Abstract
Objectives
Verinurad (RDEA3170) is a high-affinity inhibitor of the URAT1 transporter in clinical development for treating gout and asymptomatic hyperuricaemia. The aim of this Phase 2a, randomized, open-label study was to investigate the multiple-dose pharmacodynamics, pharmacokinetics and safety of oral verinurad combined with febuxostat vs febuxostat alone and verinurad alone.
Methods
Japanese male subjects aged 21–65 years with gout (n = 37) or asymptomatic hyperuricaemia (n = 35) and serum urate (sUA) ⩾8 mg/dl were randomized to febuxostat (10, 20, 40 mg) in combination with verinurad (2.5–10 mg), verinurad alone (2.5–15 mg), febuxostat alone (10, 20, 40 mg) or benzbromarone alone (50 mg). There were four treatment periods per cohort and each treatment period was 7 days. Study drugs were administered once-daily after breakfast. Plasma, serum and urine samples were measured at pre-set intervals on days –1, 7, 14, 21 and 28.
Results
Verinurad combined with febuxostat decreased sUA in dose-dependent manner, providing greater sUA lowering than febuxostat alone at the same dose (P < 0.001). Urinary uric acid excretion rate was increased by verinurad, reduced by febuxostat and comparable to baseline for verinurad combined with febuxostat. Verinurad from 2.5 mg to 15 mg was well tolerated, with no withdrawals due to adverse events. Laboratory assessments showed no clinically meaningful changes during combination treatment.
Conclusion
Verinurad combined with febuxostat decreased sUA dose-dependently while maintaining uric acid excretion similar to baseline. All dose combinations of verinurad and febuxostat were generally well tolerated. These data support continued investigation of oral verinurad in patients with gout.
Trial registration
ClinicalTrials.gov, https://clinicaltrials.gov, NCT02317861
Keywords: verinurad, febuxostat, pharmacokinetics, pharmacodynamics, serum urate, hyperuricemia, gout
Rheumatology key messages
Verinurad is in clinical development for the treatment of gout and asymptomatic hyperuricaemia.
Verinurad combined with febuxostat decreased serum urate dose-dependently in subjects with gout or asymptomatic hyperuricaemia.
Verinurad and febuxostat dose combinations were generally well tolerated in subjects with gout or hyperuricaemia.
Introduction
Gout is an inflammatory arthritis characterized by the deposition of monosodium urate crystals in the joints, tendons and other connective tissues, secondary to long-standing hyperuricaemia [1–3]. Hyperuricaemia itself is typically undetected until the symptoms of gout or its commonly associated comorbidities—including cardiovascular disease, chronic kidney disease and metabolic syndrome—are diagnosed [2, 4–6]. Successful management of gout requires a sustained reduction in the concentration of serum urate (sUA) below a target of <6.0 mg/dl, or <5.0 mg/dl in patients with severe gout symptoms, which leads over time to the dissolution of crystals, the alleviation of gout symptoms [7–9] and improved outcomes from cardiovascular, renal and other comorbidities [5].
To achieve a sustained reduction in sUA, most patients require long-term urate-lowering therapy (ULT) [3]. Currently available ULTs include the xanthine oxidase inhibitors (XOIs) allopurinol and febuxostat, which reduce the production of urate, and the uricosurics probenecid, benzbromarone, sulfinpyrazone and lesinurad, which increase the excretion of sUA by inhibiting its reabsorption [3]. Many patients fail to achieve their target sUA using an XOI as monotherapy [10, 11]. For these patients, management guidelines recommend combining ULTs with complementary mechanisms of action, such as an XOI with a uricosuric [9, 12, 13]. Japanese guidelines, in addition to providing guidance on the treatment of gout, offer recommendations on managing asymptomatic hyperuricaemia, on the basis that reducing sUA in these subjects can prevent the onset of gout [13]. The inclusion of a uricosuric in combination treatment represents a rational approach to managing this population, as inefficient renal excretion of uric acid contributes to elevated sUA in 85% of Japanese subjects with hyperuricaemia [14, 15].
The uricosuric lesinurad was recently approved in the USA and European Union in combination with an XOI for treating hyperuricaemia associated with gout in subjects not achieving target sUA with an XOI alone [16–18]. In the phase 3 clinical development programme, treatment with lesinurad 200 and 400 mg, in combination with febuxostat, resulted in more patients achieving target sUA and experiencing reduction in overall tophus area compared with febuxostat alone [17]. This treatment combination, however, showed only trends towards reductions in gout flares at 12 months at the highest dose tested (400 mg) [17], a dose that had increased renal adverse effects (compared with lesinurad 200 mg with febuxostat or febuxostat alone) and was neither submitted to, nor approved by, US and European regulatory agencies.
The clinical trial experience with ULTs has demonstrated that more precipitous and increasingly lowered sUA below target levels may lead to improved outcomes (e.g. lower gout flare incidence, more rapid tophus area reduction) [19–23].
