Practical Implications
Consider epilepsy in the differential diagnosis of patients exhibiting arc de cercle as a main semiology. Peri-ictal symptoms are key in differentiating this sign from psychogenic nonepileptic seizures.
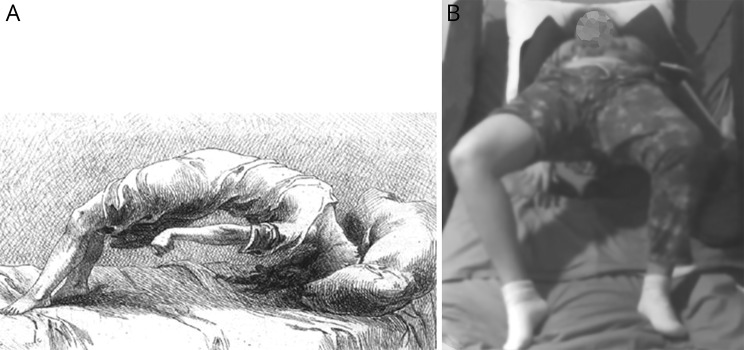
Since its description in 1885 in the Études cliniques sur l'hystéro-épilepsie ou grand hystérie by Raul Richer, the arc de cercle, or circular arc (figure 1A), has become synonymous of psychogenic nonepileptic seizures (PNES) and automatically interpreted as such by physicians. The development of extracranial and intracranial EEG recording has not confirmed the clinical importance of the arc de cercle.
Figure 1. Original drawing of the arc de cercle and patient during the arc de cercle.
(A) Original drawing of Raul Richer (in Études cliniques sur l'hystéro-épilepsie ou grand hystérie) depicts a female figure supported by her head and feet with total elevation of her legs, pelvis, and torso from the hospital bed. Her eyes are represented as closed and there is a dystonic posturing of the left arm. (B) Detailed examination of progression of motor symptoms on video-EEG is as follows: at the initiation of the movement, the patient’s back arches, her eyes close simultaneously with change of her lower facial expression with facial grimace. The face of the patient is not shown here for identity protection. She can grunt during the seizure or produce unintelligible sentences. The seizure ends with a dystonic posturing of the right arm and sometimes the right leg. See table for full description of the semiology of the seizures starting with the aura.
We describe a right-handed adolescent girl with medically refractory nonlesional left posterior insula/temporo-parietal operculum epilepsy who had arc de cercle as the main motor feature of her seizures. Her seizures began at age 12 years. She described a discomforting sensation in the back of her thigh that evolved into stiffening of the right leg and circular motion of the proximal aspect of the leg. Then the seizure quickly progressed into a violent posturing of the body consistent with the arc de cercle. She had full body elevation from the bed while her body was supported by the head and feet (figure 1B; see legend for detailed description of the motor features). Postictally, she had complete recollection of the event. These seizures frequently produced falls and often occurred out of sleep. At age 13 years, she underwent a subdural grid implantation that was followed by a dorsomedial resection of the left postcentral gyrus. Seizures relapsed at a higher frequency the day after the surgery. She also had multiple auras per day.
During noninvasive video EEG at our institution, EEG using a traditional bipolar longitudinal montage showed that ictal pattern began with a broad sharply contoured theta activity in the midline region. The rest of the EEG quickly was obscured by the muscle artifact. Analysis of the EEG in the transverse montage is shown in figure e-1 (links.lww.com/CPJ/A32). Seizure duration is 25–35 seconds and they cluster mainly during sleep. Seizure frequency is 10–15 seizures per day. Interictal sharp waves in the vertex and left centro-temporo-parietal region were more frequent postictally.
