Abstract
OBJECTIVES
To examine the effect of obesity (body mass index (BMI)≥ 30.0 kg/m2) on outcomes of older adults admitted to skilled nursing facilities (SNFs) for hip fracture postacute care (PAC).
DESIGN
Retrospective cohort study.
SETTING
U.S. Medicare- and Medicaid-certified SNFs from 2008 to 2015.
PARTICIPANTS
Medicare fee-for-service beneficiaries discharged to a SNF after hospitalization for hip fracture (N=586,683; n=82,768 (14.1%) meeting obesity criteria). Exclusion criteria were aged younger than 65, being underweight (BMI<18.5 kg/m2), and SNF use in the year prior to index hospitalization.
MEASUREMENTS
Residents were divided into 4 BMI categories according to cutoffs that the World Health Organization has established: not obese (BMI 18.5–29.9 kg/m2), mild obesity (BMI 30.0–34.9 kg/m2), moderate obesity (BMI 35.0–39.9 kg/m2), and severe obesity (BMI≥40.0 kg/m2). Robust Poisson regression was used to compare differences in average nursing facility length of stay (LOS) and rates of 30-day hospital readmission, successful discharge to community, and becoming a long-stay resident (LOS>100) according to obesity level. Models were adjusted for individual-level covariates and facility fixed effects.
RESULTS
Residents with mild (adjusted relative risk (aRR)=1.16, 95% CI=1.12–1.19), moderate (aRR=1.27, 95% CI=1.20–1.35), and severe (aRR=1.67, 95% CI=1.54–1.82) obesity were more likely to be readmitted within 30 days than those who were not obese. The average difference in LOS between residents without obesity and those with mild obesity was 2.6 days (95% CI=2.2–2.9 days); moderate obesity, 4.2 days (95% CI=3.7–5.1 days); and severe obesity, 7.0 days (95% CI=5.9–8.2 days). Residents with obesity were less likely to be successfully discharged and more likely to become long-stay nursing home residents.
CONCLUSION
Obesity was associated with worse outcomes in postacute SNF residents with hip fracture. Efforts to provide targeted care to residents with obesity may be essential to improve outcomes. Obesity may be an overlooked risk adjuster in quality-of-care measures and in payment reforms related to PAC for individuals with hip fracture.
Keywords: obesity, postacute care, hip fracture, nursing facility, successful discharge
Obesity (body mass index (BMI) ≥30.0 kg/m2) is an increasing problem in the elderly population, with a reported prevalence of 39% in adults aged 60 and older.1,2 Obesity predisposes older adults to multiple comorbidities and complicates chronic diseases, increasing demand for health services such as nursing home care.3 Rising rates of obesity in nursing homes have been documented 1,4 and may grow further because of changes in demography and greater longevity.5,6 In spite of this, obesity in the nursing home setting remains understudied while being well-researched in community-based populations of older adults.7
The effects of obesity exacerbate multiple facets of aging. The role of obesity in functional loss and disability has been particularly well documented. For example, individuals with obesity are more likely to be weaker and have poorer lower extremity function.8–11 Skilled nursing facilities (SNFs) are a major provider of rehabilitative services to older adults with these types of functional impairments. For instance, SNFs are the largest provider of postacute care (PAC) to older adults with hip fracture,12 but to our knowledge, no study has examined the consequences of obesity for functionally impaired SNF residents. To address this gap in the literature, we compared the outcomes of postacute SNF residents with hip fracture according to level of obesity. SNF residents with obesity are more likely to have specialized care needs than without obesity. For instance, additional nursing assistance is often required for residents with obesity to conduct daily activities.13 Consequently, residents of resourceful, high-quality SNFs may have better prognoses than their counterparts in lower-quality facilities. Therefore, we hold constant facility-level differences in our estimation of the association between obesity and resident outcomes.
METHODS
Data Sources
The sources of individual-level data were the Medicare Beneficiary Summary file, Medicare inpatient claims files, and Minimum Data Set (MDS) assessments. The summary file contains demographic and diagnostic covariates for currently enrolled Medicare beneficiaries. The inpatient claims files consist of fee-for-service claims from acute hospitalizations and SNF admissions, containing data such as admitting diagnosis and dates of service. The MDS is administered to all residents of Medicare- or Medicaid-certified nursing facilities upon admission and regularly thereafter until discharge. The assessment captures demographic information and comorbidities and covers multiple care areas such as cognitive and physical function and psychosocial well-being.14
Information on SNF organizational characteristics and quality measures was obtained from the Certification and Survey Provider Enhanced Reporting file and the Nursing Home Compare website (www.medicare.gov/nursinghome-compare), maintained by the Centers for Medicare and Medicaid Services (CMS).
