Abstract
Background:
Considering that better understanding of the underlying mechanisms and risk factors of arterial ischemic stroke (AIS) would be helpful for better management of stroke and its outcome in children as well as preventing or reducing the occurrence of its related potential disabilities, the aim of this study was to investigate the most common risk factors and causes of AIS in patients referred to the referral hospitals in Tehran and Isfahan cities of Iran.
Methods:
In this study, medical files of all pediatric patients admitted to the Mofid and Imam Hossein children's hospitals with the diagnosis of AIS from 2001 to 2011 and 2011 to 2016, respectively, were evaluated. Identified risk factors of AIS were categorized as arteriopathies, cardiac disorders (CDs), infection, acute head-and-neck disorders, acute systemic conditions, chronic systemic conditions, prothrombotic states, chronic head-and-neck disorders, atherosclerosis-related RFs, and others.
Results:
In this study, 61 patients were evaluated. Mean (standard deviation) age of the patients was 5.1 (3.9) years. About 62.3% of the patients were boys while 37.7% were girls (P < 0.01). A total of 36 patients (59%) had at least one risk factor for AIS. About 40.9% of patients had undetermined risk factors. CDs (21.31%) and vascular disease (21.31%) were the most common risk factors of AIS in the studied children. Nearly 11.5% of the patients had moyamoya vascular disease (MMD).
Conclusion:
The findings of our study indicated that the most common risk factors for AIS in the two studied regions are congenital heart and vascular diseases. The results of the current study could be used for planning more preventive strategies in patients suffering from the mentioned diseases. In addition, the obtained data could be used for conducting targeted education and management of high-risk patients.
Keywords: Arterial ischemic stroke, congenital heart disease, risk factor, vascular disease
Introduction
Arterial ischemic stroke (AIS) in children is a rare but important disorder with a higher rate of morbidity and mortality. It is considered as the cause of the top 10 long-term mortality in the pediatric population.[1,2] Two-third of affected patients suffer from adverse outcomes including long-term cognitive, behavioral, and functional deficits. Furthermore, it is associated with higher cost and socioeconomic burdens.[3]
Reported incidence rate for AIS is between 2 and 13 in 100,000 children per year.[4] Risk factors, clinical presentations, and AIS outcome in children are distinct from those in adults. It is a heterogeneous disorder with different causes and risk factors. Nonatherosclerotic factors such as congenital or acquired cardiac disease, large vessel arteriopathies, and prothrombotic abnormalities are the main pathogenesis of AIS in children. Infection, hematologic disorders and coagulopathies, medications, iron deficiency, metabolic disorders, trauma, and migraine are other less common causes of AIS in children.[5,6,7]
In spite of increased awareness of pediatric AIS, the etiology of the disease is not completely understood and its diagnostic and therapeutic procedures are still underdeveloped. It is well established that identification of the multiple etiologies of childhood AIS may lead to better diagnosis, management as well as its prevention.[8]
Several studies from different ethnic and geographical regions have investigated the preexisting risk factors of AIS in children. According to their results, the identified risk factors were not similar in different age, ethnic, and geographical regions. Evidence indicated that most of the studies were established in Western and European countries with few studies from Asian countries.[9,10,11] It is well established that the identification of AIS risk factors in each region is an important issue which could be used for better management, improvement of its prognosis, and prevention of its related complications. A regional study indicated that 70% of children with AIS suffered from neurological disabilities.[12]
Considering that better understanding of the underlying mechanisms and risk factors of AIS would be helpful for the improvement of rational management of stroke and its outcome in children as well as preventing or reducing the occurrence of its related potential disabilities, the aim of this study was to investigate the most common risk factors and causes of AIS in patients referred to referral hospitals in Tehran and Isfahan cities, Iran. The priority of this research is determined by the fact that the features of AIS risk factors in different ethnic and geographical regions are not similar.
Methods
In this retrospective and prospective study, the medical files of all pediatric patients admitted to the Mofid Children's Hospital in Tehran, from 2001 to 2011 retrospectively and in Imam Hossein Children's Hospital in Isfahan, prospectively from 2011 to 2016 with the diagnosis of AIS were evaluated. Both of the hospitals are Tertiary Pediatric Care Hospitals in Isfahan and Tehran.
Acute AIS is defined as an acute focal neurological deficit with the evidence of cerebral infarction in an arterial distribution on brain imaging.
Records of patients of ages 0–18 years with AIS which confirmed by brain magnetic resonance imaging (MRI) were included. Data of patients who did not undergo imaging to confirm the diagnosis of the disease, neonates and children with subdural or epidural hematomas due to head trauma as well as those with missing data in their files were excluded from the study. For all patients, brain MRI, MR angiography or conventional brain angiography, evaluation for hypercoagulable state, echocardiography, electrocardiography, lipid profile, serum homocysteine, lupus anticoagulant, and anti-cardiolipin antibodies were performed.
