Abstract
Purpose of Review
Summarize classic and recent information regarding the unique subset of ankle fractures in children with open growth plates and share the authors’ decision-making and surgical techniques.
Recent Findings
Recent research on pediatric ankle fractures has centered on the accurate prediction and prevention of growth arrest following fractures of the distal tibia. Another source of discussion is the necessity and benefit of CT scanning in classification and treatment approach.
Summary
Pediatric ankle fractures continue to pose clinical challenges for orthopedic surgeons. While open anatomic reduction and internal fixation continue to produce good outcomes for intra-articular fractures, outcomes of physeal injuries are more difficult to predict. More studies are needed to determine which patients may benefit more from surgical treatment of physeal injuries.
Keywords: Pediatric ankle fractures, Physeal fracture, Distal tibial fracture, Distal tibial physeal fracture
Introduction
Pediatric ankle fractures, defined for the purposes of this review as injuries of bones with open physes affecting the tibia and fibula distal to the metaphysis, have unique biological and mechanical attributes that create fracture patterns and treatment dilemmas different from adults. While certain treatment goals such as reestablishment of articular congruency and functional alignment to avoid untimely arthritis are common to both groups, the protection and sustenance of the physis is a priority in younger children.
The distal tibial physis, supplying 45% of the length of the tibia, is third among the most commonly injured growth plates [1–3] and estimated to account for 11–38% of physeal injuries [4•, 5]. Contrary to the upper extremity physes, however, the distal tibial physis does not take lightly to being injured with growth arrest rates up to 66.7% reported in previous literature [6•,7–8]. Due to the strong ligaments in childhood, injuries that would cause sprains in adulthood are thought to cause physeal fractures in the pediatric population. The most common mechanism of injury in pediatric ankle fractures is a twisting mechanism incurred during a ground-level fall, as may be observed when missing a step on a stair or during sports. However, higher energy mechanisms may also cause fracture: axial compression as in falls from a height, crush injuries, and open fractures with bone loss caused by lawnmowers.
Particular care should be taken to verify history corresponds to examination findings; non-specific falls in a toddler a few days before the inability to weight-bear may not be the culprit at all, and the differential diagnosis in younger children should include hematogenous osteomyelitis and several types of tumor [9]. Non-accidental trauma in very young children may present with so-called metaphyseal corner fractures of the tibia, which are considered highly suspicious for non-accidental trauma (Fig. 1) [10].
Fig. 1.

A metaphyseal corner fracture in the process of healing. This fracture was discovered during the non-accidental trauma work-up of a 2-month-old infant who presented with unexplainable lethargy (special thanks to Dr. Amisha Shah, personal collection)
Children and adolescents with ankle fractures will present with immediate onset of pain after trauma and exacerbation of pain with weight-bearing. There may be swelling or bruising of the skin, usually consistent with the amount of energy transferred during injury, and therefore correlating with the severity of injury. The skin must be examined closely to rule out open fracture. Areas of severe skin contusion and blistering, which may occur in the setting of excessive swelling, should be noted as they may influence the placement of surgical incisions later on. Significant displacement will cause visible deformity and may interfere with the vascular supply of the foot. Both major pulses to the foot, the tibialis posterior and the dorsalis pedis, should be palpated and capillary refill assessed at presentation. A complete neurological examination of the lower extremity distal to the injury includes superficial sensation on the dorsal and plantar aspects of the foot. Points of maximal tenderness will be the clue to understand injury.
Examination with palpation is important in the differentiation of ankle sprains from fractures and diagnosing associated fractures. Tenderness on bony prominences indicates physeal injury or bony fracture whereas ligamentous tenderness is more frequent in sprains. Palpation should be taken above the ankle to the knee to rule out high fibular fractures (Maisonneuve fracture) and below for fifth metatarsal or midfoot fractures.
Compartment syndrome is rare following ankle fractures but may occur. Clinicians should remain vigilant for the clinical symptoms of compartment syndrome. The extensor retinaculum syndrome may occur in a subset of patients where excessive translation of fragments causes compression of the structures in the anterior aspect of the ankle, most notably the deep peroneal nerve. Findings are pain out of proportion to the injury, hypoesthesia or anesthesia of the first web space, and weakness of toe extensors [11, 12]. Extensor retinaculum syndrome must be addressed expediently with a surgical release.
Imaging
While there are clinical guidelines in research regarding the appropriateness to order radiographs [13, 14], the cost and radiological burden of three views of the ankle are low, and in most North American centers, radiographs are obtained on a routine basis for pediatric foot and ankle trauma. Anteroposterior, lateral, and mortise views of the ankle should be obtained with the ankle in the neutral position, and where possible, weight-bearing views of the ankle can be performed to rule out syndesmotic injury [15]. Radiographs should be reviewed with special care given the appearance of the physis, and widening here should be ruled out. Stress views of the ankle are usually not obtained routinely; however, in certain patterns, they may be helpful in assessing stability and may yield clues to the extensiveness of the injury. Gravity stress views or weight-bearing views may be better tolerated than the standard external rotation view [15].