Verinurad, a next-generation URAT1 inhibitor, demonstrates high potency in inhibiting URAT1 [24]. Verinurad doses as low as 2.5 mg produce significant sUA lowering in humans [25, 26], and this greater reduction in sUA may lead to improved outcomes and medical benefits for patients with gout. Verinurad in monotherapy studies has been associated with increased urinary uric acid concentrations and low rates of serum creatinine (sCr) elevation [25, 26]. Verinurad co-administered with an XOI has produced no cases of sCr elevation, which may be explained by the known inhibitory effects of XOIs on urate production [27–29]. The combination of verinurad with an XOI therefore has the potential to lower sUA to a greater extent than by XOIs alone, while reducing incidences of renal uric acid crystallization and sCr elevation.
This study evaluated the multiple-dose pharmacodynamics (PD), pharmacokinetics (PK) and safety of oral verinurad in combination with febuxostat compared with febuxostat alone or verinurad alone in Japanese male adults with gout or asymptomatic hyperuricaemia (RDEA3170-205, NCT02317861). Febuxostat doses (10, 20 or 40 mg) were selected based on the initial recommended dose and most commonly prescribed maintenance doses in Japan. Benzbromarone (50 mg) was investigated as a reference URAT1 inhibitor [30].
Methods
Study design and subjects
Japanese male subjects with gout or hyperuricaemia and a screening sUA ⩾8 mg/dl participated in this phase 2a, randomized, open-label, single-centre study. All subjects were aged 21–65 years with body weight ⩾50 kg and BMI 18–40 kg/m2. Gout was diagnosed by the treating physician from the subject’s history and available laboratory data.
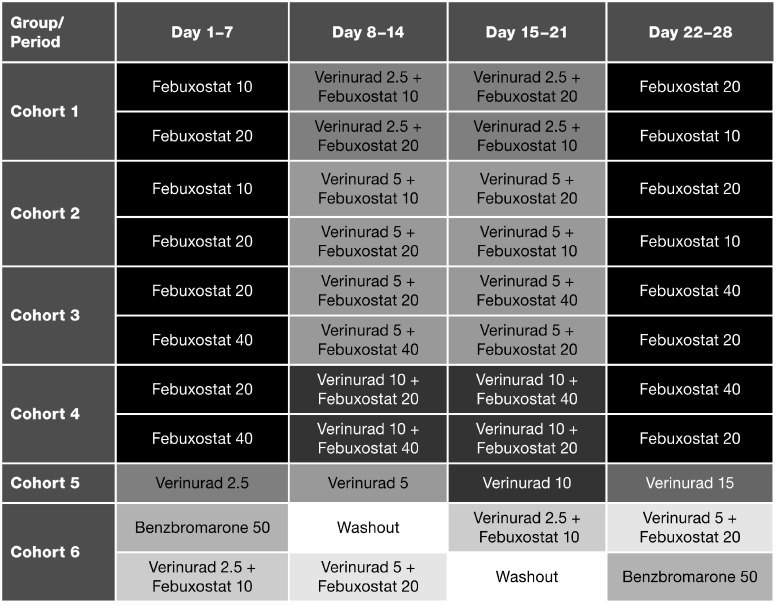
Six cohorts of subjects were randomized into treatment sequences to receive febuxostat (10, 20 or 40 mg) in combination with verinurad (dose range 2.5–10 mg), febuxostat alone (10, 20 or 40 mg), verinurad alone (dose range 2.5–15 mg) or benzbromarone alone (50 mg) (Fig. 1). There were four 7-day treatment periods per cohort and no washout periods between treatments, with the exception of cohort 6 (see Fig. 1). All study drugs were administered orally once daily in the morning after breakfast.
Fig. 1.
Study design
Doses are in milligrams.
The study was conducted in accordance with ethical principles that have their origin in the Declaration of Helsinki and are consistent with the International Conference on Harmonisation/Good Clinical Practice and the Japanese Good Clinical Practice for Trials on Drugs (The Ministry of Health, Labour and Welfare Ordinance No. 28, 27 March 1997), partially revised by the Ministry of Health, Labour and Welfare Ordinance and their related notifications. The protocol, study and consent form were approved by an independent institutional review board (SOUSEIKAI Hakata Clinic). All subjects provided informed consent to participate in the study.
Blood and urine sampling
Serial plasma, serum and urine samples (total catch) were measured at frequent pre-set intervals on days –1, 7, 14, 21 and 28 for PD and PK assessments. On urine collection days, subjects were requested to drink 240 ml of water immediately after they rose in the morning (within 2 h pre-dose) in order to maintain urine output.