Risk factors and defined conditions thought to be associated with childhood AIS were divided into 10 categories including arteriopathies, cardiac disorders (CDs), infection, acute head-and-neck disorders, acute systemic conditions, chronic systemic conditions, prothrombotic states, chronic head-and-neck disorders, atherosclerosis-related RFs, and others.
The protocol of the study was approved by the Pediatrics Review Board members and Ethical Committee of Isfahan and Tehran Universities of Medical Sciences.
Data of the selected patients were retrieved from their medical files and recorded in a questionnaire.
Data regarding the demographic characteristics of the patients, laboratory findings, radiological results, and risk factors were also recorded in the questionnaire.
Statistical analysis
Recorded data were analyzed using SPSS ver. 20 software (SPSS Inc., Chicago, Illinois, USA).
Results
During the study period, 72 patients (49 from Tehran and 23 from Isfahan) were admitted to the referral hospitals with a definitive diagnosis of AIS. From the selected cases, 11 patients were excluded due to missing and incomplete data. The age of studied patients ranged from 5 months to 13 years. Mean (standard deviation) age of the patients was 5.1% (3.9). About 62.3% (38/61) of the patients were boys while 37.7% were girls (P < 0.01).
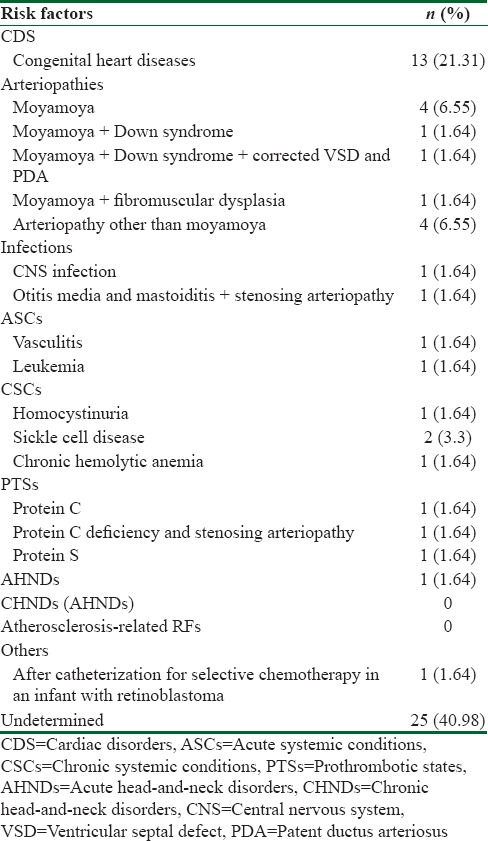
The distribution of different identified risk factors in the studied children with AIS is presented in Table 1. A total of 36 patients (59%) had at least one risk factor for AIS. Nearly 40.9% of patients had undetermined risk factors. CDs (21.31%) and vascular disease (21.31%) were the most common risk factors of AIS in the studied children. About 11.5% of the patients had moyamoya vascular disease (MMD) vascular disease.
Table 1.
Distribution of different identified risk factors in the studied children with arterial ischemic stroke
Brain MRI showed stroke in the territory of the middle cerebral artery in 56 patients, posterior cerebral artery in two patients, and anterior cerebral artery in three patients.
Discussion
In this study, we reported AIS risk factors among children who referred to the two referral pediatrics hospitals in Tehran and Isfahan. Our findings indicated that among the pediatrics population, the most common cause of AIS was congenital heart disease and vascular disease.
As mentioned, understanding the risk factors of AIS in each population would be useful for practicing physicians to determine high-risk population for AIS which would consequently result in proper management of the disease as well as its prevention.
Although there have been many studies in this field from different countries and populations, there is no published data on the risk factors of pediatric AIS among the Iranian population.
In this study, AIS occurred most frequently among boys than in girls. Our findings were similar to those reported by many studies in this field.[13,14,15] Several studies indicated that male children are at greater risk for AIS. Evidence indicated that higher susceptibility of male children to AIS is regardless of their age, type of stroke, or history of trauma.[13,14,15,16] However, the cause of male predominance is not determined yet.
The results of previous studies in this field demonstrated that only half of the AIS pediatric cases have an identified risk factor, and in a great number of the cases, undetermined risk factors were reported.[17] In this study, 40.1% of cases were classified as having undetermined risk factors.