The treating physician should have a low threshold for obtaining CT scans in pediatric ankle fractures. The concern for radiation exposure has been previously addressed, and a standard ankle CT is estimated to be equivalent to the dose received by 0.9 chest radiographs [16]. Especially in fractures involving the joint surface, CT can provide invaluable information and has been shown to change surgical indications as well as surgical strategy [17–20]. MRIs of the ankle can provide further information to soft tissue structures about the ankle and the health of cartilage [21], but are often prohibitive in price and availability to achieve mainstream use in the treatment of acute ankle fractures.
Classification
The most commonly utilized classification for pediatric ankle fractures is the time-renowned Salter-Harris classification [22, 23]. Briefly, in Salter-Harris (SH)-I injuries, the fracture line extends transversely across the physis (Fig. 2). In SH-II fractures, the fracture line extends to a variable degree transversely across the physis and then changes direction to exit metaphyseally, creating the so-called Thurston-Holland (TH) fragment (Fig. 3). In SH-III fractures, the fracture line begins in the epiphysis, travels toward the physis, and exits through the physis. In SH-IV fractures, the fracture extends vertically across the physis, involving the epiphysis and metaphysis both. SH-V injuries are often underappreciated at the time of injury and are thought to be caused by axial compression of the physis, resulting commonly in growth arrest. A sometimes added type is the SH-VI, which, as sometimes happens in open fractures, is when a portion of the growth plate is missing. The commonly accepted rule is that severity of growth plate fractures increases with the Salter grade, and so do their most feared complication, premature physeal closure.
Fig. 2.

A classic Salter-Harris-I fracture of the distal tibia
Fig. 3.
Salter-Harris-II fracture of the distal tibia and fibular shaft fracture in a 12-year-old male (a, b). The patient underwent closed reduction and long-leg casting. Post-reduction radiographs did not allow adequate assessment of the physis (c, d), so a CT scan was performed (e, f). Physeal widening on the sagittal images was measured as 2 mm, and decision was made for conservative treatment. Radiographs at 6 months are not conclusive for continued growth at the physis; however, growth is going to be monitored for 2 years post-injury or until symmetric growth arrest lines are observed (g, h)
Dias and Tachdjian classified pediatric ankle fractures depending on the position of the foot in relationship to the force applied [24]. A supination inversion injury was thought to cause an SH-I injury of the fibula and a SH-IV injury of the medial malleolus, in essence a bimalleolar fracture of the ankle. Supination and external rotation are thought to cause distal metadiaphyseal fractures not involving the growth plates. Pronation-eversion and external rotation was noted to cause a high fibular fracture and a SH-II fracture of the distal tibia with the TH fragment located posterolaterally. Supination and plantarflexion were thought to cause the classic SH-II fracture of the distal tibia with the TH fragment posteriorly, with or without fibular involvement. Other classifications of pediatric ankle injuries exist, although they are not as commonly utilized in clinical practice [25].
Another subgroup of pediatric ankle fractures is the so-called transitional fractures. These occur in a very specific time window, during the progressive closure of the distal tibial physis [26]. The average age for girls of distal tibial physeal closure is 12–15, whereas in boys it is 14–18 years. There is a distinct pattern to the closure of the distal tibial physis, which begins centrally, proceeds to the medial aspect of the physis, and finishes with the lateral aspect, a sequence that takes approximately 18 months to complete. This allows a distinct pattern of injury depending on where the patient is in this pattern of closure. Patients in the earlier phases of closure often present with triplane fractures, whereas those in the later phases where only the lateral aspect of the physis is open present with Tillaux fractures. Triplane fractures are defined as three-dimensionally complex fractures affecting the distal growth plate of the tibia, extend intra-articularly, and appear to have different SH grades on different radiographic projections (i.e., a SH-IV injury in the antero-posterior radiograph and a SH-II in the lateral) (Fig. 4) [27]. The Tillaux fracture is an avulsion of the fragment where the anterior tibiofibular ligament originates and usually occurs with an external rotation mechanism (Fig. 5). In both triplane and Tillaux fractures, as the growth plate is in its natural process of closure, there usually is no consequence of physeal arrest due to the fracture. Often, both distal tibial growth plates have completed closure by the time the patient has completed the acute treatment process (3–6 months).
Fig. 4.
A 12-year-old female sustained this triplane fracture due to a twisting injury while playing lacrosse. a–d AP radiograph reveals a SH-IV injury whereas on lateral a SH-II injury is appreciated, typical for triplane fractures. CT scans revealed more than 2 mm of gapping at the fracture line; for this reason, the patient was indicated for operative fixation. 6.5 cannulated screws were utilized to compress the posterior malleolar fracture first, followed by open reduction of the joint line and fixation of the latter by a 4.5 cannulated screw (h, i). Six months post-injury, fracture is healed and growth plates are closing (j, k). Patient has full range of motion compared to the opposite ankle and has resumed sports at her pre-injury level
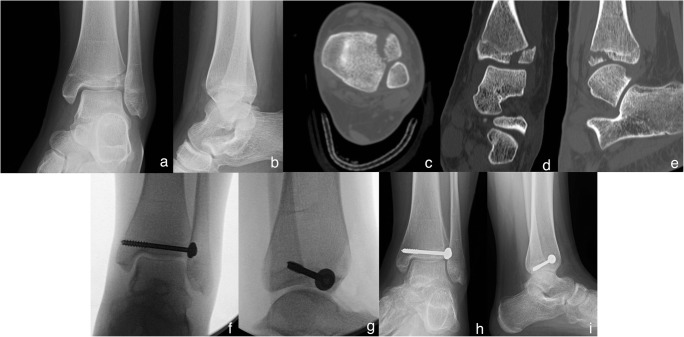
Fig. 5.
