Abstract
Objective
To compare objectively-measured physical activity (PA) in older adults with symptomatic knee osteoarthritis (SxOA) with similarly aged adults without osteoarthritis (OA) or knee symptoms from the general population.
Methods
We included people age 50–85 years with SxOA from the Osteoarthritis Initiative (OAI, n=491), and people age 50–85 years from the general population from the National Health and Nutrition Examination Survey (NHANES, n=449). A uniaxial accelerometer was worn for ≥10 hours/day for ≥4 days in the NHANES in 2003–2004 (Actigraph 7124) and in the OAI in 2008–2010 (Actigraph GT1M). We calculated time spent in moderate-vigorous PA (MVPA in minutes/day) and described differences in MVPA and demographic variables between the samples. We conducted matched-pairs sensitivity analyses to further evaluate the role of potential confounders.
Results
Both cohorts had similarly low levels of PA in age and sex specific strata. Time in MVPA ranged from a median of 1 to 22 minutes/day in people with SxOA, and from 1 to 24 minutes/day in the general population without OA or knee pain. These results were similar in sensitivity analyses.
Conclusion
Time spent in MVPA was similarly low in those with SxOA as in older adults without knee pain or OA.
INTRODUCTION
Conventional wisdom suggests that persistent knee pain, a hallmark symptom of knee osteoarthritis (OA), hinders participation in physical activity (PA). Indeed, people with knee OA perceive pain as a barrier to being active[1], and they self-report participating in less PA than healthy adults [2–6]. Yet, more recent research using objectively-measured PA shows mixed results, and challenges the notion that people with knee OA are less physically active than the general population [7, 8].
Physical activity monitors (i.e. pedometers, accelerometers) provide objective, valid, and reliable measurement of physical activity frequency, intensity, and duration [9], allowing researchers to more precisely estimate PA relative to self-report questionnaires [10]. Using these more precise tools, it remains unclear how the PA levels of people with knee PA compare to the general population. Small studies have directly compared PA in people with knee OA and healthy controls using objective measures [11–13]. Synthesizing these studies, Wallis et al.[14] estimated that people with knee OA are 75% as active as healthy controls. On the other hand, most studies objectively measuring PA in large populations of people with knee OA have not directly compared to a general population or healthy control. Rather, these studies [5, 7, 8] have discussed their results relative to published epidemiological studies of people from the general population that reported PA levels and the prevalence of meeting national guidelines for aerobic PA [10, 15]. In contrast to the smaller studies with direct comparisons, the population-based studies concluded that the prevalence of meeting national PA guidelines for aerobic activity among people with knee OA was low (6–30%) [5, 7, 8], but similar to estimates in the general population (2–10%) [5, 7, 8, 10, 14, 15].
Larger datasets and intentionally-defined groups will allow us to more confidently understand if people with symptomatic knee OA (SxOA) are less active than people without knee OA or knee symptoms from the general population. Such an investigation is important since it is commonly perceived that knee OA is a barrier to PA [1]. Moreover, investigating PA is important since inactivity is a global pandemic that contributes to the incidence and progression of many chronic diseases including cardiovascular disease[16–19], diabetes[17–19], and cancer[19, 20], and consequently is responsible for over 5.3 million deaths yearly [21].
The purpose of this study was to compare objectively-measured moderate-vigorous PA (MVPA) in older adults with SxOA with similarly aged adults without knee symptoms or self-reported OA from the general population in the United States (US). We hypothesized that those with symptomatic knee OA spend less time in MVPA than adults without knee symptoms or self-reported OA. We focused specifically on MVPA since it is the recommended intensity to meet national PA guidelines for aerobic activity[22].
