Abstract
HF is the leading cause of readmissions in patients age ≥ 65 years with high associated societal and economic costs. The utilization metric of 30-day risk standardized readmission rates (RSRRs) has therefore become a target to reduce health care costs. In this review, we discuss in detail the implementation, effectiveness, and unintended consequences of the Hospital Readmissions Reduction Program (HRRP) - the major healthcare policy approach in the U.S. to reduce readmissions by financially penalizing hospitals with higher than average 30-day RSRRs. The HRRP was enacted by the Patient Protection and Affordable Care Act of 2010 (popularly known as ‘Obamacare’). The public reporting of RSRRs began in June 2009 and the HRRP readmission penalties went into effect starting fiscal year 2013. The policy had limited success in achieving its primary objective of reducing readmissions as the achieved reduction in heart failure readmissions was much smaller (~9%) than anticipated (~25%) with some of the reduction in RSRRs attributable to the artifact of administrative upcoding post-HRRP rather than an actual decline in readmissions. From the time of passage of this law, there have been significant concerns regarding gaming of the system such as increase in observation stays, delaying readmissions beyond discharge day 30th, and inappropriate triage strategies in emergency departments in order to achieve lower readmission rates to avoid penalties. A series of independent reports have now suggested that implementation of the HRRP was associated with an increase in 30-day, 90-day, and 1-year risk-adjusted heart failure mortality in U.S. with reversal in decade long trend of declining heart failure mortality. We review the evidence behind effect of the HRRP on readmissions and mortality outcomes as well as discuss various lessons to be learned from the design, implementation, and consequences of this policy.
Heart failure (HF) hospitalizations account for over a million admissions annually in both U.S. and Europe.1 The readmission rates following hospitalization for HF are high with approximately a fifth of patients readmitted within 30 days in the U.S.,2 though readmission rates are lower in many European countries. HF is the leading cause of readmissions in older patients age ≥ 65 years with high associated societal and economic costs.1 The utilization metric of 30-day risk standardized readmission rates (RSRRs) has therefore become a target to reduce health care costs in the U.S. In the last decade, two major healthcare policy approaches to reducing 30-day readmissions have been public reporting of individual hospital’s 30-day RSRRs and financially penalizing hospitals with higher than average 30-day RSRRs.
Medicare and Health Policy Innovations to Reduce Readmissions
Medicare is a large federal health insurance system in the U.S. for 57 million people aged 65 or older who have worked and payed into Medicare through payroll taxes, and certain younger individuals with disabilities, end-stage renal disease or amyotrophic lateral sclerosis.3 Medicare accounts for 15% of total federal spending.3 It is administered through the Centers for Medicare and Medicaid Services (CMS), a federal agency within the U.S. Department of Health and Human Services. Most of the U.S. hospitals bill Medicare and are, thus, bound by the rules of the CMS. Traditionally, innovations in health policy including delivery system reforms and improvements in value of health care such as reducing 30-day readmissions in HF have come from the CMS through its Medicare program. In June of 2009, CMS began publically reporting 30-day RSRRs for patients discharged after hospitalization for HF. Public reporting aimed to improve transparency and informed choice for patients as well as to incentivize hospitals to reduce their 30-day RSRRs. However, even after years of public reporting, there was no measurable change in trends for 30-day RSRRs.4
The Hospital Readmissions Reduction Program
The Patient Protection and Affordable Care Act of 2010 (popularly known as ‘Obamacare’) enacted the Hospital Readmissions Reduction Program (HRRP). Prior to the HRRP, hospitals had no financial incentive to reduce readmissions under the fee-for-service payment models. The HRRP established financial penalties to incentivize hospitals to reduce their 30-day readmissions after hospitalizations for target conditions (initially targeting HF, acute myocardial infarction, and pneumonia). The HRRP had a penalty-free implementation phase from time of passage of the law in March 2010 to end of the FY 2012 (September 2012). Starting October 2012, the HRRP penalties went into effect. In the penalty-phase, it requires the CMS to reduce payments to hospitals whose 30-day RSRRs for target conditions are higher than national average. Up to 3% of a hospital’s entire inpatient Medicare payment is at risk, not just the payment resulting from target condition readmissions. There is no reward or bonus for hospitals that improve their readmission rates. Further, as the readmission rates across the nation improves over time, so does the national average. Therefore, avoiding penalties is always a moving target for hospitals and they may face penalties even if there is improvement in their 30-day RSRRs. In FY 2017, 79% of the acute care hospitals in U.S. were penalized under the HRRP resulting in a total revenue of $528 million for the CMS.5
