Abstract
Retronychia is a recently described disorder caused by ingrowth of the proximal nail plate into the proximal nail fold. It is suspected when there is persistent paronychia, particularly in the setting of trauma. This disease is probably underdiagnosed due to limited knowledge among dermatologists and the presence of incomplete clinical forms. Nail plate avulsion is the diagnostic and curative procedure of choice, despite reports of relapse.
Keywords: Nail diseases; Nails, ingrown; Paronychia
INTRODUCTION
Retronychia, described by De Berker and Renall in 1999, refers to the proximal nail plate ingrowth into the proximal nail fold.1 The condition emerged as a distinct entity in 2008 when De Berker et al. presented a series of 19 cases in meetings of the European Nail Society (ENS).2 Less than 100 cases of retronychia have been reported in the literature.1-16 Trauma or systemic illness are the most common precipitating events, causing disruption of longitudinal nail bed growth and vertical growth of the new plate into the proximal nail fold. The condition is associated with multiple generations of nail plate misalignment beneath the proximal nail.2
EPIDEMIOLOGY
Retronychia is a disease of adulthood predominating in females, although it has also been reported in children and in eldery.1-4,6 It mainly affects the halluces due to frequent trauma to these toes , and less frequently the fingernails.1-3,5,6 Bilateral involvement and retronychia in multiple digits have been reported. 1,2,5,6, 7,9,10
PATHOPHYSIOLOGY
Normal nail growth involves the production of the nail plate from the nail matrix, which moves outward over the nail bed.11 Usually, as seen in Beau's line and onychomadesis, the original nail remains aligned in the horizontal axis so that the newly forming nail is able to push the separated original nail out distally.2,11 Retronychia begins with disruption of the nail's longitudinal growth due to an acute injury, usually of a physical or systemic nature. Such injury leads to separation of the old plate from the matrix and nail bed, with vertical growth of the new nail plate into the PNF.10,11
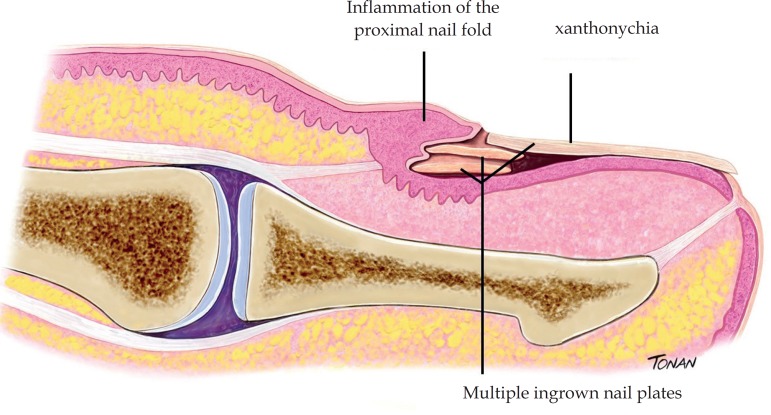
After a precipitating event (trauma), complete onychomadesis cannot occur, since the nail plate may remain held in the lateral wings of the nail matrix due to curvature of these areas, leading to embedding of the upper old nail into the ventral aspect of the proximal nail fold and secondary paronychia (Figure 1).10
Figure 1.
Retronychia: Longitudi nal view showing multiple ingro wn nail plates, xanthonychia and inflammation of the proximal nail fold. Illustration by Rodrigo Tonan
Some authors have observed in their patients that the old nail remains firmly attached to the nail bed and nail folds, and cannot be pushed out by the new plate, suggesting that where such adherence is firmer the shedding process proceeds abnormally.2
Meanwhile, there are reports of pronounced onycholysis of affected nails.3 This may have two interrelated consequences. First, the nail is no longer attached to the nail bed and can be pushed back into the nail pocket, injuring the overlying proximal nail fold. In severe onycholysis, the nail bed does not support this forward growth. The nail, which is loose in its pocket, is permanently pushed against the proximal nail fold, causing inflammation, accounting for the clinical signs of pain, paronychia, and granulation tissue. Repetitive disruption of nail matrix growth can lead to stacking of nail plates. Repeated injury prevents the new plate from adhering to the nail bed, thereby perpetuating the cycle.3
The most common triggers are repeated minor injuries (e.g., poorly fitting shoes, sports practices like jogging or hiking), and local trauma that causes pressure against the free edge. In some cases, no triggers are identified.2,6 Systemic conditions (arthritis, thrombophlebitis, postpartum) including severe stress episodes that affect the matrix region, usually highly sensitive to hypoxia, have been described as causes of this entity.2,6,8,12 Lateral deviation of the big toe has been considered a potential predisposing factor, as well as reflex hypertension of halluces.5,6
