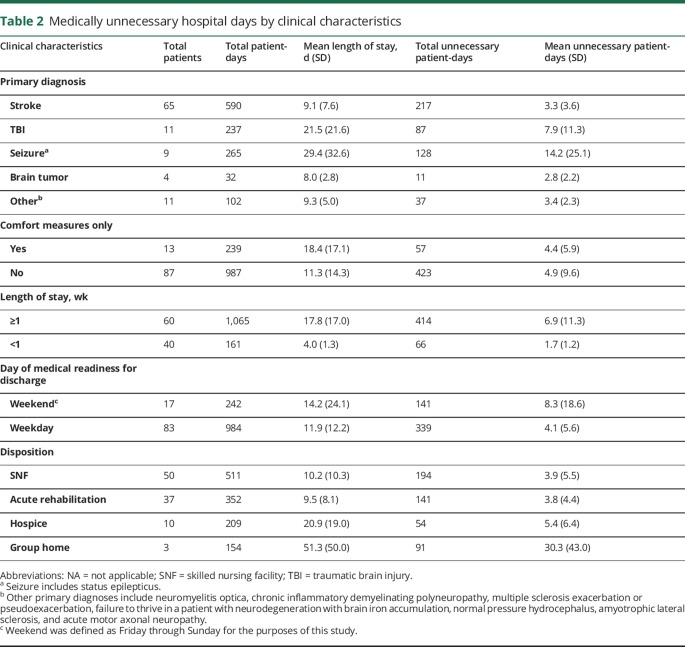
Medically unnecessary days by patient ranged from 0 to 80 days (mean 4.8, median 2.5, IQR 1–5 days) (figure 1). Race and insurance status were not associated with unnecessary hospital days. Medically unnecessary days were associated with medical readiness for discharge on the weekend (mean 8.3 vs 4.1 days; p = 0.05). Five patients who developed hospital-acquired complications had greater medically unnecessary days on average compared to those without complications (17.8 vs 7.6 days; p = 0.04). In addition, those ≤60 years of age had more unnecessary days compared to other patients (mean 7.6 vs 3.9 days; p = 0.04).
Figure 1. Distribution of neurology inpatients ordered by medically unnecessary patient-days.
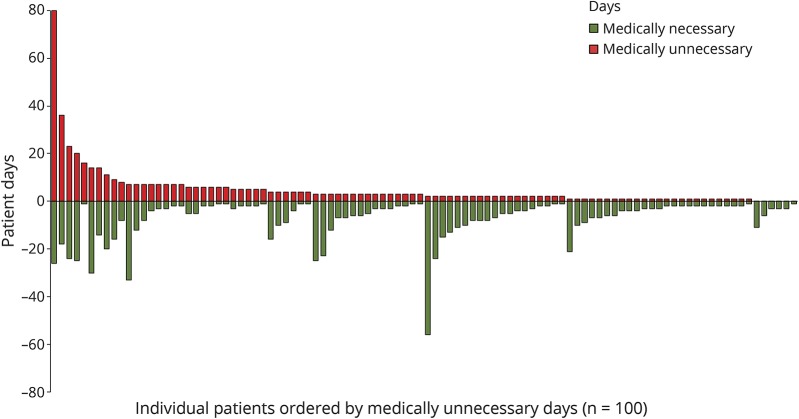
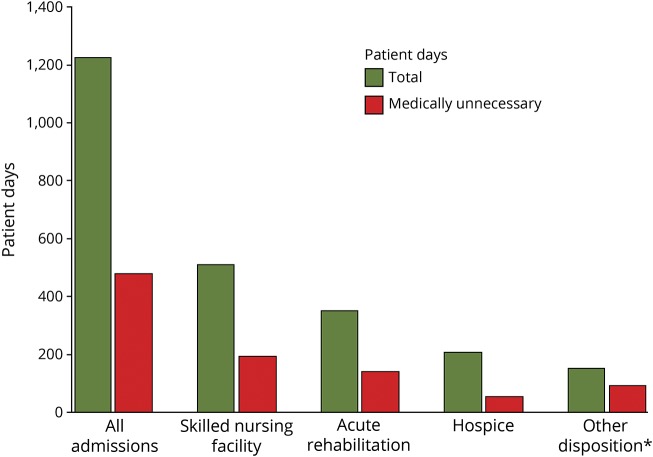
There was a cumulative 1,226 patient-days across all admissions examined in the study, and 480 patient-days (39% of total) occurred following medical readiness for discharge or were medically unnecessary. The proportion of patient-days that were medically unnecessary was similar for those discharged to skilled nursing, acute rehabilitation, and hospice/palliative care (figure 2). Two of 3 patients discharged to a group home had complex barriers to discharge related to longstanding developmental disabilities and therefore the number of medically unnecessary patient-days for this category was high (table 2). An analysis with these patients excluded demonstrated that unnecessary days still amounted to 36% of total hospital days in the study.