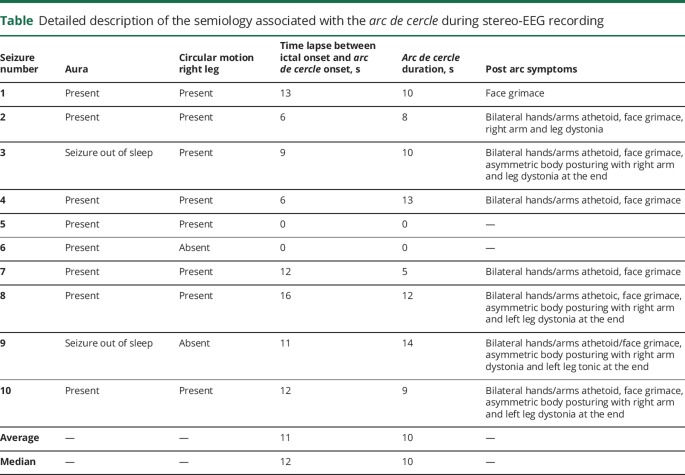
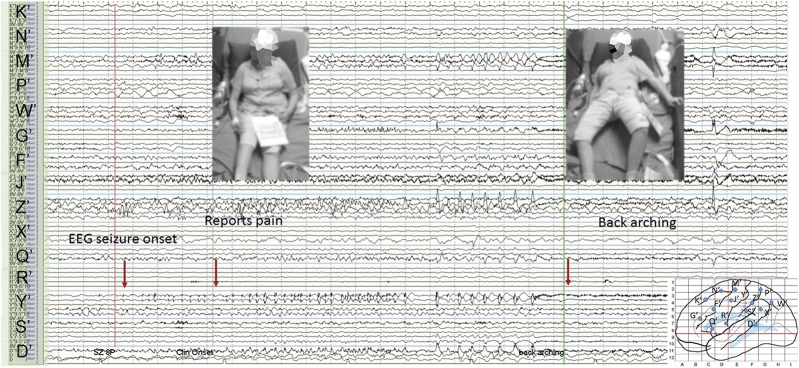
The patient underwent stereo-EEG (SEEG).1 The table has a summary of the ictal sequence of the seizures recorded on SEEG. Figure 2 shows the video and intracranial EEG findings. The aura of back leg sensation occurred at the time of the ictal onset in the left posterior insula (figure e-2, links.lww.com/CPJ/A32, left side). The arc de cercle appeared when the seizure propagated to the cingulate gyrus and paracentral lobule. Cortical stimulation of the cingulate or the posterior insula alone did not reproduce the arc de cercle.
Table.
Detailed description of the semiology associated with the arc de cercle during stereo-EEG recording
Figure 2. Ictal stereo-EEG (SEEG) recording during a typical seizure with aura and motor symptoms (arc de cercle).
The ictal onset of the seizures (aura of sensation in the back of the leg) correlated with rhythmic spikes localized to the left posterior insula (electrode Y′1–4) or a more widespread pattern involving mesial/dorsofrontal contacts (mesial D′, G′). Within 1–6 seconds, there was a sustained fast activity in the anterior/middle cingulate (mesial contacts G′ and Z′ electrodes) and dorsal precentral gyrus/paracentral lobule (mesial contacts J′ and M′). On SEEG, the arc de cercle symptom appeared when the seizure propagated from the posterior insula to the cingulate gyrus and paracentral lobule.
During an ictal SPECT injection at the time of the pelvic elevation, there was an activation of the posterior insula, cingulate gyrus, both paracentral lobules, basal ganglia, and cerebellum (figure e-2, links.lww.com/CPJ/A32, right side). Magnetoencephalography and PET were concordant with the epileptogenic zone localized by SEEG.
The patient did not undergo surgical resection of the posterior dominant insula because of the high risk for motor and language deficit.
