Abstract
Background
Fornier gangrene is an extremely rare disease of the genitals. This disease is a result of the urogenital tract, anorectal area, and genital skin infections, appearing usually in immunocompromised patients with diabetes, obesity, and malignant neoplasms. The basic treatment of Fournier gangrene includes an emergency surgical intervention combined with antibiotic therapy and detoxification.
Methods
A review of recent papers comprising studies and reviews published in 2005–2016 was performed. The clinical cases were studied at the Department of Purulent Surgery Central Clinical Hospital No. 1, where 7 patients were diagnosed and treated.
Results
The etiology, pathogenesis, clinical and laboratory presentation, diagnosis, treatment, and prognosis of Fournier gangrene are described in this article. The authors have described several clinical cases of patients with Fournier gangrene and with necrotic cellulitis and fasciomyositis of anterior abdominal wall, which is a manifestation of Fournier gangrene. Making allowance for the unfavorable epidemiological situation of syphilis in Russia, the increase in the incidence of complicated, atypical chancre, and therefore, the need for differentiation of Fournier gangrene with such manifestations of syphilis as necrotizing, esthiomenous chancre, indurative edema, the appropriate clinical examples are well explained in this article.
Keywords: Fournier gangrene, Necrotising fasciitis, Differential diagnosis, Treatment, Prognosis
Introduction
Despite the relative rarity, Fournier gangrene was and remains a formidable disease with severe complications and a high level of mortality.
Fournier gangrene is a specific form of necrotizing fasciitis, localized on the external genital organs, as well as in the perianal region, accompanied by thrombosis of the feeding arteries, leading to gangrene of the skin and subcutaneous tissue, with manifestations of severe intoxication and multiple organ failure [1].
Despite the rarity of this disease, unfavorable prognosis related to this disease depends much on the timing of medical care. The treatment delay is accompanied by a high lethality, reaching 90%, due to the development of septic shock and its associated complications [2].
Search Methods
This article contains the literature research and clinical cases studied at the clinic of surgery department of the Ural State Medical University. The literature research was performed using such databases as MEDLINE in Pubmed and eLibrary. The MeSH terms used to search were “Fournier gangrene” and “necrotising fasciitis” during December 2016. The articles in English and Russian were chosen and reviewed description. Also, the methods of differential diagnosis and therapy of treating Fournier's gangrene were studied in recent papers.
In the Department of Purulent Surgery Central Clinical Hospital No. 1, Ekaterinburg, from 2007 to 2016 years, 7 men with Fournier's Gangrene were treated. Patients entered a severe condition in the period from 3 to 5 days after the onset of the disease. All the patients gave their informed consent to participate in the research. The study was approved by a local Ethical Committee of the Ural State Medical University (protocol #2 from February 16, 2018).
All cases presented with fever; in the blood tests of patients marked leukocytosis with a shift to young forms. Patients under general anesthesia were treated using the following treatment methods: autopsy, drainage of foci of necrosis with wide incisions in the region of the penis, scrotum, perineum, inguinal region, lateral surfaces of the abdominal wall and necrectomy, with stage necrectomy being performed according to indications.
Patients received the initial treatment with cephalosporins of the third generation with preparations of the nitroimidazole group, then taking into account the data of the culture method of investigation, determination of sensitivity to antibacterial drugs.
All patients later underwent autodermoplasty or overlapping of secondary seams. The early postoperative period proceeded without complications.
Epidemiological Situation
The disease bears the name of the famous French venereologist - Jean Alfred Fournier. In 1883, the scientist made a report on the case of gangrene on a young man's genitals. His lecture on this subject became widely known. J.A. Fournier considered genital trauma to be one of the factors predisposing to the disease and described the gangrene that arose due to ligation of the genitals with the aim of preventing night enuresis or with the purpose of contraception [2].
Fournier gangrene is an extremely rare disease that occurs in 1.6 cases per 100,000 men per year, amounting to 0.02–0.09% of total admissions to the surgical hospital. The average age of patients is 50.9 years and the ratio of men to women is 10: 1 [3]. Seasonal fluctuations are not characteristic for the incidence of Fournier gangrene; endemic regions are not described.
