Summary
Objective
Prior studies have suggested that weight misperception – underestimating one's actual weight – may be associated with reduced engagement in weight loss programmes, decreasing the success of initiatives to address obesity and obesity‐related diseases. The purpose of this study was to examine the factors associated with weight misperception among Eastern Caribbean adults and its influence on engagement in weight control behaviour.
Methods
Data from the Eastern Caribbean Health Outcomes Research Network (ECHORN) Cohort Study were analysed (adults aged 40 and older, residing in the US Virgin Islands, Puerto Rico, Barbados and Trinidad). Weight misperception is defined as participants who under‐assess their weight measured by body mass index (BMI). Multivariable logistic regression (n = 1,803 participants) was used to examine the association of weight misperception with BMI category, age, gender, education, history of non‐communicable disease and attempt to lose weight.
Results
Weight misperception was common, with 54% of overweight (BMI 25–29 kg m−2), and 23% of obese class I (BMI 30–34.9 kg m−2) participants under‐assessing their actual weight. Participants with higher levels of education, versus lower, had decreased odds of weight misperception (OR 0.5, p < 0.001). There were no significantly reduced odds of weight misperception in women versus men (OR 1.13, p = 0.367) or in individuals with history of diabetes versus none (OR 0.88, p = 0.418). Participants with weight misperception had 85% (p < 0.0001) lower odds of attempting weight loss than those with accurate weight perception.
Conclusion
Weight misperception is common among adults with overweight and obesity in the Eastern Caribbean and is associated with lower likelihood of attempting weight loss. Obesity interventions, targeting similar populations, should incorporate approaches for addressing weight misperception to achieve measurable success.
Keywords: Caribbean, ECHORN, obesity, perception
Introduction
The global burden of obesity has been increasing steadily over the past three decades with 1.9 billion overweight adults and more than half a billion obese in 2014 1. Obesity and its associated comorbid conditions 2, 3, 4 cause 5% of deaths worldwide at a cost of US$ 2 trillion 5. Multiple factors contribute to this obesity pandemic: the obesogenic food environment, decreased energy expenditure and psychosocial factors 6. The latter includes weight perception that has received significant attention in the last decade 7, 8, 9, 10, 11. Evidence suggests that the increasing rate of overweight and obesity has been accompanied by decreasing perception of overweight status 12, 13. This psychosocial phenomenon has important public health implications as it lowers awareness of obesity‐related risk factors, utilization of the health system and interest in, or attempts at, weight loss 8, 14.
Current obesity interventions often try to achieve a 5–10% reduction in weight that has been associated with improvements in hypertension, cardiovascular disease and diabetes 15, 16, 17. Participant perception of their weight has been shown to influence the effectiveness of these interventions 18. Weight misperception is the term that has been coined to describe individuals who are overweight and obese but who perceive themselves to be of a ‘normal’ weight. Prior studies have shown that weight misperception is more common among men, those of lower socioeconomic status, and among some racial/ethnic minority groups in the USA 19, 20. Evidence suggests that weight perception (and misperception) stems in part from sociocultural body image norms and ideals 21, 22, 23, 24. The varied prevalence of weight misperception among subpopulations and its significant public health impact speaks to the importance of quantifying and qualifying weight misperception among different populations as a first step to addressing obesity in these groups.
To our knowledge, this paper is the first to describe weight misperception and weight control behaviour among adults in the Eastern Caribbean. This is a region of the world that is experiencing an increasing burden of obesity and non‐communicable diseases (NCDs) 25, 26 and contributes a sizeable proportion of the immigrant minority population to the USA. This information is, therefore, relevant to regional health and civil society organizations that are targeting obesity in the Caribbean 26, 27, 28, 29 as well as US‐based initiatives seeking to address obesity disparities by tailoring interventions to minority populations that include Caribbean and Caribbean‐descent individuals 30.
This study used data from the Eastern Caribbean Health Outcomes Research Network (ECHORN) Cohort Study (ECS). The ECS follows community‐dwelling adults on the islands of the US Virgin Islands, Puerto Rico, Barbados and Trinidad with the goal of furthering our understanding of risk factors and early predictors for cancer, diabetes and cardiovascular disease in this population. The hypothesis for this study was that the rate of weight misperception would be high and that this would be associated with lower rates of engagement in weight loss activities. However, given evidence around strong and prevalent body image ideals in similar populations 21, 22, 23, 24, 31, 32, the prediction was that the rate of weight misperception may be similar in men and women and not influenced by socioeconomic status in the same way as reported in other US‐based studies.
Methods
Study population
Data were derived from the ECS at baseline. Eligibility criteria included: age > 40 years, English or Spanish speaking, reliable contact information, has been semi‐permanent or permanent resident of the island for the past 10 years with no plans to relocate in the next 5 years. Pregnancy was an exclusionary criterion. A random sampling frame was used for recruitment at each site: small islands included the entire island; larger islands (Puerto Rico, Trinidad) selected two communities with demographics representative of the island (similar distributions of age, race/ethnicity, sex and educational levels to the general island population). ECS baseline participants were enrolled between 2013 and 2016. They completed a baseline survey that captured sociodemographic, health status and health behaviour information. The survey was conducted using computer guided and audio‐assisted software. Participants also completed a brief physical exam and laboratory assessment.
The ECHORN Cohort Study was approved by the Yale University Human Subjects Investigation Committee and the Institutional Review Boards of the University of the West Indies, the Ministry of Health Trinidad and Tobago, the University of Puerto Rico, Medical Sciences Campus and the University of the US Virgin Islands. Informed consent was required for participation in the study. The approvals also included the use and analysis of de‐identified, programmatic data.
Measures
Body Mass Index (BMI). Height and weight of the participants was measured using standardized anthropometric methods. BMI was calculated, and participant weight status was classified as normal (BMI 18–24 kg m−2), overweight (BMI 25–29 kg m−2), obese class I (BMI 30–34 kg m−2) or obese classes II and III (BMI ≥ 35 kg m−2).
