Abstract
Purpose of Review
The purposes of this review are to (1) discuss the epidemiology and workup of the rare posterior cruciate ligament (PCL) avulsion fracture, (2) review the indications for nonoperative and operative management of patients with PCL avulsion fractures, (3) examine surgical outcomes in this patient population, and (4) discuss the authors’ preferred management algorithm and surgical approach.
Recent Findings
In accordance with the rarity of these injuries, the literature is sparse regarding surgical outcomes. Many of these injuries are in the setting of a multi-ligamentous injury. Most authors suggest that displaced PCL avulsion fractures should undergo operative fixation and current data suggests excellent outcomes when treating these patients with either open or arthroscopic fixation, with a low complication rate.
Summary
PCL avulsion fractures, although rare, should undergo fixation when displacement is present. Current studies report successful outcomes and a low complication rate.
Keywords: Posterior cruciate ligament (PCL), Avulsion fracture, PCL facet
Introduction
Posterior cruciate ligament (PCL) tears are uncommon injuries, and posterior cruciate ligament avulsion fractures are an extremely rare variant of this injury. A PCL injury most commonly results in an intrasubstance tear; however, femoral detachment and tibial avulsion patterns have been described [1•]. The reported incidence of general PCL injuries varies between 3 and 38% of acute knee injuries ([2–4], with more recent reports showing an increased incidence over the years [5]. The wide range noted in the reported incidence can be attributed to variable clinical presentations, including asymptomatic PCL injury [6]. Despite the low incidence of PCL injuries, resulting instability and early degenerative changes can be debilitating to patients, which are mostly young males [7]. Although there are many case series published on the management and outcomes of PCL avulsion fractures, no optimal surgical management has been suggested. In this chapter, we aim to present a concise review of PCL avulsion fractures and the available treatment options. Our preferred treatment method is also offered.
Etiology and Epidemiology
In a recent review of PCL avulsion fractures, Hooper et al. reported the mechanism of injury is similar to intrasubstance PCL tears [1•]. Most commonly, as a result of a motor vehicle accidents and especially motorcycle injuries, a dashboard injury occurs when a posterior directed force is applied to the proximal tibia when the knee is flexed. Therefore, PCL avulsion fractures are more frequently reported in China, India, and other countries where motorcycle transportation is more prevalent [7]. The second most frequent mechanism is sports-related trauma, in which the mechanism is knee hyperextension [1•]. Tibial-sided PCL avulsion fractures are the most common form of isolated bony PCL disruption. However, concomitant injuries can occur quite frequently. Hooper et al. reported meniscal injuries in 16.8% and additional ligamentous injuries in 19% of patients [1•], and a series reported by Pardiwala et al. revealed intra-articular pathology in 28% of patients [8•].
In contrast to intrasubstance PCL tears seen in adults, skeletally immature patients are predisposed to osteochondral avulsions as well, as ligaments are stronger than the developing physis [9]. Among pediatric PCL avulsion fractures, femoral-sided avulsions are more common than those on the tibial side.
Imaging
PCL avulsion fractures are important to identify as early reduction of a displaced fragment results in improved rates of union [10]. While multiple views of the knee may provide information about other injuries, the lateral view is the most valuable. PCL avulsion fractures appear as a focal discontinuity of the PCL facet at the posterior aspect of the tibia [11] (Fig. 1). Caution must be used to avoid underestimation of fragment displacement. Since the PCL inserts about 10 mm distal to the joint line, fragments with less than 10 mm displacement may not be appreciated on radiographs. Typically, those fragments that are easily visualized on standard radiographs are usually displaced more than 10 mm [12]. In patients where an avulsion is suspected but not clearly visualized on radiographs or displacement is uncertain, an MRI (Fig. 2) is recommended [12, 13]. The PCL avulsion fracture appears radiographically as focal discontinuity of the posterior aspect of the tibia [14]. Computed tomography (Fig. 3) with 3D reconstructions can provide additional information regarding the size and comminution of the fracture fragments and can be utilized for preoperative planning.
Fig. 1.