The authors note that the cause of Fournier's gangrene can be established in 95% of cases; the disease usually occurs because of infectious processes of the urogenital tract, anorectal area, or skin of the genitals. Fournier gangrene develops commonly in immunocompromised patients with diabetes, obesity, and malignant neoplasms. Kincius et al. [4] who conducted a study among patients with Fournier's gangrene found a high proportion of people with diabetes mellitus. The cause of Fournier gangrene was polymicrobial association, with Proteus Mirabilis being the most predominant bacterium. Taken et al. [5] described the case of 65 patients with Fournier gangrene in 8 years of follow-up. The authors also note that the most frequent concomitant pathology was diabetes mellitus; the cause of the development of swelling was a perianal abscess. Yoshino et al. [6] described the case of an anal fistula in a patient with type 2 diabetes mellitus, resulting in an abscess of pararectal tissue complicated by Fournier gangrene. Mosayebi et al. [7] described Fournier gangrene in a newborn with acute myeloid leukemia. Ishida et al. [8] led a clinical case of the occurrence of Fournier gangrene in a patient who received chemotherapy for colon cancer. The patient took bevacizumab for 6 courses, against which the intestinal perforation developed, complicated by the Fournier gangrene [8]. Sheehy et al. [9] described the rare case of acute pancreatitis as the cause of Fournier gangrene. Wanis et al. [10] observed Fournier gangrene in a young immunocompetent patient due to late diagnosed perforated appendicitis. Obi [11] cited cases of patients with isolated Fournier gangrene of the penis. In addition to the idiopathic Fournier gangrene, the author states that the trauma of the penis resulting from oral sex and the infection of the urogenital tract are among the causes for disease progression [11].
Pathogenesis
Bacteremia is considered a starting link in the mechanism of the development of necrosis of the fascia that initiates the cytokine cascade leading to the damage of the endothelium, which in turn activates by means of thromboplastin, a coagulation cascade with inhibition of fibrinolysis and the formation of disseminated microthrombosis of vessels feeding the fascia. In addition, damage to the endothelium leads to extravasation of the liquid part of the blood, swelling of tissues, leukocyte infiltration, all leading to the ischemic necrosis of the fascia [2].
Fournier's disease proceeds clinically with marked symptoms of intoxication. Local manifestations include ulceration in the balanus, prepuce, skin of the penis, or scrotum. Within a few hours, the genitalia hyperemia increases and tissue necrosis occurs. Urination becomes painful and difficult. The disease lasts from 5 to 8 days [2]. Symptomatology is characterised by common necrosis of the skin, subcutaneous tissue, muscles, accompanied by the development of sepsis, multi-organ failure, leading to death. The diagnosis can be established untimely due to a number of reasons, including obesity of the patient, concealing the patient's complaints of pain in the genitals.
The favorable prognosis is related to the end of the process of tissue rejection, reparative phenomena are observed, after which scars form on the site of the torn tissues, leading to the deformation of the genital organs.
In the laboratory examination, a general leukocytosis, or leukopenia, the appearance of young forms, the toxic granularity of neutrophils, anemia, and lymphopenia are observed in the general blood test. Park et al. [12], in an analysis of factors related to mortality from necrotizing soft tissue infections, found that patients with a high body mass index or abnormal leukocyte, C-reactive protein and platelet counts reflecting the severity of the infectious process or impaired renal function have an unfavorable outcome.
Doluoğlu et al. [13] in the study of the outcomes of 39 patients with Fournier gangrene found that an unfavorable prognosis was significantly more frequent in patients with elevated urea levels, low albumin, and hematocrit. Sen et al. [14] indicate the need to determine glycated hemoglobin in order to predict the outcome of the disease, since patients with a high level of this indicator in the study had a significantly more often adverse outcome.
A semi-quantitative method for assessing the risk of developing a necrotic infection (Laboratory Risk Indicator for Necrotizing Fasciitis - LRINEC) based on the evaluation of 6 laboratory parameters, including the number of leukocytes and values of hemoglobin, sodium, glucose, serum creatinine, and C-reactive protein. As a threshold value for the development of Fournier gangrene, a score of 6 was recorded. Kincius et al. [4] showed that in patients with a favorable outcome of the disease, the median LRINEC was 5 compared to 10 in patients with a lethal outcome.