Weight misperception
Participants answered the question: ‘Do you consider yourself to be 1. Right weight, 2. Underweight, 3. Overweight’. This is a standard question that has previously been used by the National Health and Nutrition Examination Survey 33 and assumes that persons with obesity would also classify themselves as ‘overweight’. For this study, weight misperception was defined as ‘under‐assessors’, those who perceive their weight to be less than it actually is (as measured by BMI). Therefore, participants who had a BMI ≥ 25 kg m−2 and answered ‘right weight’ or ‘underweight’ were classified as having weight misperception. Similarly, those who had a normal weight (BMI 18–25 kg m−2) and who responded ‘underweight’ were under‐assessors and classified as having weight misperception. The goal of this study was to understand weight misperception in the context of obesity and inform interventions, therefore, ‘over‐assessors’ were not included in the definition of misperception.
Weight control behaviour
Participant engagement in weight control behaviour was determined based on their answer to the question: ‘Are you currently trying to: 1. Lose weight, 2. Stay the same weight, 3. Gain weight, 4. Do nothing’. If participants answered they were trying to ‘lose weight’, they were classified as engaging in weight loss activities. Any other response, they were classified as not engaging in weight control behaviour.
Other covariates
The following covariates were used in the analysis: age, gender, education level (high school diploma and higher or less than a high school diploma), self‐reported NCD (pre‐diabetes, diabetes, hypertension, cardiovascular disease) and physical activity (low, moderate or high). For physical activity, the Global Physical Activity Questionnaire (GPAQ) was used 34; established methods were used to translate GPAQ responses to metabolic equivalent time (MET‐minute) and determine overall high (vigorous‐intensity activity on at least 3 d achieving minimum of 1,500 MET‐minute per week, or vigorous‐intensity activities achieving a minimum of 3,000 MET‐minute per week), moderate (not meeting high criteria but who have ≥3 d of vigorous intensity activity of at least 20 min per day or ≥5 d of moderate‐intensity activity; walking at least 30 min per day or ≥5 d of walking; moderate or vigorous‐intensity activities with minimum of 600 MET‐minute per week) and low (not meeting moderate or high criteria) physical activity level 35. Diet and nutrition related data were not available at the time of these analyses.
Study sample
All participants who had data available for analysis were initially included (n = 2,693). Pregnant women were not included in our cohort study. Figure 1 depicts how the final sample size of 1,803 participants was obtained. First, participants who did not have a BMI available (n = 103) were excluded. Then, participants who did not answer the weight perception question (n = 14) were excluded; followed by the four participants who had not answered the weight management question. Individuals with underweight BMI status (<18 kg m−2, n = 31) were then excluded as they were not relevant to our discussion around weight misperception and weight management. Next, 44 participants with a normal BMI, but who perceived themselves as overweight (18–24 kg m−2), were excluded: these individuals are not classified as ‘under‐assessors’ and therefore do not meet our weight misperception definition. An additional 694 participants were excluded because they had one of the following variables of interest missing: age, education, gender, self‐reported NCD, GPAQ. This left us with a final sample size of 1,803. This sample size is comparable with other published weight perception studies that were not solely based on national survey data 18, 31, 32.
Figure 1.
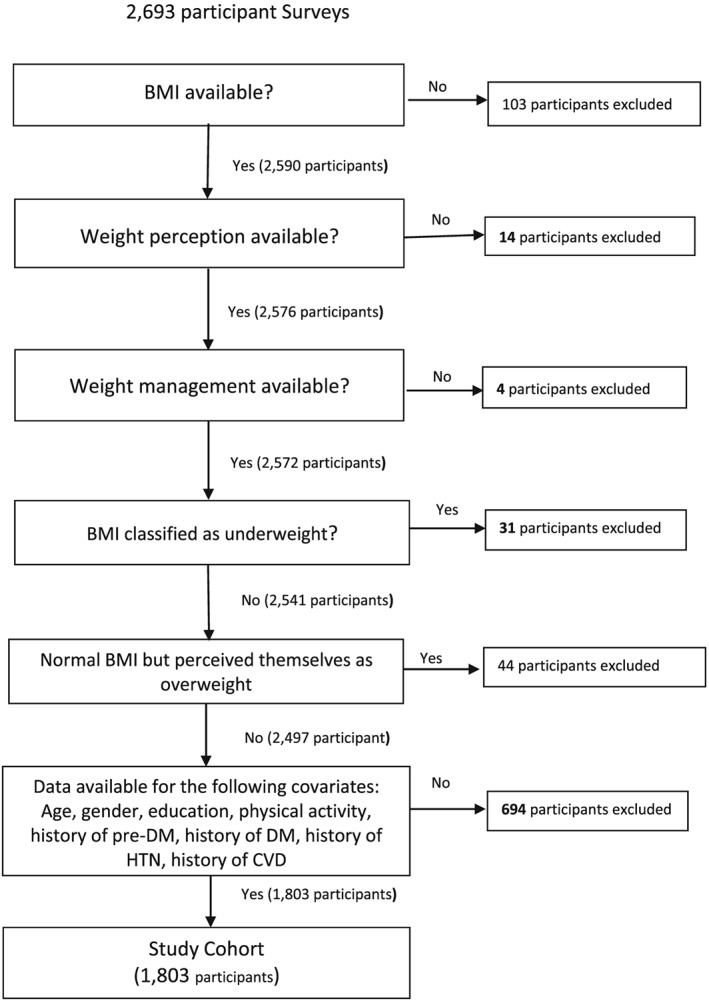
A schematic diagram describing participant exclusions and final study sample. BMI, body mass index; CVD, cardiovascular disease.
Statistical analysis
Bivariate analyses, using chi‐squared, were used to compare demographic and clinical characteristics of subjects across BMI categories. Two multivariable logistic regression models were then used to test our hypotheses. The first was the weight misperception model that tested the null hypothesis that there was no relationship between weight misperception and weight control activity or any of the other variables of interest. The second was the weight control activity model that tested the null hypothesis that there was no association between weight control activity and weight misperception or any of the other variables of interest. In both models, adjusted analyses were conducted controlling for: age, gender, education level, BMI, physical activity, history of any NCD and weight control/weight misperception. Total number of NCDs was not included in the adjusted model to avoid collinearity. Data were analysed using SAS software (version 9.4; SAS Institute, Cary, NC).
