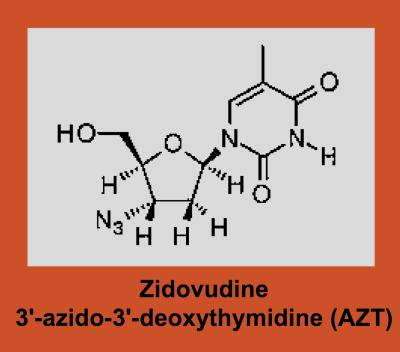
The introduction of zidovudine (3′-azido-3′-deoxythymidine; AZT; Scheme S1) into clinical practice in 1987 ushered in the therapeutic era of the AIDS epidemic. Not long thereafter, isolation of an AZT-resistant variant of HIV type 1 (HIV-1) was reported (1). Work by several groups demonstrated the association between emergence of AZT resistance and disease progression in patients receiving antiretroviral therapy (2–4). High-level AZT resistance requires mutations at reverse transcriptase (RT) codons 41, 67, 70, 210, 215, and 219, which emerge in an ordered fashion (5, 6). The K70R mutation usually is the first to emerge. Although this mutation produces only a modest decrease in drug susceptibility, K70R mutants are selected rapidly after initiation of AZT (7). Subsequently, variants with mutations at codon 215 emerge and replace the K70R mutants. A likely explanation for the slower emergence of mutants carrying T215Y or F substitutions is the requirement for a double-nucleotide mutation at this codon [215T(ACC) to 215Y(TAC) or 215F(TTC), respectively].
Scheme 1.
Transmission of an AZT-resistant isolate of HIV-1 was first reported in 1992 (8). Recent studies show a prevalence of AZT resistance mutations in viral sequences from newly infected individuals of 5–10% (9, 10), documenting a dramatic increase in the transmission of AZT-resistant HIV-1 over the past decade. In the absence of continued selective pressure from AZT-containing therapy, resistant variants eventually are replaced by AZT-susceptible revertants. Such revertants frequently involve the substitution at codon 215 of unusual amino acids such as aspartate, asparagine, cysteine, or serine in place of the mutant and wild-type residues more commonly encountered at this position. The 215D(GAC), 215N(AAC), 215C(TGC), and 215S(TCC) variants can each arise as a result of single nucleotide changes from 215Y or -F and appear to be more common than wild-type 215T revertants. In contrast to strains carrying the 215Y or -F mutation, variants with these alternative amino acid residues are AZT-sensitive. Moreover, these partial revertants appear to be fitter than the 215Y virus when tested in growth competition experiments (11, 12).
In this issue of PNAS, García-Lerma et al. (13) report that 215C, -D, -N, and -S variants were observed in 3.3% of virus sequences from a cohort of 603 untreated individuals with recently diagnosed HIV-1 infection. In addition, they demonstrate that recombinant viruses carrying 215C or -D mutations readily give rise to AZT-resistant 215Y mutants when passaged in vitro in the presence of AZT. These findings have importance with regard to the epidemiology of transmission of drug-resistant HIV-1 and imply that the 215C, -D, -N, or -S variants represent intermediate forms that may have significant consequences with regard to the emergence of drug resistance in patients subsequently treated with AZT- or stavudine (d4T)-containing regimens. Previous studies documented the occurrence of these variants after discontinuation of AZT in patients harboring AZT-resistant (215Y) strains of HIV-1, or in newly infected individuals who had acquired an AZT-resistant virus by transmission (11, 12, 14). In contrast to the acutely infected patients described in earlier reports, the patients studied by García-Lerma et al. had established HIV-1 infection of unknown duration. Detection of the 215C, -D, -N, or -S variants circulating in these patients provides a kind of fossil record of past infection with AZT-resistant HIV-1.
Much attention has focused recently on the consequences of interrupting antiretroviral therapy in patients infected with highly drug-resistant viruses. In nearly all such cases, high-level drug resistance evolved after infection with drug-sensitive HIV-1 as a consequence of sequential therapy with partially suppressive regimens. Studies show that interruption of antiretroviral therapy leads to the re-emergence of wild-type, drug-sensitive virus, and is accompanied by substantial increases in plasma HIV-1 RNA titer (15, 16). The increase in plasma HIV-1 RNA is correlated to the increased replicative capacity of the re-emergent drug-sensitive virus relative to the drug-resistant species that predominate before the treatment interruption. In these studies, the simultaneous loss of resistance to several antiretroviral drugs in different classes strongly suggests that outgrowth of residual drug-sensitive virus, rather than reversion of multiple drug resistance mutations, is responsible for the rapid shift in drug susceptibility. Latently infected resting memory CD4+ cells or long-lived productively infected cells are presumed to serve as the reservoir of this drug-sensitive virus (17).