Study Sample
We identified fee-for-service beneficiaries discharged to a SNF after a short-term acute hospitalization between January 1, 2008, and September 30, 2015, with a primary diagnosis of hip fracture. Residents were classified as having hip fracture if the primary diagnosis field of their hospital claim contained an International Classification of Diseases, Ninth Revision (ICD-9) code of 820.00–820.32, 733.14, 733.15, 733.96, 733.97, 808.0, or 808.1. We also classified residents with a Medicare Severity Diagnosis-Related Group between 533 and 536 as having hip fracture. We excluded residents younger than 65, with SNF use in the year prior to index hospitalization, considered underweight (BMI <18.5 kg/ m2), and with a BMI that was likely to have been coded incorrectly (e.g., >90 kg/m2). We did not include residents with index hospitalizations after September 2015 because of the switch to the ICD-10 coding system. The final cohort consisted of 586,683 SNF residents.
Primary Exposure Variable
BMI was derived from the resident’s height and weight recorded during the MDS admission assessment, calculated as weight in pounds divided by height in inches squared times the constant 703 [BMI=weight (pounds)/height (inches)2 × 703)]. To enhance interpretability of analyses, we divided residents into those without obesity (BMI 18.5–29.9 kg/m2) and those with mild (BMI 30.0–34.9 kg/ m2), moderate (BMI 35.0–39.9 kg/m2), and severe (BMI ≥40.0 kg/m2) obesity.15
Outcome Variables
We examined whether the following outcomes varied according to obesity level: 30-day hospital readmission, SNF or nursing home length of stay (LOS), successful discharge to community,12,16 and becoming a long-stay resident. All outcomes were derived from Medicare claims and MDS assessments using the Residential History File methodology.17 Residents were followed for 180 days after SNF admission and on each day of the follow-up period were determined to be still in the SNF, in another inpatient setting (e.g., hospital, inpatient rehabilitation facility, another SNF), or dead. We also tracked hospice use during follow-up.
Residents were classified as readmitted if they stayed overnight in a general acute hospital during the first 30 days of follow-up. LOS was defined as the number of days of continuous SNF or nursing home use. Thus, we did not abbreviate LOS when residents were transferred to other SNFs or depleted their SNF benefit and became nursing home residents. Residents with a LOS of 100 or more days (the maximum for Medicare SNF coverage) were classified as long stay. Residents were considered successfully discharged if they exited the SNF within 90 days of admission and remained in the community for 30 days without dying, using hospice, or reentering the inpatient healthcare system. Residents who died or reentered the healthcare system within 30 days of discharge, died during the SNF stay, or were not discharged within 90 days of SNF admission were not considered discharged successfully.
Other Study Variables
Information on age, sex, race, dual eligibility for Medicaid, and dementia status were obtained from the Medicare enrollment file. Comorbidity burden was captured using the Deyo-Charlson comorbidity index,18 calculated from the diagnoses listed on the index hospitalization claim. Surgical treatment type was ascertained from the procedure codes listed on the claim. Residents were classified as having received no surgical treatment, open reduction and internal fixation, major joint replacement, closed reduction and internal fixation, or internal fixation without reduction. Physical function was captured using a composite of self-performance ratings of activities of daily living from the MDS assessment.19,20 Cognitive function was summarized using the MDS-based Cognitive Performance Scale score, which ranges from 1 (intact) to 6 (very severe impairment).21
Statistical Analysis
We used robust Poisson regression22 to calculate the relative risk (RR) of 30-day hospital readmission, successful discharge, and becoming a long-stay resident for residents with mild, moderate, and severe obesity. We also used a Poisson model to calculate adjusted mean LOS according to obesity level through marginal standardization (predictive margins). We did not predict LOS for residents who were not discharged from the SNF or nursing home at the end of the 180-day follow-up period. We excluded residents from analyses if they were admitted or died at a point that censored the relevant window of observation for a particular outcome. Regression models were adjusted for age, age squared, female sex, non-white race, Deyo-Charlson score, CPS score, dementia, dual eligibility, surgical treatment type, year fixed effects, and SNF fixed effects. Data were analyzed using Stata MP version 14.2 (StataCorp, College Station, TX). Null hypotheses were tested assuming a two-sided type I error probability of 0.05.
Secondary Analysis
We modeled the association between continuous BMI and outcomes, also including second- and third-order polynomial terms. We then used marginal standardization to estimate the adjusted rate of each outcome per point of BMI between 19 and 50.
The institutional review board of Brown University approved the study protocol.