This 12-year-old female sustained this Tillaux fracture due to a missed step going down the stairs (a, b). The patient was short-leg casted and underwent CT scanning, which revealed unacceptable fracture gap at the joint (c–e). Note on CT closure of the medial and posterior areas of the growth plate. She underwent open reduction and fixation with a single cannulated screw (f, g). At her 3-month follow-up, complete physeal closure about the ankle is noted (h, i)
Management
The goal of treatment in pediatric ankle fractures is to reestablish joint congruency and the ankle mortise, lower extremity alignment, and physeal anatomy and thus preserve pain-free ankle function well into adulthood. Several considerations enter the equation when making treatment decisions for ankle fractures in children, and all should take into account the presence of the physis. Children who have sustained ankle fractures and have more than 3 years of growth remaining should be monitored for growth arrest with serial biannual or annual radiographs until symmetric growth can be seen. Most treatment decisions are based on the distal tibial component and the status of the syndesmosis; fibular fractures in isolation are rarely an indication for operative treatment at our institution.
Non-displaced fractures regardless of classification are treated conservatively with appropriate immobilization and protected weight-bearing. Serial radiographs every 1–2 weeks for the first 3 weeks should be considered to rule out late displacement in cast. We generally complete cast treatment in 4–6 weeks depending on patient age and fracture type, and then allow weight-bearing in a fracture boot.
Displaced fractures should undergo an attempt at closed reduction. At our institution, this is generally performed under conscious sedation. As a rule, as repetitive closed reduction attempts may cause damage to the physis, therefore, no more than two attempts should be undertaken. We prefer a long leg cast for significantly displaced distal tibial SH-I or SH-II fractures as we believe this allows for better rotational control. Post-reduction radiographs are obtained and alignment and physeal reduction evaluated. If post-reduction radiographs are too low quality to fully appreciate these in satisfactory detail, we will obtain CT scanning and three-dimensional reconstructions. If reduction is satisfactory, the cast is bivalved and the patient discharged with standard NWB and elevation precautions. Radiographs are obtained at 5–7 days to verify reduction is maintained; loss of reduction is exceedingly rare. The cast is overwrapped at this visit. At the 10–14-day visit, the cast is often trimmed to a short leg. It is removed at 4–6 weeks and the patient placed in a walking boot and allowed to progressively weight-bear. We do not routinely refer to outpatient PT but will prescribe self-directed ankle ROM exercises with and without resistance bands. Low-impact weight-bearing activities are encouraged. Return to sport is allowed after restoration of near-normal/symmetric range of motion and in excess of 4+/5 strength in major muscle groups, usually at 3–4.5 months post-injury.
If post-reduction radiographic examinations reveal unacceptable alignment (> 5° of varus/valgus, > 10° of ante/recurvatum) and/or physeal widening < 3 mm, we determine the amount of growth remaining in the child [28]. In children with > 3 years of growth remaining, we will usually observe alterations in alignment to that degree. In children with < 3 years of growth remaining, we will usually observe physeal widening as no significant clinical impact of possible growth arrest is expected. In children with < 3 years of growth remaining and unacceptable alignment, or > 3 years of growth remaining and physeal widening, surgical treatment is often considered. While alignment can be addressed with closed reduction and often percutaneous pinning, physeal widening requires an open approach to the area of concern. Coronal and sagittal images of the CT are especially helpful in this regard; periosteal entrapment is often found at the site of physeal widening. A small incision centered in this area is conducive for removing the periosteum and achieving anatomic reduction. Fixation is then performed with screws outside the physis (utilizing the TH fragment) or, if not possible, smooth, stainless pins across the physis. Unfortunately, previous studies have not shown a reliable reduction of premature physeal arrest (PPA) even with meticulous surgical reduction of the physis [29].
Fractures that involve the weight-bearing surface of the tibia and are displaced are also initially addressed with closed reduction and casting. Very distal fractures such as Tillaux fractures are usually placed in a short leg cast, whereas intra-articular fractures involving the metaphysis and thought to have a rotational component are placed in a long leg cast. A CT is obtained routinely post-reduction and the joint surface inspected. Displacement in excess of 2 mm at the weight-bearing surface of the tibia is considered a surgical indication. For SH-III and SH-IV fractures of the medial malleolus that have 1 mm or more displacement, we will usually recommend surgical fixation due to this particular fracture’s predilection for nonunion and growth arrest [30–32, 33•, 34•].