Diagnosis
The methods that are used in the diagnosis of Fournier gangrene are radiography, ultrasound, computed tomography, and magnetic resonance imaging.
When radiographing the affected area, gas can be detected in the depth of soft tissues, which is an absolute indication for surgical intervention, as well as a foreign body that promotes the onset of the disease. To search for gas and liquid in deep, inaccessible for palpation tissues, ultrasound is used, which also helps to assess blood flow and testicular status. It should be noted that unlike most of the urological diseases, the testicles are not affected by Fournier gangrene, which is due to the autonomy of their blood supply and independent of the blood supply of the scrotum and penis [2].
Histological examination reveals necrosis of superficial and deep fascia, fibrinoid coagulation in the lumen of vessels, polymorphic cell infiltration of tissues, and necrotic detritus. Pathognomonic is the thrombosis of vessels that feed tissues of a given localization. However, with significant pathomorphological changes in deep tissues, the skin remains intact for a long time.
Treatment
Patients with Fournier gangrene are subject to emergency hospitalization in a surgical hospital. The prognosis of the disease is serious and the lethality reaches 90%. Sorensen et al. [15] found a lower mortality rate for patients with Fournier gangrene in specialized medical institutions due to more rational treatment and care. In a retrospective cohort study, Jerraya et al. [16] revealed the following prognostic factors of unfavorable prognosis of Fournier gangrene: tissue damage beyond the perineum, severe sepsis and/or septic shock, pulse over 90 per min, leukocytes more than 20 × 109/L, and urea level equal to 7 mmol/L.
The basis of therapy for Fournier gangrene is an emergency surgical intervention in combination with antibacterial and detoxification therapy.
Taking into account the polymicrobial (aerobic and anaerobic) causative microflora, the drugs of choice for antibacterial therapy of Fournier gangrene are considered II–III generation cephalosporins with antibiocics of the group of nitroimidazole, fluoroquinolones, aminoglycosides. In severe forms of the disease, antibiotics from the class of carbapenems are included in the complex processes of the antibacterial therapy [1].
Reconstructive surgical treatment is performed after the formation of granulation tissue; it includes skin plasty by local tissues, split autodermoplasty, muscle plastic, stem plastic, and combined methods. In all cases, rehabilitation treatment and reconstructive interventions are required.
Yoshino et al. [17] described the clinical case of Fournier gangrene in a patient with rectal cancer in which a transferostomy was established, and a necrotomy of perineal and perianal tissue was performed. Fifty days later, the patient underwent radical total pelvic exenteration with sacral resection. Restoration of soft tissue defect was carried out using the rectus muscle, gluteus muscle, and the femoral muscle. Postoperative complications were not recorded and the patient was discharged. Researchers note that the combination of these diseases is extremely rare and treatment in such cases is more complex [17].
Izadi et al. [18] indicate that when the scrotal is affected less than 50%, the defect can be restored by a displaced graft. Immersion of the testicles in the medial femoral tissue pocket is less effective, since it can lead to necrosis of the spermatic cord. Splintered skin flaps can be used if the vaginalis of the testis is not affected. This operation leads to a good aesthetic result, as when using a flap on the leg. With deeper defects, in the absence of the vaginal lining of the testicles, muscle flaps are used, including the rectus abdominis muscle, or local skin-fascial flaps, such as an anterior medial flap of the hip and an anterolateral flap of the thigh. The authors note that early surgical treatment, together with the use of a broad spectrum of antibiotics, is necessary for the successful fight against this disease. The type of reconstructive surgery will depend on the area and depth of the granulating wounds [18].