PATIENTS AND METHODS
Sample
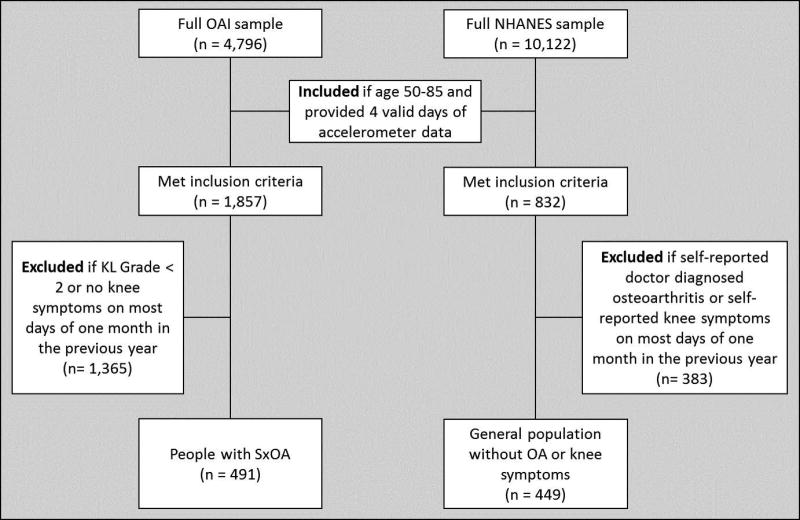
Older adults with SxOA (n= 491) from the Osteoarthritis Initiative (OAI)
We used data from the OAI to describe PA in people with SxOA. The OAI is a large multi-center prospective cohort study of individuals with or at risk for knee OA in the US. From 2008–2010, objective PA data were collected in a subset of individuals in the OAI in conjunction with the 4 year follow-up (from time of enrollment). Of this subset, we included people age 50–85 years who participated in the accelerometer study and provided at least 4 valid days of data. We excluded people without radiographic OA (Kellgren-Lawrence (KL) grade <2) or no knee pain, aching, or stiffness on most days of a month during the previous year. We excluded people with asymptomatic radiographic knee OA because the symptoms associated with OA are generally expected to be the limiting factor for PA participation [1]. This resulted in a sample of adults with SxOA (Figure 1), defined as Kellgren–Lawrence grade ≥ 2 and the presence of knee pain, aching, or stiffness on most days of a month during the previous year.
Figure 1.
Flowchart describing how the analytic samples were derived from the full OAI and NHANES samples.
General population of older adults (n=449) from the National Health and Nutrition Examination Survey (NHANES)
We used data from the NHANES to represent PA in the general population. NHANES has been administering series of surveys regarding health and nutrition in a nationally representative sample of non-institutionalized people across the country since 1999. In the 2003–2004 and 2005–2006 NHANES cycles, objective PA data were collected with accelerometers in a subset of the sample. We used data from the 2003–2004 cycle because this cycle additionally included questions related to arthritis and joint pain. We included participants age 50–85 years who participated in the accelerometer study and provided at least 4 valid days of data (defined in data analysis). Participants from the NHANES were excluded if they self-reported OA or knee symptoms. Specifically, people with OA were identified as those who answered yes to the question “Has a doctor or other health professional ever told you that you had arthritis?” and indicated “osteoarthritis” as the type. Participants with knee symptoms were identified as those who pointed to the right or left knee during a personal interview asking which joints had pain, aching, stiffness, or swelling in the previous 12 months.
Data collection
Demographics
Demographic variables were collected with questionnaires and during examinations in both cohort studies. Age was recorded. Height was measured with a stadiometer. Weight was measured with a balance beam scale in the OAI and a digital scale in the NHANES. Body mass index (BMI, kg/m2) was calculated from height and weight. Race (white, black, other), education level (less than high school, high school graduate, some college, at least college graduate), marital status (married, not married), income level (<$25k, >$25k), and presence of comorbidity (with at least 1 comorbidity, none) were described as proportions within concordant response categories between the OAI and the NHANES questionnaires. Presence of comorbidity was defined as people who reported history of or current heart attack, heart failure, stroke, emphysema, chronic bronchitis, chronic obstructive pulmonary disease, or asthma, as these cardiopulmonary pathologies potentially restrict participation in PA.
PA assessment
PA was measured in the NHANES and the OAI with an Actigraph uniaxial accelerometer. The participants were instructed to wear the Actigraph at the right hip during waking hours for 7 consecutive days. The NHANES used the Actigraph 7164, whereas the OAI used the Actigraph GT1M. In a direct comparison of these models during self-paced walking, Kozey et al. observed that time spent in higher activity intensity categories (ie. MVPA) and medium-speed walking were not different between models [23]. Since our analysis was limited to higher intensity activity (i.e. MPVA), potential bias due to different Actigraph models was minimized.
Other Lower Quarter Pain
Pain in the lower quarter (LQ pain) other than the knee may also limit PA. To adjust for the existence of other pain, we identified people in each sample who reported LQ pain, i.e. pain in the lower limb or low back pain. The knee was not included in the definition for LQ pain since it was in the exclusion criteria for the study samples. In each data set, there were differences in the questions regarding LQ pain, thus there were small differences in how lower limb pain was defined. For the OAI, presence of LQ pain was defined as reported ankle or foot pain on most of the last 30 days or hip pain on most days of one month in the last year, or low back pain in the last 30 days. For the NHANES, presence of LQ pain was defined as people who reported hip or ankle pain in the last year, foot pain in the last month lasting more than 24 hours, or low back pain in the last 3 months or lasting more than 24 hours in the last month.
