Abstract
Lung cancer is one of the major causes of death in the world. Small cell carcinoma is the most aggressive type and can spread rapidly. The association of a small cell carcinoma with hepatic hilar metastasis and biliary obstruction is rare. Endoscopic ultrasound allows the aspiration of a cytology sample from adenopathies for diagnostic purpose. We present the case of a patient with lung cancer, with lymph node metastasis to the hepatic hilum and extrinsic biliary tree compression. Endoscopic ultrasound allowed the definitive diagnosis of hepatic hilar metastasis of a lung small cell carcinoma. To the author's knowledge it was the first time that endoscopic ultrasound was used for the diagnosis of hepatic hilar lymph node metastasis of lung cancer.
Keywords: Endoscopic ultrasonography, hilar lymph nodes, jaundice, lung cancer, small cell carcinoma
INTRODUCTION
Lung cancer is the leading cause of cancer mortality in the world. Neuroendocrine tumors comprise from typical carcinoid with low malignancy and slow growth to the highly aggressive small cell carcinoma. At the time of diagnosis, approximately 30% of patients have the disease limited to the hemithorax, supraclavicular lymph nodes, or mediastinal tumors. This histological type accounts for about 20% of all lung tumors that metastasizes early, with the sites of metastasis being most frequently the liver, bones, brain, and adrenal gland. The association of a small cell carcinoma with jaundice is rare. In certain situations it is vital to exclude other causes of adenopathies besides lung cancer. The endoscopic ultrasound may have a fundamental role in this setting, allowing sample collection for a definitive diagnosis.
CASE REPORT
A 61-year-old male presented right chest pain, exacerbated by inspiration, with evolution of a month and progressive worsening. He denied weight loss, cough, sputum, or dyspnea. The past medical history revealed tobacco consumption (50 packs per year), with no other relevant history. Thoracic-abdominal-pelvic computed tomography (CT) showed in the right lung upper lobe (RUL) a 10 × 7.8 cm lesion (greater dimensions), in contact with pleura and a mediastinal adenopathy with 2 cm of greater diameter.
Subsequently, a positron emission tomography was performed, in which hypermetabolism of 18-fluorodeoxyglucose was observed in the RUL and right tracheobronchial lymph node. These findings were consistent with lung cancer and lymph node metastasis. Transthoracic biopsy of lung mass was performed and the histological examination revealed a non-small cell lung carcinoma (NSCLC).
The endobronchial ultrasound with biopsy of mediastinal lymphadenopathy showed a neuroendocrine SCLC. The diagnosis of lung cancer mixed cellularity (T3N2M0; tumor, node, and metastasis (TNM) classification) was assumed.
The patient initiated treatment with etoposide, carboplatin, and radiotherapy. Reassessment after 6 months with CT showed onset of abdominal lymphadenopathy (celiac trunk) and slight increase in the mediastinal lymphadenopathy (2 × 3.5 cm). They were considered metastasis of lung cancer and the patient initiated second-line chemotherapy with paclitaxel. Nevertheless, the disease maintained progression with increased mediastinal lymphadenopathy.
Then, the patient initiated third line chemotherapy with topotecan. The thoracic adenopathy stabilized, but progression of the disease occurred with onset of multiple lymph nodes involving the hepatic hilum [Figure 1], causing moderate dilatation of the main bile duct and of right and left hepatic duct.
Figure 1.