As soon as the HRRP program was announced substantial concerns were raised about potential for unintended consequences, particularly for HF patients.6, 7 Lesser resourced hospitals caring for the most vulnerable patients were projected to be the ones most likely to be penalized. Further concerns were raised that metric focused health systems may be incentivized to provide care in a way that was not patient-centered. There is also inherent tension between how the hospitals are reimbursed by the CMS and the readmissions reduction incentive by the HRRP. In the U.S., under the Inpatient Prospective Payment System (IPPS), the CMS payments to hospitals is based on the Diagnosis-related groups (DRGs). DRG is a patient classification scheme relating the cost incurred by a hospital to the patients it treats (case-mix) based on patients’ illnesses, their severity, and expected resource intensity for their management. DRG serves as a basic unit of payment for a given diagnosis. For example, if a Medicare patient is admitted under HF and shock DRG, a fixed payment will be made to the hospital by the CMS instead of the actual cost incurred by the hospital. If a hospital could provide care at a cost less than the DRG payment for that diagnosis, then it can make money. This incentivizes hospitals to reduce patients’ length of stay for any given diagnosis. However, shorter length of stay in HF patients without complete decongestion may increase the risk of 30-day readmission. With the HRRP, hospitals are also penalized for 30-day readmissions, creating a real fiscal challenge for hospitals in trying to balance length of stay under the fixed payment DRG system with 30-day readmissions risking penalties under the HRRP. Despite the substantial concerns raised, CMS proceeded with implementation without any guidance or evidence-based resource on how to achieve the goal of reducing 30-day readmissions.
Has the HRRP been Successful in Reducing Readmissions?
Unlike public reporting, the stick approach of the HRRP has been touted as a success in reducing 30-day readmissions.2, 8, 9 The 30-day RSRRs in HF declined from 23.5% in 2008 to 21.4% in 2014.8 However, the reduction in readmissions was mostly abrupt immediately following passage of the law.2 This may imply that hospitals were able to quickly identify root causes for their high readmission rates and then devised and successfully implemented strategies that led to immediate improvement in processes of care, which in turn led to rapid reduction in readmission rates. However, the data from 2010 to 2012 suggest that adoption and effect of multicomponent strategies to reduce readmission rates (that include discharge planning, medication management, patient education, and improvement in care transition processes) has been modest.10
An alternative mechanism accounting for the rapid reduction in 30-day RSRRs post-HRRP may be related to “gaming” of the system. In a national survey of hospital leaders in mid-2012, 26.6% of leaders reported that it was more than moderately likely that hospitals would increase the use of observation status to improve their perceived performance on readmissions, and 15.1% felt it was more than moderately likely that hospitals would increasingly avoid high-risk patients.11 As 30-day RSRR metric is risk adjusted, upcoding would result in lowering RSRR without a true reduction in readmissions. Recent data has suggested that up to two-third reduction in 30-day RSRR following the HRRP may be attributable to upcoding.12 The data based on clinical risk-adjustment rather than administrative risk-adjustment (subject to upcoding) showed no significant improvement in risk-adjusted readmissions in the first two years following implementation of the HRRP13, further lending support that a true reduction in readmissions following the HRRP is much lower than suggested. In addition to upcoding, other strategies may have been used to reduce 30-day RSRRs. If a patient presenting in emergency department is admitted under ‘observation status’, it is considered outpatient care rather than readmission even if the actual stay spans over days. Although the study by Zuckerman et al. showed no significant overall correlation between within hospital change in readmission rate with change in observation use, however, they found that the rate of rise in observation stays in U.S. for the HRRP target conditions has become steeper compared with non-target conditions in the post-HRRP implementation period suggesting some of the reduction in readmissions may be due to shift from inpatient admissions to observation stays.2
Even with this gaming of the system, the overall reduction in 30-day RSRRs is relatively modest compared with suggested reduction from previous literature that showed over one-quarter of readmissions may be avoidable.14 A long-term examination of data beyond 30 days showed readmissions reduction after HF hospitalization is even more modest with less than 1% absolute reduction in 1-year risk-adjusted readmissions.13 This suggests that many of the prevented 30-day readmissions are just readmissions delayed beyond discharge day 30th after index HF hospitalization. Thus, the totality of evidence indicates that the magnitude of reduction in readmissions after implementation of the HRRP is far lower than initially suggested and the results achieved have been disappointing at best.