Data analysis
Accelerometer data from the OAI and NHANES were processed using the same methods, and are consistent with processing of Actigraph data in prior studies [7]. A SAS macro provided by the National Cancer Institute (Available at http://riskfactor.cancer.gov/tools/nhanes_pam) was used to determine Actigraph wear time. Non-wear time was defined as ≥60 minutes of zero activity, with allowance for up to 2 minutes of activity counts 0–100, and subtracted from 24 hours to determine wear time [15]. A valid wear day was defined as a day with ≥10 hours of wear time. Participants were included if 4–7 valid wear days were available, regardless of day of the week. A MVPA minute was analytically identified by activity counts ≥ 2020/min [15]. The primary variable of interest was average min/day spent in MVPA.
Statistical analysis
The NHANES is a national probability sample. Sample weights are provided to account for subgroup oversampling and nonresponse in the NHANES 2003–2004 cycle. To account for the NHANES analytic subsample (having at least 4 valid wear days of accelerometer monitoring), sample weights were recalculated from the publically available NHANES sample weights to account for this additional sampling stage (https://epi.grants.cancer.gov/nhanes_pam/reweight.html) [15]. NHANES descriptive statistics (mean and standard deviation, median and interquartile range [IQR], and proportions with associated 95% confidence intervals) utilized the recalculated weights for the analytic subsample. The OAI descriptive analyses utilized unweighted observed data.
Due to different NHANES and OAI sampling procedures, we were unable to traditionally adjust for potential confounders. Therefore, sensitivity analyses were conducted which identified matched NHANES/OAI pairs using the following criteria: age (± 2.5 years), BMI (± 2.5 kg/m2), sex, and post high school education (none vs. at least some). From the matched pairs, we compared the time spent in MVPA between the OAI and the NHANES using generalized estimating equations, controlling for LQ pain, and the interaction between group and LQ pain.
RESULTS
In general, the sample of people with SxOA was 54% female, with an average age of 65.5 years (95% CI 64.7 to 66.3) and average BMI of 29.7 kg/m2 (95% CI 29.2 to 30.1). The general population sample without OA or knee pain was 45% female, with an average age of 63.0 years (95% CI 61.6 to 64.4) and average BMI of 27.4 kg/m2 (95%CI 26.9 to 28.1). The demographics are further described by sex and age group in Table 1.
Table 1.
Demographics stratified by sex and age group for the general population without OA or knee symptoms (General – from the NHANES) and for people with SxOA (from the OAI).
| Sample | Men
|
Women
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Age 50–59 | Age 60–69 | Age 70–79 | Age 80–85 | Age 50–59 | Age 60–69 | Age 70–79 | Age 80–85 | ||
| n | SxOA | 74 | 73 | 69 | 10 | 73 | 101 | 75 | 16 |
| General | 67 | 76 | 66 | 40 | 53 | 71 | 42 | 34 | |