Analytical methods
Verinurad concentrations in plasma and urine and febuxostat concentrations in plasma were measured by Ardea Biosciences, Inc. (San Diego, CA, USA). Plasma samples were extracted by protein precipitation and analytes quantified by high-performance liquid chromatography– tandem mass spectrometry [31, 32]. Urine samples were prepared by dilution with water and quantified by high-performance liquid chromatography–tandem mass spectrometry. Detail on quantitative determination of benzbromarone and performance of the assays is provided in supplementary data, section ‘Assay methodology’, available at Rheumatology online.
Endpoints and determinations
All subjects who received at least one dose of verinurad, febuxostat or benzbromarone and had evaluable PD data made up the PD population; all who received at least one dose of verinurad or febuxostat and had evaluable PK data made up the PK population; and all who received at least one dose of verinurad, febuxostat or benzbromarone constituted the safety population.
PD assessments included maximum percentage change and mean percentage change in sUA concentration from baseline on days 7, 14, 21 and 28; proportions of subjects with sUA ⩽6.0 mg/dl at 4 h post-dose; rate of urinary uric acid excretion [ReUR (mg/h)]; and fractional excretion of uric acid for each 24-h collection period [FEUA (%)]. For PD analyses, a mixed-effects model was used on Emax with treatment as a fixed effect, baseline concentration as a covariate and subject as a random effect separately for each cohort. Least squares means were calculated for each treatment group and the differences between treatment groups, together with 95% CI. Statistical testing of mean changes in sUA was conducted at an α level of 0.05; the tests are included for descriptive purposes only, given this is an early phase study. No adjustments were made for multiple comparisons. PD analyses were performed using SAS version 9.3 (SAS Institute Inc., Cary, NC, USA).
PK assessments for verinurad and febuxostat included area under the plasma concentration–time curve from time zero to 24 h post-dose (AUC0–24), maximum observed plasma concentration (Cmax), time to maximum observed plasma concentration (Tmax) and plasma terminal half-life (t½). The amount of verinurad excreted in urine over 24 h (Ae0–24), percentage of unchanged verinurad in urine (fe0–24) and renal clearance of verinurad (CLR0–24) were also assessed. For PK analyses, a mixed-effects model was used to assess the impact of verinurad or febuxostat on AUC, Cmax, Ae0–24 and CLR0–24 of the verinurad–febuxostat combination, with treatment as a fixed effect and subject as a random effect. Geometric mean squares (95% CI) are presented for verinurad alone or in combination with febuxostat 10, 20 or 40 mg, and for febuxostat alone or in combination with verinurad 2.5, 5 or 10 mg, together with geometric least squares mean ratios (90% CI). PK analyses were conducted by Ardea Biosciences, Inc., using Phoenix WinNonlin version 6.3 (Certara, Princeton, NJ, USA).
Subjects were monitored for safety throughout the study and at follow-up (day 42). Safety assessments included adverse events (AEs) coded according to the Medical Dictionary for Regulatory Activities (version 18.0), clinical laboratory evaluations, vital signs, electrocardiograms and physical examinations. Any renal serious events were to be reviewed by an independent adjudication committee. Any haematology, chemistry or urinalysis abnormalities considered clinically relevant were to be assigned a severity rating by the investigator, based on Rheumatology Common Toxicity Criteria version 2.0 2007 [33]. Safety data are summarized by descriptive statistics using SAS version 9.3.
Results
Subjects
Seventy-two subjects with gout (n = 37) or asymptomatic hyperuricaemia (n = 35) were randomized to treatment sequences in each of the six cohorts. There were two treatment sequences for each cohort with six subjects in each treatment sequence. All subjects completed the study per protocol.
Demographic and other baseline characteristics of subjects grouped by cohort are summarized in Table 1. All subjects were males aged 21–65 years. Mean age, weight and BMI were similar between the cohorts. The mean screening sUA ranged from 8.53 to 9.17 mg/dl across the cohorts.
Table 1.
Demographic and other baseline characteristics
| Cohort 1 | Cohort 2 | Cohort 3 | Cohort 4 | Cohort 5 | Cohort 6 | |
|---|---|---|---|---|---|---|
| (n = 12) | (n = 12) | (n = 12) | (n = 12) | (n = 12) | (n = 12) | |
| Age, mean (s.d.), years | 41.1 (10.6) | 44.7 (16.2) | 44.2 (8.2) | 43.2 (9.8) | 48.1 (12.8) | 44.4 (13.8) |
| Body weight, mean (s.d.), kg | 82.27 (14.14) | 78.48 (16.84) | 74.16 (8.62) | 78.47 (11.8) | 78.96 (10.94) | 73.83 (6.05) |
| BMI, mean (s.d.), kg/m2 | 28.1 (4.5) | 27.5 (5.3) | 24.9 (2.5) | 27.1 (4.2) | 27.4 (3.4) | 25.2 (2.6) |
| Gout, n (%) | 5 (41.7) | 6 (50.0) | 6 (50.0) | 7 (58.3) | 6 (50.0) | 7 (58.3) |
| Asymptomatic hyperuricaemia, n (%) | 7 (58.3) | 6 (50.0) | 6 (50.0) | 5 (41.7) | 6 (50.0) | 5 (41.7) |
| sUA, screening, mean (s.d.), mg/dl | 9.17 (1.09) | 8.56 (0.60) | 8.53 (0.74) | 8.99 (0.95) | 8.57 (0.61) | 8.86 (0.85) |
| eGFR, mean (s.d.), ml/min | 119 (19.7) | 120 (32.2) | 113 (19.7) | 106 (23.8) | 105 (24.0) | 107 (22.2) |
eGFR= [(140 − age) × ideal body weight (kg)]/[72 × serum creatinine (mg/dl)]. eGFR: estimated glomerular filtration rate based on serum creatinine, age and ideal body weight; sUA: serum urate.