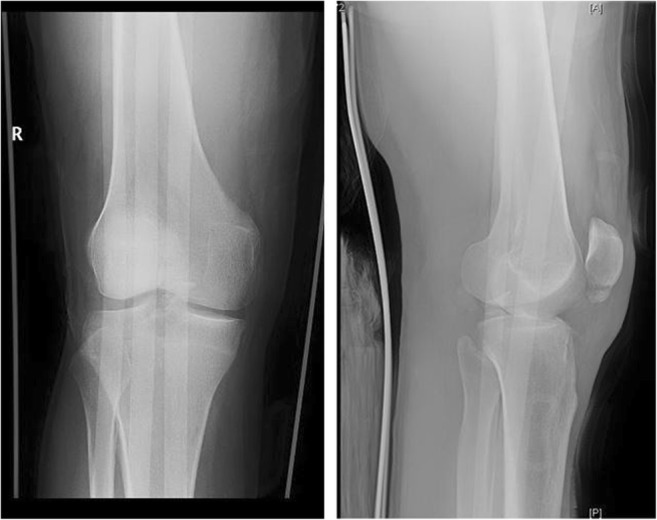
a, b AP and lateral images of a 25-year-old male status post motorcycle accident. This patient sustained a comminuted, displaced PCL facet fracture with nondisplaced fibular head fracture and a nondisplaced inferior pole patella fracture with intact extensor mechanism
Fig. 2.

Sagittal T1-weighted image showing a PCL facet fracture with PCL clearly attached to the displaced fragment
Fig. 3.

CT sagittal cut showing comminuted, displaced PCL avulsion fracture. The proximal fragment is attached to the PCL. The distal fragment is attached to the medial meniscus root. A non-absorbable suture was placed into the meniscus root and the suture placed into a knotless anchor on the posterior tibial cortex. The PCL fragment was ultimately secured with a screw and washer
Management
There are currently a variety of treatment approaches for PCL avulsion fractures, with none emerging as a gold-standard surgical technique [15, 16]. Treatment options depend on the type and size of the fracture, the amount of displacement, comminution, and concomitant injuries [14]. Since most PCL injuries occur in young, active patients, it is generally recommended that a displaced avulsion fracture should be reduced and fixed in a timely fashion to stabilize the joint and prevent nonunion [17]. Zhao et al. suggested nonoperative treatment can be successfully utilized in fractures displaced less than 5 mm [12]. Additionally, regardless of the displacement, posterior translation of the tibia in 90° of flexion with posterior drawer should be less than 10 mm [18].
Nonoperative management of avulsion fractures relies on restoration of the tibiofemoral relationship achieved with immobilization followed by physical rehabilitation. In a comprehensive review of nonoperative and operative rehabilitation protocols after PCL injury, Pierce et al. suggested a three-phase protocol [19]. In the first 6-week phase, immobilization and limited weight bearing can be achieved using a cylindrical cast in 15° of flexion or with posterior support preventing subluxation of the tibia, with the use of an extension or dynamic anterior drawer brace [20, 21]. Quadriceps strengthening and hamstring stretching are emphasized. During the second phase, full weight bearing is resumed with continued strengthening and range of motion exercises. Twelve weeks following the injury, the third phase is focused on return to pre-injury athletic activities [19].
Operative Approach
A simplified posterior approach first described by Burks and Schaffer in 1990 has become the standard open approach to the PCL avulsion fracture [22]. The patient is placed in the prone position with the knee flexed to 30°. A gentle, inverted L incision is made along the flexion crease, continuing toward the medial gastrocnemius through skin and fascia. The interval between the medial gastrocnemius and semimembranosus is bluntly dissected, exposing the capsule, which is vertically incised. The tibial attachment of the PCL is now exposed while the neurovascular bundle is protected by the medial gastrocnemius, which is retracted laterally. Alternatively, the gastrocnemius may be split to allow more access laterally [23], or a midline incision can be utilized [24, 25]. Fixation may be obtained with screws with or without washers, wire fixation, or suture fixation.
More recently, Gavaskar et al. described a minimally invasive approach utilizing the interval between the two heads of the gastrocnemius [26]. In their cohort of 22 patients, they reported stable fixation and no complications utilizing a minimally invasive approach centered over the intersection of the tibial eminence and a transverse line 1 cm proximal to the tibial articular surface obtained using fluoroscopy. Following the approach, one to two cannulated screws and washers were placed.
