Abstract
Background
We sought to compare trends of suicide-related behavior (SRB) before and after initiation of antiepileptic drug (AED) therapy among AED users (with and without epilepsy) to that of individuals without AED use controlling for sociodemographic characteristics and mental health comorbidity.
Methods
We used national Veterans Health Administration (VHA) data for post-9/11 veterans who received VHA care (2013–2014) without prior AED use. We conducted generalized estimation equation (GEE) analyses, stratified by epilepsy status and type of AED received, to assess the trend of SRB prevalence the year prior to and after the index date (date of first AED prescription/date of first health care encounter for non-AED users) controlling for sociodemographic factors and mental health comorbidity.
Results
The GEE analysis showed significant curvilinear trends of SRB prevalence over the 24-month study period among the AED users, indicating that the probability of SRB diagnoses increased over time with a peak before the index month and decreased thereafter. Similar patterns were observed among non-AED users, but significantly lower odds for SRB. Among AED users, there were no significant differences by epilepsy status; however, higher SRB prevalence and differential SRB trajectory measures were observed among those who received AEDs with mood-stabilizing action.
Conclusions
The peak of SRB prior to and rapid reduction in SRB after initiation of AED, and the finding that individuals eventually prescribed a mood-stabilizing AED (vs other AED or levetiracetam) had higher odds of SRB, suggests a strong possibility that the relationship of AED and SRB is one of residual confounding.
Although the Food and Drug Administration (FDA) has labeled all antiepileptic drugs (AEDs) as suicidogenic, only lamotrigine and topiramate of over 30 AEDs were associated with increased suicide-related behavior (SRB).1,2 The high prevalence of comorbid behavioral health issues in patients treated with AEDs suggests that these positive associations are sensitive to confounding by indication, preexisting mental health conditions, and medications received.3 Thus, the association of SRB and AEDs is still a matter of debate and could affect care of patients receiving AEDs.
With increasing use of AEDs in other conditions, well-designed prospective long-term studies of AED use among patients with epilepsy, pain disorders (e.g., headache, neuropathic pain), and psychiatric conditions are required to understand their causal role in SRB. Two prior longitudinal studies found that peak SRB was prior to exposure, suggesting that symptoms may prompt AED prescription.4,5 While work by Pugh et al.4 focused exclusively on older veterans prescribed an AED without a control group, Hesdorffer et al.5 examined SRB among incident epilepsy patients. Type of AED prescribed or the indication for use was not studied.
This study addresses these gaps by systematically examining the temporal relationship between SRB and AED exposure in previously deployed post-9/11 US veterans. We compared trends of SRB among those prescribed AED for epilepsy, for nonepileptic conditions, and without AED use while taking into account the risk for SRB associated with comorbid psychiatric conditions and concomitant medications. We also evaluated variation in SRB among individuals prescribed AED with a mood-stabilizing action vs other AED.
Methods
Data sources and population
Using the roster of veterans who served in post-9/11 conflicts, we identified individuals who received care in the Veterans Health Administration (VHA) during fiscal years (FY) 2013 and 2014. To ensure accuracy in identifying comorbid conditions and medication use, we required that participants have at least 1 year of VHA care prior to the index date (the first AED initiation date during the study period among AED users and the date of the first visit to VHA care in the study period among non-AED users). For those who met inclusion criteria, we obtained information on demographic characteristics, diagnosis codes, types of care received, and specific medications dispensed from VHA outpatient and mail order pharmacies, using the national VHA inpatient, outpatient, and pharmacy benefits data.