Figure 2. Total and medically unnecessary patient-days by planned discharge disposition.
*Two of 3 patients discharged to a group home had complex barriers to discharge related to longstanding developmental disabilities and therefore the proportion of medically unnecessary to total patient-days for this category was high (0.59 vs 0.36; p = 0.04). An analysis with these patients excluded demonstrated that unnecessary days still amounted to 36% of total hospital days in the study.
Discussion
Inpatient excess, which was over one-third of hospital days for those with planned discharge to post-acute care within our institution's data, can lead to hospital overflow and may propagate costs through unnecessary use of resources.18,19 The average cost of a hospital day in our institution was determined to be $1,047, but costs are reported as high as $2,456 per day for nonprofit hospitals in New York on average,20 and therefore medically unnecessary days have the potential to be costly. This may not encompass indirect costs of excess days (e.g., effect on upstream bed availability, patient satisfaction, provider burnout)21,22 and when generalized to all hospital services for the entire year, costs are likely even higher.
Periodic peaks in hospital capacity23 may lead to potential negative consequences for patients and the providers caring for them.24 Similarly, discharge delays may escalate hospital capacity, and subsequently strain physicians and staff, decreasing their efficiency and productivity. Overflow also has the potential to expose patients to a greater risk of adverse events and hospital-acquired complications, such as those seen within our institution's data.
Due to difficulties in identifying reasons for unnecessary hospital days within a retrospective review, causes for delays were unable to be described for most patients. However, causes of excess days that could be identified ranged from suboptimal post-acute care bed availability, application processing time for admission to post-acute care facilities, time for evaluation by post-acute care facilities, facility denial and reapplication to another facility, issues in financing medication costs (e.g., chemotherapy, multiple sclerosis disease-modifying therapy), insurance processing and approval, insurance denials, and obstacles related to guardianship status.25 Developing a better understanding and wider recognition of these issues is needed to improve patient flow and quality of care, and is an area in need of future research to improve quality of care.
The experiences with discharge delays for inpatients awaiting post-acute care is not new, nor is it an issue confined to our institution, or even the United States.26 Awaiting placement to a nursing facility has long been cited as an issue leading to discharge delays.10,11,26 However, none has focused on this burden exclusively in the post-acute care population. Furthermore, prior studies are outdated and took place in an era when length of stay was not commonly tracked as a metric for efficiency, and the value of patient flow was not fully realized.12 Our findings underscore the continued relevance of discharge delays for those destined for post-acute care and highlight the need to improve coordination between acute and post-acute care facilities.
A recent survey of health care quality improvement officers found more than half report that inpatient and post-acute care is only somewhat or not at all coordinated.14 Coordination in the acute to post-acute care continuum is in need of structure and organizational innovation to enhance patient flow and throughput.23 Therefore, opportunities exist to improve patient flow from acute to post-acute facilities, primarily at the level of the hospital and broader health care system.