Despite the success with open fixation, arthroscopic fixation has gained more popularity in the recent years due to the potential decrease in patient morbidity and to aid those unfamiliar or inexperienced with the open approach. Advantages of the arthroscopic technique include diagnosis and treatment of associated ligament injury, meniscal, and chondral injuries [27•]. Various techniques have been described that differ in arthroscopic portals, tibial tunnels, and the type of fixation used. Cannulated screws, tension band wires, K-wires, anchors, sutures, and suspensory fixation methods have been described [1•].
Surgical Outcomes
Several studies have performed retrospective comparisons of open versus arthroscopic surgical approaches [27•, 28]. Ling et al. reported on a randomized study with a small sample size that evaluated open screw fixation with or without arthroscopy (n = 13, n = 16) at a mean follow-up of 46 months. One or more concomitant intra-articular injuries were identified in 84.6% of cases in the arthroscopy group. No significant difference in postoperative range of motion, Lysholm score, or KT-1000 instrumented STS laxity was identified. There were significant differences in residual knee pain at final follow-up in the arthroscopy group (25%, n = 4) compared with control group (7%), n = 1. Of note, prior to final evaluation, two patients in the non-arthroscopy group, classified as pain free at the final evaluation, underwent arthroscopic treatment in the interim. However, these findings must be interpreted with caution given the small sample size and the fact that even the patients that were treated with arthroscopy had fixation through an open approach. Sabat et al. provided a retrospective review of patients with PCL avulsion fractures treated with arthroscopic suture fixation versus open screw fixation [27•]. At 1 year follow-up, laxity measurements favored arthroscopic management while Lysholm, Tegner activity, IKDC scores and one-leg hop test were similar between the two groups. Both of these studies had similar rates of return to sports, which may put into question significance of reported laxity and unaddressed intra-articular pathology in open cases. However, Pardiwala et al. noted need for a second stage arthroscopy between 6 and 19 months in 50% of patients with preoperative intra-articular pathology whose PCL avulsion injuries were treated via open approach [8•]. In a recent systematic review by Hooper et al. in 28 studies with a total of 637 patients, those treated arthroscopically had better IKDC grade A scores and higher return to pre-injury activity. However, this conclusion should be interpreted with caution as only a few of the included studies reported these outcomes. Lysholm scores were comparable between the arthroscopic (95) and open (92.8) groups [1•].
Zhu et al. reported on a series of 16 patients treated arthroscopically using high-strength suture and 4.5 mm tunnels medial and lateral to the tibial tubercle. The sutures were passed around the tibial insertion of the PCL and tied over the tibial tubercle. In their series after 13.6 months follow-up, Lysholm scores were 95.2 and all patients regained preinjury activity level. One patient required manipulation under anesthesia at 6 weeks after surgery. No other complications were reported [29].
Khatri et al. reported on a series of 27 patients treated with open reduction and internal fixation at a mean follow-up of 22 months. Mean postoperative Lysholm score was 90.8. Twenty patients had grade 1 laxity, and seven patients had grade 2 laxity. However, the authors did not find statistically significant difference between residual laxity and functional outcomes. They used an immediate range of motion protocol. In this series, two patients required manipulation under anesthesia, but both had a delay in treatment secondary to medical complications [30].
The most common complication reported in both open and arthroscopic techniques is arthrofibrosis, which is more frequently reported with the arthroscopic approach (0–36%) vs open approach (0–25%) [1•]. Delays in surgical treatment and commencement of range of motion have been reported as risk factors [24, 30]. It is therefore important to achieve stable fixation to avoid prolonged immobilization. This, however, may be challenging in comminuted fragments where suture fixation is used. Symptomatic hardware necessitating removal has also been reported [8•, 31]. Nonunion and postoperative infection rates are similar between the two approaches [1•].