Study design
We conducted a retrospective cohort study to compare the temporal trend of SRB outcomes 1 year before and after the index date among post-9/11 veterans between those with vs without AED exposure, using a new-user monotherapy design. This design was used to reduce survivor and chronology biases that occur in cohort studies with repeated exposures.4,6
Study measures
Exposure to seizure medications
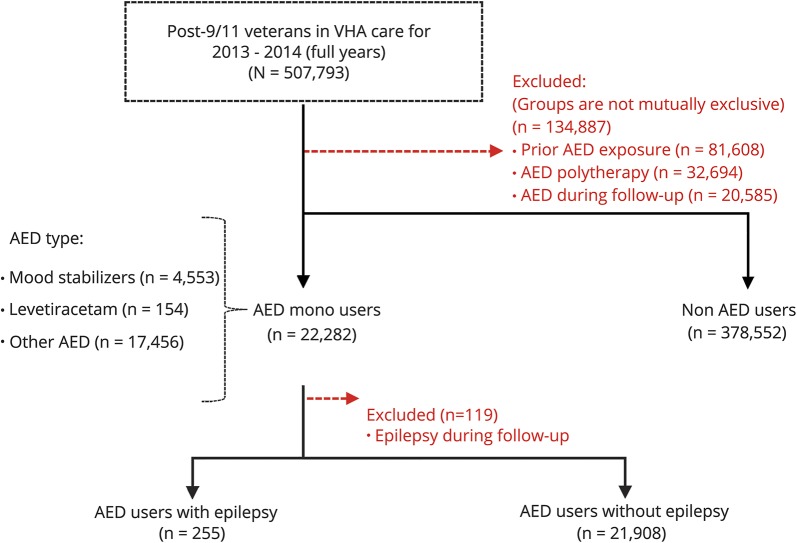
VHA product names included in the VHA Pharmacy Benefits Management database were used to identify prescription of any of the following AEDs: carbamazepine, clobazam, clonazepam, eslicarbazepine acetate, ethosuximide, gabapentin, lacosamide, lamotrigine, levetiracetam, oxcarbazepine, perampanel, phenobarbital, phenytoin, pregabalin, primidone, retigabine, rufinamide, sodium valproate, tiagabine, topiramate, vigabatrin, and zonisamide. Individuals with a first (monotherapy) prescription for an AED dispensed from the VHA during FY13 and FY14 were included as AED users, with the date of the first AED dispensed as the index date. Those with use of AEDs prior to October 1, 2012, those who received new AEDs after the index date, and those prescribed multiple AEDs FY13–15 were excluded (figure 1). Individuals with no AED prescription during the study period were included as non-AED users, with the date of the first visit to VHA care during FY13–FY14 as the index date.
Figure 1. Study population and case ascertainment.
AED = antiepileptic drug; VHA = Veterans Health Administration.
AED users were further grouped as those with epilepsy (who met the criteria for epilepsy using our previously validated epilepsy identification algorithm7,8) and without epilepsy. Individuals who were classified as having epilepsy by the algorithm eventually during follow-up period after the index date (n = 119) were excluded from the analysis. We further identified AED users as those who received an AED with known mood-stabilizing action (carbamazepine, oxcarbazepine, lamotrigine, and sodium valproate), levetiracetam (as it was described to be independently associated with psychiatric adverse outcomes), and other AEDs.9–11
Suicide-related behavior
SRB was defined using ICD-9-CM codes (V62.84: suicidal ideation, E950–E958: suicide attempt, completed suicide, and self-inflicted injury12,13) in VHA inpatient and outpatient data files 1 year prior to and 1 year after the index date. We identified the date of all SRB episodes and identified SRB for participants as a dichotomous variable each month during the 24-month study period (1 for each 30-day period before and after the index date). Consistent with the procedure used in prior studies of SRB associated with medication use, the index date was included in the period 30 days prior to the index date.4,12,14 A sensitivity analysis was also conducted including the index date in the period 30 days after the index date to determine the consistency of the results. For patients who died within a year after the index date, the monthly SRB indicator after the date of death was treated as censored.
Demographic covariates
Demographic characteristics including age (≤25 years, 26–40 years, and >40 years), sex, race/ethnicity (non-Hispanic white, black, Hispanic, other), and an indicator of poverty threshold (VHA means test: those with very low income do not have copayment15) were obtained from VHA inpatient and outpatient data.
Clinical covariates
We developed indicators for conditions that have previously been associated with SRB such as depression, anxiety, bipolar disorder, posttraumatic stress disorder (PTSD), substance use disorder, and schizophrenia using previously validated ICD-9-CM code algorithms during the year prior to index date to control for baseline clinical characteristics in statistical models.15–17 Clinical conditions that have been previously associated with AED use or SRB, including chronic pain conditions (migraine, back pain, neuropathic pain), traumatic brain injury (TBI), dementia, and a count of physical comorbidity (Selim Comorbidity index) were included as covariates in the analysis.17–21 We also adjusted for indicators of psychiatric comorbidity severity/duration (e.g., prior prescription of antidepressant/antipsychotic medication, prior psychiatric hospitalization).22
Statistical analysis
We characterized the study cohort using descriptive statistics of patient characteristics and compared patient characteristics between AED users with epilepsy, AED users without epilepsy, and non-AED users with χ2 statistics. To compare the trend of SRB between AED users and non-AED users over time, we used Generalized Estimating Equation (GEE) analysis that modeled the log-odds of SRB as a linear function of time and time squared, an indicator of AED exposure, 2-way interactions between AED exposure with time factors, and adjusting for covariates. To further determine if the difference in SRB trend between AED users vs nonusers differed before and after the index date, GEE models were refined by including an indicator to identify time period after the index date, and 3-way interactions among post index date indicator, time factors, and AED exposure indicators. To determine if SRB patterns vary by epilepsy status among AED users, we conducted similar GEE analyses to compare the SRB trend between AED users with and without epilepsy adjusting for covariates and inverse propensity score weights (IPSW) predicting epilepsy to balance baseline covariates between AED users with and without epilepsy. Finally, we conducted GEE analyses among AED users to determine whether SRB trends differed for AEDs with mood-stabilizing action, levetiracetam, and other AEDs.