RESULTS
Between 2008 and 2015, 586,683 hospitalized Medicare fee-for-service beneficiaries discharged to SNF with hip fracture were identified. The prevalence of obesity was 14.1%: 10.2% with mild obesity, 2.8% with moderate obesity and 1.1% with severe obesity. Resident characteristics are summarized in aggregate and according to obesity level in Table 1. Mean age was 83.9±7.4 and decreased with obesity level. Seventy-four percent of beneficiaries were female; women were more likely to be moderately (78%) or severely (83%) obese. The proportion non-white was 6% and was similar across obesity strata. At the time of admission, 17% of residents were dually eligible for Medicaid. Between 21% and 31% of residents with obesity were dually eligible. Mean Deyo-Charlson score was 1.2±1.5, with 31% of residents having a score of 2 or greater. Deyo-Charlson scores were higher in residents with obesity, reaching an average of 1.7±1.8 in residents with severe obesity. Mean activity of daily living score was 18.4±3.5 and was similar in residents with different obesity levels. Thirty-nine percent of residents had dementia, ranging from 19% to 29% in those with obesity. Correspondingly, the distribution of CPS scores was lower in residents with obesity. Approximately 83% of residents underwent surgical treatment for hip fracture, most commonly open reduction and internal fixation or joint replacement (57%) rather than closed reduction and internal fixation or internal fixation without fracture reduction (25%). Residents with obesity were more likely to undergo open reduction and internal fixation and less likely to have joint replacement surgery.
Table 1.
Study Cohort Characteristics According to Obesity: 2008–2015
| Characteristic | All Residents, N = 586,683 | Not Obese (BMI< 30.0 kg/m2), n = 503,915 | Obese | ||
|---|---|---|---|---|---|
| Mildly (BMI 30.0–34.9 kg/m2), n = 59,705 | Moderately (BMI 35.0–39.9 kg/m2), n = 16,401 | Severely (BMI ≥40.0 kg/m2), n = 6,662 | |||
| Participant | |||||
| Age, mean ± SD | 83.9 ± 7.4 | 84.5 ± 7.2 | 81.5 ± 7.3 | 79.2 ± 7.3 | 76.7 ± 7.3 |
| Aged ≥80, n (%) | 433,431 (74) | 385,732 (77) | 37,332 (63) | 8,017 (49) | 2,350 (35) |
| Female, n (%) | 438,009 (75) | 375,316 (74) | 44,433 (74) | 12,759 (78) | 5,501 (83) |
| Not white, n (%) | 35,256 (6) | 30,496 (6) | 3,268 (5) | 1,010 (6) | 482 (7) |
| Medicare and Medicaid dually eligible, n (%) | 101,690 (17) | 82,717 (16) | 12,703 (21) | 4,237 (26) | 2,033 (31) |
| Activity of daily living score, mean ± SD (range 0–28, higher = worse) | 18.4 ± 3.5 | 18.4 ± 3.6 | 18.3 ± 3.4 | 18.4 ± 3.3 | 18.8 ± 3.1 |
| Activity of daily living score ≥23, n (%) | 50,107 (9) | 43,749 (9) | 4,469 (7) | 1,240 (8) | 649 (10) |
| Charlson Comorbidity Index, mean ± SD | 1.2 ± 1.5 | 1.2 ± 1.4 | 1.4 ± 1.5 | 1.5 ± 1.6 | 1.7 ± 1.8 |
| Charlson Comorbidity Index ≥2, n (%) | 181,607 (31) | 150,149 (30) | 21,902 (37) | 6,636 (40) | 2,920 (44) |
| Cognitive Performance Scale score, n (%) | |||||
| 0 | 101,946 (40) | 84,707 (38) | 12,115 (51) | 3,576 (56) | 1,548 (61) |
| 1–2 | 68,497 (27) | 59,902 (27) | 6,329 (26) | 1,650 (26) | 616 (24) |
| 3–4 | 63,072 (25) | 57,462 (26) | 4,390 (18) | 931 (15) | 289 (11) |
| 5–6 | 20,554 (8) | 19,194 (9) | 1,081 (5) | 206 (3) | 73 (3) |
| Dementia, n (%) | 228,924 (39) | 206,239 (41) | 17,421 (29) | 4,008 (24) | 1,256 (19) |