For Tillaux fractures, closed reduction is attempted with plantarflexion, inversion, and manual pressure on the fragment. Patient is placed in a short leg cast, which is then bivalved. CT scan is obtained. If < 2 mm displacement, it may be treated conservatively. If > 2 mm of displacement, surgical treatment is recommended. With Tillaux fractures, the benefits of open versus closed surgical reduction continue to be discussed. Preoperative planning is performed utilizing CT scanning on all patients. The location of the Tillaux fragment in relation to the plafond should be analyzed. Intraoperative fluoroscopy in various angles should be trialed to find the projection where maximal distraction of the fracture gap is appreciated, usually on an external rotation view. Pure distraction 2–4 mm of drift can often be addressed by lagging across the fracture without a formal open reduction. If there is in excess of 4-mm displacement and/or a rotational component, a percutaneous periarticular reduction clamp can be placed over the fragment and the medial malleolus through stab incisions and reduction attempted. Fractures not amenable to reduction through these techniques are usually addressed through an open approach. As mentioned above, limited incisions are placed over the maximal displacement of the fracture utilizing preoperative CT scans and fluoroscopy projections.
Triplane fractures require more dedicated preoperative planning. Anatomic reconstruction of the joint surface is the primary objective. A common pitfall in triplane fractures is to address fragments in the wrong sequence, over-compress a fracture line, and as a result be unable to reduce the joint line. For this reason, we prefer to fix fragments with joint components first and metaphyseal fragments later. Again, fragments with 2–4 mm of distraction often do not require open reduction but can be addressed with lag by design. In fractures with shortening of the posterior fragment, fibular fixation can be considered to obtain length. We utilize 4.5-mm cannulated screws for epiphyseal fixation. We have found that 6.5-mm cannulated screws in the tibial metaphysis work very well to compress larger fragments. In fractures with an SH-4 component posteriorly that is displaced proximally, a limited posterolateral approach to the tibia can facilitate reduction. A cannulated screw can perform in an anti-glide fashion to aid temporary reduction. We also make copious use of periarticular clamps through stab incisions to aid percutaneous reduction (Fig. 6).
Fig. 6.
This triplane fracture in this 13-year-old female was sustained due to a fall (a, b). She was closed reduced under sedation and casted (c, d), then a CT scan obtained (e–g). Due to the proximal displacement of the posterior malleolar piece as noted on CT scan (f), decision was made to proceed with a posterolateral approach to the distal tibia and push fragment distally. An anti-glide screw was placed at the tip of the fracture line in anti-glide fashion (h). This was performed without drilling to allow the screw’s mass to push the fragment downward. Attention was then turned to the joint line without rigid fixation of the posterior piece to avoid over compressing the joint line and failing with reduction of the lateral joint fragment. Several projections were trialed to find this semi-external rotated view where the fracture line was noted to be most prominent (i). A large periarticular fracture clamp was then applied percutaneously and adequate reduction could be seen on fluoroscopy (j). The joint was fixed utilizing a 4.5 cannulated screw which lagged the fracture further (k, i). Finally, the posterior piece was fixed utilizing a 6.5 cannulated screw (l). Final radiographs reveal adequate joint line reduction (m–p)
Ankle fractures that are treated operatively in our institution are placed in a short leg cast that is bivalved in the operating room to accommodate swelling. Patients return to the office in 10–14 days for a wound check and cast change. They are kept non-weight-bearing for 6 weeks, at which time the cast is discontinued, radiographs are obtained, and a CAM boot is provided. They begin weight-bearing with the CAM boot and are prescribed self-directed ankle exercises. At the 12th-week follow-up, CAM boot is discontinued and patients with near-normal range of motion and adequate muscle strength are allowed to return to low-impact physical activity. Full-contact and high-impact activities are usually allowed at 4.5 months post-operatively.
Fibular Fractures
Fibular fractures in isolation are often non- or minimally displaced. These are generally treated with immobilization and protected weight-bearing. Fibular fractures accompanying displaced fractures of the distal tibia may be included in surgical planning for mainly two reasons: (1) to establish length and facilitate tibial reduction and (2) to provide additional fixation. In an ankle where > 3 years of growth is expected, the fibular physis should be respected and if fixation across it is necessary, smooth K-wires utilized. The relationship between the fibula and tibia is not static and changes during growth [35, 36].
Complications
Premature Physeal Closure
Premature physeal closure (PPC) is a significant problem in pediatric ankle fractures. Complete physeal arrest of the tibia may result in leg length discrepancy, whereas partial arrest may cause angular deformities. The physes of the tibia and fibula are often not equally affected, leading to asymmetric growth in the ankle mortise resulting in angular deformities. It has yet to be established how much growth exactly needs to be present for premature physeal closure to cause clinically significant deformity. What is more, despite extensive research on the subject, a decrease in PPC rates with surgical treatment has not been conclusively proven.