| Age (years, mean (95%CI)) | SxOA | 55.6 | 64.0 | 74.3 | 81.3 | 55.0 | 64.8 | 74.2 | 81.8 |
| (55.0–56.2) | (63.3–64.7) | (73.7–75.0) | (80.5–82.1) | (54.4–55.6) | (64.3–65.4) | (73.5–74.8) | (81.2–82.4) | ||
| General | 53.5 | 64.6 | 74.5 | 83.5 | 53.2 | 62.9 | 73.8 | 82.6 | |
| (52.7–54.3) | (63.3–66.0) | (72.7–74.8) | (83.2–83.9) | (52.1–54.2) | (62.3–63.6) | (72.7–74.8) | (82.2–83.1) | ||
| BMI (kg/m2, mean (95%CI)) | SxOA | 30.2 | 30.0 | 28.8 | 27.4 | 30.9 | 31.1 | 27.8 | 26.2 |
| (29.3–31.1) | (29.1–30.8) | (27.8–29.8) | (23.9–30.9) | (29.5–32.3) | (30.0–32.2) | (26.7–28.9) | (23.8–28.5) | ||
| General | 28.0 | 28.6 | 27.5 | 25.2 | 26.7 | 27.1 | 27.5 | 26.6 | |
| (27.0–28.9) | (27.6–29.6) | (26.0–28.9) | (24.5–25.9) | (25.3–28.0) | (25.8–28.4) | (26.0–28.9) | (25.8–27.5) | ||
| Education (% Less than high school % high school graduate % Some college % At least college graduate) | SxOA | 2.8 | 4.1 | 4.3 | 10 | 1.4 | 1 1 | 2.7 | 0 |
| 9.7 | 6.8 | 11.6 | 0 | 16.4 | 3.9 | 20 | 25.0 | ||
| 13.9 | 19.2 | 13.0 | 0 | 21.9 | 31.7 | 26.7 | 12.5 | ||
| 73.6 | 69.9 | 71.0 | 90 | 60.3 | 53.5 | 50.7 | 62.5 | ||
| General | 8.5 | 12.4 | 48.5 | 32.2 | 11.8 | 24.2 | 30.3 | 43.3 | |
| 18.0 | 19.8 | 12.9 | 12.8 | 17.7 | 30.9 | 21.5 | 39.8 | ||
| 41.0 | 41.9 | 14.1 | 21.6 | 44.6 | 26.1 | 32.7 | 13.6 | ||
| 32.6 | 26.0 | 24.4 | 33.4 | 26.0 | 18.8 | 15.6 | 3.3 | ||
| Race (% white % black %other) | SxOA | 81.1 | 78.1 | 89.9 | 100 | 64.4 | 65.3 | 86.7 | 93.8 |
| 17.6 | 17.8 | 8.7 | 0 | 34.2 | 31.7 | 12 | 6.3 | ||
| 1.4 | 4.1 | 1.4 | 0 | 1.4 | 3 | 1.3 | 0 | ||
| General | 76.5 | 74.7 | 81.4 | 89.7 | 64.9 | 74. | 77.7 | 78.7 | |
| 7.4 | 10.9 | 6.0 | 6.3 | 14.9 | 14.0 | 6.3 | 5.7 | ||
| 16.1 | 14.4 | 12.6 | 4.0 | 20.2 | 11.9 | 16.0 | 15.6 | ||
| Marital status(% married) | SxOA | 78.9 | 84.3 | 87.9 | 77.8 | 59.7 | 60.8 | 56.9 | 53.3 |
| General | 90.6 | 88.9 | 75.5 | 76.0 | 71.0 | 61.6 | 47.2 | 23.0 | |
| Income (% <25k) | SxOA | 10.3 | 9.6 | 3.0 | 0 | 7.4 | 12.0 | 25.4 | 33.3 |
| General | 12.5 | 19.2 | 24.1 | 37.0 | 14.1 | 30.2 | 62.6 | 59.2 | |
| Comorbidity (% with comorbidity) | SxOA | 13.5 | 16.4 | 21.7 | 30.0 | 17.8 | 18.8 | 21.3 | 31.3 |
| General | 12.3 | 22.7 | 42.0 | 44.4 | 42.1 | 20.1 | 35.8 | 20.0 | |
| Wear time (minutes/day, mean (95% CI)) | SxOA | 14.3 | 14.1 | 13.4 | 12.9 | 14.7 | 14.0 | 13.4 | 14.1 |
| (14.0–14.7) | (13.8–14.4) | (13.1–13.7) | (11.8–13.9) | (14.4–15.0) | (13.8–14.8) | (13.2–13.7) | (13.3–14.9) | ||
| General | 14.5 | 14.5 | 13.9 | 13.5 | 14.5 | 14.1 | 14.0 | 13.9 | |
| (14.1–14.8) | (14.1–14.9) | (13.3–14.5) | (12.4–14.7) | (13.9–15.0) | (13.6–14.6) | (13.4–14.5) | (13.4–14.4) | ||
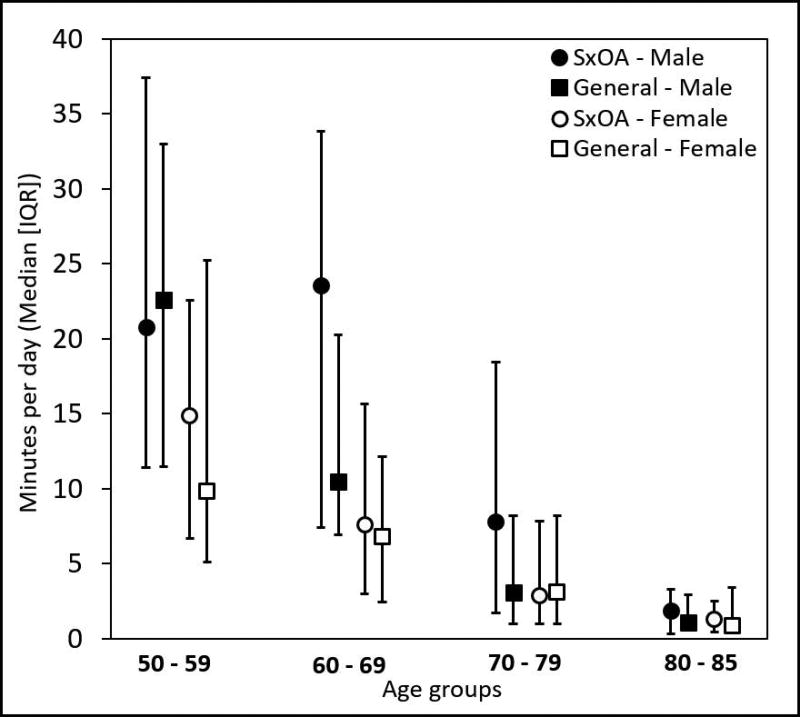
Time spent in MVPA was low and similar in people with SxOA compared with the general US population within age- and sex-specific strata. People with SxOA spent 1 to 24 min/day in MVPA (median), while the general population spent 1 to 22 min/day in MVPA (Figure 2). In both groups, time spent in MVPA decreased as age increased, and was generally higher in men compared to women.