The HRRP and Unintended Consequences
Since implementation of the HRRP, serious concerns have been raised regarding gaming of the system such as inappropriate triage strategies in emergency departments, increased use of observation stays when admissions would have been warranted, and delaying readmissions beyond discharge day 30th and its effects on HF patient care and survival.7, 13 Further, in addition to gaming, the financial penalties from the HRRP have been shown to fall disproportionately on safety-net hospitals (hospitals providing care to poor and vulnerable patients) as the RSRR metric was not adjusted for socio-economic factors, a major determinant of readmissions.15 Although 2% of the U.S. acute care hospitals are safety-net, they provide 20% of uncompensated care with relatively scant revenue generation.16 Disproportionate penalties from the HRRP may have compromised the ability of these already financially stricken hospitals to provide care for HF patients and need investigation in future studies. Studies investigating trends in 30-day, 90-day, and 1-year HF mortality in fee-for-service Medicare beneficiaries have suggested a recent reversal of the decade long trend in declining HF mortality in the U.S. coinciding with implementation of the HRRP (Figure).8, 13, 17–20 In a 100% fee-for-service Medicare sample, Dharmarajan et al. showed a 1.3% increase in 30-day risk standardized HF mortality from 2008 to 2014.8 Another study in fee-for-service Medicare beneficiaries found a declining 1-year risk-adjusted HF mortality from 2002 to 2010 followed by a 3.3% increase from 2010 to 2012 again coinciding with implementation of the HRRP.17 A recent study also showed that from 2009 to 2015, 600 studied hospitals with poor performance on baseline 30-day mortality had a small improvement (0.5% decline) in 30-day HF mortality. But this was offset by 3,196 other hospitals in this study where 30-day HF mortality increased on average by 1.1% during the same time period coincidental with the HRRP implementation.19
Figure. Absolute change in risk-adjusted heart failure readmission and mortality rates following implementation of the HRRP.