| Surgical treatment, n (%) | |||||
| None | 100,834 (17) | 88,232 (18) | 9,004 (15) | 2,488 (15) | 1,110 (17) |
| Open reduction and internal fixation | 154,698 (26) | 129,261 (26) | 17,557 (29) | 5,422 (33) | 2,458 (37) |
| Joint replacement | 183,256 (31) | 160,424 (32) | 17,485 (29) | 4,044 (25) | 1,303 (20) |
| Close reduction and internal fixation | 111,517 (19) | 94,658 (19) | 12,054 (20) | 3,453 (21) | 1,352 (20) |
| Internal fixation only | 36,378 (6) | 31,340 (6) | 3,605 (6) | 994 (6) | 439 (7) |
| Facility characteristic | |||||
| Occupancy rate, mean ± SD | 84.0 ± 14.2 | 84.1 ± 14.2 | 83.9 ± 14.4 | 83.7 ± 14.5 | 83.4 ± 14.4 |
| Number of beds, mean ± SD | 121.7 ± 72.9 | 121.9 ± 73.2 | 120.2 ± 71.3 | 120.8 ± 71.3 | 120.4 ± 67.6 |
| % Medicaid, mean ± SD | 44.8 ± 25.4 | 44.7 ± 25.4 | 45.2 ± 25.3 | 46.3 ± 25 | 47.7 ± 24.7 |
| Star ratinga, mean ± SD | 3.4 ± 1.3 | 3.4 ± 1.3 | 3.4 ± 1.3 | 3.3 ± 1.3 | 3.3 ± 1.3 |
| Star rating, n (%) | |||||
| 1–2 | 136,802 (27) | 116,914 (27) | 14,039 (27) | 4,075 (29) | 1,774 (31) |
| 3 | 98,773 (20) | 84,735 (20) | 10,090 (20) | 2,826 (20) | 1,122 (19) |
| 4–5 | 263,554 (53) | 226,261 (53) | 27,198 (53) | 7,216 (51) | 2,879 (50) |
| Region, n (%) | |||||
| Northeast | 112,924 (19) | 97450 (20) | 11,314 (19) | 2,976 (18) | 1,184 (18) |
| Midwest | 146,465 (25) | 122,677 (25) | 16,904 (29) | 4,792 (30) | 2,092 (32) |
| South | 217,382 (37) | 188,027 (38) | 21,250 (36) | 5,797 (36) | 2,308 (35) |
| Pacific | 103,137 (18) | 89,891 (18) | 9,594 (16) | 2,650 (16) | 1,002 (15) |
| Rural, n (%) | 117,545 (20) | 98,949 (20) | 13,167 (22) | 3,814 (23) | 1,615 (24) |
| For-profit facility, n (%) | 379,192 (65) | 325,638 (65) | 38,261 (65) | 10,809 (66) | 4,484 (68) |
Refers to the Nursing Home Compare overall rating of the skilled nursing facility (SNF) for the month the resident was admitted to the facility. Only available for residents admitted to SNF after 2009.
BMI = body mass index; SD = standard deviation.
Table 1 shows the characteristics of SNFs attended by the average resident in our sample. Residents on average stayed in a SNF with an 84±14% occupancy rate and 122±73 beds, that was for-profit and rated 3.4±1.3 stars, and had 45±25% of beds funded by Medicaid. The majority of facility characteristics were comparable across residents with different obesity levels, although residents with severe obesity were more likely to be admitted to a SNF with a slightly higher percentage of Medicaid beds, that was rated 1 or 2 stars, and that was in a rural area.
Table 2 displays the rates and aRRs of 30-day hospital readmission and adjusted nursing home LOS according to level of obesity. The 30-day readmission rate was 11.8% for residents without obesity, 12.6% for residents with mild obesity (aRR=1.16, 95% CI=1.12–1.19), 13.9% for residents with moderate obesity (RR=1.27, 95% CI=1.20–1.35), and 16.9% for residents with severe obesity (RR=1.67, 95% CI=1.54–1.82). Average LOS in the SNF or nursing home was 36.1 days for residents without obesity, 38.6 days for residents with mild obesity (adjusted difference=2.6 days, 95% CI=2.2–2.9 days), 40.5 days for residents with moderate obesity (adjusted difference=4.4 days, 95% CI=3.7–5.1 days), and 43.1 days for residents with severe obesity (adjusted difference=7.0 days, 95% CI=5.9–8.2 days).
Table 2.