Delayed presentation
If left untreated, long-term PCL avulsion fractures may lead to malunion, nonunion, or instability [10]. Early studies in the literature did not achieve satisfactory results [25, 32]. However, more recently, better outcomes have been attained [33–35]. In the few published small series, residual sagittal instability is common; however, resolution of symptoms and good to fair outcomes are achieved despite these observations [33, 34]. Singla et al. reported a 10-point mean Lysholm score improvement from 82 preoperatively to 92 postoperatively in their series [34]. This outcome is comparable to those achieved with acute fixation of PCL avulsion fractures. Those patients with symptomatic nonunion can be treated with open fixation or PCL reconstruction, similar to that of the anterior tibial avulsion which can be seen with anterior cruciate ligament avulsions.
Pediatric patients
PCL avulsion fractures are very rare in the pediatric population. Reports of successful nonoperative treatment of up to 7 mm of displacement have been described [36]. However, the diagnosis is often delayed or missed because examination of the knee can be non-specific. Additionally, the injury may not be recognized on radiographs secondary to an open proximal tibial physis, insufficient ossification of the fragment, and low suspicion of the injury due its rarity. If suspected, radiographic comparison to the contralateral joint, stress views, and further imaging with MRI should be considered [37]. Acute treatment of avulsion fractures has been reported with favorable outcomes using open reduction and internal fixation, primary repair, pullout suture repair, and bio-absorbable suture anchor [37]. Despite some case reports with unsuccessful treatment of subacute PCL avulsion fractures [38, 39], most authors recommend surgical treatment [17, 33, 37].
Authors preferred treatment method
Nondisplaced or minimally displaced PCL avulsion fractures can be treated nonoperatively, regardless of whether or not they are associated with other ligamentous injuries. In the case of a multiple-ligament injury that requires early fixation of other structures, we will typically treat the fracture nonoperatively with liberal use of a PCL brace, keeping the patient locked in full extension for 3 weeks and avoiding active hamstring contraction that can bring the tibia posteriorly. After 3 weeks, we begin a range of motion protocol and discontinue the PCL brace at the 6-week time point. At 3 months postoperatively, images are obtained (or, if imaging is difficult, one can consider a low-dose CT scan) to assess for fracture healing followed by a return to sport protocol. In the case of isolated PCL fractures, patients can expect to return to full sport by 4–6 months after the injury. However, in the case of the multi-ligament injury, the other injuries typically are the rate-limiting factor regarding return to play.
We prefer operative fixation for any displaced PCL tibial facet fracture. For the treatment of tibial-based PCL avulsion fractures, options consist of arthroscopic-assisted versus open fixation. In our experience, open reduction through a posteromedial approach offers a reproducible, reliable method for obtaining direct compression with anatomic fixation.
Although arthroscopic-assisted fixation is certainly a reasonable option, we prefer open reduction as we can directly visualize the fragment and directly assess the reduction. We find that even with good arthroscopic visualization plus or minus the use of a posteromedial portal or a 70° arthroscope, it is difficult to perfectly assess the reduction. What seemingly may be a perfect reduction intraoperatively via the arthroscope may ultimately be non-anatomic and lead to malunion or residual posterior laxity. In addition, in the treatment of comminuted fractures that may involve the meniscus root insertion on a separate fragment, the open posterior approach allows direct visualization of these fragments as well, which can be fixed with suture anchor constructs or trans-tibial fixation.
For fixation of these PCL avulsion fractures, we place the patient in the prone position under general anesthesia with all bony prominences well-padded and a tourniquet placed high on the thigh. Prior to positioning, a well-documented, thorough exam under anesthesia plus or minus the assistance of fluoroscopy is used to confirm or refute the existence of multi-ligamentous instability. We begin the procedure by making a posteromedial curvilinear incision, beginning about 6 cm distal to the joint line, extending proximal and then curving more horizontal by the popliteal crease. Typically, one does not need to extend the incision more proximal to the popliteal fossa, but in the case of difficult exposure or concern about the whereabouts of the neurovascular bundle, this is certainly an acceptable option and is done with proximal extension of the lateral aspect of the incision. For surgeons unfamiliar with the location of the bundle or the approach, it may be helpful to have a vascular surgeon assist with the approach.
The plane between the medial head of the gastrocnemius and the semimembranosus is then developed. A retractor is placed under the gastrocnemius which is reflected laterally (Fig. 4), protecting the neurovascular bundle. In cases of difficult exposure or a tight gastrocnemius that may be preventing exposure, it is acceptable to release the gastrocnemius proximally and repair it at the end of the case. We have done this several times with no detrimental effect on the patient.