Clinical Observation
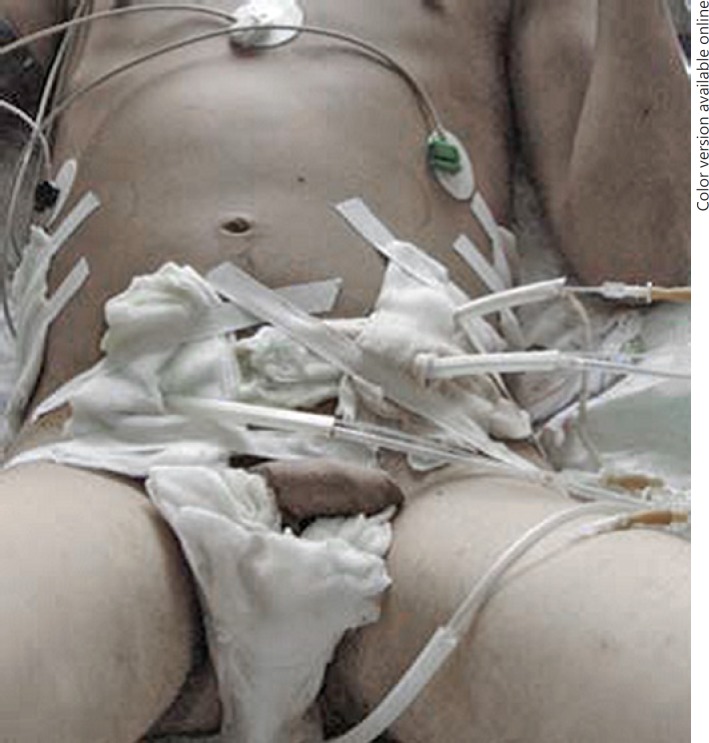
Patient K. applied for medical care to Central Hospital No. 1 with complaints of pain and redness in the region of the genitals and a rise in body temperature of up to 38°C. From the anamnesis it was known that K. considered himself sick the fifth day, when after a trauma of the penis, weakness and fever with chills appeared, followed by reddening in the scrotum and perineum. Before admission to the hospital he received no treatment. On the fifth day, due to the persistence of high temperature, the ambulance brigade admitted him to the Central Clinical Hospital No. 1. Initially, the phlegmon of the penis was diagnosed; it was opened and drained. The high temperature was subsequently contained, the hyperemia and edema spread to the inguinal areas, and the operation was performed on the second day. The following procedures were done: excision of necrosis, opening of purulent foci, drainage of previously opened spaces, and sanitation with antiseptics (Fig. 1). The total lesion area was 6% of the body surface. Antibiotic therapy was carried out and the patient's condition stabilized. After 23 days, secondary surgical treatment was performed - wound plasty was performed with local tissues (Fig. 2). The patient was discharged in a satisfactory condition on day 38 after the onset of the disease.
Fig. 1.
A Fournier gangrene patient after opening and draining the foci of the scrotum, penis, abdominal wall, hips, perianal area.
Fig. 2.
The patient after the Fournier gangrene. Plasticity of the scrotum, penis, perineum with a free perforated skin flap from the thigh.
Gangrene Fournier is also treated precisely as a special case of necrotizing fasciitis, which combines various purulent necrotic processes in localization, but with common pathogenetic mechanisms of development, the leading role in which belongs to fascia lesions and the spread of infection along fascial spaces.
The following clinical case clearly demonstrates the clinical and anamnestic features of necrotizing fasciitis, of which gangrene Fournier is a particular manifestation, in comparison with other infections of soft tissues. The rapid spread of the pathological process in the depths of tissues along the fascia, the lag of the external changes of the skin over the focus, and the absence of significant subjective sensations as a result of the destruction of the superficial nerves in the subcutaneous tissue lead to an underestimation of the severity of the process. Patients are late in seeking medical help. Necrotizing fasciitis is characterized by a sudden acute development of systemic intoxication and bacterial (septic) shock.