Pharmacodynamics
sUA
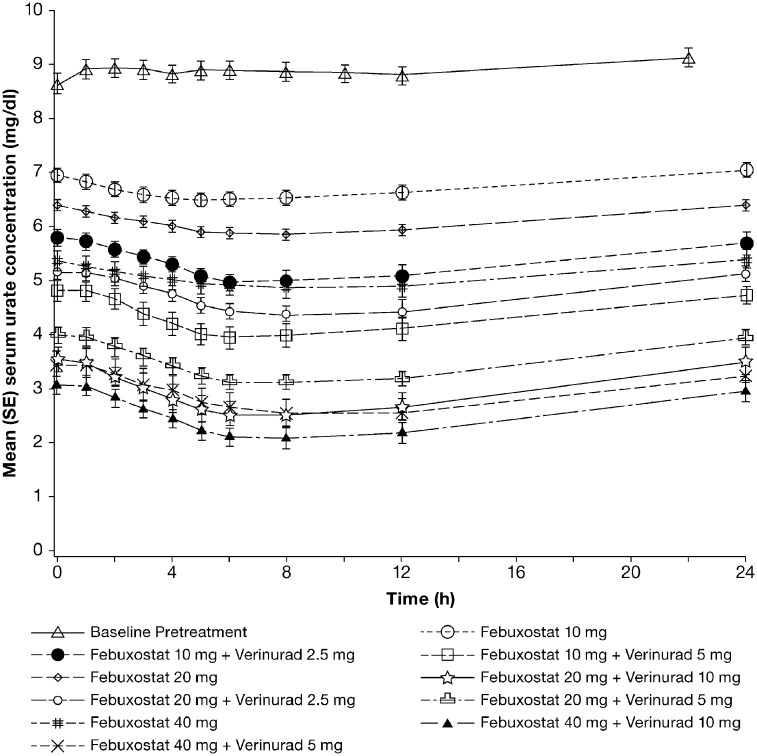
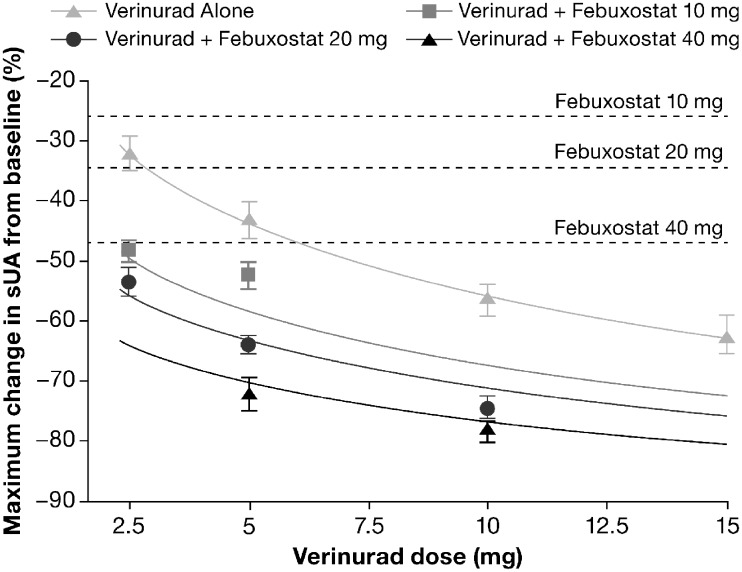
The time courses of mean sUA levels for febuxostat alone and for verinurad combined with febuxostat are shown in Fig. 2, demonstrating a downward trend in sUA for up to 12 h with each treatment. Both the mean changes in sUA (Fig. 2) and the maximum percentage changes in sUA (Fig. 3) were dose-dependent, and were greater for verinurad combined with febuxostat than for febuxostat alone. Percentage changes in sUA from baseline to 4 h post-dose are shown in supplementary Table S1, available at Rheumatology online, for the treatments in each cohort. All reductions in sUA from baseline to 4 h post-dose were significantly greater for verinurad combined with febuxostat than for febuxostat alone at the same dose or at the next higher febuxostat dose in each cohort (P < 0.001). Benzbromarone 50 mg was generally similar in sUA-lowering effect to verinurad 5 mg combined with febuxostat 20 mg (supplementary Fig. S1, available at Rheumatology online).