Our findings in this field are similar to studies conducted in Turkey and USA.[18,19]
Different studies from various regions have reported different features for the risk factors of childhood AIS. In a narrative review study, Lyle et al. reported that the most common risk factors of AIS are congenital heart disease, sickle cell disease, arterial dissection, and MMD.[9]
In another review study, Lo et al. showed that the most common identified risk factors of AIS in hospitalized children are congenital heart disease and infections such as sepsis and meningitis/encephalitis.[10]
In the International Pediatric Stroke Study which was a multi-center, international observational cohort study, 676 children with AIS were evaluated and the risk factors of the disease were determined. According to their findings, 31% had CDs, 24% had infections, 13% had prothrombotic disorders, and 6% had sickle cell disease.[11] In another population-based case–control study, the Kaiser Pediatric Stroke Study, the risk factors of AIS were investigated in Northern California. Their results indicated that CDs, infection, prothrombotic disorders, and sickle cell disease were the risk factors for 10, 40, 0, and 2% of AIS cases, respectively.[20] In the Great Ormond Street Hospital series, the most common risk factors were infections (37%), sickle cell disease (17%), and CDs (12%), respectively.[21]
Two different studies from Turkey have shown that infections and CDs, mainly its congenital forms, were the most common risk factors for AIS.[18,22]
Jeong et al. in their study in Korea reported the risk factors of AIS in children as follows: arteriopathy (MMD), cardiac disease, prothrombotic condition, and hematologic disease, respectively.[23]
In a study in Taiwan, Lee et al. evaluated the risk factors of childhood AIS. The most common risk factors were vascular disease and infections.[24]
The literature review demonstrated that childhood AIS is associated with different risk factors in the different population. Cardiac diseases are the main risk factor of AIS in China, North America, and Hong Kong.[10,15,20] Vascular disease including MMD, coagulation disorders, and infections are the main risk factor of pediatrics AIS in Japanese, European, and Asian children.[18,22,25] Sickle cell disease was the most common risk factor in African – American children.[26]
In our study, the most common risk factors were congenital heart disease and vascular diseases, mainly MMD. Infection was not a common cause of AIS in our studied population.
Our findings could be implacable for health-care professionals to develop facilities to manage vascular and CDs in children properly and timely and improve the medical care of patients with the mentioned disease.
The limitations of this study were its retrospective design in more than half of the patients, small sample size, and evaluation of hospital-based population. However, using population-based studies provide more detailed information about the patients and risk factors of AIS. It is suggested that planning prospective studies would also reduce the rate of undetermined cases.
The strength of the current study was that for the first time the risk factors of AIS among pediatric population in two large cities in Iran were determined. The results of this study would be used as baseline data as well as pilot study for the future nationwide studies.
Conclusions
The findings of our study indicated that the most common risk factors of AIS in the two studied regions are congenital heart disease and vascular disease. The results of the current study could be used for planning more preventive strategies in patients suffering from the mentioned diseases. In addition, obtained data could be used for conducting targeted education and management of high-risk patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Friedman N. Pediatric stroke: Past, present and future. Adv Pediatr. 2009;56:271–99. doi: 10.1016/j.yapd.2009.08.003. [DOI] [PubMed] [Google Scholar]
- 2.National Vital Statistics System, National Center for Health Statistics, Centers for Disease Control and Prevention (CDC). 10 Leading Causes of Death by Age Group, United States-2012. CDC. [Last accessed on 2015 Jan 23]. Available from: http://www.cdc.gov/injury/wisqars/pdf/leading_causes_of_death_by_age_group_2012-a.pdf .
- 3.Gardner MA, Hills NK, Sidney S, Johnston SC, Fullerton HJ. The 5-year direct medical cost of neonatal and childhood stroke in a population-based cohort. Neurology. 2010;74:372–8. doi: 10.1212/WNL.0b013e3181cbcd48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roach ES, Golomb MR, Adams R, Biller J, Daniels S, Deveber G, et al. Management of stroke in infants and children: A scientific statement from a Special Writing Group of the American Heart Association Stroke Council and the Council on Cardiovascular Disease in the Young. Stroke. 2008;39:2644–91. doi: 10.1161/STROKEAHA.108.189696. [DOI] [PubMed] [Google Scholar]