Figure 2.
Median minutes per day (IQR) in MVPA for people with SxOA (from the OAI) and the general population without OA or knee symptoms (General – from the NHANES).
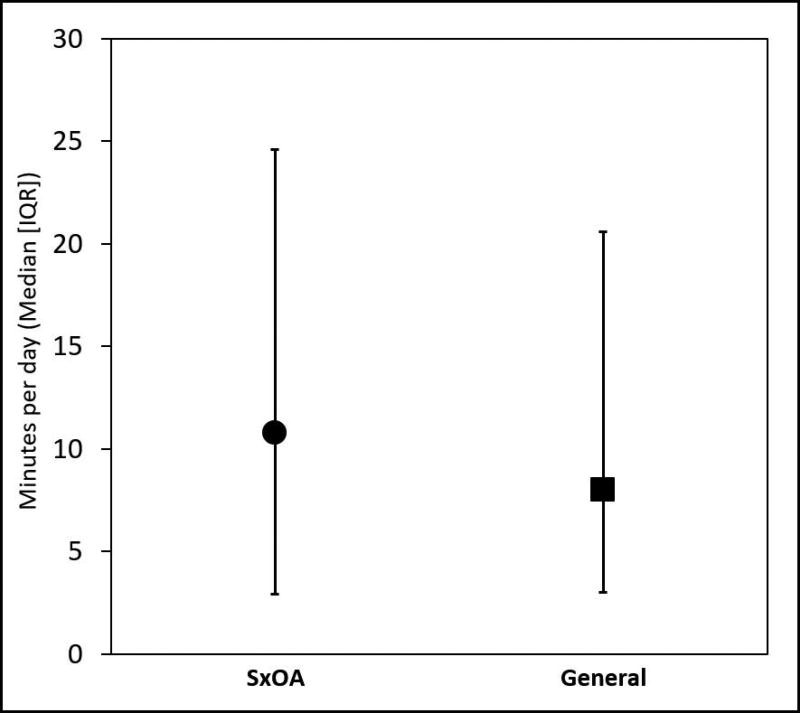
For our sensitivity analyses, the matching criteria produced 212 matches. Within each subsample, the median (IQR) time spent in MVPA was 10.8 (2.9–24.6) min/day in those with SxOA and 8.0 (3.0–20.6) min/day in the general population (Figure 3). Time spent in MVPA was log transformed for the analysis due to a skewed distribution. People with SxOA spent 28% (95% CI 6 to 54%, p-value=0.009) more time in MVPA than the general population without OA or knee pain. While a significant difference was found between the matched groups, this difference was attenuated by controlling for differences in education (12% difference, 95% CI −7 to 36%, p-value=0.26). The interaction between group and LQ pain was not significant, and therefore removed from the model.
Figure 3.
Median minutes per day (IQR) in MVPA for matched cohort for the sensitivity analysis. People with SxOA (n=212) were matched by age, BMI, sex, and college attendance to the general population without OA or knee symptoms (n=212).
DISCUSSION
We observed that people with SxOA and those in the general population accumulate similarly low amounts of objectively-determined MVPA. This observation was consistently held between people with SxOA and those from the general population for both men and women across the age ranges (Figure 1).
Low levels of MVPA in people with knee OA and adults from the general population observed in this study was not surprising. Contemporary studies consistently show a high prevalence of physical inactivity in the US [15, 24]. Despite national campaigns and increasing attention on the consequences of physical inactivity, only modest improvements in PA participation have been observed in the last 20 years [25], and the proportion of people who meet PA guidelines remains low. If people in the general population acquire PA from normal activities of daily life, it is not surprising that people with SxOA also exhibit at least this level of PA. Continued efforts are needed to design and implement national programs to successfully increase leisure time PA, regardless of the presence of knee symptoms.
Our sensitivity analysis offered further support of low amounts of MVPA among people with SxOA and the general population with OA or knee symptoms. In the sensitivity analysis, we identified pairs from each sample matched for age, sex, BMI, and post high school education, and controlled for the presence of other LQ pain. In this constrained analysis, both adults with SxOA and matched adults not reporting knee symptoms accumulated low levels of MVPA (median 10.8 vs. 8.0 minutes/day, Figure 3). Although the group difference was statistically significant controlling for LQ pain, the magnitude was small (<3 minute difference) and likely not clinically meaningful in the context of a 1440 minute day. Despite matching for post high school education, this may not adequately address differences in education level (see Education demographics in Table 1). In further analyses, group differences in PA were largely explained by explicitly controlling for differences in education levels between the matched samples, using education as a four-level covariate as indicated by the categories in Table 1. These findings support the observation that adults with SxOA did similar levels of MVPA to the general population without OA or knee symptoms.