Results
Characteristics of the study population
The gender distribution of the sample was 65.6% female and 34.4% male, the average age of the study population was 57 ± 10 years, and the majority (65%) had a high school diploma or greater level of education. Importantly, we did not find any statistically significant difference between our sample population (n = 1,803) and the cohort population (n = 2,693) in average age, gender distribution, average BMI, educational level or prevalence of self‐reported NCDs (diabetes, prediabetes, hypertension, cardiovascular disease). Table 1 shows the measured BMI distribution by selected characteristics of the study population. The combined prevalence of overweight and obesity was 76% with an average BMI of 29.6 ± 6.5 kg m−2. There was no difference in educational level between BMI categories. Statistically significant differences between BMI categories were observed for age, gender, physical activity level, history of pre‐diabetes, history of diabetes, history of hypertension and number of NCDs. Weight misperception was present in nearly one‐third (30%) of the cohort and varied by BMI category with the highest prevalence of 54% among overweight, and 23% among obese class I, participants. The prevalence of engagement in weight control activities increased with increasing BMI.
Table 1.
Measured BMI distribution of ECS adults and selected characteristics
| Demographic characteristic | Total (n = 1,803) | Normal (18.5 < BMI < 25) | Overweight (25 < BMI < 30) | Obese | p‐value* | ||
|---|---|---|---|---|---|---|---|
| Class I (30 < BMI < 35) | Class II (35 < BMI < 40) | Class III (BMI > 40) | |||||
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||
| Age | 0.0008 | ||||||
| 40–50 | 446 (24.7) | 84 (19.7) | 149 (22.9) | 116 (28.8) | 65 (29.0) | 32 (32.3) | |
| 50–59 | 663 (36.8) | 146 (34.2) | 238 (36.6) | 156 (38.7) | 82 (36.6) | 41 (41.4) | |
| 60–69 | 457 (25.4) | 122 (28.6) | 173 (26.6) | 87 (21.6) | 54 (24.1) | 21 (21.2) | |
| 70+ | 237 (13.1) | 75 (17.6) | 90 (13.9) | 44 (10.9) | 23 (10.3) | 5 (5.1) | |
| Gender | <0.0001 | ||||||
| Male | 620 (34.4) | 193 (45.2) | 253 (38.9) | 111 (27.5) | 49 (21.9) | 14 (14.1) | |
| Female | 1,183 (65.6) | 234 (54.8) | 397 (61.1) | 292 (72.5) | 175 (78.1) | 85 (85.9) | |
| Educational level | 0.7945 | ||||||
| Less than a high school diploma | 633 (35.1) | 154 (36.1) | 229 (35.2) | 146 (36.2) | 71 (31.7) | 33 (33.3) | |
| High school diploma or higher | 1,170 (64.9) | 273 (63.9) | 421 (64.8) | 257 (63.8) | 153 (68.3) | 66 (66.7) | |
| Physical Activity | <0.0001 | ||||||
| Low | 815 (45.2) | 171 (40.1) | 263 (40.5) | 214 (53.1) | 110 (49.1) | 57 (57.6) | |
| Moderate | 338 (18.8) | 80 (18.7) | 121 (18.6) | 77 (19.1) | 46 (20.5) | 14 (14.1) | |
| High | 650 (36.1) | 176 (41.2) | 266 (40.9) | 112 (27.8) | 68 (30.4) | 28 (28.3) | |
| History of pre‐diabetesa | 0.0111 | ||||||
| No pre‐diabetes | 1,709 (94.8) | 416 (97.4) | 616 (94.8) | 375 (93.1) | 206 (92.0) | 96 (97.0) | |
| Pre‐diabetes | 94 (5.2) | 11 (2.6) | 34 (5.2) | 28 (7.0) | 18 (8.0) | 3 (3.0) | |
| History of diabetes | 0.0316 | ||||||
| No diabetes | 1,397 (77.5) | 337 (78.9) | 521 (80.2) | 301 (74.4) | 171 (76.3) | 67 (67.7) | |
| Diabetes | 406 (22.5) | 90 (21.1) | 129 (19.9) | 102 (25.3) | 53 (23.7) | 32 (32.3) | |
| History of hypertensiona | <0.0001 | ||||||
| No hypertension | 919 (51.0) | 269 (63.0) | 351 (54.0) | 186 (46.2) | 80 (35.7) | 33 (33.3) | |
| Hypertension | 884 (49.0) | 158 (37.0) | 299 (46.0) | 217 (53.9) | 144 (64.3) | 66 (66.7) | |
| History of CVDa | 0.2472 | ||||||
| No CVD | 1,529 (84.8) | 366 (85.7) | 552 (84.9) | 343 (85.1) | 192 (85.7) | 76 (76.8) | |
| CVD | 274 (15.2) | 61 (14.3) | 98 (15.1) | 60 (14.9) | 32 (14.3) | 23 (23.2) | |
| Number of NCDsb | <0.0001 | ||||||
| No NCD | 705 (39.1) | 205 (48.0) | 272 (41.9) | 139 (34.5) | 63 (28.1) | 26 (26.3) | |
| 1 NCD | 622 (34.5) | 138 (32.3) | 228 (35.1) | 139 (34.5) | 89 (39.7) | 28 (28.3) | |
| 2 NCDs | 392 (21.7) | 70 (16.4) | 118 (18.2) | 107 (26.6) | 58 (25.9) | 39 (39.4) | |
| 3+ NCDs | 84 (4.7) | 14 (3.3) | 32 (4.9) | 18 (4.5) | 14 (6.3) | 6 (6.1) | |
| Weight perception | <0.0001 | ||||||
| Weight MIS‐perception | 545 (30.2) | 76 (17.8) | 353 (54.3) | 94 (23.3) | 18 (8.0) | 4 (4.0) | |
| Accurate weight perception | 1,258 (69.8) | 351 (82.2) | 297 (45.7) | 309 (76.7) | 206 (92.0) | 95 (96.0) | |
| Weight control behaviour | <0.0001 | ||||||
| Trying to lose weight | 836 (46.4) | 28 (6.6) | 286 (44.0) | 263 (65.3) | 169 (75.5) | 90 (90.9) | |
| NOT trying to lose weight | 967 (53.6) | 399 (93.4) | 364 (56.0) | 140 (34.7) | 55 (24.6) | 9 (9.1) | |
Values are n (col%) for categorical variables.
p‐value connotes significance of chi‐squared test of association between BMI categories and selected characteristic. Significant values p < 0.05 denoted with bold.
Self‐reported history of pre‐diabetes, diabetes, hypertension or cardiovascular disease (CVD).