Patient T. 56 years old, entered the intensive care unit of City Clinical Hospital No. 40 with the diagnosis “Erysipelatous inflammation of the anterior abdominal wall. Obesity of the second degree. Necrotic cellulite?” (Fig. 3). At hospitalization the following were observed: leukocytes 40 × 109 and a stab-shift 28%. Fatal outcome 2 h after hospitalization. The final diagnosis was as follows: “Necrotizing cellulite, necrotizing fasciomyositis of anterior abdominal wall, unspecified etiology. Septic shock.” From anamnesis: a week ago, after returning from the garden site, noted the appearance of itching in the crease in the lower abdomen “at the site of the bite of the midges?” Soon, a slight soreness appeared on the spot of the comb, the skin of the abdomen did not examine. Family members did not notice changes in the general condition of the patient. A week later, the symptoms of acute intoxication developed (the patient was at work). The patient was taken to the emergency department by an ambulance.
Fig. 3.
Necrotic cellulite, necrotic fasciomyositis of the anterior abdominal wall of a 56-year-old man.
Differential Diagnosis
Differential diagnosis in the early stages of Fournier gangrene should be performed with gangrenous balanitis in diabetics, and among women with gangrenous diabetic vulvitis, ulcerative and gangrenous forms of inguinal lymphogranulomatosis, soft chancre, and acute ulcers of the genitals.
Given the clinical features of syphilis at the present time, the growth of cases of complicated, atypical solid chancres, it becomes necessary to differentiate such manifestations of syphilis such as necrotic, phagadenic chancre, inducible edema, and ectimoid syphilidae with Fournier gangrene [19, 20].
With necrotic chancroid, necrosis initially has a localization of the solid chancre. The phagadenic chancre is characterized by the spread of the necrotic process beyond the chancre, both in the periphery and in the depth. Tissue destruction may lead to bleeding. The abundance of secondary microflora does not help in detecting Treponema pallidum. Serological reactions are crucial to successful diagnosis (Fig. 4).
Fig. 4.
Complicated hard chancre is phagadenism.
Indurative edema, which is an atypical solid chancre, can cause diagnostic errors with the choice of a surgical method of treatment. Indurative edema is a dense edema leading to a significant increase in the volume of the tissue site in areas with a richly developed lymphatic network, imitating an abscess clinic. Characteristic localizations in men are the preputial sack and scrotum; in women localizations are in the large and small labia. The absence of acute inflammatory phenomena, insignificant subjective sensations, prolonged course without the dynamics of the clinic (several months), and regional sclerodenitis lead one to suspect primary syphilis (Fig. 5).
Fig. 5.
Primary syphilis. The combination of ulcerative chancre with atypical chancre is an inductive swelling of the large and minor labia on the left.
One of the factors contributing to the development of Fournier gangrene is genito-urinary infection. Sexually transmitted infections are now characterized by polymicrobial associations, including bacterial-viral, which leads to malignancy [19].
Conclusions
With regard to the development and treatment of Fournier gangrene, the doctor treating outpatients should be able to differentiate manifestations of venereal diseases from the initial stages of Fournier gangrene in order to prevent the development of this traumatic disease.
The outcome of the disease depends on the adequate treatment tactics followed by the doctor.
Disclosure Statement
The work was carried out in accordance with the plan of scientific research of the Ural State Medical University. There are no conflicts of interests and no funding sources to declare.