Fig. 4.
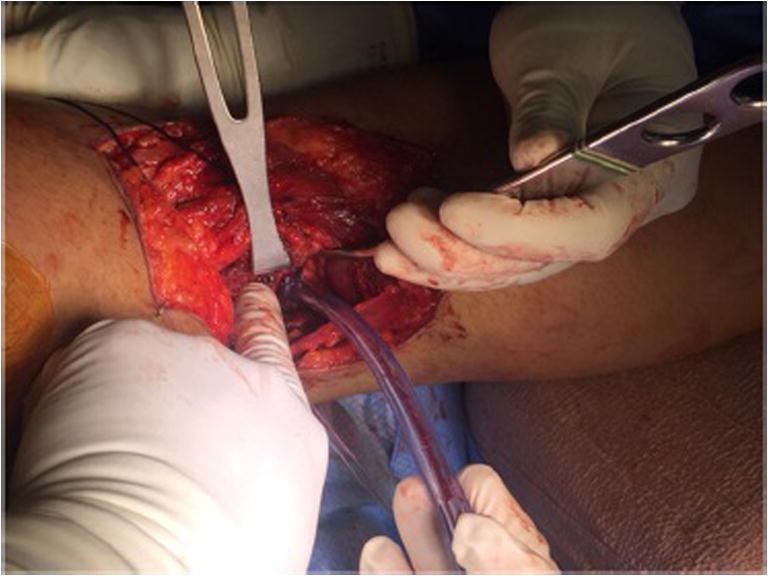
Open posterior approach for reduction of PCL avulsion fracture through an extensile approach (proximal is to the left and medial is on the bottom of the page). Please note the use of the retractor to pull the medial gastrocnemius laterally, protecting the neurovascular bundle. The screw and washer can be seen in the fragment just next to the retractor
With reflection of the gastrocnemius comes exposure of the posterior joint capsule. Occasionally, there is a branch of the middle geniculate artery which lies on the capsule that needs to be ligated or cauterized for hemostasis. A longitudinal capsulotomy is then made, and a small self-retaining retractor or two small Hohmann retractors can be placed inside the joint to provide exposure of the fracture fragment.
Once the fragment is isolated and the fracture pattern established, the fracture site is irrigated and the clot is debrided. The fracture is reduced and held in place with a dental pick or a K-wire such that there is ample room for the placement of a 4.0-mm cancellous screw (Fig. 5). A partially threaded, unicortical cancellous screw is then placed in lag mode with a small washer, perpendicular to the fracture site, obtaining compression and fixation. We find one screw is ample fixation as many times the fragment is too small to accommodate two screws. However, if fragment size is sufficient, we will place two screws to provide more rotational control. The tourniquet is then deflated, hemostasis is assessed, and the incision closed in layers. The patient is turned supine and then placed into a PCL brace to prevent posterior tibial displacement.
Fig. 5.

Fluoroscopic postoperative image showing anatomic reduction of PCL facet fracture using a screw and washer
Postoperatively, we endorse foot-flat weight bearing and allow for passive range of motion immediately under the supervision of physical therapy. Active hamstring activation is minimized for the first 3 weeks after surgery, and we begin full weight bearing at 6 weeks postoperatively. We allow running at 3 months under the supervision of physical therapy. As this is a bony injury, we expect that healing would occur rapidly and allow sport-specific exercises at 4–5 months postoperatively, with return to sport between 6 and 9 months depending on strength, range of motion, proprioception, and pain-free status.
Conclusion
PCL avulsion fractures are rare injuries that can lead to significant morbidity when not recognized and treated properly. Patients should be counseled on the presence of other intra-articular pathology. Although traditionally treated with open reduction and internal fixation, more recent studies show successful outcomes with both the open and arthroscopic-assisted treatment.
Conflict of Interest
All authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on PCL Update
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.• Hooper PO. Management of posterior cruciate ligament tibial avulsion injuries: a systematic review. Am J Sports Med. Most complete and upto date systematic review of outcomes of open and arthroscopic approaches to PCL avulsion fractures. This paper eveluates 28 studies from 1975 to the date of publication. They conclude that similar outcomes are achieved with both techniques. Arthroscopic approach allows for treament of concomitant intraarticular pathology.