Fig. 2.
Mean (s.e.) serum urate concentrations (mg/dl): febuxostat alone or combined with verinurad
Pharmacodynamic analysis set, pooled cohort data.
Fig. 3.
Mean (s.e.) Maximum percentage change in sUA: verinurad, febuxostat or verinurad combined with febuxostat
Solid lines are predictive trend lines based on additive changes from febuxostat and verinurad at various doses. Dashed horizontal lines represent the maximum change in sUA from baseline with febuxostat alone. Pharmacodynamic analysis set, pooled cohort data. sUA: serum urate.
The proportions of subjects with sUA ⩽6.0 mg/dl at 4 h post-dose are shown in supplementary Table S2, available at Rheumatology online. All subjects achieved sUA ⩽6.0 mg/dl 4 h after treatment with verinurad 10 or 15 mg alone, benzbromarone 50 mg alone or verinurad in combination with febuxostat (with one exception in the verinurad 2.5 mg and febuxostat 10 mg group). At 4 h after treatment with febuxostat 10, 20 or 40 mg alone, sUA was ⩽6.0 mg/dl in 20.8, 50.1 and 83.3%, respectively (pooled cohorts).
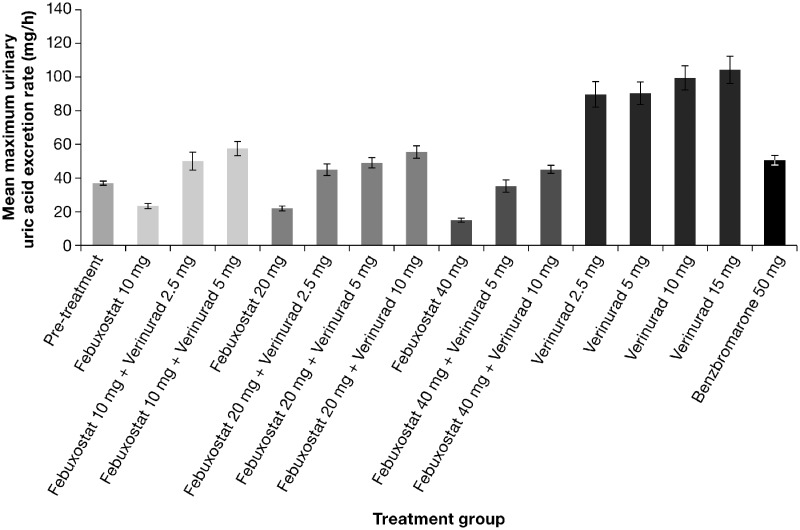
Urinary uric acid
Mean maximum ReUR was increased by verinurad alone and reduced by febuxostat alone in a dose-dependent manner relative to baseline. For verinurad combined with febuxostat, the mean maximum ReUR was similar to baseline and lower than or comparable to benzbromarone (Fig. 4).
Fig. 4.
Mean (s.e.) maximum urinary uric acid excretion rate (mg/h): verinurad, febuxostat or verinurad combined with febuxostat
Pharmacodynamic analysis set.
FEUA was increased in a dose-dependent manner by verinurad alone and reduced by febuxostat alone relative to baseline. For verinurad combined with febuxostat, FEUA was increased but to a lesser extent than for verinurad alone at the same dose (data not shown).
Pharmacokinetics
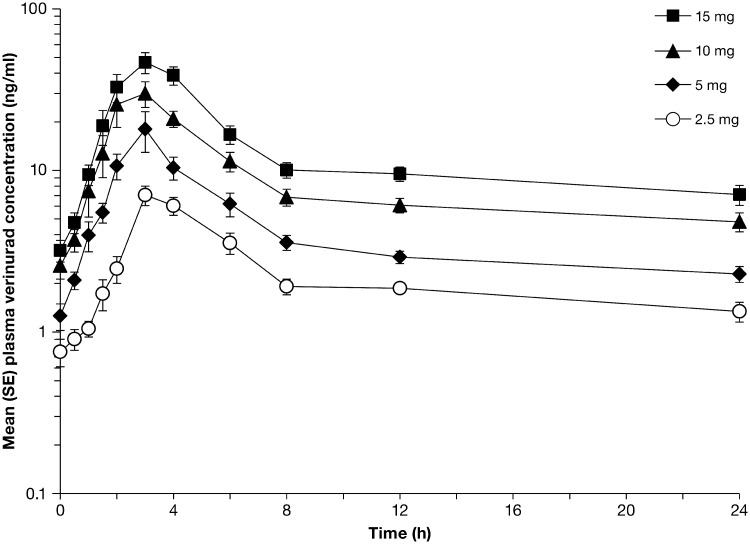
Median Tmax of verinurad ranged from 3 to 4 h and mean t½ from 13 to 24 h for varying verinurad doses alone or in combination with febuxostat (supplementary Table S3, available at Rheumatology online). The Cmax and AUC0–24 of verinurad alone or in combination with febuxostat exhibited dose-related increases in the dose range investigated (Fig. 5 and supplementary Table S3, available at Rheumatology online). Plasma exposures of verinurad were generally comparable in the absence or presence of febuxostat, with geometric mean ratios ranging from 86.6 to 122% for Cmax and 99.8 to 109% for AUC0–24 with varying doses of febuxostat. Similarly, plasma exposures of febuxostat were not consistently affected by varying doses of verinurad (supplementary Table S4, available at Rheumatology online).