Premature physeal closure in the fibula will cause overgrowth of the tibia and often result in a valgus deformity. Overgrowth of the fibula is better tolerated as there is some room for the fibula to migrate proximally; however, the exact amount of overgrowth that can be tolerated is unclear, and fibular impingement may occur. Even with symmetric growth arrest, due to faster longitudinal growth of the fibula proximally compared to the proximal tibia, overgrowth and impingement at the ankle may occur [35].
Aitken in his 1965 paper on growth plate fractures suggested that whether or not clinically significant growth arrest would occur is determined at the time of injury [37•]. Research into PPC since his time has not proven him wrong; while exuberant and repeated attempts at reduction and poor surgical technique can certainly add insult to injury where the physis is concerned, meticulous open reduction has not been proven to reliably alter growth arrest rates in the majority of distal tibial physeal fractures. While anatomical reduction does seem to give the physis a fighting chance in SH-III and SH-IV injuries [31, 38], we believe that mechanism of injury [8, 30], initial displacement [33, 39••], comminution [30], and post-reduction displacement [6•] are more important as these appear to be indications on the severity of the injury to the growth plate. Barmada et al. reported that widening of the physis in excess of 3 mm after a closed reduction attempt was indicative of periosteal entrapment at the physis, and operative removal of this entrapped periosteum resulted in lower growth arrest rates (60 versus 17%) [6•]. We agree with Aitken that physeal arrest is often determined at the time of injury; that being said, we recommend a low threshold for surgical reduction and fixation of SH-III and SH-IV fractures. SH-II fractures continue to pose a dilemma as reliable predictors of growth arrest remain absent. For these patients, we will usually make a case-by-case decision, erring on the surgical side for younger patients who have a great deal of growth remaining. Regardless of treatment chosen, however, children with a history of physeal fracture should be monitored with radiographs every 6–12 months until definitive evidence of the resumption of growth in the form of symmetric Harris growth arrest lines are noted [4•] or natural physeal closure is achieved.
Superficial Wound Complications and Deep Infection
Superficial wound necrosis can be avoided with meticulous management of soft tissues and avoidance of raising flaps especially on the lateral aspect of the ankle. Surgical site infection is quite rare and is managed according to standard principles.
Malunion
Malunion is uncommon. Malunions not affecting the joint are managed with benign neglect if adequate remodeling is likely or standard deformity correction. For malunions involving the joint line, an osteotomy and fixation may be appropriate.
Posttraumatic Arthritis
There is a scarcity of studies with long-term follow-up and clinical outcomes for pediatric ankle fractures. Caterini et al. reported on 68 patients with an average of 27 years of follow-up, 47 of which they classified as having a good result. Of their patients, 11.8% had radiographic signs of osteoarthritis, and the vast majority of these had sustained SH-III or SH-IV injuries. The authors indicated that the type of SH lesion, the amount of initial displacement, and the quality of reduction were the main predictors of result. Transitional fractures in the long term also have generally good outcomes as long as final fracture gap and/or step-off is less than 2–2.5 mm [40••, 41].
Nonunion
While delayed union and nonunion are rare in the pediatric age group, these can be a significant problem in SH-III and SH-IV fractures of the medial malleolus. To minimize this risk, surgical treatment has been recommended for fractures with more than 1 mm of displacement for this particular subset [30–32, 33•, 34•].
Other less common complications including osteonecrosis of the tibial metaphysis following SH-I fractures [42, 43] extensor retinaculum/compartment syndrome [11, 12], reflex sympathetic dystrophy/complex regional pain syndromes [44] have been reported.
Recent Developments and Future Directions
The most significant recent development in pediatric ankle fractures has been the adoption of CT scanning as a routine procedure in triplane fractures. Through a 2015 study by Eismann et al., several qualified observers were asked to classify 25 triplane fractures with radiographs alone and then with CT scans on two separate occasions [19]. After reviewing tomography scans, raters changed the fracture pattern in 46% of ratings, the displacement from < 2 to > 2 mm in 39% of ratings, the treatment from non-operative to operative in 27% of ratings, and either the orientation or number of screws in 41% of ratings. The authors concluded that CT scans had a definitive impact on fracture classification, displacement, and, most importantly, treatment plan and recommended its utilization in the treatment of triplane fractures. In another study by Nenopoulos et al., the authors included all distal tibial intra-articular fractures [20]. Among their 64 patients, 18 were indicated for surgery with radiographs alone. This number rose to 42 after inclusion of CT images, and the authors concluded that despite higher cost, utilization of CT gives indisputable benefits to the understanding and appropriate treatment of intra-articular fractures of the ankle in children.
In a recent meta-analysis of open versus closed treatment of distal physeal fractures, Asad et al. reported on a total of 970 eligible cases [29]. The overall rate of PPC was 13% and SH-II fractures comprised 60%; in the subset of SH-I and SH-II patients, PPC was seen in 23.4–31.6%. The authors found no difference in the odds ratio for premature physeal closure between ORIF and closed treatment. This was also true for a subgroup analysis of SH-I and SH-II fractures; ORIF patients had PPC 31.6% whereas those managed conservatively had a 23.4% rate of PPC; these numbers were not statistically significant.