- 2.Barros MA. Surgical treatment of avulsion fractures at the tibial insertion of the posterior cruciate ligament: functional result. Rev Bras Ortop (English ed.). 50(6):631–7. [DOI] [PMC free article] [PubMed]
- 3.Fanelli GC. Posterior cruciate ligament injuries in trauma patients: Part II. Arthroscopy. 11(5):526–9. [DOI] [PubMed]
- 4.Janousek AT. Posterior cruciate ligament injuries of the knee joint. Sports Med (Auckland). 28(6):429–41. [DOI] [PubMed]
- 5.Mariani PP. Surgical treatment of posterior cruciate ligament and posterolateral corner injuries. An anatomical, biomechanical and clinical review. Knee. 10(4):311–24. [DOI] [PubMed]
- 6.Petrigliano FA. Isolated posterior cruciate ligament injuries of the knee. Sports med Arthrosc Rev. 14(4):206–12. [DOI] [PubMed]
- 7.Joshi S. Open reduction and internal fixation of isolated posterior cruciate ligament avulsion fractures: clinical and functional outcome. Knee Surg Relat Res. 2017;29(3):210–216. doi: 10.5792/ksrr.17.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pardiwala DN, Agrawal D, Patil V, Saini U, Dhawal P. Paper 133: comparison of open versus arthroscopic fixation for isolated PCL tibial bony avulsions. A prospective randomized study with minimum 2 year follow up. Arthroscopy. 2012;28(9):e413–e414. doi: 10.1016/j.arthro.2012.05.616. [DOI] [Google Scholar]
- 9.Parkkari J. The risk for a cruciate ligament injury of the knee in adolescents and young adults: a population-based cohort study of 46 500 people with a 9 year follow-up. Br J Sports Med. 42(6):422–6. [DOI] [PubMed]
- 10.Gwinner C. All-arthroscopic treatment of tibial avulsion fractures of the posterior cruciate ligament. GMS. Interdiscip Plast Reconstr Surg DGPW. 2016:5. [DOI] [PMC free article] [PubMed]
- 11.Griffith JF. Cruciate ligament avulsion fractures. Arthroscopy. 20(8):803–12. [DOI] [PubMed]
- 12.Zhao J. Arthroscopic treatment of acute tibial avulsion fracture of the posterior cruciate ligament with suture fixation technique through Y-shaped bone tunnels. Arthroscopy. 22(2):172–81. [DOI] [PubMed]
- 13.Dhillon MS. Posterior cruciate ligament avulsion from the tibia: fixation by a posteromedial approach. Acta Orthop Belg. 69(2):162–7. [PubMed]
- 14.White EA. Cruciate ligament avulsion fractures: anatomy, biomechanics, injury patterns, and approach to management. Emerg Radiol. 2013;20(5):429–440. doi: 10.1007/s10140-013-1121-0. [DOI] [PubMed] [Google Scholar]
- 15.Chen C-H. Surgical treatment of posterior cruciate ligament injury. Chang Gung Med J. 30:480–92. [PubMed]
- 16.Malempati C. Current arthroscopic concepts in repairing posterior cruciate ligament tibial-sided avulsions. Orthopedics (Thorofare, N.J.). 38(9):563–9. [DOI] [PubMed]
- 17.Hoogervorst P. Pseudo-arthrosis repair of a posterior cruciate ligament avulsion fracture. Knee Surg Sports Traumatol Arthrosc. 18(11):1612–6. [DOI] [PMC free article] [PubMed]
- 18.Veltri. Isolated and combined posterior cruciate ligament injuries. J Am Acad Orthop Surg. 1(2):67–75. [DOI] [PubMed]
- 19.Pierce CM. Posterior cruciate ligament tears: functional and postoperative rehabilitation. Knee Surg Sports Traumatol Arthrosc. 21(5):1071–84. [DOI] [PubMed]
- 20.Jung YB. Active non-operative treatment of acute isolated posterior cruciate ligament injury with cylinder cast immobilization. Knee Surg Sports Traumatol Arthrosc. 16(8):729–33. [DOI] [PubMed]
- 21.Meyers MH. Fracture of the intercondylar eminence of the tibia. J Bone Joint Surg (Am Vol). 52(8):1677–84. [PubMed]