This case documents that arc de cercle is an ictal epileptic symptom that seems to be produced by activation of an extensive motor network in the brain as suggested by the ictal SPECT and SEEG. Somatosensory and viscerosensory are the most common auras described in insular epilepsy.2,3 Motor semiology associated to seizures arising from the posterior insula region include hypomotor behaviors such as axial and limbs dystonia, pelvic trusting, kicking, rocking, and other repetitive movements.4 Nevertheless, electrical stimulation of the insula fails to reproduce motor symptoms,2 which typically occur due to propagation to other motor structures in the frontal lobe and cingulate regions.5
To clinically differentiate the epileptic arc de cercle from PNES, we could not rely exclusively on the presence of stereotypical symptoms.6,7 Peri-ictal symptoms in our patient were vital to provide the correct diagnosis and included a consistent aura, sudden onset of seizures out of sleep, presence of athetoid, tonic and dystonic symptoms, and short duration of the seizures.3 Eye closure during the seizures also has been used to differentiate epilepsy from PNES but is not a specific sign either. The eye features associated with PNES are the resistance to eye opening during the spell or the presence of eye flutter.
The presence of ictal and interictal epileptiform discharges in our case also supported the diagnosis of epilepsy, which was finally confirmed with SEEG. It is important to recommend that extracranial EEG analysis in patients with arc de cercle be performed using the transverse bipolar montage in addition to the traditional longitudinal bipolar montage so subtle midline abnormalities will not be missed.
Author contributions
Pestana Knight conceptualized the report, analyzed and interpreted the clinical data, and drafted/revised the manuscript. Grinenko interpreted the clinical data and revised the manuscript. Bulacio conceptualized the report, analyzed and interpreted the clinical data, and revised the manuscript. Bingaman interpreted and analyzed the clinical data and revised the manuscript. Gupta interpreted and analyzed the clinical data and revised the manuscript. Chauvel conceptualized the report, analyzed and interpreted the clinical data, and drafted/revised the manuscript.
Study funding
No targeted funding reported.
Disclosure
E.M. Pestana Knight is funded by HRSA grant #H98MC26260-05-00. O. Grinenko, J. Bulacio, and W. Bingaman report no disclosures. A. Gupta serves on a scientific advisory board for Tuberous Sclerosis Alliance; serves on the editorial boards of Pediatric Neurology and Epilepsy Currents; serves as a consultant for Eisai Inc. and Mallinckrodt; and receives research support from Tuberous Sclerosis Alliance. P. Chauvel reports no disclosures. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
References
- 1.Alomar S, Mullin JP, Smithason S, Gonzalez-Martinez J. Indications, technique, and safety profile of insular stereoelectroencephalography electrode implantation in medically intractable epilepsy. J Neurosurg 2018;128:1147–1157. [DOI] [PubMed] [Google Scholar]
- 2.Mazzola L, Mauguiere F, Isnard J. Electrical stimulations of the human insula: their contribution to the ictal semiology of insular seizures. J Clin Neurophysiol 2017;34:307–314. [DOI] [PubMed] [Google Scholar]
- 3.Freri E, Matricardi S, Gozzo F, Cossu M, Granata T, Tassi L. Perisylvian, including insular, childhood epilepsy: presurgical workup and surgical outcome. Epilepsia 2017;58:1360–1369. [DOI] [PubMed] [Google Scholar]
- 4.Obaid S, Zerouali Y, Nguyen DK. Insular epilepsy: semiology and noninvasive investigations. J Clin Neurophysiol 2017;34:315–323. [DOI] [PubMed] [Google Scholar]
- 5.Hagiwara K, Jung J, Bouet R, et al. How can we explain the frontal presentation of insular lobe epilepsy? The impact of non-linear analysis of insular seizures. Clin Neurophysiol 2017;128:780–791. [DOI] [PubMed] [Google Scholar]
- 6.Herskovitz M. Stereotypy of psychogenic nonepileptic seizures. Epilepsy Behav 2017;70:140–144. [DOI] [PubMed] [Google Scholar]
- 7.Syed TU, LaFrance WC Jr, Kahriman ES, et al. Can semiology predict psychogenic nonepileptic seizures? A prospective study. Ann Neurol 2011;69:997–1004. [DOI] [PubMed] [Google Scholar]