Standard protocol approvals, registrations, and patient consents
This observational study received institutional review board approvals from the University of Texas Health Science Center at San Antonio and the Edith Nourse Rogers VA medical center including a waiver of informed consent as there was no contact with participants in this retrospective database study.
Data Availability
Anonymized data not published within this article will be made available by request from any qualified investigator.
Results
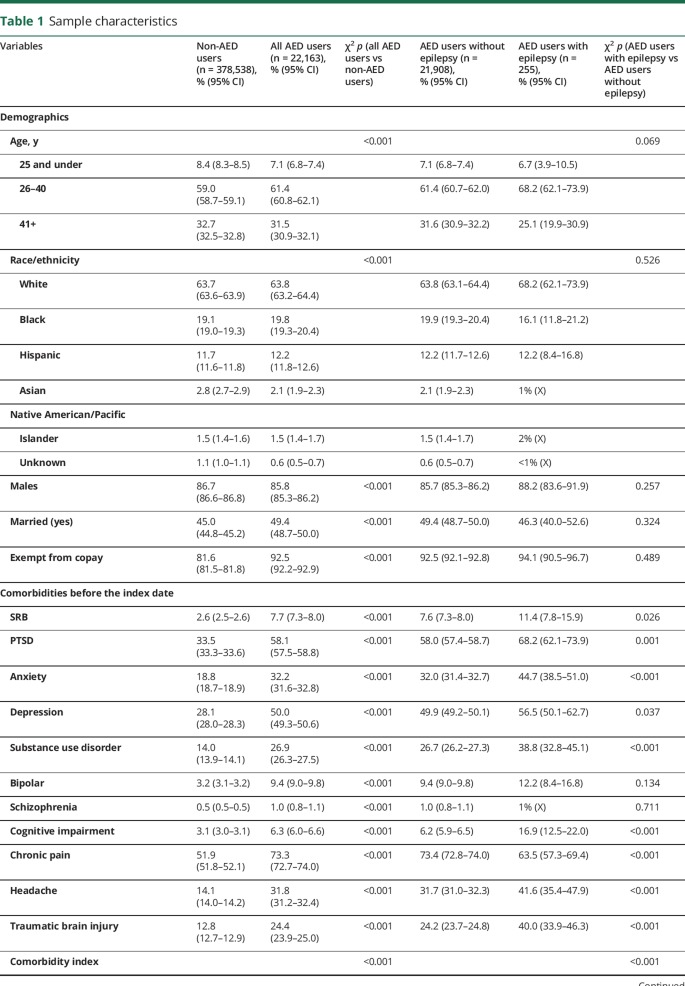
From the overall population of post-9/11 veterans seeking VHA care in FY13–FY14 (n = 507,793), 22,282 received new AED monotherapy (figure 1). Among AED monotherapy users, 255 met epilepsy criteria; 21,908 received AED for other conditions. Table 1 describes the demographic and clinical characteristics of the sample, which was primarily male with a mean age of 36.6 years (SD 10.1) and exempt for copay due to low income. There were significant differences in the proportions of demographic and clinical characteristics between AED users and non-AED users (table 1). Compared to non-AED users, AED users were significantly more likely to be have mental health conditions, TBI, pain conditions, physical comorbidity, psychiatric hospitalization, and prescriptions for antidepressant/antipsychotic medications prior to the index date. Among AED users, compared to those without epilepsy, those with epilepsy had significantly higher rates of PTSD, anxiety, depression, substance abuse, cognitive diagnosis, chronic pain, TBI, physical comorbidity, and SRB before index date.
Table 1.