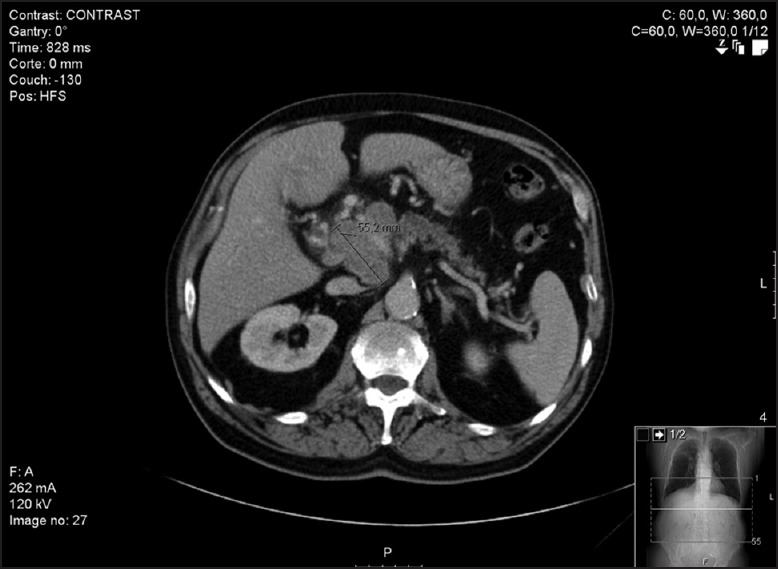
Computed tomography. Lymph nodes involving the hepatic hilum
To exclude other causes of hepatic hilar adenopathy, and given the lack of response to chemotherapy and radiotherapy, a fine-needle aspiration (25-G) guided by endoscopic ultrasound of the hepatic hilar lymph nodes was performed [Figure 2a and b]. Cytology revealed the presence of a small cell carcinoma [Figure 3a–d]. The immunocytochemical study showed positivity to chromogranin, synaptophisin, and thyroid transcription factor-1 (TTF-1). He underwent endoscopic retrograde cholangiopancreatography (ERCP), in which a stenosis of the distal third of the main biliary duct was identified. Sphincterotomy and placement of a metallic biliary stent with 10 Fr were performed.
Figure 2.
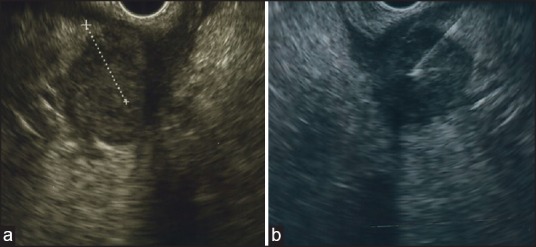
Endoscopic ultrasound. (a) Hilar lymph node; and (b) fine-needle aspiration
Figure 3.
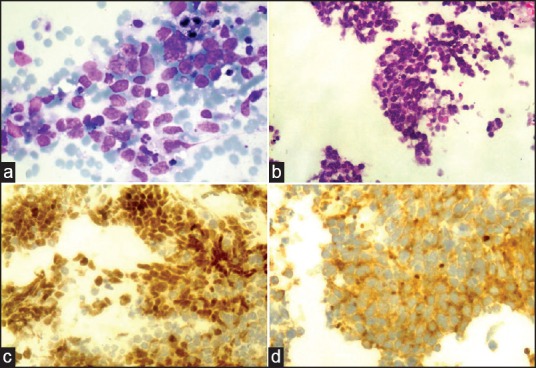
Cytological examination. (a) Lymph node containing metastatic small cell carcinoma (Diff-Quick stain, ×400); (b) histological small cell pattern in a cell block section (H and E stain, ×250); (c) thyroid transcription factor-1 (TTF-1) immunohistochemical staining, nuclear positivity (×250); (d) Synaptophysin positivity, that confirms neuroendocrine differentiation (×250)
A palliative radiotherapy of the hilar lymph nodes and subsequent etoposide cycle was performed; however, without response. The patient was admitted 1 month after for worsening of general condition with prostration, and died during that hospitalization.