- 5.Bernard TJ, Goldenberg NA. Pediatric arterial ischemic stroke. Hematol Oncol Clin North Am. 2010;24:167–80. doi: 10.1016/j.hoc.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 6.Steinlin M. A clinical approach to arterial ischemic childhood stroke: Increasing knowledge over the last decade. Neuropediatrics. 2012;43:1–9. doi: 10.1055/s-0032-1307449. [DOI] [PubMed] [Google Scholar]
- 7.Jordan LC, Hillis AE. Challenges in the diagnosis and treatment of pediatric stroke. Nat Rev Neurol. 2011;7:199–208. doi: 10.1038/nrneurol.2011.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosa M, De Lucia S, Rinaldi VE, Le Gal J, Desmarest M, Veropalumbo C, et al. Paediatric arterial ischemic stroke: Acute management, recent advances and remaining issues. Ital J Pediatr. 2015;41:95. doi: 10.1186/s13052-015-0174-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lyle CA, Bernard TJ, Goldenberg NA. Childhood arterial ischemic stroke: A review of etiologies, antithrombotic treatments, prognostic factors, and priorities for future research. Semin Thromb Hemost. 2011;37:786–93. doi: 10.1055/s-0031-1297169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lo W, Stephens J, Fernandez S. Pediatric stroke in the United States and the impact of risk factors. J Child Neurol. 2009;24:194–203. doi: 10.1177/0883073808322665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mackay MT, Wiznitzer M, Benedict SL, Lee KJ, Deveber GA, Ganesan V, et al. Arterial ischemic stroke risk factors: The international pediatric stroke study. Ann Neurol. 2011;69:130–40. doi: 10.1002/ana.22224. [DOI] [PubMed] [Google Scholar]
- 12.Nasiri J, Ariyana A, Yaghini O, Ghazavi MR, Keikhah M, Salari M, et al. Neurological outcome after arterial ischemic stroke in children. Adv Biomed Res. 2016;5:107. doi: 10.4103/2277-9175.183668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fullerton HJ, Wu YW, Zhao S, Johnston SC. Risk of stroke in children: Ethnic and gender disparities. Neurology. 2003;61:189–94. doi: 10.1212/01.wnl.0000078894.79866.95. [DOI] [PubMed] [Google Scholar]
- 14.Salih MA, Abdel-Gader AG, Al-Jarallah AA, Kentab AY, Alorainy IA, Hassan HH, et al. Stroke in saudi children. Epidemiology, clinical features and risk factors. Saudi Med J. 2006;27(Suppl 1):S12–20. [PubMed] [Google Scholar]
- 15.Chung B, Wong V. Pediatric stroke among Hong Kong Chinese subjects. Pediatrics. 2004;114:e206–12. doi: 10.1542/peds.114.2.e206. [DOI] [PubMed] [Google Scholar]
- 16.Golomb MR, Fullerton HJ, Nowak-Gottl U, Deveber G, International Pediatric Stroke Study Group Male predominance in childhood ischemic stroke: Findings from the international pediatric stroke study. Stroke. 2009;40:52–7. doi: 10.1161/STROKEAHA.108.521203. [DOI] [PubMed] [Google Scholar]
- 17.Ganesan V, Kirkham F. London: Mac Keith Press; 2011. Stroke and Cerebrovascular Disease in Childhood. [Google Scholar]
- 18.Per H, Unal E, Poyrazoglu HG, Ozdemir MA, Donmez H, Gumus H, et al. Childhood stroke: Results of 130 children from a reference center in central Anatolia, Turkey. Pediatr Neurol. 2014;50:595–600. doi: 10.1016/j.pediatrneurol.2013.12.023. [DOI] [PubMed] [Google Scholar]
- 19.Pergami P, Thayapararajah SW, Seemaladinne N. West Virginia university pediatric stroke registry: Clinical description and risk factors identification in patients from a rural area. Clin Pediatr (Phila) 2015;54:40–6. doi: 10.1177/0009922814543324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hills NK, Johnston SC, Sidney S, Zielinski BA, Fullerton HJ. Recent trauma and acute infection as risk factors for childhood arterial ischemic stroke. Ann Neurol. 2012;72:850–8. doi: 10.1002/ana.23688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ganesan V, Prengler M, McShane MA, Wade AM, Kirkham FJ. Investigation of risk factors in children with arterial ischemic stroke. Ann Neurol. 2003;53:167–73. doi: 10.1002/ana.10423. [DOI] [PubMed] [Google Scholar]
- 22.Incecik F, Hergüner MO, Altunbasak S. Risk factors and treatment outcomes for children with arterial ischemic stroke. J Clin Neurosci. 2010;17:1000–2. doi: 10.1016/j.jocn.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 23.Jeong G, Lim BC, Chae JH. Pediatric stroke. J Korean Neurosurg Soc. 2015;57:396–400. doi: 10.3340/jkns.2015.57.6.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee YY, Lin KL, Wang HS, Chou ML, Hung PC, Hsieh MY, et al. Risk factors and outcomes of childhood ischemic stroke in Taiwan. Brain Dev. 2008;30:14–9. doi: 10.1016/j.braindev.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 25.Lynch JK, Han CJ. Pediatric stroke: What do we know and what do we need to know? Semin Neurol. 2005;25:410–23. doi: 10.1055/s-2005-923535. [DOI] [PubMed] [Google Scholar]
- 26.Baker C, Grant AM, George MG, Grosse SD, Adamkiewicz TV. Contribution of sickle cell disease to the pediatric stroke burden among hospital discharges of African-Americans-United States, 1997-2012. Pediatr Blood Cancer. 2015;62:2076–81. doi: 10.1002/pbc.25655. [DOI] [PMC free article] [PubMed] [Google Scholar]