By contrast, because HIV-1 transmission usually involves infection with an oligoclonal viral population no reservoir of drug-sensitive virus exists in patients who become infected with drug-resistant HIV-1. In this setting, emergence of drug-susceptible variants requires back-mutation. Studies in which serial samples are available following transmission of AZT-resistant HIV-1 document the emergence of 215C, -D, -N, and -S variants over time (11, 12, 14). These observations support the conclusion by García-Lerma et al. that the viruses carrying the 215 variants identified in their cross-sectional study most likely emerged as a result of back-mutation from 215Y or -F. However, the possibility that the AZT-sensitive revertants were themselves transmitted from patients who had previously been treated with AZT cannot be excluded.
An important finding by García-Lerma et al. is their demonstration that serial passage of recombinant viruses carrying the 215C or -D mutations in the presence of AZT leads rapidly to selection of AZT-resistant variants carrying the 215Y mutation. The mean time to emergence of 215Y was 25 days for the 215C variants and 31 days for the 215D variants. By contrast, passage of wild-type control viruses in the presence of AZT led to emergence of AZT resistance mutations after a mean of 63 days. These results are consistent with a recent report that noted rapid selection of 215Y on initiation of d4T in a patient whose virus carried a mixture of the 215D and -S mutations. [The thymidine analog d4T selects for the same mutations as does AZT (18).] These findings highlight the potential clinical importance of identifying these intermediate forms in the virus population by resistance testing.
Studies show that interruption of antiretroviral therapy leads to the re-emergence of wild-type, drug-sensitive virus, and is accompanied by substantial increases in plasma HIV-1 RNA titer.
Nevertheless, the clinical significance of transmitted AZT resistance remains controversial. Early studies with AZT monotherapy provide conflicting data (8, 19), and more recent data are confounded by the use of potent triple-therapy regimens. Studies in chronically infected patients who received prior AZT therapy suggest that presence of AZT resistance mutations (in the absence of resistance to other components of the regimen) does not significantly reduce the antiviral activity of combination regimens that include a protease inhibitor (20). Different results might be obtained by using alternative triple-therapy regimens that include a non-nucleoside RT inhibitor or the nucleoside abacavir in place of a protease inhibitor. Such regimens are highly effective in treating drug-naive patients, but may be compromised in patients with preexisting AZT resistance (21).
Recent work suggests that primer unblocking by pyrophosphorylysis is the major mechanism of ZDV resistance (22). This reaction (in essence the reversal of DNA polymerization) results in the removal of the terminal AZT monophosphate from the growing DNA strand, thereby relieving the block to reverse transcription. ATP can serve as a pyrophosphate donor for primer unblocking (23). Removal of the terminal nucleotide leads to formation of an AZT-adenine dinucleotide tetraphosphate. Modeling of the predicted three-dimensional structure of AZT-resistant RT suggests that presence of a tyrosine or phenylalanine residue at position 215 stabilizes the pyrophosphate donor in the substrate binding pocket through stacking interactions between the aromatic side chain of these amino acid residues and the adenine of ATP, thus favoring excision of the terminal AZT-MP (24). Although an increased rate of pyrophosphorylysis would be advantageous in the presence of AZT, it could result in a decreased rate of reverse transcription. A reduction in the net polymerization rate is partially offset by the observed increase in processivity that is also associated with presence of the 215Y mutation (22, 25). Nevertheless, the replacement of 215Y by alternative amino acids that lack the same potential for stabilizing ATP as a pyrophosphate donor suggests that enhanced pyrophosphorylysis has a selective disadvantage in the absence of AZT. It would be interesting to compare rates of ATP-dependent primer unblocking in RT purified from AZT-resistant virus and from the AZT-sensitive revertants described by García-Lerma and others.