Sample characteristics
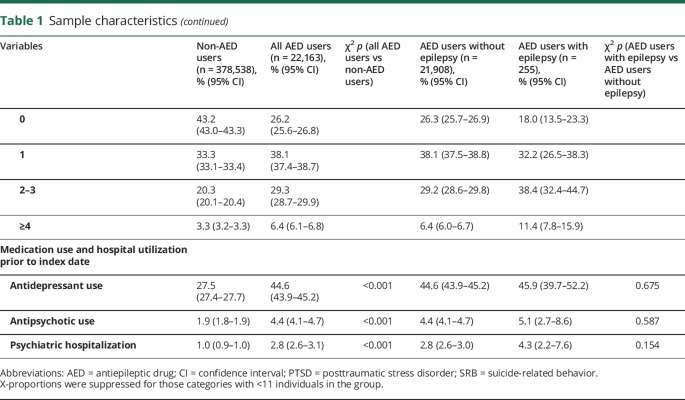
The GEE analysis revealed a significant curvilinear trend of SRB prevalence (on the log-odds scale) over the 24-month study period for AED users where the probability of SRB diagnoses increased over time before the index month and then decreased after the index month (figure 2 and see table e-1, links.lww.com/CPJ/A36 for GEE results). Similar curvilinear trajectory (i.e., increased SRB probability over time before the index month and then decreased after the index month) was observed among non-AED users, but with significantly lower likelihood of SRB throughout. The SRB probability trajectory was significantly different between AED users and non-AED users after balancing covariates (see estimates of interactions between time factors and AED exposure groups in table e-1). Indicators of prior psychiatric comorbidity, medication, and hospitalization were all significantly associated with increased odds of SRB (table e-1).
Figure 2. Likelihood of suicide-related behavior over time by antiepileptic drug (AED) exposure and epilepsy status.
There were significant differences in the SRB trajectory measures before and after the index date in all the study groups, indicating the SRB trajectory was asymmetric around the index month (see estimates of 2-way interactions between post index date indicator and time factors in table e-1, links.lww.com/CPJ/A36). As shown in figure 2, there was a steeper rate of increase in SRB probability 6 months prior to the index month than the rate of decrease in SRB probability 6 months after the index month. Although the change in the SRB trajectory measure before and after the index month was not significantly different among AED users with and without epilepsy, a significant difference existed between the AED users and non-AED users (see estimates of 3-way interactions among post index date indicator, time factors, and AED exposure indicators in table e-1).
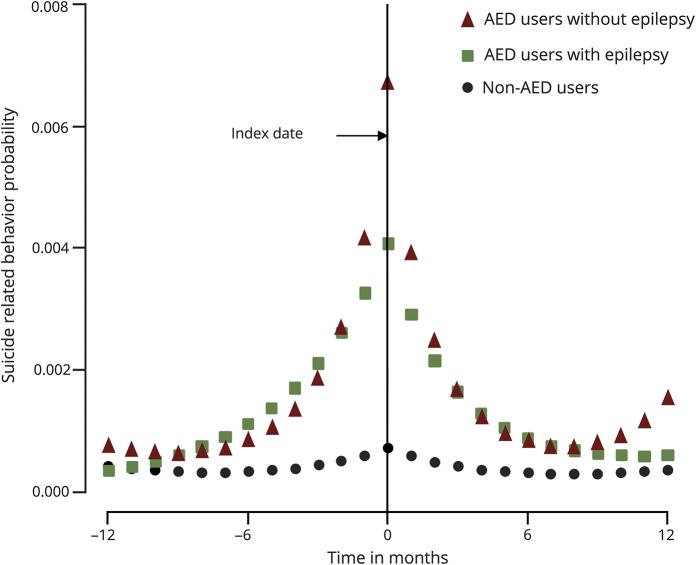
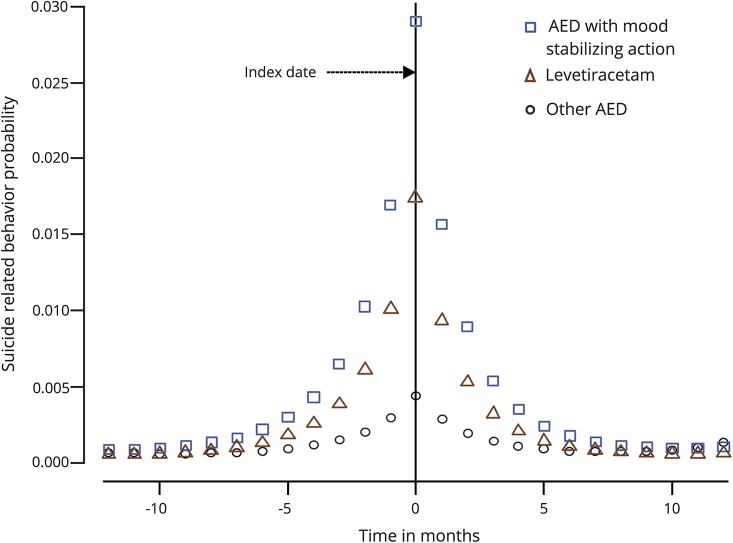
Among AED users, GEE analyses found no significant differences in SRB probabilities over the 24-month period for those with and without epilepsy after balancing covariates using the IPSW (table e-2, links.lww.com/CPJ/A36). Examination of SRB trends by type of AED prescribed suggested that individuals prescribed AED with a mood-stabilizing action had a significantly higher likelihood of SRB and an asymmetric trajectory around index month compared to those receiving levetiracetam or other AED (figure 3 and table e-3). No differences in the trajectory measures were observed between those receiving levetiracetam compared to other AEDs.