Hospital partnership with post-acute care facilities holds the potential to ease referrals and increase accessibility of post-acute care beds.7 These arrangements may range from joint ventures to bed leasing to preferred referral networks.14,27 Such relationships may help with control over the quality of care within these facilities to promote accountability and good outcomes, allow for the integration of electronic health records, improve management of regional populations, and formulate contractual agreements that ensure streamlined transitions in care, which may include coverage of post-acute care services by insurance payers. These types of organizational interventions may ultimately decrease length of stay by reducing unnecessary hospital days14; however, overly narrow networks will need to be avoided to maintain optimal patient choice.28,29
While our study took place in a hospital with a post-acute care network, continued delays may be related to the limited network size, scope, and interfacility coordination with respect to the patient population, which has grown in recent years due to expansion of the acute care network. Our institution has formed a post-acute care committee with a neighboring affiliate hospital consisting of administration, faculty, staff, and trainees with the purpose of designing solutions that will address discharge delays for patients going to post-acute care facilities. Similar committees or efforts have been launched within other health care facilities and statewide organizations.30,31
In addition to hospital-level solutions, health system policies have the potential to incentivize organizations, including neuromedicine service lines, to enhance patient-centered care, focus on population health management, and develop longitudinal care teams and post-acute care networks that drive value-based care. This may include restructuring or expanding current bundled payment policies. For instance, the Centers for Medicare & Medicaid Services recently introduced new payment strategies that will bundle acute and post-acute care payments together for certain disease processes in hopes to improve care coordination across the continuum of hospital to post-acute care.32,33 A wider adoption of bundled payment policies that group acute and post-acute care payments may better align incentives to reduce unnecessary days. Developing other public policies to incentivize health care organizations to invest in service innovation and care coordination may also help to promote quality of care and patient flow from acute to post-acute facilities.34
It is uncertain how patient flow from acute to post-acute care will be influenced by the recently passed Improving Medicare Post-Acute Transformation (IMPACT) Act of 2014.35 The law attempts to create uniformed patient assessment methods for those within post-acute care facilities, and sets a timetable for developing, implementing, and reporting quality metrics.36 These reform efforts, while directed at improving quality, have the potential to make bed offers from post-acute care facilities even more selective, providing an even greater challenge for discharge delays. The law will further prepare for coming value-based payment reform by developing a prototype for a cross-setting, site-neutral prospective payment system for post-acute care (due for release in October 2021).36 Part of the initiative will be to evaluate the payment system's effect on post-acute care placement, which will be especially important for acute care facilities interested in optimizing hospital-wide patient flow.
Our study has important limitations. The study took place within a single large academic medical center, and others' institutional practices on patient flow and hospital discharge for patients departing to post-acute care may vary. The generalizability of these findings is unclear; however, prior studies from the 1990s of patients with neurologic disease and stroke within international facilities found similar discharge delays related to nursing home placement,10,11 and therefore, this problem is not new and unlikely to be confined to one region or locale. However, discharge practices may be influenced by resource availability and therefore discharge delays due to post-acute care facility placement may be regionally variable. For example, the upstate New York area is without long-term acute care hospitals, which creates barriers in discharging patients with ongoing complex care needs such as tracheostomy or mechanical ventilation. While we include some information on the availability of social support and living arrangements (table 2), this information is unlikely to fully elucidate the complex social situations that many patients and families encounter. In addition, our study takes place in a limited timeframe examining 100 sequential patients and therefore our study may be subject to variable peaks and latencies in inpatient census. It is partly reassuring that our neurology service census averages approximately 27 patients per day throughout the year and during the study timeframe the average census was 28 patients per day.
Finally, our definition of medical readiness for discharge was internally developed and subject to the judgement of the physician and health care team, and therefore, may not be generalizable to all hospital service lines or neurology inpatients within other facilities. Prior efforts have been made to assess appropriate stays on medical and surgical units16; however, many of these criteria would not be fitting for a modern-day neurology service. Although our criteria are generally consistent with those used previously,15,16 there is a clear need to develop more universally applied criteria for medical necessity and discharge preparedness for patients with neurologic illness, which could also facilitate a larger-scale epidemiologic examination of this problem.
Given the high utilization of post-acute care and potential for interrupted patient flow in discharge to post-acute care, more research is needed to identify the large-scale burden of these delays with attention to neurologic patients, who often utilize more acute care and have more disability on discharge than most patients. Furthermore, research is needed to monitor and develop the scale and success of post-acute care networks and the effect of acute to post-acute bundled payment policies on patient flow.
Acknowledgment
The authors thank Michelle Murphy (Neurology Nurse Manager, Department of Neurology, Strong Memorial Hospital, University of Rochester Medical Center), Dr. Carolyn Zyloney (Chief Neurology Resident, Department of Neurology, University of Rochester Medical Center), and Dr. Ross Hamilton (Chief Neurology Resident, Department of Neurology, University of Rochester Medical Center) for their assistance in data collection and reporting of medical readiness for discharge.