Another ongoing discussion is the necessity of open reduction in intra-articular fractures. In a 2014 study by Choudhry et al., authors performed a retrospective radiographic review and found 28 patients with either a triplane or Tillaux fracture, who underwent appropriate joint line imaging with CT, and had 2–10 years of follow-up [41] and results of two validated outcome measures to assess their functional status. The authors found that as long as residual articular displacement is < 2.5 mm, neither the presence of articular gap and/or step-off nor the magnitude of displacement was predictive of a poor outcome. We agree with previous authors that closed reduction and percutaneous fixation is generally sufficient to address the joint line in the vast majority of transitional fractures.
Conclusion
Several aspects of pediatric ankle fractures have been clarified. First, intra-articular fractures should be reduced and fixed to less than 2–2.5 mm of displacement to optimize outcomes. Additionally, we reviewed the risk of premature growth arrest and its consequences in physeal fractures. While we know that anatomic reduction seems to improve outcomes in SH-III and SH-IV fractures of the distal tibia, accurate prediction of the behavior of SH-II fractures continues to be elusive. More and better data is required to determine which patients are better surgical candidates and in which patients growth arrest will become a clinical problem.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Foot and Ankle Trauma
Contributor Information
Z. Deniz Olgun, Phone: 412-692-9885, Email: olgunmd@gmail.com.
Stephanie Maestre, Email: maestres@upmc.edu.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major Importance
- 1.Peterson CA, Peterson HA. Analysis of the incidence of injuries to the epiphyseal growth plate. The Journal of Trauma: Injury, Infection, and Critical Care. 1972;12:275–281. doi: 10.1097/00005373-197204000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Mann DC, Rajmaira S. Distribution of physeal and nonphyseal fractures in 2,650 long-bone fractures in children aged 0-16 years. J Pediatr Orthop. 1990;10:713–716. doi: 10.1097/01241398-199011000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Mizuta T, Benson WM, Foster BK, Paterson DC, Morris LL. Statistical analysis of the incidence of physeal injuries. J Pediatr Orthop. 1987;7:518–523. doi: 10.1097/01241398-198709000-00003. [DOI] [PubMed] [Google Scholar]
- 4.•.Hynes D, O’Brien T. Growth disturbance lines after injury of the distal tibial physis. Their significance in prognosis. J Bone Joint Surg Br. 1988;70:231–3. Twenty-six distal tibial fractures were reviewed and growth disturbance lines were evaluated. A “normal” pattern was seen to occur in patients who did not have growth arrest. [DOI] [PubMed]
- 5.O WH, Craig C, Banks HH. Epiphyseal injuries. Pediatr. Clin. North Am. 1974;21:407–422. [DOI] [PubMed]
- 6.•.Barmada A, Gaynor T, Mubarak SJ. Premature physeal closure following distal tibia physeal fractures: a new radiographic predictor. Journal of Pediatric Orthopaedics. 2003;23:733–9. Out of 92 fractures reviewed, 27.2% had growth arrest. Salter-Harris III and IV fractures had the greatest rate (38%), whereas physeal widening in excess of 3mm in Salter-Harris I and II fractures was associated with periosteal entrapment and subsequent physeal arrest (60% in wider physes vs. 17% in normal width). [DOI] [PubMed]
- 7.Nenopoulos SP, Papavasiliou VA, Papavasiliou AV. Outcome of physeal and epiphyseal injuries of the distal tibia with intra-articular involvement. J Pediatr Orthop. 2005;25:518–522. doi: 10.1097/01.bpo.0000158782.29979.14. [DOI] [PubMed] [Google Scholar]
- 8.Rohmiller MT, Gaynor TP, Pawelek J, Mubarak SJ. Salter-Harris I and II fractures of the distal tibia: does mechanism of injury relate to premature physeal closure? Journal of Pediatric Orthopaedics. Journal of Pediatric Orthopaedics; 2006;26:322–328. [DOI] [PubMed]
- 9.Flynn JM, Widmann RF. The limping child: evaluation and diagnosis. Journal of the American Academy of Orthopaedic Surgeons. 9:89. [DOI] [PubMed]