Self reported history of non‐communicable disease (NCD) including pre‐diabetes, diabetes, hypertension and cardiovascular disease.
BMI, body mass index; ECS, Eastern Caribbean Health Outcomes Research Network (ECHORN) Cohort Study.
Weight misperception
Table 2 presents the unadjusted and adjusted odds of weight misperception by selected characteristics. The adjusted model shows greater odds of misperception for those who are overweight (OR 13.55, 95% CI 9.66, 19.01) and obese class I (OR 4.11, 95% CI 2.78, 6.07) compared with normal weight participants, and age at least 70 compared with 40–50‐year‐olds (OR 1.87, 95% CI 1.21, 2.90). Higher level of education had significantly reduced odds of weight misperception (OR 0.50, 95% CI 0.39, 0.64) as did history of pre‐diabetes (OR 0.31, 95% CI 0.16, 0.62). Within obesity class, analyses were conducted to determine how odds of weight misperception varied among participants in the lower versus higher quartile of each obesity class. Results fell in line with the overall trend that is seen in Table 2 with decreasing odds of weight misperception as the BMI increased (data not shown). For example, for the overweight BMI class (25–29.9 kg m−2), the odds ratio within quartiles was as follows: BMI 25.0–26.2 kg m−2 (OR 11.31, 95% CI 7.56, 16.92); BMI 26.3–27.6 kg m−2 (OR 7.84, 95% CI 5.33, 11.53); BMI 27.7–28.8 kg m−2 (OR 4.18, 95% CI 2.87, 6.11); BMI 28.9–29.9 kg m−2 (OR 2.59, 95% CI 1.76, 3.82). The association of the level of physical activity as reported by the GPAQ is similar to previously reported studies where participants with high levels of physical activity had a higher odds of weight misperception (OR 1.48, 95% CI 1.11, 1.95). In the adjusted model, there was no gender difference in the odds of weight misperception. Therefore, gender stratified analyses were not conducted. Notably, the number of chronic diseases a participant had did not significantly influence the odds of weight misperception.
Table 2.
Unadjusted and adjusted odds of weight misperception by selected characteristics
| Demographic characteristic | Unadjusted | Multivariable (adjusted) | ||||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p‐value | OR | 95% CI | p‐value* | |||
| Weight control | ||||||||
| Not trying to lose weight | Reference | Reference | ||||||
| Trying to lose weight | 0.23 | 0.18 | 0.29 | <0.0001 | 0.156 | 0.12 | 0.21 | <0.0001 |
| Age | ||||||||
| 40–50 | Reference | Reference | ||||||
| 50–59 | 1.23 | 0.93 | 1.62 | 0.1525 | 1.08 | 0.77 | 1.50 | 0.6717 |
| 60–69 | 1.69 | 1.26 | 2.26 | 0.0005 | 1.26 | 0.87 | 1.83 | 0.2271 |
| 70+ | 2.66 | 1.90 | 3.73 | <0.0001 | 1.87 | 1.21 | 2.90 | 0.0052 |
| Gender | ||||||||
| Male | Reference | Reference | ||||||
| Female | 0.78 | 0.63 | 0.96 | 0.0199 | 1.13 | 0.87 | 1.46 | 0.3673 |
| BMI class | ||||||||
| Normal | Reference | Reference | ||||||
| Overweight | 5.49 | 4.10 | 7.35 | <0.0001 | 13.55 | 9.66 | 19.01 | <0.0001 |
| Obese class I | 1.41 | 1.00 | 1.97 | 0.0492 | 4.11 | 2.78 | 6.07 | <0.0001 |
| Obese class II + III | 0.34 | 0.21 | 0.56 | <0.0001 | 1.14 | 0.66 | 1.97 | 0.6294 |
| Educational level | ||||||||
| Less than high school diploma | Reference | Reference | ||||||
| High school diploma and higher | 0.55 | 0.45 | 0.68 | <0.0001 | 0.50 | 0.39 | 0.64 | <0.0001 |
| Physical Activity | ||||||||
| Low | Reference | Reference | ||||||
| Moderate | 1.03 | 0.78 | 1.37 | 0.8299 | 0.99 | 0.70 | 1.39 | 0.9349 |
| High | 1.41 | 1.13 | 1.76 | 0.0027 | 1.48 | 1.11 | 1.95 | 0.0066 |
| History of pre‐diabetesa | ||||||||
| No pre‐diabetes | Reference | Reference | ||||||
| Pre‐diabetes | 0.323 | 0.18 | 0.60 | 0.0003 | 0.31 | 0.16 | 0.62 | 0.0009 |
| History of diabetesa | ||||||||
| No diabetes | Reference | Reference | ||||||
| Diabetes | 1.00 | 0.79 | 1.28 | 0.9729 | 0.88 | 0.64 | 1.20 | 0.418 |
| History of hypertensiona | ||||||||
| No hypertension | Reference | Reference | ||||||
| Hypertension | 1.11 | 0.91 | 1.36 | 0.3153 | 1.11 | 0.85 | 1.46 | 0.4334 |
| History of CVDa | ||||||||
| No CVD | Reference | Reference | ||||||
| CVD | 0.98 | 0.74 | 1.30 | 0.9066 | 0.97 | 0.69 | 1.37 | 0.8666 |
| Number of NCDsb | ||||||||
| No NCD | Reference | N/A | ||||||
| 1 NCD | 1.02 | 0.81 | 1.29 | 0.8395 | ||||
| 2 NCDs | 0.95 | 0.73 | 1.25 | 0.7244 | ||||
| 3+ NCDs | 0.92 | 0.56 | 1.51 | 0.7365 | ||||
Significant values with p < 0.05 denoted in bold.
Binary multivariable regression model adjusted for all variables in the table. Significant values denoted with bold font.
Self‐reported history of pre‐diabetes, diabetes, hypertension or cardiovascular disease (CVD).
Total number of self‐reported history of non‐communicable diseases (NCD) including pre‐diabetes, diabetes, hypertension and cardiovascular disease. Not included in multivariable model (overlap with independent NCD variable).
BMI, body mass index.