Figure 3. Likelihood of suicide-related behavior over time among antiepileptic drug (AED) users by type of AED received.
Discussion
The FDA's analysis and subsequent black box recommendation regarding SRB risk and AED was highly contested given the dependence on self-reported data, the lack of a systematic and prospective assessment, and the questionable validity of the measures used.23 Consistent with this skepticism, there was no effect on the utilization of AED after the FDA report.24 Since the FDA warning, several studies have been conducted to determine if specific AED have increased SRB risk, but results have been conflicting in that, while some studies have shown increased risk of SRB for certain AED, a similar number of studies have demonstrated a protective effect.25,26 Results of systematic reviews and meta-analysis of these existing studies also demonstrate considerable heterogeneity in these studies at the clinical and methodologic level.26 This study addresses several gaps by comparing temporal trends in SRB in AED users vs nonusers controlling for baseline comorbidity, examining differences in SRB for AED users with and without epilepsy, and comparing SRB for different types of AED in the population of post-9/11 veterans in VHA care FY13–FY14. Similar to findings in studies of older veterans and civilians we found that, compared to non-AED users, SRB was higher among those who received AED, but that difference was evident long before the initiation of AED therapy.4,5 These data have major implications for our understanding of the “link” between AED and SRB.
Findings from this study of relatively younger veterans are consistent with the results from our prior study of older veterans, in that the SRB patterns are similar in both populations.4 The current study further adds to the results of the previous study by comparing the trends to a control group of non-AED users and also examined separately the SRB trends among those prescribed AEDs for conditions other than epilepsy (a major portion of AED users) and those prescribed AEDs for epilepsy, thus adjusting for the risk of SRB due to epilepsy per se. These findings in different populations of veterans suggest that SRB is not temporally associated with initiation of AED treatment. SRB trends in our study were similar to those studies with antidepressant medications that also found that risk was highest in the month before the initial treatment (talk therapy or prescription), supporting evidence that suicide attempt or mental health concerns may prompt initiation of treatment.12,27 Similarly, our finding of reduction in risk after initiation of treatment is more consistent with decline in risk after initiation of treatment and probably reflects a relative improvement in depression rather than a specific effect of treatment on suicidality.
Several population-based studies and meta-analyses have found that suicide is an important contributor to the elevated mortality observed in epilepsy and that individuals with epilepsy have a higher risk of suicide, even when coexisting psychiatric disease, demographic differences, and socioeconomic factors were taken into account.28–30 In a study of the Clinical Practice Research Datalink from the United Kingdom, Hesdorffer et al.5 found that suicide attempts and recurrent suicide attempts were more common in patients with epilepsy compared to randomly selected controls, and that suicide attempts were associated with epilepsy even before epilepsy manifests. Our study found similar differences between patients with epilepsy and patients without AED exposure. However, among those with AED exposure, we found similar patterns of SRB among those with epilepsy and those for whom AED was prescribed for other indications, which suggests a role of preexisting mental health comorbidities, poor coping skills, or impulsivity in SRB. Given the significantly higher likelihood of psychiatric conditions that are associated with SRB in AED users, the finding of increased risk associated with eventual AED use suggests the possibility of residual confounding associated with underlying mental health conditions that cannot be adequately adjusted for with administrative data.