The current study clarifies conflicting reports from previous studies regarding the PA level of people with SxOA relative to people in the general population without OA or knee symptoms. Smaller studies have reported lower levels of PA in people with knee OA compared to a healthy control group [11–13]. Conversely, previous studies using larger cohorts of people with knee OA [5, 7, 8, 14] reported a similar prevalence of meeting 2008 national PA guidelines using accelerometer-determined PA relative to reports from population-based studies [10, 15]. Similarly, a systematic review and meta-analysis by Wallis et al.[14] also noted that 59–87% of adults with knee OA fail to meet PA guidelines, which was consistent with findings in the general population [15]. The current study improves upon the current literature by directly comparing time spent in MVPA in people with SxOA to people without knee symptoms or OA using large datasets.
Modifiable barriers to participating in PA are similar in older adults with and without knee OA [26–28]. Common barriers that emerge from qualitative studies include physical limitations (i.e. pain severity, comorbidities, concerns for injury), social influences (i.e. lack of spousal support, lack of encouragement from others, anxiety), personal beliefs of benefits (i.e. no perceived benefits, ineffective, poor self-confidence), and environment (i.e. built environment, weather, affordability) [26–28]. Facilitators to PA participation are also similar among older adults with and without knee OA, including education regarding benefits and modes of PA, encouragement from physical therapists and physicians, positive self-image and self-confidence, ease of accessibility, and good social support [26–28]. While these qualitative studies provide a rich understanding regarding barriers and facilitators to PA, our understanding of the extent to which these factors indeed impact PA participation are limited. For example, people with knee OA perceive pain to be a barrier to PA [1]. Although the current study lacked data from the NHANES to evaluate the impact of knee pain severity on PA levels, a study by White and colleagues [8] observed that the proportions of people who met the 2008 Physical Activity Guidelines did not differ based on the presence of radiographic OA, or based on knee pain severity [8]. Taken together, these studies suggest that pain itself may be a perceived barrier, but potentially not the primary barrier to general levels of PA.
Our study has several limitations. As stated earlier, the two study samples employed different Actigraph models. The primary discordance between the two models was in measuring slow walking [23]. Thus, we only compared PA metrics that reflected MVPA to avoid inconsistencies due to Actigraph model. Another limitation of the Actigraph assessment of PA is that it does not include time in non-ambulatory PA, such as swimming or cycling. However, walking is the primary mode of MVPA for older adults[3], thus we do not expect that this limitation would alter the conclusions of this study. It should be noted that the NHANES is not a norm-referenced sample, and thus does not necessarily reflect a sample of healthy people. To reflect the general US population, the NHANES sample includes people with comorbidities or other chronic diseases [29]. Thus, it is not appropriate to conclude that people with OA have similar levels of PA as healthy adults per se. There is some indication that the 2003–2004 sample from the NHANES was particularly inactive [10, 30], and that adults in the United States may have increased physical activity levels between 2003–2004 (when NHANES data were collected) and 2008–2010 (when the OAI data were collected)[10]. Despite these potential differences, rates of physical inactivity remain high, thus we do not expect that the general conclusions of this study would change[10].
CONCLUSION
People with symptomatic knee OA and in the general population without OA or knee symptoms do little recommended MVPA. The results of this study reiterate the need for successful interventions to increase PA in the general population, as well as people with knee OA.
SIGNIFICANCE AND INNOVATIONS.
This study utilizes large well-established cohorts to compare objectively measured moderate-vigorous physical activity in people with symptomatic knee OA and people from the general population without OA or knee pain.
Physical activity was similarly low in both cohorts.
This study reiterates the pressing need to develop and implement successful interventions to increase PA in the general population and people with symptomatic knee OA, as the general population is doing as little as people with symptomatic knee OA.
Acknowledgments
Funding: Funding for DKW was provided by NIH U54 GM104941 and K12 HD055931. This study was funded in part by the National Institute for Arthritis and Musculoskeletal Diseases (grants R01-AR054155, R21-AR059412, and P60-AR064464) and by the Falk Medical Trust. The Osteoarthritis Initiative (OAI) is a public-private partnership comprised of five contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health, a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners include Merck Research Laboratories; Novartis Pharmaceuticals Corporation, GlaxoSmithKline; and Pfizer, Inc. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health. This manuscript was prepared using an OAI public use data set and does not necessarily reflect the opinions or views of the OAI investigators, the NIH, or the private funding partners.