Impact of Obesity on Postacute Outcomes
| Obesity Level | 30-day Readmission | Length of Stay | ||
|---|---|---|---|---|
|
|
|
|||
| n/N (%) | Adj. RR (95% CI) | Adj. Mean | Difference (95% CI) | |
| Non-Obese: BMI< 30 | 58855/498346 (11.8) | Referent | 36.1 | Referent |
|
| ||||
| Mild: BMI 30.0–34.9 | 7501/59335 (12.6) | 1.16 (1.12, 1.19) | 38.6 | 2.6 (2.2, 2.9) |
|
| ||||
| Moderate: BMI 35.0–39.9 | 2258/16298 (13.9) | 1.27 (1.20, 1.35) | 40.5 | 4.4 (3.7, 5.1) |
|
| ||||
| Severe: BMI ≥40.0 | 1121/6633 (16.9) | 1.67 (1.54, 1.82) | 43.1 | 7.0 (5.9, 8.2) |
|
| ||||
| Successful Dischargea | Became Long-Stay Resident | |||
|
|
|
|||
| n/N (%) | Adj. RR (95% CI) | n/N (%) | Adj. RR (95% CI) | |
|
| ||||
| Non-Obese: BMI< 30 | 353272/498392 (70.9) | Referent | 32059/498346 (6.4) | Referent |
|
| ||||
| Mild: BMI 30.0–34.9 | 43115/59081 (73.0) | 0.96 (0.95, 0.97) | 3407/59335 (5.7) | 1.06 (1.01, 1.11) |
|
| ||||
| Moderate: BMI 35.0–39.9 | 11585/16204 (71.5) | 0.93 (0.91, 0.95) | 951/16298 (5.8) | 1.19 (1.10, 1.30) |
|
| ||||
| Severe: BMI ≥40.0 | 4299/6572 (65.4) | 0.82 (0.80, 0.85) | 485/6633 (7.3) | 1.57 (1.38, 1.79) |
BMI=Body Mass Index; Adj.=Adjusted; RR= Relative Risk. Models are adjusted for age, age-squared, sex, non-White race, Charlson comorbidity score, Cognitive Performance Scale score, dementia, Medicaid eligibility, surgical treatment type, year fixed effects and facility fixed effects.
See methods for a detailed description of this outcome.
Rates and adjusted risks of successful discharge to community and of becoming a long-stay resident conferred by obesity are listed in Table 2. The proportion of residents without obesity who were successfully discharged to the community was 70.9%. Of residents with mild obesity, 73.0% were discharged successfully, although in adjusted comparisons, mild obesity was associated with a lower probability of successful discharge (aRR=0.96, 95% CI=0.95–0.97). The rate of successful discharge of residents with moderate obesity was 71.5%, but in the adjusted comparison, moderate obesity was associated with lower likelihood of successful discharge (aRR=0.93, 95% CI=0.91–0.95). Of residents with severe obesity, 65.4% were successfully discharged (aRR=0.82, 95% CI=0.80–0.85).
Of residents without obesity, 6.4% became long-stay residents. Of residents with mild obesity, 5.7% became long-stay residents, although in adjusted comparisons, mild obesity conferred greater risk of becoming a long-stay resident (aRR=1.06, 95% CI=1.01–1.11). Of residents with moderate obesity, 5.8% became long-stay residents, although in adjusted comparisons, moderate obesity was associated with greater probability of becoming a long-stay resident (aRR=1.19, 95% CI=1.10–1.30). Of residents with severe obesity, 7.3% became long-stay residents (aRR=1.57, 95% CI=1.38–1.79).
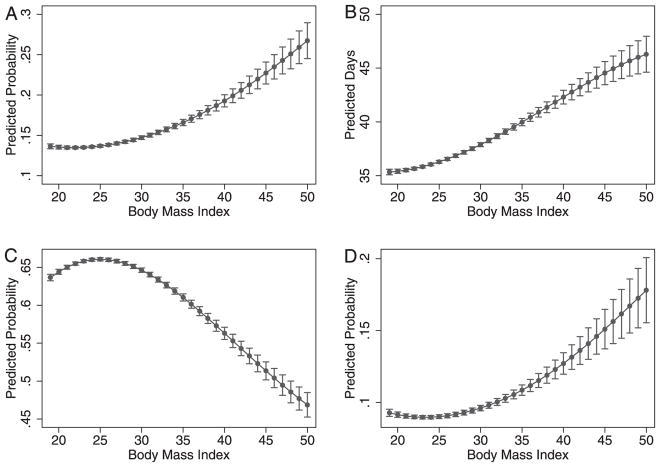
The adjusted rates of outcomes per point of BMI are illustrated in Figure 1. The probability of readmission (Figure 1A), average LOS (Figure 1B), and probability of becoming a long-stay resident increased curvilinearly across levels of BMI (Figure 1D). The probability of successful discharge (Figure 1C) decreased across levels of BMI.
Figure 1.
Adjusted rates of outcomes with 95% confidence interval according to body mass index: (A) 30-day hospital readmission, (B) length of nursing facility stay, (C) successful discharge to community, (D) became long-stay resident.
DISCUSSION
To our knowledge, this is the first study of obesity in post-acute SNF residents with hip fracture. The prevalence of obesity (14.1%) observed in our cohort is somewhat lower than previously reported in studies of SNF residents.1,4 This may be attributable to the selection of healthier surgical candidates and the protective effect of obesity against hip fracture.23 Moderate obesity was prevalent in 2.8% of residents and severe obesity in 1.1%.