Due to the increasing use of AED in the management of pain, migraine, and certain psychiatric disorders, clinicians should be aware of the potential risk of and protective factors in preventing SRB and specific AEDs.31–34 Although only carbamazepine, valproate, and lamotrigine have FDA indication for the treatment of psychiatric conditions, virtually all new AEDs have claimed efficacy for some psychiatric symptoms or disorders.33 Consistent with prior literature, our study found that the probability of SRB was higher among those receiving mood stabilizers compared to those receiving non-mood stabilizers; however, temporal patterns show that risk was higher even before the AED was dispensed.14,35,36 Given the considerable CNS polypharmacy in the post-9/11 veterans, clinicians may prescribe medications that address multiple indications simultaneously.33,37 Our earlier finding of “rational polypharmacy” in post-9/11 veterans with epilepsy suggests this is common among veterans with epilepsy.38
SRB risk declined significantly after the initiation of the treatment with mood-stabilizing AEDs, which is consistent with the study by Tsai et al.,39 which concluded that immediate or recent use of any mood stabilizer considerably lowers the rate of death, suicide, or suicidal behavior in bipolar disorder patients. The asymmetry of the SRB probability before and after the index date suggested a potential long-term effect of AED on SRB. The shallower slope of SRB after the index date suggests the gradual positive effect of AEDs on SRB. However, the slight increase in SRB for AED users without epilepsy suggests that a longer observation period may be useful to better understand the longer-term relationship of AED and SRB. The significant differential trend in the SRB trajectory among those receiving AEDs with mood-stabilizing action compared to those receiving other AEDs suggests that mental health and behavioral comorbidities play an important role in influencing these SRB patterns both before and after the initiation of AED therapy. Thus the confounding effect of these factors needs to be considered in evaluating the risk of SRB with AED therapy.
Limitations
Despite the strengths of the study, there are also limitations. Requiring that participants have at least 1 year of VHA care prior to the index date and excluding those with prior AED use guaranteed that no AED were prescribed within the VHA 1 year prior to index date; however, AED prescriptions from sources other than VHA may have occurred. Given that the vast majority of the veterans in this study (>80%) receive care and medications at no cost, they have major incentive to use VHA for medication. Thus, the study results can be reasonably generalized to the new monotherapy AED users in VHA care. Study data were collected for administrative purposes and hence sensitivity of identifying and ascertaining a psychiatric condition can be low, with a possible misclassification bias. Also, information regarding the severity of the psychological comorbidities was limited and thus can lead to residual confounding. Due to the study design, long-term consequences of AED use beyond 1 year and the effect of multiple AEDs were not evaluated. Finally, individuals with no follow-up visit were considered to have no suicidal episodes, which may lead to information bias.
In the veteran population, approximately 20 individuals complete suicide each day.40 This study provides important information to guide clinicians. Consistent with literature suggesting a bidirectional relationship between SRB and epilepsy, we confirmed a finding from our prior study that SRB peaks prior to AED prescription. Thus, prevention efforts should focus on understanding patient mental health status and suicidal ideation on a regular basis. Furthermore, clinicians may be reassured that the large proportion of increased risk of suicide is preexisting to the initiation of AED therapy and should educate people with epilepsy and neurologic conditions accordingly.
Acknowledgment
The authors thank the Joint Trauma Registry and the VA Office of Patient Care Services, which provided data on TBI severity.
Author contributions
Hari Krishna Raju Sagiraju: study concept and design, interpretation of data, manuscript preparation. Chen-Pin Wang: study concept and design, analysis and interpretation of data. Megan E. Amuan: study concept and design, analysis and interpretation of data. Anne C. Van Cott: study concept and design, critical revision of manuscript for intellectual content. Hamada Hamid Altalib: study concept and design, critical revision of manuscript for intellectual content. Mary Jo V. Pugh: study concept and design, acquisition of data, study supervision, interpretation of data, and critical revision of manuscript for intellectual content.
Study funding
Funded by VA Health Services Research and Development Service 1I01HX000329-01A1 (PI: Dr. Mary Jo Pugh).