References
- 1.Aliev SA, Rafiev SF, Rafiev FS, Aliev ES. Furnier's disease in surgeon practice. Surdery J n.a. N.I.Pirogov. 2008;11:58–63. [PubMed] [Google Scholar]
- 2.Ephimenko NA, Privolnee VV. Furnier's gangrene. Clin Microbiol Antimicrob Chemother. 2008;10:25–34. [Google Scholar]
- 3.Prohorov AV. Furnier's gangrene. Kazan Med J. 2016;97:256–261. [Google Scholar]
- 4.Kincius M, Telksnys T, Trumbeckas D, Jievaltas M, Milonas D. Evaluation of LRINEC scale feasibility for predicting outcomes of Fournier gangrene. Surg Infect (Larchmt) 2016;17:448–453. doi: 10.1089/sur.2015.076. [DOI] [PubMed] [Google Scholar]
- 5.Taken K, Oncu MR, Ergun M, Eryilmaz R, Demir CY, Demir M, et al. Fournier's gangrene: Causes, presentation and survival of sixty-five patients. Pak J Med Sci. 2016;32:746–750. doi: 10.12669/pjms.323.9798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yoshino Y, Funahashi K, Okada R, Miura Y, Suzuki T, Koda T, et al. Severe Fournier's gangrene in a patient with rectal cancer: case report and literature review. World J Surg Oncol. 2016;14:34. doi: 10.1186/s12957-016-0989-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mosayebi Z, Omidian A, Movahedian AH, Kompani F, Hosseininodeh SS. Fournier's gangrene in a neonate with acute myeloid leukemia: a case report. Iran J Pediatr. 2016;26:e4537. doi: 10.5812/ijp.4537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ishida T, Shinozaki H, Ozawa H, Kobayashi T, Kato S, Wakabayashi T, et al. A Case of Fournier's gangrene Caused by Small Intestinal Perforation during Bevacizumab Combination Chemotherapy. Gan To Kagaku Ryoho. 2016;43:909–911. [PubMed] [Google Scholar]
- 9.Sheehy SA, Kelly ME, Francis EC, Sweeney KJ, Hussey A. A rare case of Fournier's gangrene. J Surg Case Rep. 2016;5:1–3. doi: 10.1093/jscr/rjw069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wanis M, Nafie S, Mellon JK. A case of Fournier's gangrene in a young immunocompetent male patient resulting from a delayed diagnosis of appendicitis. J Surg Case Rep. 2016;2016:pii. doi: 10.1093/jscr/rjw058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Obi AO. Isolated Fournier's gangrene of the penis. Niger J Clin Pract. 2016;19:426–430. doi: 10.4103/1119-3077.179297. [DOI] [PubMed] [Google Scholar]
- 12.Park SJ, Kim DH, Choi CI, Yun SP, Kim JH, Seo HI, et al. Necrotizing soft tissue infection: analysis of the factors related to mortality in 30 cases of a single institution for 5 years. Ann Surg Treat Res. 2016;91:45–50. doi: 10.4174/astr.2016.91.1.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Doluoğlu ÖG, Karagöz MA, Kılınç MF, Karakan T, Yücetürk CN, Sarıcı H, et al. Overview of different scoring systems in Fournier's gangrene and assessment of prognostic factors. Turk J Urol. 2016;42:190–196. doi: 10.5152/tud.2016.14194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sen H, Bayrak O, Erturhan S, Borazan E, Koc MN. Is hemoglobin A1c level effective in predicting the prognosis of Fournier gangrene? Urol Ann. 2016;8:343–347. doi: 10.4103/0974-7796.184905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sorensen MD, Krieger JN. Fournier's gangrene: epidemiology and outcomes in the general US population. Urol Int. 2016;97:249–259. doi: 10.1159/000445695. [DOI] [PubMed] [Google Scholar]
- 16.Jerraya H, Fehri H, Khalfallah M, Abdesselem MM, Dziri C. Predictive factors of mortality in Fournier's gangrene. Tunis Med. 2015;93:800–803. [PubMed] [Google Scholar]
- 17.Yoshino H, Kawakami K, Yoshino G, Sawada K. Case of anal fistula with Fournier's gangrene in an obese type 2 diabetes mellitus patient. J Diabetes Investig. 2016;7:276–278. doi: 10.1111/jdi.12355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Izadi D, Coelho J, Gurjal S, Salim F. Fournier's gangrene and the reconstructive challenges for the plastic surgeon. Eplasty. 2016;16:ic38. [PMC free article] [PubMed] [Google Scholar]
- 19.Surganova VI, Vishnevskaya IF, Mihaylova OO. Multiple ectims and acneiform pustular syphilides in patients with secondary syphilis of the skin and mucous membranes against HIV infection. Clin Dermatol Venereol. 2013;6:23–26. [Google Scholar]
- 20.Ufimtseva MA, Gerasimova NM, Surganova VI, Ivashkevitch GA. Ectimatous syphilid in secondary fresh syphilis. Clin Dermatol Venereol. 2005;2:22–23. [Google Scholar]
- 21.Ufimtseva MA, Malishevskaya NP, Syrneva TA. Clinical and epidemiological features of syphilis in the territories of the urals, siberia and the far east. Russian J Dermatovenereol. 2009;2:68–73. [Google Scholar]