Footnotes
Editorial, page 281
Author contributions
Debra E. Roberts: study concept or design, acquisition of the data, drafting of the manuscript, critical revision for important intellectual content, interpretation of the analysis, study supervision and coordination. Robert G. Holloway: critical revision for important intellectual content, interpretation of the analysis. Benjamin P. George: study concept or design, acquisition of the data, drafting of the manuscript, critical revision for important intellectual content, statistical analyses, interpretation of the analysis.
Study funding
No targeted funding reported.
Disclosure
D.E. Roberts serves on a scientific advisory board for Cryothermic Systems. R.G. Holloway serves as a consultant for MCG, Inc. and receives research support from NIH (NCATS, NINDS). B.P. George reports no disclosures. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
References
- 1.Tian W. An all-payer view of hospital discharge to postacute care, 2013. 2016. Available at: ncbi.nlm.nih.gov/books/NBK373736/. Accessed January 21, 2018. [PubMed]
- 2.Sarajuuri JM, Kaipio ML, Koskinen SK, Niemela MR, Servo AR, Vilkki JS. Outcome of a comprehensive neurorehabilitation program for patients with traumatic brain injury. Arch Phys Med Rehabil 2005;86:2296–2302. [DOI] [PubMed] [Google Scholar]
- 3.Claassen J, Lokin JK, Fitzsimmons BF, Mendelsohn FA, Mayer SA. Predictors of functional disability and mortality after status epilepticus. Neurology 2002;58:139–142. [DOI] [PubMed] [Google Scholar]
- 4.Feigenson JS, Scheinberg L, Catalano M, et al. The cost-effectiveness of multiple sclerosis rehabilitation: a model. Neurology 1981;31:1316–1322. [DOI] [PubMed] [Google Scholar]
- 5.A data book: healthcare spending and the Medicare program. Available at: medpac.gov/-documents-/data-book. Accessed January 21, 2018.
- 6.Institute of Medicine Report. Variation in health care spending: target decision making, not geography [online]. Available at: nationalacademies.org/. Accessed February 25, 2017. [PubMed]
- 7.Buntin MB, Garten AD, Paddock S, Saliba D, Totten M, Escarce JJ. How much is postacute care use affected by its availability? Health Serv Res 2005;40:413–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.George BP, Doyle SJ, Albert GP, et al. Interfacility transfers for US ischemic stroke and TIA, 2006–2014. Neurology 2018;90:e1561–e1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Landro L. What the hospitals of the future look like [online]. Available at: wsj.com/articles/what-the-hospitals-of-the-future-look-like-1519614660. Accessed March 15, 2018.
- 10.Schluep M, Bogousslavsky J, Regli F, Tendon M, Prod'hom LS, Kleiber C. Justification of hospital days and epidemiology of discharge delays in a department of neurology. Neuroepidemiology 1994;13:40–49. [DOI] [PubMed] [Google Scholar]
- 11.van Straten A, van der Meulen JH, van den Bos GA, Limburg M. Length of hospital stay and discharge delays in stroke patients. Stroke 1997;28:137–140. [DOI] [PubMed] [Google Scholar]
- 12.Rutherford PA, Provost LP, Kotagal UR, Luther K, Anderson A. Achieving Hospital-Wide Patient Flow. IHI White Paper. Cambridge: Institute for Healthcare Improvement; 2017. [Google Scholar]
- 13.Blewett LA, Kane RL, Finch M. Hospital ownership of post-acute care: does it increase access to post-acute care services? Inquiry 1995;32:457–467. [PubMed] [Google Scholar]
- 14.Gittlen S. Survey snapshot: how to achieve post-acute care coordination [online]. Available at: catalyst.nejm.org/survey-post-acute-care-coordination/. Accessed January 31, 2018.