Footnotes
Potential conflict of interest: None
References
- 1.Gyurcsik NC, Brawley LR, Spink KS, Brittain DR, Fuller DL, Chad K. Physical activity in women with arthritis. Examining perceived barriers and self-regulatory efficacy to cope. Arthritis Care & Research. 2009;61(8):1087–1094. doi: 10.1002/art.24697. [DOI] [PubMed] [Google Scholar]
- 2.Abell JE, Hootman JM, Zack MM, Moriarty D, Helmick CG. Physical activity and health related quality of life among people with arthritis. Journal of Epidemiology and Community Health. 2005;59(5):380–385. doi: 10.1136/jech.2004.028068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hootman JM, Macera CA, Ham SA, Helmick CG, Sniezek JE. Physical activity levels among the general US adult population and in adults with and without arthritis. Arthritis Care & Research. 2003;49(1):129–135. doi: 10.1002/art.10911. [DOI] [PubMed] [Google Scholar]
- 4.Shih M, Hootman JM, Kruger J, Helmick CG. Physical activity in men and women with arthritis National Health Interview Survey 2002. Am J Prev Med. 2006;30(5):385–393. doi: 10.1016/j.amepre.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 5.Farr JN, Going SB, Lohman TG, Rankin L, Kasle S, Cornett M, Cussler E. Physical activity levels in patients with early knee osteoarthritis measured by accelerometry. Arthritis Care & Research. 2008;59(9):1229–1236. doi: 10.1002/art.24007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Herbolsheimer F, Schaap LA, Edwards MH, Maggi S, Otero Á, Timmermans EJ, Denkinger MD, van der Pas S, Dekker J, Cooper C, et al. Physical Activity Patterns Among Older Adults With and Without Knee Osteoarthritis in Six European Countries. Arthritis Care & Research. 2016;68(2):228–236. doi: 10.1002/acr.22669. [DOI] [PubMed] [Google Scholar]
- 7.Dunlop DD, Song J, Semanik PA, Chang RW, Sharma L, Bathon JM, Eaton CB, Hochberg MC, Jackson RD, Kwoh CK, et al. Objective physical activity measurement in the osteoarthritis initiative. Are guidelines being met? Arthritis & Rheumatism. 2011;63(11):3372–3382. doi: 10.1002/art.30562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.White DK, Tudor-Locke C, Felson DT, Gross KD, Niu J, Nevitt M, Lewis CE, Torner J, Neogi T. Do radiographic disease and pain account for why people with or at high risk of knee osteoarthritis do not meet physical activity guidelines? Arthritis & Rheumatism. 2013;65(1):139–147. doi: 10.1002/art.37748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Medicine & Science in Sports & Exercise. 1998;30(5):777–781. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 10.Tucker JM, Welk GJ, Beyler NK. Physical Activity in U.S. Adults: Compliance with the Physical Activity Guidelines for Americans. American Journal of Preventive Medicine. 2011;40(4):454–461. doi: 10.1016/j.amepre.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 11.Watanabe H, Urabe K, Takahira N, Ikeda N, Fujita M, Obara S, Hendona T, Aikawa J, Itoman M. Quality of Life, Knee Function, and Physical Activity in Japanese Elderly Women with Early-Stage Knee Osteoarthritis. Journal of Orthopaedic Surgery. 2010;18(1):31–34. doi: 10.1177/230949901001800107. [DOI] [PubMed] [Google Scholar]
- 12.Winter CC, Brandes M, Müller C, Schubert T, Ringling M, Hillmann A, Rosenbaum D, Schulte TL. Walking ability during daily life in patients with osteoarthritis of the knee or the hip and lumbar spinal stenosis. a cross sectional study. BMC Musculoskeletal Disorders. 2010;11(1):233. doi: 10.1186/1471-2474-11-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brandes M, Schomaker R, Möllenhoff G, Rosenbaum D. Quantity versus quality of gait and quality of life in patients with osteoarthritis. Gait & Posture. 2008;28(1):74–79. doi: 10.1016/j.gaitpost.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 14.Wallis JA, Webster KE, Levinger P, Taylor NF. What proportion of people with hip and knee osteoarthritis meet physical activity guidelines? A systematic review and meta-analysis. Osteoarthritis and Cartilage. 2013;21(11):1648–1659. doi: 10.1016/j.joca.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 15.Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, Mcdowell M. Physical Activity in the United States Measured by Accelerometer. Medicine & Science in Sports & Exercise. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 16.Li J, Siegrist J. Physical activity and risk of cardiovascular disease--a meta-analysis of prospective cohort studies. Int J Environ Res Public Health. 2012;9(2):391–407. doi: 10.3390/ijerph9020391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sluik D, Buijsse B, Muckelbauer R, et al. Physical activity and mortality in individuals with diabetes mellitus. A prospective study and meta-analysis. Archives of Internal Medicine. 2012;172(17):1285–1295. doi: 10.1001/archinternmed.2012.3130. [DOI] [PubMed] [Google Scholar]