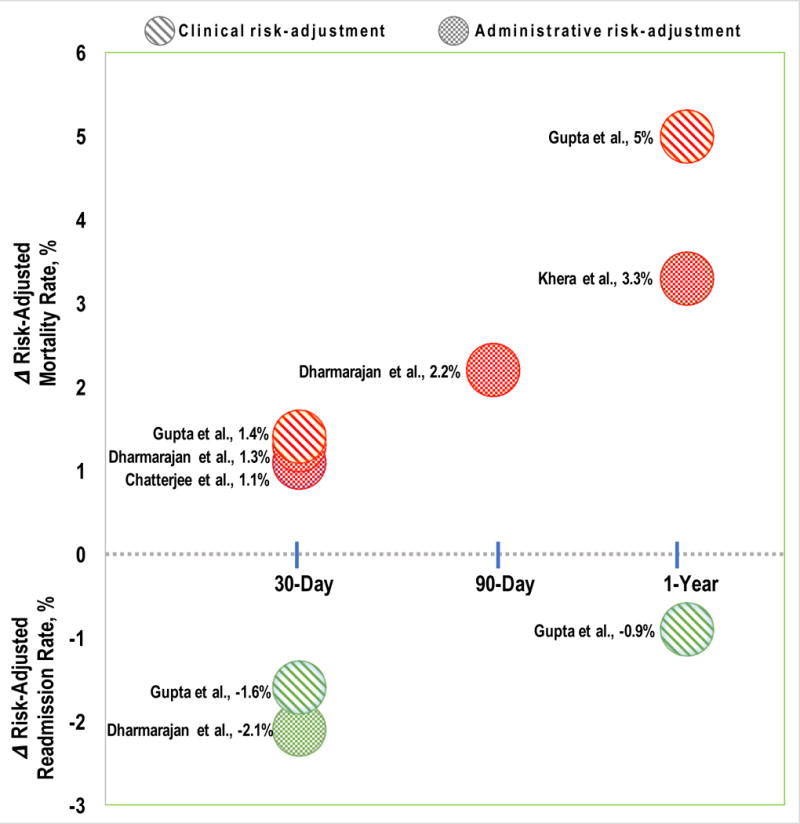
Figure summarizes the estimated absolute changes in 30-day, 90-day, or 1-year risk-adjusted readmissions (green circles) and mortality (red circles) after hospitalization for heart failure post implementation of the HRRP. The study by Gupta et al. (line pattern) used prospective clinical registry data for risk-adjustment. Rest of the studies (check pattern) used administrative (billing codes) data for risk-adjustment. Comparative time periods used in estimation of change in rates were: Chatterjee et al., 2009 to 2015; Dharmarajan et al., 2008 to 2014; Gupta et al., pre-HRRP period (2006-2010) to post-HRRP period (2012-2014); Khera et al., 2010 to 2012.
This figure highlights: 1) The HRRP implementation was associated with a modest reduction in readmissions and an increase in both short-term and long-term mortality after heart failure hospitalization in multiple independent investigations; 2) decline in readmissions was higher and rise in mortality was lower in heart failure post-HRRP in studies with administrative risk-adjustment compared with the study utilizing clinical risk-adjustment, suggesting evidence of upcoding post-HRRP; 3) a significant proportion of reduction in 30-day readmissions was lost at 1-year suggesting some of the readmissions were not prevented but delayed beyond discharge day 30th. HRRP, Hospital Readmissions Reduction Program
All three of these studies8, 17, 19 used administrative data for risk adjustment and neither of these directly tested the association of the HRRP implementation with trends in mortality following HF hospitalization. Using the American Heart Association’s Get With The Guidelines-HF registry data and with two different methodological approaches (interrupted time-series and survival analyses) exploiting detailed clinical risk-adjustment and accounting for within hospital clustering of patients, we recently showed that implementation of the HRRP was associated with a 1.4% increase in 30-day and 5% increase in 1-year risk-adjusted HF mortality.13 The findings were robust across race/ethnicity, teaching hospital status, and rural or urban hospital location. Although increasing patient severity of illness over time could explain these time trends of increasing HF mortality, we found no such evidence of increase in patient severity of illness in the post-HRRP implementation period compared with the pre-HRRP period. These multiple independent reports of increasing HF mortality post-HRRP suggest that the HRRP may have incentivized hospitals in a way that compromised the care of HF patients with adverse consequences on patient survival.
Lessons Learned
There are lessons to be learned or reaffirmed from the design and implementation of the HRRP and the consequences resultant from it (Table). First, financial incentives work and serious harm may result from health policies that incentivize utilization reduction over meaningful quality, safety, and hard patient outcomes. Here, the HRRP levied financial penalties of up to 3% of a hospital’s total inpatient Medicare revenue for 30-day readmissions, which were up to 15 times more than the financial penalties in place for 30-day mortality. This created a very strong incentive for hospitals to reduce 30-day readmission rates and may have led to diversion of resources away from meaningful quality improvement and patient safety with adverse consequences on patient survival. A recent study has shown that lower hospital-level 30-day risk-standardized mortality rate is associated with improved long-term survival in patients hospitalized with HF independent of mortality differences within first 30 days.21 These data strongly suggest that hospitals’ performance on 30-day mortality may be a better and more patient-centric metric for quality improvement than 30-day readmissions. Further, mortality should be weighted more than readmissions in determining financial penalties.