Although the study of drug resistance tends to focus on a small number of mutations that can be shown to produce a measurable effect on drug susceptibility, the viral genetic background plays an important role in modulating the phenotypic expression of these mutations. For example, the V75T mutation confers modest resistance to d4T when present in HIV-1Hxb2 but not in HIV-1NL4–3 or HIV-1RF (26). Similarly, García-Lerma et al. found that the effect on viral fitness of 215C, -D, or -S depended on the specific genetic background in which the mutants were tested. Thus, whereas 215D viruses were fitter than 215S when the 210W mutation was also present, 215S appeared fitter than 215D in a wild-type background. Likewise, 215C viruses were fitter than 215S when present together with 41L and 210W, but 215S appeared fitter than 215C in the wild-type background. Moreover, introduction of 215C into an RT background derived from a patient isolate resulted in a virus that was less fit than wild-type (215T), whereas 215C and 215T viruses were similarly fit in an Hxb2 background. These results highlight the importance of testing the effects of novel resistance mutations in several different viral genetic backgrounds.
Little is known about the mechanism by which the 41L mutation contributes to AZT resistance. This mutation confers only modest resistance to AZT by itself, but augments the level of resistance when present together with 215Y. The 41L mutation rarely is seen in the absence of 215Y, and maintenance of 41L in the population entails a significant fitness cost to the virus in the absence of AZT (27). When present together the 41L and 215Y mutations confer ≈60-fold reduction in susceptibility to AZT (6). Viruses that carry these mutations are substantially less fit than wild type in the absence of AZT. Emergence of the 41L and 215Y mutations requires mutation of three nucleotides (two for T215Y and one for M41L). For this reason, high-level resistance usually develops slowly when AZT is used to treat patients with wild-type virus. Data from García-Lerma et al. and other groups suggest that the 41L mutation is relatively stable in the virus population when present together with 215C, -D, or -S. These AZT-susceptible revertants are just as fit as wild-type in the absence of AZT, but retain the potential for rapid emergence of high-level AZT resistance by a single nucleotide substitution at codon 215. In this sense, these revertants are better adapted than the ancestral wild-type strain to future AZT exposure.
The work carried out by García-Lerma et al. provides an important link between surveillance for the spread of drug-resistant HIV-1 in the population and a more fundamental understanding of how HIV-1 adapts to replicate under varying selective pressures. As transmission of drug-resistant HIV-1 increases worldwide, long-term virologic study of newly infected individuals identified through existing surveillance programs will be needed to uncover novel pathways for viral adaptation.
Footnotes
See companion article on page 13907.
References
- 1.Larder B A, Darby G, Richman D D. Science. 1989;243:1731–1734. doi: 10.1126/science.2467383. [DOI] [PubMed] [Google Scholar]
- 2.Kozal M J, Shafer R W, Winters M A, Katzenstein D A, Merigan T C. J Infect Dis. 1993;167:526–532. doi: 10.1093/infdis/167.3.526. [DOI] [PubMed] [Google Scholar]
- 3.D'Aquila R T, Johnson V A, Welles S L, Japour A J, Kuritzkes D R, DeGruttola V, Reichelderfer P S, Coombs R W, Crumpacker C S, Kahn J O, et al. Ann Intern Med. 1995;122:401–408. doi: 10.7326/0003-4819-122-6-199503150-00001. [DOI] [PubMed] [Google Scholar]
- 4.Japour A J, Welles S, D'Aquila R T, Johnson V A, Richman D D, Coombs R W, Reichelderfer P S, Kahn J O, Crumpacker C S, Kuritzkes D R. J Infect Dis. 1995;171:1172–1179. doi: 10.1093/infdis/171.5.1172. [DOI] [PubMed] [Google Scholar]
- 5.Larder B A, Kemp S D. Science. 1989;246:1155–1158. doi: 10.1126/science.2479983. [DOI] [PubMed] [Google Scholar]