- 15.White CM, Statile AM, White DL, et al. Using quality improvement to optimise paediatric discharge efficiency. BMJ Qual Saf 2014;23:428–436. [DOI] [PubMed] [Google Scholar]
- 16.Gertman PM, Restuccia JD. The appropriateness evaluation protocol: a technique for assessing unnecessary days of hospital care. Med Care 1981;19:855–871. [PubMed] [Google Scholar]
- 17.Health People 2020: healthcare associated infections [online]. Available at: healthypeople.gov/2020/topics-objectives/topic/healthcare-associated-infections. Accessed April 9, 2018.
- 18.Wennberg JE, Freeman JL, Culp WJ. Are hospital services rationed in New Haven or over-utilised in Boston? Lancet 1987;1:1185–1189. [DOI] [PubMed] [Google Scholar]
- 19.Bazzoli GJ, Brewster LR, Liu G, Kuo S. Does US. Hospital capacity need to be expanded? Health Aff 2003;22:40–54. [DOI] [PubMed] [Google Scholar]
- 20.State health facts: hospital adjusted expenses per inpatient day by ownership, 2015 [online]. Available at: kff.org/health-costs/state-indicator/expenses-per-inpatient-day-by-ownership/. Accessed May 21, 2018.
- 21.Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc 2015;90:1600–1613. [DOI] [PubMed] [Google Scholar]
- 22.Tawfik DS, Phibbs CS, Sexton JB, et al. Factors associated with provider burnout in the NICU. Pediatrics 2017;139:e20164134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Litvak E, Bisognano M. More patients, less payment: increasing hospital efficiency in the aftermath of health reform. Health Aff 2011;30:76–80. [DOI] [PubMed] [Google Scholar]
- 24.Weissman JS, Rothschild JM, Bendavid E, et al. Hospital workload and adverse events. Med Care 2007;45:448–455. [DOI] [PubMed] [Google Scholar]
- 25.Chen JJ, Finn CT, Homa K, St Onge KP, Caller TA. Discharge delays for patients requiring in-hospital guardianship: a cohort analysis. J Healthc Qual 2016;38:235–242. [DOI] [PubMed] [Google Scholar]
- 26.McDonagh MS, Smith DH, Goddard M. Measuring appropriate use of acute beds: a systematic review of methods and results. Health Policy 2000;53:157–184. [DOI] [PubMed] [Google Scholar]
- 27.Inpatient & Beyond: The Post-Acute Care Conundrum. Charlotte: Premier, Inc.; 2016. [Google Scholar]
- 28.Castle NG. The nursing home compare report card: consumers' use and understanding. J Aging Soc Pol 2009;21:187–208. [DOI] [PubMed] [Google Scholar]
- 29.Schapira MM, Shea JA, Duey KA, Kleiman C, Werner RM. The nursing home compare report card: perceptions of residents and caregivers regarding quality ratings and nursing home choice. Health Serv Res 2016;51(suppl 2):1212–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.The Final Frontier: Ochsner's post-acute network development and optimization [online]. Available at: amga.org/Store/detail.aspx?id=WEB_013118_OCH. Accessed May 18, 2018.
- 31.Center for post-acute care [online]. Available at: calhospital.org/center-post-acute-care. Accessed May 21, 2018.
- 32.Ellimoottil C, Ryan AM, Hou H, Dupree J, Hallstrom B, Miller DC. Medicare's new bundled payment for joint replacement may penalize hospitals that treat medically complex patients. Health Aff 2016;35:1651–1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Matchar DB, Nguyen HV, Tian Y. Bundled payment and care of acute stroke: what does it take to make it work? Stroke 2015;46:1414–1421. [DOI] [PubMed] [Google Scholar]
- 34.Moses H III, Matheson DH, Cairns-Smith S, George BP, Palisch C, Dorsey ER. The anatomy of medical research: US and international comparisons. JAMA 2015;313:174–189. [DOI] [PubMed] [Google Scholar]
- 35.IMPACT Act of 2014 data standardization & cross setting measures [online]. Available at: cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-of-2014-Data-Standardization-and-Cross-Setting-Measures.html. Accessed May 1, 2018.
- 36.DeJong G. Coming to terms with the IMPACT Act of 2014. Am J Occup Ther 2016;70:7003090010p1–7003090010p6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to the potential for loss of patient confidentiality, complete individualized data cannot be made publicly available; however, anonymized data may be shared at the request of any qualified investigator.