- 10.Kleinman PK, Marks SC, Blackbourne B. The metaphyseal lesion in abused infants: a radiologic-histopathologic study. American Journal of Roentgenology. American Roentgen Ray Society. 2012;146:895–905. doi: 10.2214/ajr.146.5.895. [DOI] [PubMed] [Google Scholar]
- 11.Mubarak SJ. Extensor retinaculum syndrome of the ankle after injury to the distal tibial physis. J Bone Joint Surg Br. 2002;84:11–14. doi: 10.1302/0301-620X.84B1.11800. [DOI] [PubMed] [Google Scholar]
- 12.Haumont T, Gauchard GC, Zabee L, Arnoux J-M, Journeau P, Lascombes P. Extensor retinaculum syndrome after distal tibial fractures: anatomical basis. Surg Radiol Anat. 2007;29:303–311. doi: 10.1007/s00276-007-0215-3. [DOI] [PubMed] [Google Scholar]
- 13.Dowling SK, Wishart I. Use of the Ottawa ankle rules in children: a survey of physicians’ practice patterns. Canadian Journal of Emergency Medicine. Cambridge University Press; 2011;13:333–338. [PubMed]
- 14.Stiell IG, Greenberg GH, McKnight RD, Nair RC, McDowell I, Reardon M, et al. Decision rules for the use of radiography in acute ankle injuries. Refinement and prospective validation. JAMA. 1993;269:1127–1132. doi: 10.1001/jama.269.9.1127. [DOI] [PubMed] [Google Scholar]
- 15.Gill JB, Risko T, Raducan V, Grimes JS, Schutt RC. Comparison of manual and gravity stress radiographs for the evaluation of supination-external rotation fibular fractures. The Journal of Bone and Joint Surgery-American Volume. 2007;89:994–999. doi: 10.2106/JBJS.F.01002. [DOI] [PubMed] [Google Scholar]
- 16.Biswas D, Bible JE, Bohan M, Simpson AK, Whang PG, Grauer JN. Radiation exposure from musculoskeletal computerized tomographic scans. The Journal of Bone and Joint Surgery-American Volume. 2009;91:1882–1889. doi: 10.2106/JBJS.H.01199. [DOI] [PubMed] [Google Scholar]
- 17.Cutler L, Molloy A, Dhukuram V, Bass A. Do CT scans aid assessment of distal tibial physeal fractures? J Bone Joint Surg Br. 2004;86:239–243. doi: 10.1302/0301-620X.86B2.13624. [DOI] [PubMed] [Google Scholar]
- 18.Liporace FA, Yoon RS, Kubiak EN, Parisi DM, Koval KJ, Feldman DS, et al. Does adding computed tomography change the diagnosis and treatment of Tillaux and triplane pediatric ankle fractures? Orthopedics. 2012;:1–5. [DOI] [PubMed]
- 19.Eismann EA, Stephan ZA, Mehlman CT, Denning J, Mehlman T, Parikh SN, et al. Pediatric triplane ankle fractures: impact of radiographs and computed tomography on fracture classification and treatment planning. The Journal of Bone and Joint Surgery-American Volume. 2015;97:995–1002. doi: 10.2106/JBJS.N.01208. [DOI] [PubMed] [Google Scholar]
- 20.Nenopoulos A, Beslikas T, Gigis I, Sayegh F, Christoforidis I, Hatzokos I. The role of CT in diagnosis and treatment of distal tibial fractures with intra-articular involvement in children. Injury. 2015;46:2177–80. [DOI] [PubMed]
- 21.Seifert J, Matthes G, Hinz P, Paris S, Mutze S, Ekkernkamp A, et al. Role of magnetic resonance imaging in the diagnosis of distal tibia fractures in adolescents. Journal of Pediatric Orthopaedics. 23:727. [DOI] [PubMed]
- 22.Salter RB. Injuries of the epiphyseal plate. Instr Course Lect. 1992;41:351–359. [PubMed] [Google Scholar]
- 23.Salter RB, Harris WR. Injuries involving the epiphyseal plate. J Bone Joint Surg Am. The Journal of Bone and Joint Surgery-American Volume; 1963;45:587–622.
- 24.Dias LS, Tachdjian MO. Physeal injuries of the ankle in children: classification. Clin Orthop Relat Res. 1978;:230–3. [PubMed]
- 25.Peterson HA. Physeal fractures: part 3. Classification Journal of Pediatric Orthopaedics. 1994;14:439–448. doi: 10.1097/01241398-199407000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Ogden JA, McCarthy SM. Radiology of postnatal skeletal development. VIII. Distal tibia and fibula. Skelet Radiol. 1983;10:209–220. doi: 10.1007/BF00357893. [DOI] [PubMed] [Google Scholar]
- 27.Cooperman DR, Spiegel PG, Laros GS. Tibial fractures involving the ankle in children. The so-called triplane epiphyseal fracture. The Journal of Bone and Joint Surgery-American Volume. 1978;60:1040–1046. doi: 10.2106/00004623-197860080-00003. [DOI] [PubMed] [Google Scholar]
- 28.Cummings RJ, Shea KG. Distal tibial and fibular fractures. In: Beaty JH, Kasser JR, eds. Rockwood and Wilkins’ Fractures in children. 7th Edition. Philadelphia, Pa. Lippincott Williams & Wilkins; 2010.