Disclosure
H.K.R. Sagiraju and C.-P. Wang report no disclosures. M.E. Amuan receives research support from VA Health Services Research and Development Service. A.C. Van Cott has received research support from NIH. H. Hamid Altalib receives research support from US Department of Defense. M.J.V. Pugh serves as an Associate Editor for BMC Health Services Research and BMC Geriatrics; serves as a consultant for Brain Sentinel 2018; and receives research support from Brain Sentinel, VA Health Services Research and Development Service, NIH/NICHD, US Department of Defense, and VA Rehabilitation Research and Development. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
References
- 1.Busko M. FDA advisory members agree antiepileptics pose suicidality risk, nix need for black-box warning. Medscape 2008. Available at: medscape.com/viewarticle/577432. Accessed March 27, 2018. [Google Scholar]
- 2.Hesdorffer DC, Kanner AM. The FDA alert on suicidality and antiepileptic drugs: fire or false alarm? Epilepsia 2009;50:978–986. [DOI] [PubMed] [Google Scholar]
- 3.Grimaldi-Bensouda L, Nordon C, Rossignol M, et al. . Antiepileptic drugs and risk of suicide attempts: a case–control study exploring the impact of underlying medical conditions. Pharmacoepidemiol Drug Saf 2017;26:239–247. [DOI] [PubMed] [Google Scholar]
- 4.Pugh MJ, Hesdorffer D, Wang CP, et al. . Temporal trends in new exposure to antiepileptic drug monotherapy and suicide-related behavior. Neurology 2013;81:1900–1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hesdorffer DC, Ishihara L, Webb DJ, Mynepalli L, Galwey NW, Hauser WA. Occurrence and recurrence of attempted suicide among people with epilepsy. JAMA Psychiatry 2016;73:80–86. [DOI] [PubMed] [Google Scholar]
- 6.Ray WA. Evaluating medication effects outside of clinical trials: new-user designs. Am J Epidemiol 2003;158:915–920. [DOI] [PubMed] [Google Scholar]
- 7.Pugh MJ. Epilepsy among Iraq and Afghanistan war veterans: United States, 2002–2015. MMWR Morb Mortal Wkly Rep 2016;65:1224–1227. [DOI] [PubMed] [Google Scholar]
- 8.Pugh MJ, Orman JA, Jaramillo CA, et al. . The prevalence of epilepsy and association with traumatic brain injury in veterans of the Afghanistan and Iraq wars. J Head Trauma Rehabil 2015;30:29–37. [DOI] [PubMed] [Google Scholar]
- 9.Mula M, Trimble MR, Yuen A, Liu RS, Sander JW. Psychiatric adverse events during levetiracetam therapy. Neurology 2003;61:704–706. [DOI] [PubMed] [Google Scholar]
- 10.Andersohn F, Schade R, Willich SN, Garbe E. Use of antiepileptic drugs in epilepsy and the risk of self-harm or suicidal behavior. Neurology 2010;75:335–340. [DOI] [PubMed] [Google Scholar]
- 11.Nadkarni S, Devinsky O. Psychotropic effects of antiepileptic drugs. Epilepsy Curr 2005;5:176–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Simon GE, Savarino J, Operskalski B, Wang PS. Suicide risk during antidepressant treatment. Am J Psychiatry 2006;163:41–47. [DOI] [PubMed] [Google Scholar]
- 13.Finley EP, Bollinger M, Noël PH, et al. . A national cohort study of the association between the polytrauma clinical triad and suicide-related behavior among U.S. veterans who served in Iraq and Afghanistan. Am J Public Health 2015;105:380–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patorno E, Bohn RL, Wahl PM, et al. . Anticonvulsant medications and the risk of suicide, attempted suicide, or violent death. JAMA 2010;303:1401–1409. [DOI] [PubMed] [Google Scholar]
- 15.Pugh MJV, Copeland LA, Zeber JE, et al. . The impact of epilepsy on health status among younger and older adults. Epilepsia 2005;46:1820–1827. [DOI] [PubMed] [Google Scholar]
- 16.Selim AJ, Fincke G, Ren X. The Comorbidity Index in Measuring and Managing Health Care Quality. Gaithersburg: Aspen Publishers; 2002. [Google Scholar]
- 17.Selim AJ, Fincke BG, Ren XS, et al. . Comorbidity assessments based on patient report: results from the Veterans Health Study. J Ambul Care Manage 2004;27:281–295. [DOI] [PubMed] [Google Scholar]
- 18.Hope OA, Zeber JE, Kressin NR, et al. . New-onset geriatric epilepsy care: race, setting of diagnosis, and choice of antiepileptic drug. Epilepsia 2009;50:1085–1093. [DOI] [PubMed] [Google Scholar]
- 19.Juurlink DN, Herrmann N, Szalai JP, Kopp A, Redelmeier DA. Medical illness and the risk of suicide in the elderly. Arch Intern Med 2004;164:1179–1184. [DOI] [PubMed] [Google Scholar]