Table.
Lessons Learned from Implementation of the Hospital Readmissions Reduction Program
| Lesson Learned | Explanation | |
|---|---|---|
| 1. | 30-day risk-standardized readmission rate is a poor target for health policy interventions especially those that penalizes based on readmission rates. | Readmissions in heart failure may be more related to socioeconomic determinants of health and patient severity of illness than the actual quality of care provided. |
| 2. | Financial incentives work and work bi-directionally. | Financial incentives cannot be expected to work in only one direction towards effectiveness. ‘Gaming’ of system should be anticipated with counter measures in place to avoid unintended consequences. |
| 3. | Incentivize the right measure(s). | Directly incentivizing improvement in care transition processes and post-discharge care may be better than incentivizing reduction in 30-day readmissions without providing guidance and resources on how to achieve that goal. |
| 4. | Pre-specified, independent, and mandatory post-implementation monitoring of effectiveness and safety of major health policy changes must be instituted. | Akin to post-marketing surveillance of drugs; pre-specified mandatory monitoring of health policies for intended and unintended consequences post-implementation. |
| 5. | Advocate for evidence-based health policy. | Hold health policy to comparable standards as drugs and devices. Health policy trials and pilots are feasible and should be conducted before widespread implementation of a novel major public health policy. |
Second, post-implementation monitoring for intended and unintended consequences akin to post-marketing surveillance of effectiveness and safety for drugs should be an integral part of the health policy implementation process. This is even more important for health policies as unlike drugs that go through years of development and rigorous testing for efficacy and safety prior to their approval, policies often bypass these steps. Even though the inverse association between readmissions and mortality in HF was known for a long time22, 23, the HRRP policy incentivizing reduction in HF readmissions was implemented without any monitoring in place. This may have led to delayed identification of potential unintended consequences on mortality in HF from implementation of the HRRP.
Third, similar to drug and devices, we must strive to hold the health policies to high standards of rigorous testing and evidence-base prior to their implementation.24–26 The HRRP aimed to reduce readmissions by penalizing hospitals for higher than average readmission rates instead of directly incentivizing improvement in care transition processes and post discharge outpatient follow-up. A clustered randomized trial comparing these two approaches to reducing readmission rates while monitoring effects on mortality and utilization may have been better than a series of observational studies trying to uncover the unintended consequences of one of these approaches post-implementation. Further, serious potential harm to Medicare beneficiaries as a result of implementation of this untested policy could have been avoided. Randomized trials of major healthcare policies are even more relevant in the context of the policies such as the HRRP that are implemented widely and thus, leaving no good natural control for post-implementation assessment of their effectiveness and safety.
Conclusion
In summary, implementation of the HRRP, a statutorily mandated U.S. federal program aimed to reduce 30-day readmission rates by financially penalizing hospitals for higher than average RSRRs, was associated with only a modest reduction in readmissions and an increase in both short-term (30-day and 90-day) and long-term (1-year) mortality following hospitalization for HF. Future policies aimed to reduce HF utilization should have a direct focus on meaningful patient quality and safety metrics including patient survival.
Acknowledgments
Disclosures: Dr. Ankur Gupta is supported by the NIH grant number 5T32HL094301. Dr. Gregg Fonarow reports research support from NIH, consulting with Abbott, Amgen, Novartis, and Medtronic, and serving as a GWTG Steering Committee member.