Weight control behaviour
Table 3 reports the unadjusted and adjusted odds of engaging in weight control behaviour. In the adjusted model, there is 85% reduced odds (OR: 0.15, 95% CI 0.11, 0.20) of engaging in weight control behaviour among those with weight misperception. There are significantly higher odds of engaging in weight control behaviour among females (OR 1.59, 95% CI 1.23, 2.07) compared with males. In gender stratified analyses (data not shown), weight misperception led to lower odds of engaging in weight control behaviour in men (OR 0.12; p < 0.0001) than in women (OR 0.17; p < 0.0001). There was a dose–response relationship between BMI category and weight control behaviour such that as BMI category increased (from overweight to obese I to obese II and III), the odds of ‘trying to lose weight’ also increased. In the adjusted model, participants with a higher level of education had lower odds of engagement in weight control activity (OR 0.73, 95% CI 0.56, 0.95). Notably, however, the number of NCDs did not influence the odds of engagement in weight control activity. It is also noteworthy that there is a correlation between the level of physical activity and reported engagement in weight control behaviour: higher odds of reporting attempt to lose weight if GPAQ indicates high physical activity versus low physical activity levels (OR 1.42, 95% CI 1.07, 1.88).
Table 3.
Unadjusted and adjusted odds of engaging in weight control behaviour
| Demographic characteristic | Unadjusted | Multivariable (adjusted) | ||||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p‐value | OR | 95% CI | p‐value* | |||
| Weight perception | ||||||||
| Accurate weight perception | Reference | Reference | ||||||
| Weight MIS‐perception | 0.23 | 0.18 | 0.29 | <0.0001 | 0.15 | 0.11 | 0.20 | <0.0001 |
| Age | ||||||||
| 40–50 | Reference | Reference | ||||||
| 50–59 | 0.77 | 0.60 | 0.98 | 0.0316 | 0.84 | 0.62 | 1.15 | 0.2775 |
| 60–69 | 0.42 | 0.32 | 0.55 | <0.0001 | 0.46 | 0.32 | 0.65 | <0.0001 |
| 70+ | 0.22 | 0.16 | 0.32 | <0.0001 | 0.28 | 0.17 | 0.44 | <0.0001 |
| Gender | ||||||||
| Male | Reference | Reference | ||||||
| Female | 1.96 | 1.60 | 2.39 | <0.0001 | 1.59 | 1.23 | 2.07 | 0.0005 |
| BMI class | ||||||||
| Normal | Reference | Reference | ||||||
| Overweight | 11.19 | 7.40 | 16.92 | <0.0001 | 25.38 | 16.16 | 39.85 | <0.0001 |
| Obese class I | 26.76 | 17.33 | 41.33 | <0.0001 | 35.82 | 22.50 | 57.03 | <0.0001 |
| Obese class II + III | 57.65 | 36.00 | 92.32 | <0.0001 | 55.55 | 33.76 | 91.38 | <0.0001 |
| Educational level | ||||||||
| Less than high school diploma | Reference | Reference | ||||||
| High school diploma and higher | 1.13 | 0.93 | 1.37 | 0.2161 | 0.73 | 0.56 | 0.95 | 0.0195 |
| Physical Activity | ||||||||
| Low | Reference | Reference | ||||||
| Moderate | 0.96 | 0.74 | 1.24 | 0.7482 | 1.06 | 0.76 | 1.47 | 0.7295 |
| High | 0.90 | 0.73 | 1.11 | 0.3291 | 1.42 | 1.07 | 1.88 | 0.0145 |
| History of pre‐diabetesa | ||||||||
| No pre‐diabetes | Reference | Reference | ||||||
| Pre‐diabetes | 1.84 | 1.20 | 2.81 | 0.0049 | 1.11 | 0.66 | 1.87 | 0.6957 |
| History of diabetesa | ||||||||
| No diabetes | Reference | Reference | ||||||
| Diabetes | 1.09 | 0.87 | 1.36 | 0.4448 | 1.31 | 0.96 | 1.79 | 0.0874 |
| History of hypertensiona | ||||||||
| No hypertension | Reference | Reference | ||||||
| Hypertension | 1.20 | 0.99 | 1.44 | 0.0575 | 0.97 | 0.74 | 1.27 | 0.8189 |
| History of CVDa | ||||||||
| No CVD | Reference | Reference | ||||||
| CVD | 1.17 | 0.90 | 1.51 | 0.2391 | 1.26 | 0.89 | 1.78 | 0.1915 |
| Number of NCDsb | ||||||||
| No NCD | Reference | N/A | ||||||
| 1 NCD | 1.04 | 0.84 | 1.30 | 0.7024 | ||||
| 2 NCDs | 1.33 | 1.04 | 1.70 | 0.025 | ||||
| 3+ NCDs | 1.54 | 0.98 | 2.43 | 0.0617 | ||||
Significant values with p‐value < 0.05 denoted in bold.
Binary multivariable regression model adjusted for all variables in the table. Significant values denoted with bold font.
Total number of self‐reported history of non‐communicable diseases (NCD) including pre‐diabetes, diabetes, hypertension and cardiovascular disease. Not included in multivariable model (overlap with independent NCD variable).
BMI, body mass index.
Discussion
This study identified that weight misperception was common among ECS participants with 31% of the entire cohort, 54% of overweight and 23% of obese class I participants under‐assessing their actual weight. Importantly, weight misperception conferred significantly lower odds of engaging in weight control behaviour. This corroborates evidence from other populations that an individual will not seek a solution (weight control) to a problem (overweight) they do not recognize exists 8, 36, 37. These results are also consistent with health behaviour theories that suggest that perceived susceptibility to a given condition is necessary to promote healthful behaviour change. This highlights the importance of addressing weight perception as part of any lifestyle or behaviour change intervention that targets a similar population.
This study uses a more comprehensive definition of weight misperception for purposes of understanding societal and cultural views by focusing on ‘under‐assessors’ across the spectrum of BMI. In so doing, the study adds to the established weight misperception literature in the following significant ways that will be elaborated upon in the succeeding text: it addresses weight misperception in a diverse Caribbean population highlighting its prevalence, associated factors and gender indifference. Furthermore, it underscores the fact that weight misperception remains prevalent in individuals with several NCDs, thereby highlighting the importance of providers discussing weight and its contribution to chronic disease during patient visits. Additionally, this study indicates that the relationship between weight misperception and weight control behaviour could potentially be bidirectional.