Residents with obesity were younger and correspondingly had lower rates of cognitive impairment and dementia, although they had higher comorbidity burdens, which is traditionally associated with obesity. In unadjusted comparisons, the probability of 30-day hospital readmission was higher in residents with mild, moderate, and severe obesity. LOS, successful discharge, and becoming a long-stay resident did not seem to vary according to obesity level until we accounted for dementia and cognitive impairment. Dementia confounds the association between obesity and these outcomes because it is a risk factor for being frail or underweight24 and for outcomes related to nursing home LOS.25,26 After controlling for dementia and other covariates, we found that obesity conferred a strong risk for all outcomes. Although the largest risks were associated with moderate and severe obesity, even mild obesity had nontrivial effects. For instance, residents with mild obesity were found to stay in the SNF or nursing home for 2.6 additional days, on average. We also found a precise, incremental relationship between BMI and adverse outcomes (Figure 1). Thus, even smaller amounts of excess adiposity should not be overlooked when considering the risk of adverse outcomes.
Eighty-three percent of our hip fracture cohort was admitted to a SNF for postsurgical care and rehabilitation. Examining and improving postacute outcomes for these residents is becoming increasingly important because CMS has begun piloting episode-based payment initiatives such as the Surgical Hip and Femur Treatment (SHFFT) and the Comprehensive Care for Joint Replacement (CJR) models,27,28 which were implemented during 2016 in more than 800 hospitals in 67 Metropolitan Statistical Areas. Hospitals participating in SHFFT and CJR are held accountable financially for the quality and cost of care during the 90-day period after surgery. Total costs for services and items related to the surgery paid under Medicare Parts A and B are compared with a target episode price based on historical spending on the procedure. The difference between the payments made and the target price determines whether the hospital receives additional Medicare payments or pays Medicare. The target prices are adjusted for area-level trends in spending but are otherwise superficially risk adjusted. Critics and supporters of SHFFT, CJR, and other bundled payment initiatives have raised concerns about the current approach to risk adjustment and believe that, without better risk adjustment, hospitals serving individuals with multimorbidity will be penalized under the cost and reimbursement structure. For instance, individuals with chronic kidney disease and chronic obstructive pulmonary disease are known to have higher intra- and postoperative costs.29 Our results suggest that individuals with obesity merit similar concerns and warrant careful consideration of payment and outcomes adjustment according to obesity level.
It has been suggested that insufficient risk adjustment may lead to disparities in access to surgical care.30 More than 90% of respondents to a survey of the members of the American Association of Hip and Knee Surgeons revealed that current bundled payment initiatives would discourage them from operating on high-risk individuals.31 Leaving unaddressed the excess risk of adverse outcomes in PAC in residents with obesity may lead to patient selection and thereby decrease rates of surgery for individuals in hospitals participating in bundled payment initiatives, increase the difficulty of PAC placement, and ultimately compromise access to services.
To prevent readmissions and excess resource use of residents with obesity, efforts should be made to address their unique needs in SNFs. Our results suggest that outcomes are poor even after accounting for facility-level factors such as quality and available resources. It is reasonable to assume that the resources needed in SNFs to address obesity, such as staffing, equipment, and training in how to care for residents with obesity, are likely to be universally lacking. Residents with obesity require a higher allocation of staff time than those without obesity with similar care needs,13,32 particularly for functional rehabilitation, yet the Medicare Resource Utilization Group payment system does not incorporate obesity into its payment formula, and only a few states include a Medicaid per diem add-on for obesity (e.g., New York). Attention needs to be paid to the incentives for and disincentives to providing care to residents with obesity in SNFs as they relate to appropriate allocation of resources.
Results from this study also have implications for measurement of outcomes, which is relevant given the passage and implementation of the Improving Medicare Post-Acute Care Transformation Act of 2014.33 With the introduction of universal quality measures for PAC, studies like this are valuable in informing the design and risk adjustment of these cross-setting quality indicators. Our results suggest that attention must be paid to obesity when designing these measures not only to even the playing field for PAC providers, but also to avoid disincentives to serving individuals with obesity.
This study has several strengths, including the use of a cohort design with comprehensive population-level data that was complete in more than 99% of records. Prior studies have demonstrated the importance of distinguishing cases of extreme obesity,10 and because of the large sample size, we were able to make inferences about residents with moderate and obesity levels. Several limitations are also worth noting. First, although BMI is the most widely used measure of obesity, its accuracy declines among individuals with extreme stature and short stature is not uncommon in elderly populations. Second, we included only age-entitled Medicare fee-for-service beneficiaries without SNF use in the year prior to hospitalization. Therefore, our results may not be generalizable to older adults who repeatedly use SNF services, who are enrolled in Medicare Advantage, or whose primary payer is not Medicare. Finally, residual confounding may have affected our point estimates, a common shortcoming of cohort studies.