- 29.Asad WA, Younis MHS, Ahmed AF, Ibrahim T. Open versus closed treatment of distal tibia physeal fractures: a systematic review and meta-analysis. Eur J Orthop Surg Traumatol Springer Paris. 2017;18:1–7. doi: 10.1007/s00590-017-2062-1. [DOI] [PubMed] [Google Scholar]
- 30.Spiegel PG, Cooperman DR, Laros GS. Epiphyseal fractures of the distal ends of the tibia and fibula. A retrospective study of two hundred and thirty-seven cases in children. The Journal of Bone and Joint Surgery-American Volume. 1978;60:1046–1050. doi: 10.2106/00004623-197860080-00004. [DOI] [PubMed] [Google Scholar]
- 31.Kling TF, Bright RW, Hensinger RN. Distal tibial physeal fractures in children that may require open reduction. The Journal of Bone and Joint Surgery-American Volume. 1984;66:647–657. doi: 10.2106/00004623-198466050-00002. [DOI] [PubMed] [Google Scholar]
- 32.Cass JR, Peterson HA. Salter-Harris type-IV injuries of the distal tibial epiphyseal growth plate, with emphasis on those involving the medial malleolus. The Journal of Bone and Joint Surgery-American Volume. 1983;65:1059–1070. doi: 10.2106/00004623-198365080-00005. [DOI] [PubMed] [Google Scholar]
- 33.•.Caterini R, Farsetti P, Ippolito E. Long-term followup of physeal injury to the ankle. Foot Ankle. 1991;11:372–83. Sixty-eight patients who had a physeal injury about the ankle at an average age of 12 years were studied at an average follow-up of 27 years, 47 of whom had a good result, and 11.8% had radiographic findings of arthritis. Type of Salter-Harris lesion, amount of initial displacement, and quality of reduction were determinants of outcome. [DOI] [PubMed]
- 34.•.Luhmann SJ, Oda JE, O'Donnell J, Keeler KA, Schoenecker PL, Dobbs MB, et al. An analysis of suboptimal outcomes of medial malleolus fractures in skeletally immature children. Am J. Orthop. 2012;41:113–6. Retrospective review of 24 medial malleolus fractures in children with suboptimal outcomes (malunion and physeal damage) found that malreductions as little as 2 mm are poorly tolerated. Authors suggest operative fixation to within 1 mm of displacement. [PubMed]
- 35.Karrholm J, Hansson LI, Selvik G. Changes in tibiofibular relationships due to growth disturbances after ankle fractures in children. The Journal of Bone and Joint Surgery-American Volume. 1984;66:1198–1210. doi: 10.2106/00004623-198466080-00007. [DOI] [PubMed] [Google Scholar]
- 36.Chung T, Jaramillo D. Normal maturing distal tibia and fibula: changes with age at MR imaging. Radiology. 1995;194:227–232. doi: 10.1148/radiology.194.1.7997558. [DOI] [PubMed] [Google Scholar]
- 37.•.Aitken AP. Fractures of the epiphyses. Clin Orthop Relat Res. 1965;41:19–23. Aitken’s classical text on physeal fractures discusses biology, classifications, and treatment. [PubMed]
- 38.Luhmann SJ, Oda JE, O'Donnell J, Keeler KA, Schoenecker PL, Dobbs MB, et al. An analysis of suboptimal outcomes of medial malleolus fractures in skeletally immature children. Am J Orthop. 2012;41:113–116. [PubMed] [Google Scholar]
- 39.••.Leary JT, Handling M, Talerico M, Yong L, Bowe JA. Physeal fractures of the distal tibia predictive factors of premature physeal closure and growth arrest. Journal of Pediatric Orthopaedics. Journal of Pediatric Orthopaedics; 2009;29:356–61. Premature physeal closure rate was observed as 12.1% in 124 ankle fractures followed for a minimum of 1 year. Authors observed a strong relationship between mechanism of injury and initial fracture displacement, and trends toward physeal closure with increased residual displacement and number of reduction attempts. [DOI] [PubMed]
- 40.••.Rapariz JM, Ocete G, González-Herranz P, López-Mondejar JA, Domenech J, Burgos J, et al. Distal tibial triplane fractures: long-term follow-up. Journal of Pediatric Orthopaedics. 1996;16:113–8. Thirty-five patients with triplane fractures were assessed at an average follow-up of 5 years. With adequate reduction (< 2mm displacement), patients were noted to have excellent clinical outcomes. [DOI] [PubMed]
- 41.Choudhry IK, Wall EJ, Eismann EA, Crawford AH, Wilson L. Functional outcome analysis of triplane and tillaux fractures after closed reduction and percutaneous fixation. J Pediatr Orthop. 2014;34:139–143. doi: 10.1097/BPO.0000000000000085. [DOI] [PubMed] [Google Scholar]
- 42.Lagier R. Case report 552: Post-traumatic remodelling of the distal tibial epiphysis: a form of aseptic osteonecrosis. Skeletal Radiology. 2nd ed. Springer-Verlag; 1989;18:331–333. [DOI] [PubMed]
- 43.Pugely AJ, Nemeth BA, McCarthy JJ, Bennett DL, Noonan KJ. Osteonecrosis of the distal tibia metaphysis after a salter-Harris I injury: a case report. J Orthop Trauma. 2012;26:e11–e15. doi: 10.1097/BOT.0b013e318214e03c. [DOI] [PubMed] [Google Scholar]
- 44.Wilder RT, Berde CB, Wolohan M, Vieyra MA, Masek BJ, Micheli LJ. Reflex sympathetic dystrophy in children. Clinical characteristics and follow-up of seventy patients. The Journal of Bone and Joint Surgery-American Volume. 1992;74:910–919. doi: 10.2106/00004623-199274060-00013. [DOI] [PubMed] [Google Scholar]