The odds of weight misperception were significantly higher in those who are overweight. Among individuals with obesity class I, there was alarmingly still an increased odds of weight misperception, while higher obesity classes conferred a lower odds of weight misperception. This implies that among this cohort of participants, there is a new calibration of what is considered ‘normal’ weight: overweight (by BMI) is perceived as ‘normal’ by most, and only extreme obesity is consistently considered ‘overweight’. While it was encouraging to see higher odds of engagement in weight control behaviour with increasing BMI, it is important to recognize that even after controlling for BMI, the odds of engaging in weight control behaviour among participants with weight misperception were 84% lower, compared with those with accurate weight perception. In other words, weight perception, independent of BMI has significant implications for obesity interventions.
Unlike other weight perception literature from the US mainland, we did not find a gender difference in the prevalence of weight misperception. Previous studies have reported weight misperception to be more common in men than in women 19, 20, 38. In our study, after controlling for other factors, there was no gender effect. This may be due in part to the higher proportion of women than men in ECS, as well as the overall high prevalence of weight misperception in this cohort compared with other studies 8, 14, 19, 20. However, this may also be due to an earlier onset of weight misperception in this population, with children and adolescents acquiring an understanding from their families and surrounding communities that what would be classified as ‘overweight’ is actually desirable. In US‐based studies, adolescent males are more likely to misperceive their weight than females 39; similar studies with adolescents in the Eastern Caribbean would help elucidate the origins of gender‐based weight misperception. Despite there being no differences in weight misperception between men and women, women were more likely to engage in weight control behaviour than men even after controlling for BMI and weight misperception. This is similar to findings from other studies that have examined weight loss attitudes and behaviours 8, 36, 37. This speaks to the urgency in identifying more effective ways of engaging men in discussions about healthy weight and practical approaches to reducing weight.
Interestingly, in the unadjusted analyses, we found no association between the number of reported NCDs and the odds of weight misperception. The expectation would be that with more chronic diseases associated with their weight, an individual would be more apt to realize their weight was a problem. This highlights the importance of education on the deleterious effects of obesity on health and that diseases like diabetes and hypertension are in large part related consequences of unhealthy weight. This education should start with the clinical providers, who must consistently record their patient's BMI and discuss weight status and its contribution to the patient's diabetes, hypertension or other NCD. Chart audits from practices in the region have shown under‐reporting of BMI among patients with NCDs 40, 41; if the physician does not recognize and educate the patient on the implications of their overweight or obese status, it is unlikely that the patient will have accurate weight perception. Pre‐diabetes was the only NCD that conferred a lower odds of weight misperception. This is likely due to a ‘pre‐diabetes status’ motivating individuals to act before they develop diabetes. Individuals with pre‐diabetes are likely to be more cognizant of their weight and that controlling their weight can prevent them from developing diabetes. This is consistent with data from the Diabetes Prevention Program that showed that those who misperceived their weight, and subsequently told they have pre‐diabetes, were motivated to lose weight 18. However, we found no association between the type of NCD or the number of NCDs and the odds of engaging in weight control behaviour. This is similar to prior reports and echoes the importance of education on the association of weight and NCDs 36, 42, 43.
Similar to previous reports, we found an association between educational level and weight misperception 7, 38. This is important because education can be considered a proxy for socioeconomic status; it is the most frequently used measure and correlated with many health‐related outcomes 44, 45, 46, 47. Interestingly, while those without a high school diploma had higher odds of weight misperception, the rate of overweight and obesity in those with and without a high school diploma was similar (75% and 76%, respectively). This is different from published reports from high income countries like the USA where obesity rates are higher among those with a lower education level 47, 48; and from low and middle‐income countries where obesity rates are higher among those with a higher education level 49, 50. It is possible that the similar rates of obesity among those with higher and lower educational levels are due to the combined effect of differences in weight misperception, as well as the lower odds of engagement in weight control behaviour in those with a higher education. Declining rates of physical activity with increasing socioeconomic status have been reported in other low and middle‐income countries 51. These data on the effect of educational level on weight misperception, weight control, and subsequent obesity, are evidence that health education literature targeting all levels of socioeconomic status is needed to alter the normative ideas of healthy weight and the importance of weight control.
There were a few limitations of this study to note. Its cross‐sectional design does not allow one to determine causality of weight misperception leading to a change in weight control behaviour. This study shows that the odds of weight misperception are higher in individuals who report attempting weight loss, thereby indicating the potential bidirectional nature of the association between weight misperception and engagement in weight control behaviour. Given the longitudinal nature of ECS, there is potential to answer this question with future waves of data. This study uses BMI to determine obesity status. There is some literature to support the use of anthropometric measures of central adiposity as more accurate assessments of obesity in similar population 52, 53, 54. Therefore, the prevalence of weight misperception may be different if obesity were defined by waist circumference or waist to hip ratio. In fact, unpublished data show higher rates of obesity in ECS if waist circumference and waist to hip ratio are used, so we would expect higher rates of weight misperception with central adiposity measures 55. However, the established literature on weight perception references BMI so for comparative purposes, it is used in this study. Additionally, a BMI cut‐off of 25 kg m−2 for overweight, consistent with US parameters is used. As some participants from Trinidad are Asian, there is the potential of underestimating the number of participants with overweight and obesity because the World Health Organization recommends using a BMI cut‐off of 23 kg m−2 for Asian populations 56. However, given that only four of the participants in the final sample were of Asian descent, it would not be expected to alter the results. Furthermore, this study does not measure the concordance corrected by chance that may have further accounted for any chance associations 51. Lactating women could not be excluded from the sample as this was not a question on the ECS survey; however, given the average age of the cohort study was 55, this was likely a minimal number of participants. Lastly, this study did not address weight misperception in underweight and normal weight individuals who perceive themselves to be overweight. While an important issue, it is not as relevant to the obesity discussion that is the focus of this study.
Despite these limitations, this study has thoroughly evaluated weight misperception among a cohort of adults in the Eastern Caribbean showing that it is common and reduces engagement in weight control behaviour. It shows that while there is no gender difference in weight misperception, the differences in weight control behaviour between men and women signify a continued need for effective means of engaging men in weight loss. The data support the need to provide theoretically grounded health education interventions targeting all socioeconomic strata of society and those with established chronic diseases, to increase the recognition of healthy weight and the contribution of obesity to the development of chronic diseases. The provider community, in particular, must take note of their role in educating patients about the association of their overweight or obese status with NCDs. The strong association of weight perception and engagement in weight control behaviour that is shown in the ECHORN Cohort is evidence that all weight loss and obesity interventions targeting a similar populations should incorporate discussions about weight perception as a critical first step to achieving success.