In summary, older adults with hip fracture and obesity are more likely to have poor outcomes after postacute admission to a SNF. Efforts to improve targeted care for residents with obesity may be essential to improve outcomes and ultimately provide equitable care.
Acknowledgments
Financial Disclosure: This study was funded by P01AG027296 from the U.S. National Institute on Aging (VM).
Meetings: This study was presented at the AcademyHealth and International Association of Gerontology and Geriatrics Annual Research Meetings in 2017.
Conflict of Interest: CMK, KST, PLG, and JAO have no potential conflicts of interest. VM holds stock of unknown value in PointRight, Inc., an information services company providing advice and consultation to various components of the long-term care and postacute care industry, including suppliers and insurers. PointRight sells information on the measurement of nursing home quality to nursing homes and liability insurers. VM was a founder of the company but has subsequently divested much of his equity in the company and relinquished his seat on the board. In addition, VM chairs the Independent Quality Committee for HRC Manor Care, Inc., a nursing home chain, for which he receives compensation in the range of $20,000 to $40,000. VM also serves as chair of a Scientific Advisory Committee for NaviHealth, a postacute care service organization, for which he also receives compensation in the range of $20,000 to $40,000 per year. VM serves as a technical expert panel member on several Centers for Medicare and Medicaid Services quality measurement panels. VM is a member of the boards of directors of Tufts Health Plan Foundation, Hospice Care of Rhode Island, and the Jewish Alliance of Rhode Island.
Author Contributions: CMK: study concept and design. VM: data acquisition. CMK: data analysis. CMK, KST, PLG, JAO, VM: critical interpretation of the data. CMK: drafting the article. All authors: revision of manuscript for important intellectual content, approval of final draft.
Sponsor’s Role: None.
References
- 1.Lapane KL, Resnik L. Obesity in nursing homes: An escalating problem. J Am Geriatr Soc. 2005;53:1386–1391. doi: 10.1111/j.1532-5415.2005.53420.x. [DOI] [PubMed] [Google Scholar]
- 2.Flegal KM, Kruszon-Moran D, Carroll MD, et al. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016;315:2284–2291. doi: 10.1001/jama.2016.6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elkins JS, Whitmer RA, Sidney S, Sorel M, Yaffe K, Johnston SC. Midlife obesity and long-term risk of nursing home admission. Obesity. 2006;14:1472–1478. doi: 10.1038/oby.2006.167. [DOI] [PubMed] [Google Scholar]
- 4.Felix HC, Bradway C, Chisholm L, et al. Prevalence of moderate to severe obesity among US nursing home residents, 2000–2010. Res Gerontol Nurs. 2015;8:173–178. doi: 10.3928/19404921-20150223-01. [DOI] [PubMed] [Google Scholar]
- 5.Butler RN. Population aging and health. BMJ. 1997;315:1082. doi: 10.1136/bmj.315.7115.1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spillman BC, Lubitz J. The effect of longevity on spending for acute and long-term care. N Engl J Med. 2000;342:1409–1415. doi: 10.1056/NEJM200005113421906. [DOI] [PubMed] [Google Scholar]
- 7.Bradway C, DiResta J, Fleshner I, et al. Obesity in nursing homes: A critical review. J Am Geriatr Soc. 2008;56:1528–1535. doi: 10.1111/j.1532-5415.2008.01821.x. [DOI] [PubMed] [Google Scholar]
- 8.Jenkins KR. Obesity’s effects on the onset of functional impairment among older adults. Gerontologist. 2004;44:206–216. doi: 10.1093/geront/44.2.206. [DOI] [PubMed] [Google Scholar]
- 9.Sturm R, Ringel JS, Andreyeva T. Increasing obesity rates and disability trends. Health Aff (Millwood) 2004;23:199–205. doi: 10.1377/hlthaff.23.2.199. [DOI] [PubMed] [Google Scholar]
- 10.Sharkey JR, Ory MG, Branch LG. Severe elder obesity and 1-year diminished lower extremity physical performance in homebound older adults. J Am Geriatr Soc. 2006;54:1407–1413. doi: 10.1111/j.1532-5415.2006.00842.x. [DOI] [PubMed] [Google Scholar]
- 11.Harris TB. Weight and body mass index in old age: Do they still matter? J Am Geriatr Soc. 2017;65:1898–1899. doi: 10.1111/jgs.14952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leland NE, Gozalo P, Christian TJ, et al. An examination of the first 30 days after patients are discharged to the community from hip fracture postacute care. Med Care. 2015;53:879–887. doi: 10.1097/MLR.0000000000000419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Felix HC. Personal care assistance needs of obese elders entering nursing homes. J Am Med Dir Assoc. 2008;9:319–326. doi: 10.1016/j.jamda.2008.01.011. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Medicare and Medicaid Services. [Accessed September 1, 2015];Minimum Data Set, Version 3.0. 2010 (onlinbe). Available at https://www.cms.gov/NursingHomeQualityInits/45_NHQIMDS30TrainingMaterials.asp#TopOPage.