- 6.Boucher C A B, O'Sullivan E, Mulder J W, Ramautarsing C, Kellam P, Darby G, Lange J M A, Goudsmit J, Larder B A. J Infect Dis. 1992;165:105–110. doi: 10.1093/infdis/165.1.105. [DOI] [PubMed] [Google Scholar]
- 7.Kuritzkes D R, Quinn J B, Benoit S L, Shugarts D L, Griffin A, Bakhtiari M, Poticha D, Eron J J, Fallon M A, Rubin M. AIDS. 1996;10:975–981. doi: 10.1097/00002030-199610090-00007. [DOI] [PubMed] [Google Scholar]
- 8.Erice A, Mayers D L, Strike D G, Balfour H J. N Engl J Med. 1993;328:1163–1165. doi: 10.1056/NEJM199304223281605. [DOI] [PubMed] [Google Scholar]
- 9.Little S J, Daar E S, D'Aquila R, Keiser P, Connick E, Whitcomb J, Hellmann N S, Petropoulos C J, Sutton L, Pitt J, et al. J Am Med Assoc. 1999;282:1142–1149. doi: 10.1001/jama.282.12.1142. [DOI] [PubMed] [Google Scholar]
- 10.Yerly S, Kaiser L, Race E, Bru J P, Clavel F, Perrin L. Lancet. 1999;354:729–733. doi: 10.1016/S0140-6736(98)12262-6. [DOI] [PubMed] [Google Scholar]
- 11.Goudsmit J, de Ronde A, Ho D D, Perelson A. J Virol. 1996;70:5662–5664. doi: 10.1128/jvi.70.8.5662-5664.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Ronde A, van Dooren M, van der Hoek L, Bouwhuis D, de Rooij E, van Gemen B, de Boer R J, Goudsmit J. J Virol. 2001;75:595–602. doi: 10.1128/JVI.75.2.595-602.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.García-Lerma J G, Nidtha S, Blumoff K, Weinstock W, Heneine W. Proc Natl Acad Sci USA. 2001;98:13907–13912. doi: 10.1073/pnas.241300698. . (First Published November 6, 2001; 10.1073/pnas.241300698) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yerly S, Rakik A, Kinloch-De Loes S, Hirschel B, Descamps D, Brun-Vesinet F, Perrin L. J Virol. 1998;72:3520–3523. doi: 10.1128/jvi.72.5.3520-3523.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deeks S G, Wrin T, Liegler T, Hoh R, Hayden M, Barbour J D, Hellmann N S, Petropoulos C J, McCune J M, Hellerstein J M, Grant R M. N Engl J Med. 2001;344:472–480. doi: 10.1056/NEJM200102153440702. [DOI] [PubMed] [Google Scholar]
- 16.Miller V, Sabin C, Hertogs K, Bloor S, Martinez-Picado J, D'Aquila R, Larder B, Lutz T, Gute P, Weidmann E, et al. AIDS. 2000;14:2857–2867. doi: 10.1097/00002030-200012220-00007. [DOI] [PubMed] [Google Scholar]
- 17.Finzi D, Blankson J, Siliciano J D, Margolick J, Chadwick K, Pierson T, Smith K, Lisziewicz J, Lori F, Flexner C, et al. Nat Med. 1999;5:512–525. doi: 10.1038/8394. [DOI] [PubMed] [Google Scholar]
- 18.Coakley E, Gillis J, Hammer S M. AIDS. 2000;14:F9–F15. doi: 10.1097/00002030-200001280-00002. [DOI] [PubMed] [Google Scholar]
- 19.Imrie A, Carr A, Duncombe C, Finalyson R, Vizzard J, Law M, Kaldor J, Penny R, Cooper D A. J Infect Dis. 1996;174:195–198. doi: 10.1093/infdis/174.1.195. [DOI] [PubMed] [Google Scholar]
- 20.Kuritzkes D, Sevin A, Young B, Bakhtiari M, Wu H, St. Clair M, Connick E, Spritzler J, Lederman M M. J Infect Dis. 2000;181:491–497. doi: 10.1086/315244. [DOI] [PubMed] [Google Scholar]
- 21.Opravil M, Yerly S, Staszewski S, Stone C, Ait-Khaled M, Perrin L. Antiviral Therapy. 2000;5, Suppl. 3:95–96. [Google Scholar]
- 22.Arion D, Kaushik N, McCormick S, Borkow G, Parniak M. Biochemistry. 1998;37:15908–15917. doi: 10.1021/bi981200e. [DOI] [PubMed] [Google Scholar]
- 23.Meyer P R, Matsuura S E, So A G, Scott W A. Proc Natl Acad Sci USA. 1998;95:13471–13476. doi: 10.1073/pnas.95.23.13471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boyer P L, Sarafianos S G, Arnold E, Hughes S H. J Virol. 2001;75:4832–4842. doi: 10.1128/JVI.75.10.4832-4842.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Caliendo A M, Savara A, An D, DeVore K, Kaplan J C, D'Aquila R T. J Virol. 1996;70:2146–2153. doi: 10.1128/jvi.70.4.2146-2153.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lin P F, González C J, Griffith B, Friedland G, Calvez V, Ferchal F, Schinazi R F, Shepp D H, Ashraf A B, Wainberg M A, et al. Antivir Ther. 1999;4:21–28. [PubMed] [Google Scholar]
- 27.Harrigan P R, Bloor S, Larder B A. J Virol. 1998;72:3773–3778. doi: 10.1128/jvi.72.5.3773-3778.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]