Conflicts of interest statement
The authors have no conflicts of interest to disclose.
Funding
All authors are supported in part by the following grants from the National Institutes of Health/National Institute on Minority Health and Health Disparities: U24MD006939 and U54MD010711. The work was also supported by Yale CTSA grant number UL1TR000142. Views expressed are those of the authors and do not represent those of the funding sources.
Acknowledgements
We would like to acknowledge ECHORN Cohort Study site staff and participants for their continued dedication to the project and furthering our understanding early predictors and risk factors for non‐communicable diseases among adults in the Eastern Caribbean.
This paper was written on behalf of the ECHORN Writing Group.
Hassan, S. , Ojo, T. , Galusha, D. , Martinez‐Brockman, J. L. , Adams, O. P. , Maharaj, R. , Nazario, C. , Nunez, M. , and Nunez‐Smith, M. (2018) Obesity and weight misperception among adults in the Eastern Caribbean Health Outcomes Research Network (ECHORN) Cohort Study. Obesity Science & Practice, 4: 367–378. 10.1002/osp4.280.
References
- 1. World Health Organization . Fact sheet: obesity and overweight. WHO Publications 2016. Accessed September 5, 2017.
- 2. Calle EE, Rodriguez C, Walker‐Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med 2003; 348: 1625–1638. [DOI] [PubMed] [Google Scholar]
- 3. Hubert HB, Feinleib M, McNamara PM, Castelli WP. Obesity as an independent risk factor for cardiovascular disease: a 26‐year follow‐up of participants in the Framingham Heart Study. Circulation 1983; 67: 968–977. [DOI] [PubMed] [Google Scholar]
- 4. Bastien M, Poirier P, Lemieux I, Despres JP. Overview of epidemiology and contribution of obesity to cardiovascular disease. Prog Cardiovasc Dis 2014; 56: 369–381. [DOI] [PubMed] [Google Scholar]
- 5. David FM. Homeostatic theory of obesity. Health Psychol Open 2015; 2(1): 2055102915590692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ravussin E, Ryan DH. Three new perspectives on the perfect storm: what's behind the obesity epidemic? Obesity 2018; 26: 9–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dorsey RR, Eberhardt MS, Ogden CL. Racial and ethnic differences in weight management behavior by weight perception status. Ethn Dis 2010; 20: 244–250. [PubMed] [Google Scholar]
- 8. Duncan DT, Wolin KY, Scharoun‐Lee M, Ding EL, Warner ET, Bennett GG. Does perception equal reality? Weight misperception in relation to weight‐related attitudes and behaviors among overweight and obese US adults. Int J Behav Nutr Phys Act 2011; 8: 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Murillo R, Ali SA, Carmack C, Doss D. Activity and weight misperception among overweight and obese US adults. Am J Health Behav 2016; 40: 12–20. [DOI] [PubMed] [Google Scholar]
- 10. Haynes A, Kersbergen I, Sutin A, Daly M, Robinson E. A systematic review of the relationship between weight status perceptions and weight loss attempts, strategies, behaviours and outcomes. Obes Rev 2018; 19: 347–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hazzard VM, Hahn SL, Sonneville KR. Weight misperception and disordered weight control behaviors among U.S. high school students with overweight and obesity: associations and trends, 1999–2013. Eat Behav 2017; 26: 189–195. [DOI] [PubMed] [Google Scholar]
- 12. Johnson‐Taylor WL, Fisher RA, Hubbard VS, Starke‐Reed P, Eggers PS. The change in weight perception of weight status among the overweight: comparison of NHANES III (1988–1994) and 1999–2004 NHANES. Int J Behav Nutr Phys Act 2008; 5: 9–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Johnson F, Cooke L, Croker H, Wardle J. Changing perceptions of weight in Great Britain: comparison of two population surveys. BMJ 2008; 337: a494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Powell TM, de Lemos JA, Banks K, et al. Body size misperception: a novel determinant in the obesity epidemic. Arch Intern Med 2010; 170: 1695–1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Moyer VA. Screening for and management of obesity in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2012; 157: 373–378. [DOI] [PubMed] [Google Scholar]
- 16. Leblanc ES, O'Connor E, Whitlock EP, Patnode CD, Kapka T. Effectiveness of primary care‐relevant treatments for obesity in adults: a systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med 2011; 155: 434–447. [DOI] [PubMed] [Google Scholar]
- 17. Knowler WC, Barrett‐Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002; 346: 393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hernan AL, Versace VL, Laatikainen T, Vartiainen E, Janus ED, Dunbar JA. Association of weight misperception with weight loss in a diabetes prevention program. BMC Public Health 2014; 14: 93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dorsey RR, Eberhardt MS, Ogden CL. Racial/ethnic differences in weight perception. Obesity (Silver Spring) 2009; 17: 790–795. [DOI] [PubMed] [Google Scholar]
- 20. Kuchler F, Variyam JN. Mistakes were made: misperception as a barrier to reducing overweight. Int J Obes Relat Metab Disord 2003; 27: 856–861. [DOI] [PubMed] [Google Scholar]
- 21. Chen X, Wang Y. Is ideal body image related to obesity and lifestyle behaviors in African‐American adolescents? Child 2012; 38: 219–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Killion L, Hughes SO, Wendt JC, Pease D, Nicklas TA. Minority mothers' perceptions of children's body size. Int J Pediatr Obes 2006; 1: 96–102. [DOI] [PubMed] [Google Scholar]
- 23. Kronenfeld LW, Reba‐Harreleson L, Von Holle A, Reyes ML, Bulik CM. Ethnic and racial differences in body size perception and satisfaction. Body Image 2010; 7: 131–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Barroso CS, Peters RJ, Johnson RJ, Kelder SH, Jefferson T. Beliefs and perceived norms concerning body image among African‐American and Latino teenagers. J Health Psychol 2010; 15: 858–870. [DOI] [PubMed] [Google Scholar]
- 25. Pan American Health Organization . Economic dimensions of noncommunicable diseases in Latin America and the Caribbean. World Health Organization; 2016.