- 22.Burks RT. A simplified approach to the tibial attachment of the posterior cruciate ligament. Clin Orthop Relat Res. (254):216–9. [PubMed]
- 23.Jazayeri SM. A safe postero-medial approach to posterior cruciate ligament avulsion fracture. Knee Surg Sports Traumatol Arthrosc. 17(3):244–7. [DOI] [PubMed]
- 24.Nicandri GT. Treatment of posterior cruciate ligament tibial avulsion fractures through a modified open posterior approach: operative technique and 12- to 48-month outcomes. J Orthop Trauma. 22(5):317–24. [DOI] [PubMed]
- 25.Trickey EL. Rupture of the posterior cruciate ligament of the knee. J Bone Joint Surg Br Vol. 50(2):334–41. [PubMed]
- 26.Gavaskar AS. A novel MIS technique for posterior cruciate ligament avulsion fractures. Knee. 24(4):890–6. [DOI] [PubMed]
- 27.• Sabat D. Displaced posterior cruciate ligament avulsion fractures: a retrospective comparative study between open posterior approach and arthroscopic single-tunnel suture fixation. Arthroscopy. 32(1):44–53. Retrospective comparison of 47 patients treated with open reduction and internal fixation and suture fixation with an arthroscopic approach. At one year follow up, over 90% of patients in both groups had normal or nearly normal functional outcome scores, but arthroscopic group had less residual laxity. [DOI] [PubMed]
- 28.Ling HM. Arthroscopy in avulsion fracture of posterior cruciate ligament. Chang Gung Med J. 24(5):313–7. [PubMed]
- 29.Zhu W. Treatment of tibia avulsion fracture of posterior cruciate ligament with high-strength suture fixation under arthroscopy. Eur J Trauma Emerg Surg (Munich) 2007;43(1):137–143. doi: 10.1007/s00068-015-0606-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Khatri K. Posterior cruciate ligament Tibial avulsion treated with open reduction and internal fixation through the Burks and Schaffer approach. Malays Orthop J. 2015;9(2):2–8. doi: 10.5704/MOJ.1507.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yang C-K. Surgical treatment of avulsion fracture of the posterior cruciate ligament and postoperative management. J Trauma. 54(3):516–9. [DOI] [PubMed]
- 32.Kennedy JC. The posterior cruciate ligament. J Trauma. 7(3):367–77. [DOI] [PubMed]
- 33.Torisu T. Isolated avulsion fracture of the tibial attachment of the posterior cruciate ligament. J Bone Joint Surg (Am Vol). 59(1):68–72. [PubMed]
- 34.Singla R. Fixation of delayed union or non-union posterior cruciate ligament avulsion fractures. J Orthop Surg (Hong Kong) 2014;22(1):70–74. doi: 10.1177/230949901402200118. [DOI] [PubMed] [Google Scholar]
- 35.Chiarapattanakom P. Isolated PCl avulsion from the tibial attachment: residual laxity and function of the knee after screw fixation. J Med Assoc Thail. 92(Suppl 6):S181–8. [PubMed]
- 36.Hurni Y. Pediatric posterior cruciate ligament avulsion fracture of the tibial insertion: case report and review of the literature. Surg J (New York). 3(3):e134–8. [DOI] [PMC free article] [PubMed]
- 37.Jang K-M. Delayed surgical treatment for tibial avulsion fracture of the posterior cruciate ligament in children. Knee Surg Sports Traumatol Arthrosc. 24(3):754–9. [DOI] [PubMed]
- 38.Trickey EL. Injuries to the posterior cruciate ligament: diagnosis and treatment of early injuries and reconstruction of late instability. Clin Orthop Relat Res. (147):76–81. [PubMed]
- 39.Kim SJ. Arthroscopically assisted treatment of avulsion fractures of the posterior cruciate ligament from the tibia. J Bone Joint Surg Am Vol. 83-A(5):698–708. [DOI] [PubMed]