- 20.Conwell Y, Brent D. Suicide and aging I: patterns of psychiatric diagnosis. Int Psychogeriatr 1995;7:149–164. [DOI] [PubMed] [Google Scholar]
- 21.Kaplan MS, Huguet N, McFarland BH, Newsom JT. Suicide among male veterans: a prospective population-based study. J Epidemiol Community Health 2007;61:619–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.VanCott AC, Cramer JA, Copeland LA, et al. . Suicide-related behaviors in older patients with new anti-epileptic drug use: data from the VA hospital system. BMC Med 2010;8:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Britton JW, Shih JJ. Antiepileptic drugs and suicidality. Drug Healthc Patient Saf 2010;2:181–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mittal M, Harrison DL, Miller MJ, Farmer KC, Thompson DM, Ng Y. Have antiepileptic drug prescription claims changed following the FDA suicidality warning? An evaluation in a state Medicaid program. Epilepsy Behav 2014;34:109–115. [DOI] [PubMed] [Google Scholar]
- 25.Fountoulakis KN, Gonda X, Samara M, et al. . Antiepileptic drugs and suicidality. J Psychopharmacol 2012;26:1401–1407. [DOI] [PubMed] [Google Scholar]
- 26.Ferrer P, Ballarin E, Sabate M, et al. . Antiepileptic drugs and suicide: a systematic review of adverse effects. Neuroepidemiology 2014;42:107–120. [DOI] [PubMed] [Google Scholar]
- 27.Termorshuizen F, Palmen SJ, Heerdink ER. Suicide behavior before and after the start with antidepressants: a high persistent risk in the first month of treatment among the young. Int J Neuropsychopharmacol 2016;19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bell GS, Sander JW. Suicide and epilepsy. Curr Opin Neurol 2009;22:174–178. [DOI] [PubMed] [Google Scholar]
- 29.Christensen J, Vestergaard M, Mortensen PB, Sidenius P, Agerbo E. Epilepsy and risk of suicide: a population-based case–control study. Lancet Neurol 2007;6:693–698. [DOI] [PubMed] [Google Scholar]
- 30.Meyer N, Voysey M, Holmes J, Casey D, Hawton K. Self-harm in people with epilepsy: a retrospective cohort study. Epilepsia 2014;55:1355–1365. [DOI] [PubMed] [Google Scholar]
- 31.Wiffen PJ, Derry S, Moore RA, et al. . Antiepileptic drugs for neuropathic pain and fibromyalgia (protocol). Cochrane Database of Systematic Reviews 2013:CD010567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ryder S, Stannard CF. Treatment of chronic pain: antidepressant, antiepileptic and antiarrhythmic drugs. Continuing education in anesthesia, Crit Care Pain 2005;5:18–21. [Google Scholar]
- 33.Ettinger AB, Argoff CE. Use of antiepileptic drugs for nonepileptic conditions: psychiatric disorders and chronic pain. Neurotherapeutic 2007;4:75–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Spina E, Perugi G. Antiepileptic drugs: indications other than epilepsy. Epileptic Disord 2004;6:57–75. [PubMed] [Google Scholar]
- 35.Park S, Lee HB, Ahn MH, et al. . Identifying clinical correlates for suicide among epilepsy patients in South Korea: a case–control study. Epilepsia 2015;56:1966–1972. [DOI] [PubMed] [Google Scholar]
- 36.Machado RA, Espinosa AG, Melendrez D, González YR, García VF, Rodríguez YQ. Suicidal risk and suicide attempts in people treated with antiepileptic drugs for epilepsy. Seizure 2011;20:280–284. [DOI] [PubMed] [Google Scholar]
- 37.Collett GA, Song K, Jaramillo CA, Potter JS, Finley EP, Pugh MJ. Prevalence of central nervous system polypharmacy and associations with overdose and suicide-related behaviors in Iraq and Afghanistan war veterans in VA care 2010–2011. Drugs Real World Outcomes 2016;3:45–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rohde NN, Baca CB, Van Cott AC, Parko KL, Amuan ME, Pugh MJ. Antiepileptic drug prescribing patterns in Iraq and Afghanistan war veterans with epilepsy. Epilepsy Behav 2015;46:133–139. [DOI] [PubMed] [Google Scholar]
- 39.Tsai C, Cheng C, Chou P, et al. . The rapid suicide protection of mood stabilizers on patients with bipolar disorder: a nationwide observational cohort study in Taiwan. J Affect Disord 2016;196:71–77. [DOI] [PubMed] [Google Scholar]
- 40.Suicide Among Veterans and Other Americans 2001–2014. Report Released by Office of Suicide Prevention, Department of Veterans Affairs, August 2016. Available at: mentalhealth.va.gov/docs/2016suicidedatareport.pdf. Accessed March 27, 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Anonymized data not published within this article will be made available by request from any qualified investigator.