- 26. Pan American Health Organization . Profile of capacity and response to non‐communicable diseases and their risk factors in the region of the Americas. World Health Organization regional office for the Americas; 2015.
- 27. Pan American Health Organization . Plan of action for the prevention of obesity in children and adolescents. World Health Organization; 2014.
- 28. Caribbean Public Health Agency (CARPHA) . Plan of action for promoting healthy weights in the Caribbean: prevention and control of childhood obesity. CARPHA; 2014.
- 29. Healthy Caribbean Coalition . Preventing childhood obesity in the Caribbean. Healthy Caribbean Coalition; 11 October, 2017.
- 30. National Center for Chronic Disease Prevention and Health Promotion Health equity resource toolkit for state practitioners addressing obesity disparities. 2017.
- 31. Simeon DT, Rattan RD, Panchoo K, Kungeesingh KV, Ali AC, Abdool PS. Body image of adolescents in a multi‐ethnic Caribbean population. Eur J Clin Nutr 2003; 57: 157–162. [DOI] [PubMed] [Google Scholar]
- 32. Adams OP, Lynch‐Prescod JT, Carter AO. Obesity in primary care in Barbados: prevalence and perceptions. Ethn Dis 2006; 16: 384–390. [PubMed] [Google Scholar]
- 33. Centers for Disease Control and Prevention (CDC) . National Health and Nutrition Examination Survey Questionnaire. 2015. Accessed April, 2018.
- 34. World Health Organization . The global physical activity questionnaire analysis guide. Geneva: World Health Organization; 2018.
- 35. Chu AH, Ng SH, Koh D, Muller‐Riemenschneider F. Reliability and validity of the self‐ and interviewer‐administered versions of the Global Physical Activity Questionnaire (GPAQ). PLoS One 2015; 10: e0136944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hwang JH, Ryu DH, Park SW. Interaction effect between weight perception and comorbidities on weight control behavior in overweight and obese adults: is there a sex difference? J Korean Med Sci 2015; 30: 1017–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lemon SC, Rosal MC, Zapka J, Borg A, Andersen V. Contributions of weight perceptions to weight loss attempts: differences by body mass index and gender. Body Image 2009; 6: 90–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Paeratakul S, White MA, Williamson DA, Ryan DH, Bray GA. Sex, race/ethnicity, socioeconomic status, and BMI in relation to self‐perception of overweight. Obes Res 2002; 10: 345–350. [DOI] [PubMed] [Google Scholar]
- 39. Fan M, Jin Y, Khubchandani J. Overweight misperception among adolescents in the United States. J Pediatr Nurs 2014; 29: 536–546. [DOI] [PubMed] [Google Scholar]
- 40. Adams OP, Carter AO. Are primary care practitioners in Barbados following diabetes guidelines? – a chart audit with comparison between public and private care sectors. BMC Res Notes 2011; 4: 199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Adams OP, Carter AO. Are primary care practitioners in Barbados following hypertension guidelines? – a chart audit. BMC Res Notes 2010; 3: 316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Zhao G, Ford ES, Li C, Mokdad AH. Weight control behaviors in overweight/obese U.S. adults with diagnosed hypertension and diabetes. Cardiovasc Diabetol 2009; 8: 13–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Yaemsiri S, Slining MM, Agarwal SK. Perceived weight status, overweight diagnosis, and weight control among US adults: the NHANES 2003–2008 Study. Int J Obes (Lond) 2011; 35: 1063–1070. [DOI] [PubMed] [Google Scholar]
- 44. Winkleby MA, Jatulis DE, Frank E, Fortmann SP. Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health 1992; 82: 816–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Greenlund KJ, Liu K, Dyer AR, Kiefe CI, Burke GL, Yunis C. Body mass index in young adults: associations with parental body size and education in the CARDIA Study. Am J Public Health 1996; 86: 480–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: concepts, methodologies, and guidelines. Annu Rev Public Health 1997; 18: 341–378. [DOI] [PubMed] [Google Scholar]
- 47. Cohen AK, Rai M, Rehkopf DH, Abrams B. Educational attainment and obesity: a systematic review. Obes Rev 2013; 14: 989–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Roskam AJ, Kunst AE, van Oyen H, et al. Comparative appraisal of educational inequalities in overweight and obesity among adults in 19 European countries. Int J Epidemiol 2010; 39: 392–404. [DOI] [PubMed] [Google Scholar]
- 49. Kinge JM, Strand BH, Vollset SE, Skirbekk V. Educational inequalities in obesity and gross domestic product: evidence from 70 countries. J Epidemiol Community Health 2015; 69: 1141–1146. [DOI] [PubMed] [Google Scholar]
- 50. Dinsa GD, Goryakin Y, Fumagalli E, Obesity SM. socioeconomic status in developing countries: a systematic review. Obes Rev 2012; 13: 1067–1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet (London, England) 2012; 380: 247–257. [DOI] [PubMed] [Google Scholar]
- 52. Janssen I, Katzmarzyk PT, Ross R. Waist circumference and not body mass index explains obesity‐related health risk. Am J Clin Nutr 2004; 79: 379–384. [DOI] [PubMed] [Google Scholar]
- 53. Okosun IS. Ethnic differences in the risk of type 2 diabetes attributable to differences in abdominal adiposity in American women. J Cardiovasc Risk 2000; 7: 425–430. [DOI] [PubMed] [Google Scholar]
- 54. Okosun IS, Boltri JM, Anochie LK, Chandra KM. Racial/ethnic differences in prehypertension in American adults: population and relative attributable risks of abdominal obesity. J Hum Hypertens 2004; 18: 849–855. [DOI] [PubMed] [Google Scholar]
- 55. Hassan S, Galusha, D. , Martinez‐Brockman, J.L. , Adams, P. , Maharaj, R. , Nazario, C. , Nunez, M. , Nunez‐Smith, M . Association of body mass index and waist‐to‐hip ratio with diabetes in Eastern Caribbean adults. Abstract: Obesity Society Conference, Washington D. C, Oct. 30–Nov. 1 2017. 2017.
- 56. World Health Organization Expert Consultation . Appropriate body‐mass index for Asian populations and its implications for policy and intervention strategies. Lancet (London, England) 2004; 363: 157–163. [DOI] [PubMed] [Google Scholar]