Fig. 5.
Mean (s.e.) plasma concentrations of verinurad (ng/ml) following multiple once-daily oral administration of verinurad alone
Pharmacokinetic analysis set.
The Ae0–24 of verinurad increased with increasing verinurad doses and febuxostat had no consistent effect (supplementary Table S3, available at Rheumatology online). fe0–24 was <2%. The CLR0–24 of verinurad ranged from 12.4 to 15.1 ml/min with verinurad alone and showed minimal change in the presence of febuxostat (data not shown).
Safety
Five subjects reported six treatment-emergent AEs (TEAEs) during treatment or follow-up (supplementary Table S5, available at Rheumatology online). The majority of TEAEs (n = 5) were mild or moderate in severity and there were no serious AEs or withdrawals due to AEs during the study. Incidences of TEAEs were consistently low across the cohorts.
There were no clinically meaningful changes in clinical laboratory evaluations or vital signs in any cohort. Two subjects treated with verinurad 2.5 mg or verinurad 15 mg alone (cohort 5) showed a sCr elevation ⩾1.5 × baseline. In one of these subjects, sCr increased from 0.72 mg/dl at baseline to 1.12 mg/dl on day 2, and decreased to 0.91 mg/dl on day 8 and 0.76 mg/dl at follow-up. The second subject had a baseline sCr of 0.85 mg/dl that increased to 1.34 mg/dl on day 22 and decreased to 1.07 mg/dl at follow-up. There were no cases of sCr elevation in subjects treated with verinurad combined with febuxostat.
Discussion
Verinurad is a potent, selective inhibitor of the URAT1 transporter under clinical development to meet the current unmet needs in the chronic treatment of gout and asymptomatic hyperuricaemia. In this phase 2a, randomized, open-label study of 72 adult Japanese subjects with gout or hyperuricaemia, verinurad (dose range 2.5–10 mg) in combination with febuxostat (10, 20 or 40 mg) reduced sUA in a dose-dependent manner. Verinurad combined with febuxostat provided significantly greater decreases in sUA compared with febuxostat alone at the same dose or at the higher febuxostat dose in each cohort. It is of note also that the proportion of subjects achieving sUA ⩽6.0 mg/dl at 4 h post-dose was 91.7% at the lowest dose of verinurad (2.5 mg) combined with febuxostat (10 mg), compared with 83.3% for febuxostat 40 mg alone. These observations suggest that combining two treatments with different mechanisms of action can reduce sUA levels more consistently and lead to higher target achievement rates than a single agent alone at higher doses. Two other phase 2a studies investigating verinurad in combination with febuxostat or allopurinol, which were performed in Caucasian subjects with gout, also reported superior sUA lowering for the combination versus XOI treatment alone [27, 28].
To fully characterize the rate of urinary uric acid excretion after verinurad treatment, urine samples were collected as frequently as hourly. We hypothesized that the peak rate of uric acid excretion may be a risk factor for development of acute urate nephropathy, while the 24-h elevation of uric acid excretion may be a risk factor for development of nephrolithiasis; nephrolithiasis is most likely to occur at night or in the early morning due to the low volume and relatively acidic pH of urine [34]. Consistent with the mechanism of action of verinurad via inhibition of URAT1, urinary uric acid excretion was increased by verinurad alone relative to baseline. Combining verinurad with febuxostat produced uric acid excretion levels similar to baseline and lower than or comparable to benzbromarone, a reference URAT1 inhibitor that has not been associated with acute urate nephropathy. The risk of uric acid crystallization, manifesting as acute urate nephropathy or nephrolithiasis, may therefore be lessened by combining verinurad with febuxostat. There were no cases of sCr elevation in our study during combination treatment.
Verinurad plasma Cmax and AUC exposures exhibited dose-proportional increases under steady-state conditions within the dose range investigated. Febuxostat did not affect the PK of verinurad, or vice versa, suggesting a lack of drug–drug interaction.
All dose combinations of verinurad and febuxostat were generally well tolerated, with no withdrawals due to AEs or serious AEs during study. Verinurad in combination with febuxostat was also associated with no clinical laboratory or vital sign abnormalities, consistent with an earlier drug–drug interaction study performed in volunteers [33].