DISCUSSION
This article describes the case of an obstruction of the biliary tract, secondary to extrinsic compression caused by hepatic hilar lymphadenopathy. The tumors more frequently associated with malignant biliary obstruction are the gastric, colon, and breast. Reports of cases of jaundice secondary to a small cell carcinoma metastasis are rare.[1,2,3,4,5,6]
The endoscopic ultrasound has been used to diagnose causes of enlarged lymph nodes, allowing the distinction between malignant and nonmalignant causes of hepatic hilum adenopathies, such as infectious disease.[7]
The endoscopic ultrasound is a safe, minimum invasive, and accessible method to diagnose and evaluate the hepatic hilum, even in malignant diseases.[7,8]
In this case, following a suspected obstruction of the biliary tract by an adenopathy, a diagnostic puncture was performed by endoscopic ultrasound, establishing the diagnosis. Obstruction of biliary tree caused by the spread of the tumor was resolved with a stent placement. The treatment with chemotherapy was ineffective. Unfortunately, the outcome was fatal.
The endoscopic ultrasonography has successfully been used in many cases for the diagnosis of mediastinal lymph node metastasis in lung cancer; but to the author's knowledge, it was the first time it was used for the diagnosis of hepatic hilar lymph node metastasis of lung cancer.[9]
Our approach supports the progressive use of endoscopic ultrasound in the evaluation of the liver and hilum pathology. Probably in a near future, the endoscopic ultrasound will be used more frequently in the evaluation and therapy of this pathology. In that context, some authors have characterized the anatomy of the hepatic hilum by endoscopic ultrasonography and the possibility of using that region as a landmark to study the liver anatomy segmentation.[10]
REFERENCES
- 1.Johnson DH, Hainsworth JD, Greco FA. Extrahepatic biliary obstruction caused by small-cell lung cancer. Ann Intern Med. 1985;102:487–90. doi: 10.7326/0003-4819-102-4-487. [DOI] [PubMed] [Google Scholar]
- 2.Martin A, Castagliuolo I, Mastropaolo G, et al. Cholestatic jaundice as the presenting symptom of small-cell lung cancer. Ital J Gastroenterol. 1990;22:36–9. [PubMed] [Google Scholar]
- 3.Kotan C, Er M, Ozbay B, et al. Extrahepatic biliary obstruction caused by small-cell lung cancer: A case report. Acta Chir Belg. 2001;101:190–2. [PubMed] [Google Scholar]
- 4.Sakar A, Kara E, Aydede H, et al. A case of a small-cell lung carcinoma presenting with jaundice due to pancreatic metastasis. Tuberk Toraks. 2005;53:181–4. [PubMed] [Google Scholar]
- 5.Obara M, Satoh H, Yamashita YT, et al. Metastatic small-cell lung cancer causing biliary obstruction. Med Oncol. 1998;15:292–4. doi: 10.1007/BF02787217. [DOI] [PubMed] [Google Scholar]
- 6.Jeong IB, Kim SM, Lee TH, et al. Pancreatic metastasis and obstructive jaundice in small-cell lung carcinoma. Korean J Intern Med. 2006;21:132–5. doi: 10.3904/kjim.2006.21.2.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saieg MA, Yazawa F, Horta M, et al. The utility of endoscopic ultrasound guided fine needle aspiration in the diagnosis of infectious diseases — report of three cases. Case Rep Infect Dis 2013. 2013;512182 doi: 10.1155/2013/512182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fritscher-Ravens A, Broering DC, Sriram PV, et al. EUS-guided fine-needle aspiration cytodiagnosis of hilar cholangiocarcinoma: A case series. Gastrointest Endosc. 2000;52:534–40. doi: 10.1067/mge.2000.109589. [DOI] [PubMed] [Google Scholar]
- 9.Eloubeidi MA, Cerfolio RJ, Chen VK, et al. Endoscopic ultrasound-guided fine needle aspiration of mediastinal lymph node in patients with suspected lung cancer after positron emission tomography and computed tomography scans. Ann Thorac Surg. 2005;79:263–8. doi: 10.1016/j.athoracsur.2004.06.089. [DOI] [PubMed] [Google Scholar]
- 10.Bhatia V, Hijioka S, Hara K, et al. Endoscopic ultrasound description of liver segmentation and anatomy. Dig Endosc. 2014;26:482–90. doi: 10.1111/den.12216. [DOI] [PubMed] [Google Scholar]