- 18.Wilmot EG, Edwardson CL, Achana FA, Davies MJ, Gorely T, Gray LJ, Khunti K, Yates T, Biddle SJH. Sedentary time in adults and the association with diabetes, cardiovascular disease and death. systematic review and meta-analysis. Diabetologia. 2012;55(11):2895–2905. doi: 10.1007/s00125-012-2677-z. [DOI] [PubMed] [Google Scholar]
- 19.Biswas A, Oh PI, Faulkner GE, Bajaj RR, Silver MA, Mitchell MS, Alter DA. Sedentary Time and Its Association With Risk for Disease Incidence, Mortality, and Hospitalization in AdultsA Systematic Review and Meta-analysisSedentary Time and Disease Incidence, Mortality, and Hospitalization. Annals of Internal Medicine. 2015;162(2):123–132. doi: 10.7326/M14-1651. [DOI] [PubMed] [Google Scholar]
- 20.Moore SC, Lee I, Weiderpass E, et al. ASsociation of leisure-time physical activity with risk of 26 types of cancer in 1.44 million adults. JAMA Internal Medicine. 2016;176(6):816–825. doi: 10.1001/jamainternmed.2016.1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Effect of physical inactivity on major non-communicable diseases worldwide. an analysis of burden of disease and life expectancy. The Lancet. 2012;380(9838):219–229. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Committee. PAG. Physical Activity Guidelines Advisory Committee report, 2008. To the Secretary of Health and Human Services. Part A: executive summary. Nutrition Reviews. 2009;67(2):114–120. doi: 10.1111/j.1753-4887.2008.00136.x. [DOI] [PubMed] [Google Scholar]
- 23.Kozey SL, Staudenmayer JW, Troiano RP, Freedson PS. A comparison of the ActiGraph 7164 and the ActiGraph GT1M during self-paced locomotion. Medicine & Science in Sports & Exercise. 2010;42(5):971–976. doi: 10.1249/MSS.0b013e3181c29e90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity levels. surveillance progress, pitfalls, and prospects. The Lancet. 380(9838):247–257. doi: 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]
- 25.Keadle SK, McKinnon R, Graubard BI, Troiano RP. Prevalence and trends in physical activity among older adults in the United States. A comparison across three national surveys. Preventive Medicine. 2016;89:37–43. doi: 10.1016/j.ypmed.2016.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Franco MR, Tong A, Howard K, Sherrington C, Ferreira PH, Pinto RZ, Ferreira ML. Older people's perspectives on participation in physical activity. a systematic review and thematic synthesis of qualitative literature. British Journal of Sports Medicine. 2015;49(19):1268–1276. doi: 10.1136/bjsports-2014-094015. [DOI] [PubMed] [Google Scholar]
- 27.Petursdottir U, Arnadottir SA, Halldorsdottir S. Facilitators and Barriers to Exercising Among People With Osteoarthritis. A Phenomenological Study. Physical Therapy. 2010;90(7):1014–1025. doi: 10.2522/ptj.20090217. [DOI] [PubMed] [Google Scholar]
- 28.Dobson F, Bennell KL, French SD, Nicolson PJA, Klaasman RN, Holden MA, Atkins L, Hinman RS. Barriers and Facilitators to Exercise Participation in People with Hip and/or Knee Osteoarthritis. Synthesis of the Literature Using Behavior Change Theory. American Journal of Physical Medicine & Rehabilitation. 2016;95(5):372–389. doi: 10.1097/PHM.0000000000000448. [DOI] [PubMed] [Google Scholar]
- 29.Song MR, Lee Y-S, Baek J-D, Miller M. Physical Activity Status in Adults with Depression in the National Health and Nutrition Examination Survey, 2005–2006. Public Health Nursing. 2012;29(3):208–217. doi: 10.1111/j.1525-1446.2011.00986.x. [DOI] [PubMed] [Google Scholar]
- 30.Berkemeyer K, Wijndaele K, White T, Cooper AJM, Luben R, Westgate K, Griffin SJ, Khaw KT, Wareham NJ, Brage S. The descriptive epidemiology of accelerometer-measured physical activity in older adults. International Journal of Behavioral Nutrition and Physical Activity. 2016;13(1):2. doi: 10.1186/s12966-015-0316-z. [DOI] [PMC free article] [PubMed] [Google Scholar]