References
- 1.Ambrosy AP, Fonarow GC, Butler J, Chioncel O, Greene SJ, Vaduganathan M, Nodari S, Lam CSP, Sato N, Shah AN, Gheorghiade M. The global health and economic burden of hospitalizations for heart failure: lessons learned from hospitalized heart failure registries. J Am Coll Cardiol. 2014;63(12):1123–1133. doi: 10.1016/j.jacc.2013.11.053. [DOI] [PubMed] [Google Scholar]
- 2.Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, Observation, and the Hospital Readmissions Reduction Program. N Engl J Med. 2016;374(16):1543–51. doi: 10.1056/NEJMsa1513024. [DOI] [PubMed] [Google Scholar]
- 3.The Facts on Medicare Spending and Financing. 2017 https://wwwkfforg/medicare/issue-brief/the-facts-on-medicare-spending-and-financing/ Accessed January 15, 2018.
- 4.DeVore AD, Hammill BG, Hardy NC, Eapen ZJ, Peterson ED, Hernandez AF. Has Public Reporting of Hospital Readmission Rates Affected Patient Outcomes?: Analysis of Medicare Claims Data. J Am Coll Cardiol. 2016;67(8):963–72. doi: 10.1016/j.jacc.2015.12.037. [DOI] [PubMed] [Google Scholar]
- 5.Aiming for fewer hospital U-turns: The Medicare Hospital Readmissions Reduction Program. 2017 https://wwwkfforg/medicare/issue-brief/aiming-for-fewer-hospital-u-turns-the-medicare-hospital-readmission-reduction-program/ Accessed January 15, 2018.
- 6.Butler J, Kalogeropoulos A. Hospital strategies to reduce heart failure readmissions: where is the evidence? J Am Coll Cardiol. 2012;60(7):615–7. doi: 10.1016/j.jacc.2012.03.066. [DOI] [PubMed] [Google Scholar]
- 7.Woolhandler S, Himmelstein DU. The Hospital Readmissions Reduction Program. N Engl J Med. 2016;375(5):493. doi: 10.1056/NEJMc1606658. [DOI] [PubMed] [Google Scholar]
- 8.Dharmarajan K, Wang Y, Lin Z, Normand ST, Ross JS, Horwitz LI, Desai NR, Suter LG, Drye EE, Bernheim SM, Krumholz HM. Association of Changing Hospital Readmission Rates With Mortality Rates After Hospital Discharge. JAMA: the journal of the American Medical Association. 2017;318(3):270–278. doi: 10.1001/jama.2017.8444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Desai NR, Ross JS, Kwon JY, Herrin J, Dharmarajan K, Bernheim SM, Krumholz HM, Horwitz LI. Association Between Hospital Penalty Status Under the Hospital Readmission Reduction Program and Readmission Rates for Target and Nontarget Conditions. JAMA: the journal of the American Medical Association. 2016;316(24):2647–2656. doi: 10.1001/jama.2016.18533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bradley EH, Sipsma H, Horwitz LI, Ndumele CD, Brewster AL, Curry LA, Krumholz HM. Hospital strategy uptake and reductions in unplanned readmission rates for patients with heart failure: a prospective study. J Gen Intern Med. 2015;30(5):605–11. doi: 10.1007/s11606-014-3105-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joynt KE, Figueroa JE, Oray J, Jha AK. Opinions on the Hospital Readmission Reduction Program: results of a national survey of hospital leaders. Am J Manag Care. 2016;22(8):e287–94. [PMC free article] [PubMed] [Google Scholar]