- 15.World Health Organization. [Accessed September 1, 2015];Obesity: Preventing and Managing the Global Epidemic (online) Available at http://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/
- 16.Gozalo P, Leland NE, Christian TJ, et al. Volume matters: Returning home after hip fracture. J Am Geriatr Soc. 2015;63:2043–2051. doi: 10.1111/jgs.13677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Intrator O, Hiris J, Berg K, et al. The residential history file: Studying nursing home residents’ long-term care histories. Health Serv Res. 2011;46(1p1):120–137. doi: 10.1111/j.1475-6773.2010.01194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 19.Wysocki A, Thomas KS, Mor V. Functional improvement among short-stay nursing home residents in the MDS 3. 0. J Am Med Dir Assoc. 2015;16:470–474. doi: 10.1016/j.jamda.2014.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morris JN, Fries BE, Morris SA. Scaling ADLs within the MDS. J Gerontol A Biol Sci Med Sci. 1999;54A:M546–M553. doi: 10.1093/gerona/54.11.m546. [DOI] [PubMed] [Google Scholar]
- 21.Morris JN, Fries BE, Mehr DR, et al. MDS cognitive performance scale. J Gerontol. 1994;49:M174–M182. doi: 10.1093/geronj/49.4.m174. [DOI] [PubMed] [Google Scholar]
- 22.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 23.Tang X, Liu G, Kang J, et al. Obesity and risk of hip fracture in adults: A meta-analysis of prospective cohort studies. PloS One. 2013;8:e55077. doi: 10.1371/journal.pone.0055077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tamura BK, Bell CL, Masaki KH, et al. Factors associated with weight loss, low BMI, and malnutrition among nursing home patients: A systematic review of the literature. J Am Med Dir Assoc. 2013;14:649–655. doi: 10.1016/j.jamda.2013.02.022. [DOI] [PubMed] [Google Scholar]
- 25.Smith GE, Kokmen E, O’brien PC. Risk factors for nursing home placement in a population-based dementia cohort. J Am Geriatr. 2000;48:519–525. doi: 10.1111/j.1532-5415.2000.tb04998.x. [DOI] [PubMed] [Google Scholar]
- 26.Gaugler JE, Yu F, Davila HW, et al. Alzheimer’s disease and nursing homes. Health Aff (Millwood) 2014;33:650–657. doi: 10.1377/hlthaff.2013.1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Centers for Medicare and Medicaid Services. [Accessed August 3, 2017];Comprehensive Care for Joint Replacement Model (online) Available at http://innovation.cms.gov/initiatives/ccjr/
- 28.Centers for Medicare and Medicaid Services. [Accessed August 3, 2017];Surgical Hip and Femur Fracture Treatment (SHFFT) Model (online) Available at https://innovation.cms.gov/initiatives/shfft-model/
- 29.Rozell JC, Courtney PM, Dattilo JR, et al. Should all patients be included in alternative payment models for primary total hip arthroplasty and total knee arthroplasty? J Arthroplasty. 2016;31:45–49. doi: 10.1016/j.arth.2016.03.020. [DOI] [PubMed] [Google Scholar]
- 30.Fehring TK, Odum SM, Griffin WL, et al. The obesity epidemic: Its effect on total joint arthroplasty. J Arthroplasty. 2007;22:71–76. doi: 10.1016/j.arth.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 31.Kamath AF, Courtney PM, Bozic KJ, Mehta S, Parsley BS, Froimson MI. Bundled payment in total joint care: Survey of AAHKS membership attitudes and experience with alternative payment models. J Arthroplasty. 2015;30:2045–2056. doi: 10.1016/j.arth.2015.05.036. [DOI] [PubMed] [Google Scholar]
- 32.Lapane KL, Resnik L. Weighing the relevant issues: Obesity in nursing homes. J Aging Soc Policy. 2006;18:1–9. doi: 10.1300/J031v18n02_01. [DOI] [PubMed] [Google Scholar]
- 33.Improving Medicare Post-Acute Care Transformation (IMPACT) Act 2014 (online). 113th US Congress; [Accessed August 3, 2017]. Available at https://www.congress.gov/bill/113th-congress/house-bill/4994. [Google Scholar]