Limitations of the study are its short study duration and the inclusion of only male subjects with gout. Strengths of the study include the investigation of subjects with gout or asymptomatic hyperuricaemia to provide clinical relevance, and the frequent blood and urine samplings that enhance the reliability of the PD and PK analyses. The frequent urine sampling in particular allowed detailed assessment of urinary uric acid excretion over time, which may be used to identify the dose combinations of verinurad and febuxostat that mitigate the risk of urinary over-excretion of uric acid.
In conclusion, the combination of verinurad with febuxostat in the dose ranges studied resulted in greater and more consistent sUA lowering than achieved by febuxostat alone in subjects with gout or asymptomatic hyperuricaemia. All dose combinations of verinurad and febuxostat were generally safe and well tolerated. These data in Japanese subjects support the continued development of verinurad with an XOI as a novel dual-mechanism approach to treating patients with gout or asymptomatic hyperuricaemia.
Supplementary Material
Acknowledgements
Editorial support for this manuscript was provided by Bill Wolvey of PAREXEL, which was funded by AstraZeneca.
Funding: This study was funded by Ardea Biosciences/AstraZeneca.
Disclosure statement: M.G. is an employee of and owns stock in AstraZeneca, which sponsored this study. S.L., ZS, XY, AY, and JH are former employees of Ardea Biosciences, Inc., a member of the AstraZeneca group. J.H. is a shareholder in AstraZeneca. Y.I. was a consultant to AstraZeneca K.K., Osaka, Japan. The other author has no conflicts of interest.
References
- 1. Bardin T, Richette P.. Definition of hyperuricemia and gouty conditions. Curr Opin Rheumatol 2014;26:186–91. [DOI] [PubMed] [Google Scholar]
- 2. Perez-Ruiz F, Dalbeth N, Bardin T.. A review of uric acid, crystal deposition disease, and gout. Adv Ther 2015;32:31–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rees F, Hui M, Doherty M.. Optimizing current treatment of gout. Nat Rev Rheumatol 2014;10:271–83. [DOI] [PubMed] [Google Scholar]
- 4. Grassi D, Ferri L, Desideri G. et al. Chronic hyperuricemia, uric acid deposit and cardiovascular risk. Curr Pharm Des 2013;19:2432–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Richette P, Perez-Ruiz F, Doherty M. et al. Improving cardiovascular and renal outcomes in gout: what should we target? Nat Rev Rheumatol 2014;10:654–61. [DOI] [PubMed] [Google Scholar]
- 6. Soltani Z, Rasheed K, Kapusta DR, Reisin E.. Potential role of uric acid in metabolic syndrome, hypertension, kidney injury, and cardiovascular diseases: is it time for reappraisal? Curr Hypertens Rep 2013;15:175–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Doherty M, Jansen TL, Nuki G. et al. Gout: why is this curable disease so seldom cured? Ann Rheum Dis 2012;71:1765–70. [DOI] [PubMed] [Google Scholar]
- 8. Khanna PP, Nuki G, Bardin T. et al. Tophi and frequent gout flares are associated with impairments to quality of life, productivity, and increased healthcare resource use: results from a cross-sectional survey. Health Qual Life Outcomes 2012;10:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Richette P, Doherty M, Pascual E. et al. 2016 updated EULAR evidence-based recommendations for the management of gout. Ann Rheum Dis 2017;76:29–42. [DOI] [PubMed] [Google Scholar]
- 10. Becker MA, Fitz-Patrick D, Choi HK. et al. An open-label, 6-month study of allopurinol safety in gout: the LASSO study. Semin Arthritis Rheum 2015;45:174–83. [DOI] [PubMed] [Google Scholar]
- 11. Singh JA, Akhras KS, Shiozawa A.. Comparative effectiveness of urate lowering with febuxostat versus allopurinol in gout: analyses from large U.S. managed care cohort. Arthritis Res Ther 2015;17:120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Khanna D, Fitzgerald JD, Khanna PP. et al. 2012 American College of Rheumatology guidelines for management of gout. Part 1: systematic nonpharmacologic and pharmacologic therapeutic approaches to hyperuricemia. Arthritis Care Res 2012;64:1431–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Yamanaka H. Japanese guideline for the management of hyperuricemia and gout: second edition. Nucleosides Nucleotides Nucleic Acids 2011;30:1018–29. [DOI] [PubMed] [Google Scholar]
- 14. Burns CM, Wortmann RL.. Latest evidence on gout management: what the clinician needs to know. Ther Adv Chronic Dis 2012;3:271–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Nakamura T. Guideline for the Management of Hyperuricemia and Gout. Osaka: Medical Review, 2003. [Google Scholar]