- 12.Ibrahim AM, Dimick JB, Sinha SS, Hollingsworth JM, Nuliyalu U, Ryan AM. Association of Coded Severity With Readmission Reduction After the Hospital Readmissions Reduction Program. JAMA Intern Med. 2018;178(2):290–292. doi: 10.1001/jamainternmed.2017.6148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gupta A, Allen LA, Bhatt DL, Cox M, DeVore AD, Heidenreich PA, Hernandez AF, Peterson ED, Matsouaka RA, Yancy CW, Fonarow GC. Association of the Hospital Readmissions Reduction Program Implementation With Readmission and Mortality Outcomes in Heart Failure. JAMA Cardiol. 2018;3(1):44–53. doi: 10.1001/jamacardio.2017.4265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Walraven C, Bennett C, Jennings A, Austin PC, Forster AJ. Proportion of hospital readmissions deemed avoidable: a systematic review. CMAJ. 2011;183(7):E391–402. doi: 10.1503/cmaj.101860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the Hospital Readmissions Reduction Program. JAMA: the journal of the American Medical Association. 2013;309(4):342–3. doi: 10.1001/jama.2012.94856. [DOI] [PubMed] [Google Scholar]
- 16.Neuhausen K, Spivey M, Kellermann AL. State politics and the fate of the safety net. N Engl J Med. 2013;369(18):1675–7. doi: 10.1056/NEJMp1310572. [DOI] [PubMed] [Google Scholar]
- 17.Khera R, Pandey A, Ayers CR, Agusala V, Pruitt SL, Halm EA, Drazner MH, Das SR, de Lemos JA, Berry JD. Contemporary Epidemiology of Heart Failure in Fee-For-Service Medicare Beneficiaries Across Healthcare Settings. Circulation Heart failure. 2017;10(11) doi: 10.1161/CIRCHEARTFAILURE.117.004402. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fonarow GC, Konstam MA, Yancy CW. The Hospital Readmission Reduction Program Is Associated With Fewer Readmissions, More Deaths: Time to Reconsider. J Am Coll Cardiol. 2017;70(15):1931–1934. doi: 10.1016/j.jacc.2017.08.046. [DOI] [PubMed] [Google Scholar]
- 19.Chatterjee P, Joynt Maddox KE. US National Trends in Mortality From Acute Myocardial Infarction and Heart Failure: Policy Success or Failure? JAMA Cardiol. 2018 doi: 10.1001/jamacardio.2018.0218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gupta A, Yancy CW, Fonarow GC. Evaluating Readmission-Need for More Clarity on Methods-Reply. JAMA Cardiol. 2018 Feb 14; doi: 10.1001/jamacardio.2017.5324. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pandey A, Patel KV, Liang L, DeVore AD, Matsouaka R, Bhatt DL, Yancy CW, Hernandez AF, Heidenreich PA, de Lemos JA, Fonarow GC. Association of Hospital Performance Based on 30-Day Risk-Standardized Mortality Rate With Long-term Survival After Heart Failure Hospitalization: An Analysis of the Get With The Guidelines-Heart Failure Registry. JAMA Cardiol. 2018 doi: 10.1001/jamacardio.2018.0579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pandey A, Golwala H, Xu H, DeVore AD, Matsouaka R, Pencina M, Kumbhani DJ, Hernandez AF, Bhatt DL, Heidenreich PA, Yancy CW, de Lemos JA, Fonarow GC. Association of 30-Day Readmission Metric for Heart Failure Under the Hospital Readmissions Reduction Program With Quality of Care and Outcomes. JACC Heart Fail. 2016;4(12):935–946. doi: 10.1016/j.jchf.2016.07.003. [DOI] [PubMed] [Google Scholar]
- 23.Heidenreich PA, Sahay A, Kapoor JR, Pham MX, Massie B. Divergent trends in survival and readmission following a hospitalization for heart failure in the Veterans Affairs health care system 2002 to 2006. J Am Coll Cardiol. 2010;56(5):362–8. doi: 10.1016/j.jacc.2010.02.053. [DOI] [PubMed] [Google Scholar]
- 24.Newhouse JP, Normand S-LT. Health Policy Trials. New England Journal of Medicine. 2017;376(22):2160–2167. doi: 10.1056/NEJMra1602774. [DOI] [PubMed] [Google Scholar]
- 25.Baicker K, Chandra A. Evidence-Based Health Policy. N Engl J Med. 2017;377(25):2413–2415. doi: 10.1056/NEJMp1709816. [DOI] [PubMed] [Google Scholar]
- 26.Jiang F, Zhang J, Shen X. Towards evidence-based public health policy in China. Lancet. 2013;381(9882):1962–4. doi: 10.1016/S0140-6736(13)61083-1. [DOI] [PubMed] [Google Scholar]