- 16. Bardin T, Keenan RT, Khanna PP. et al. Lesinurad in combination with allopurinol: a randomised, double-blind, placebo-controlled study in patients with gout with inadequate response to standard of care (the multinational CLEAR 2 study). Ann Rheum Dis 2017;76:811–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dalbeth N, Jones G, Terkeltaub R. et al. Lesinurad, a selective uric acid reabsorption inhibitor, in combination with febuxostat in patients with tophaceous gout: a phase III clinical trial. Arthritis Rheumatol 2017;69:1903–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Saag KG, Fitz-Patrick D, Kopicko J. et al. Lesinurad combined with allopurinol: a randomized, double-blind, placebo-controlled study in gout patients with an inadequate response to standard-of-care allopurinol (a US-based study). Arthritis Rheumatol 2017;69:203–12. [DOI] [PubMed] [Google Scholar]
- 19. Pascual E, Andres M, Vela P.. Gout treatment: should we aim for rapid crystal dissolution? Ann Rheum Dis 2013;72:635–7. [DOI] [PubMed] [Google Scholar]
- 20. Perez-Ruiz F, Calabozo M, Pijoan JI, Herrero-Beites AM, Ruibal A.. Effect of urate-lowering therapy on the velocity of size reduction of tophi in chronic gout. Arthritis Rheum 2002;47:356–60. [DOI] [PubMed] [Google Scholar]
- 21. Perez-Ruiz F. Treating to target: a strategy to cure gout. Rheumatology 2009;48(Suppl 2):ii9–ii14. [DOI] [PubMed] [Google Scholar]
- 22. Shiozawa A, Buysman EK, Korrer S.. Serum uric acid levels and the risk of flares among gout patients in a US managed care setting. Curr Med Res Opin 2017;33:117–24. [DOI] [PubMed] [Google Scholar]
- 23. Terkeltaub R, Perez-Ruiz F, Kopicko J. et al. The safety and efficacy of lower serum urate levels: a pooled analysis of gout subjects receiving lesinurad and xanthine oxidase inhibitors [abstract]. Arthritis Rheumatol 2015;67(Suppl 10):Abstract 2354. http://acrabstracts.org/abstract/the-safety-and-efficacy-of-lower-serum-urate-levels-a-pooled-analysis-of-gout-subjects-receiving-lesinurad-and-xanthine-oxidase-inhibitors/ (22 December 2017, date last accessed). [Google Scholar]
- 24. Tan PK, Liu S, Gunic E, Miner JN.. Discovery and characterization of verinurad, a potent and specific inhibitor of URAT1 for the treatment of hyperuricemia and gout. Sci Rep 2017;7:665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shen Z, Gillen M, Miner JN. et al. Pharmacokinetics, pharmacodynamics, and tolerability of verinurad, a selective uric acid reabsorption inhibitor, in healthy adult male subjects. Drug Des Devel Ther 2017;11:2077–2086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hall J, Gillen M, Liu S. et al. Pharmacokinetics, pharmacodynamics, and tolerability of verinurad, a selective uric acid reabsorption inhibitor, in healthy Japanese and non-Asian male subjects. Drug Des Devel Ther 2018;12:1799–807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Fleischmann R, Winkle P, Miner JN. et al. Pharmacodynamic and pharmacokinetic effects and safety of verinurad in combination with allopurinol in adults with gout: a phase IIa, open-label study. RMD Open 2018;4(1):e000584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Fleischmann R, Winkle P, Hall J. et al. Pharmacodynamic and pharmacokinetic effects and safety of verinurad in combination with febuxostat in adults with gout: a phase IIa, open-label study. RMD Open 2018;4(1):e000647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Goldfarb DS, MacDonald PA, Hunt B, Gunawardhana L.. Febuxostat in gout: serum urate response in uric acid overproducers and underexcretors. J Rheumatol 2011;38:1385–9. [DOI] [PubMed] [Google Scholar]
- 30. Shin HJ, Takeda M, Enomoto A. et al. Interactions of urate transporter URAT1 in human kidney with uricosuric drugs. Nephrology 2011;16:156–62. [DOI] [PubMed] [Google Scholar]
- 31. Kankam M, Gillen M, Hall J. et al. Pharmacokinetics, Pharmacodynamics, and Tolerability of Concomitant Administration of Verinurad (RDEA3170) and Allopurinol in Male Subjects With Gout. J Clin Pharmacol 2018; in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hall J, Gillen M, Yang X, Shen Z.. Pharmacokinetics, Pharmacodynamics, and Tolerability of Concomitant Administration of Verinurad and Febuxostat in Healthy Male Volunteers. J Clin Pharmcol 2018; in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Woodworth T, Furst DE, Alten R. et al. Standardizing assessment and reporting of adverse effects in rheumatology clinical trials II: the Rheumatology Common Toxicity Criteria v.2.0. J Rheumatol 2007;34:1401–14. [PubMed] [Google Scholar]
- 34. Wiederkehr MR, Moe OW.. Uric acid nephrolithiasis: a systemic metabolic disorder. Clin Rev Bone Miner Metab 2011;9:207–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.