High-frequency ultrasound studies suggested that retronychia results from a direct mechanism where the entire nail unit is embedded into the proximal nail fold region. This retrograde motion, probably caused by the development of traction forces generated by inflammation and scarring, is demonstrated as decreased distance between the origin of the nail plates and the distal interphalangeal joint in affected digits.7,8,14,16
CLINICAL MANIFESTATIONS
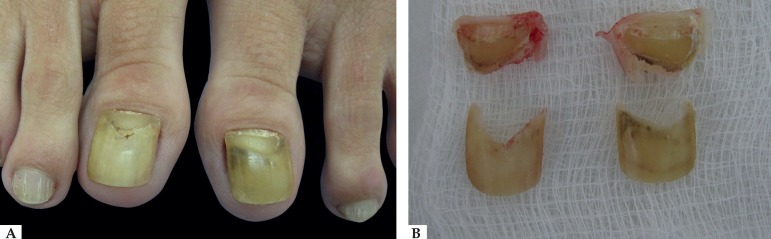
Clinical suspicion of retronychia is based on an unresolved chronic proximal paronychia in the setting of disrupted nail growth and multiple generations of nail plate.1-3,6,10 Other nail symptoms, usually present on diagnosis, are xanthonychia, pain, impaired walking (when the toenails are affected), oozing, and onycholysis (Figures 2 and 3). The presence of granulation tissue between proximal and lateral nail folds is common.
Figure 2.
A - Onycholysis and xanthonychia of both halluces in the setting of disrupted nail growth B - The avulsed nail plate presents multiple layers
Figure 3.
Periungual erythema, onycholysis, and mild yellow colo ration of the right big toenail after local trauma
Yellow discoloration of the nail can be attributed to proximal onycholysis with accumulation of inflammatory exudate, stunted nail growth, as well as multiple nail generations beneath the uppermost nail.6 Elevation of the proximal part of the nail plate occurs, and as the proximal nail fold is pushed back, the nail plate appears to be elongated.6
Two stages of retronychia are reported: the early stage (stage 1), frequently underdiagnosed and characterized by interrupted nail growth, yellowish nail plate discoloration and exudate from beneath the proximal nail fold, but with discreet paronychia; and the late stage (stage 2), where all symptoms are present, particularly intense paronychia and slight elevation of the proximal nail fold.6
DIAGNOSIS
The diagnosis of retronychia is clinical. It is suspected when there is persistent paronychia, particularly in the setting of trauma. Important clinical diagnostic criteria include chronic and often painful inflammation of the proximal nail fold, xanthonychia, granulation tissue emerging from under the nail fold, thickening of the proximal portion of the nail plate, and interruption of nail growth (Figure 4). Clinical diagnosis may be difficult, since not all symptoms may be present at the same time and disease duration can be prolonged, since patients may not be bothered by the condition.6
Figure 4.
Chronic painful paronychia, xanthonychia, thickening of the proximal portion of the nail plate, and multiple generations of nail plate. Note apparent adhesion of the plate to the lateral horns
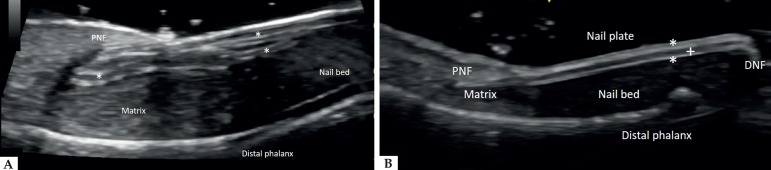
Ultrasound imaging can be used as a noninvasive confirmatory test (Figure 5). It allows clear visualization of nail components in real time and effectively rules out tumor entities and hidden complications. Important sonographic criteria for diagnosing retronychia are the presence of more than 2 overlapping nail plates, decreased distance between the origin of the nail plates and the base of the distal phalanx (level of the distal interphalangeal joint compared with the contralateral digit), decreased echogenicity, and increased blood flow in the dermis of the posterior nail fold and proximal nail bed. 7,8,14,16
Figure 5.
Ultrasound longitudinal view of the hallux distal phalanx dorsal aspect. A - Retronychia, showing 3 overlapping nail plates* (PNF: proximal nail fold). B - Normal nail unit in the contralateral hallux, (PNF: proximal nail fold; DNF: distal nail fold; * dorsal and ventral nail plates; + inter-plate space)
Differential diagnosis should include diseases that can present as chronic paronychia (e.g., candidiasis or bacterial infections, rheumatoid arthritis, psoriasis), subungual tumors (Bowen's disease, keratoacanthomas, and amelanotic melanoma), and cysts.10,15
TREATMENT
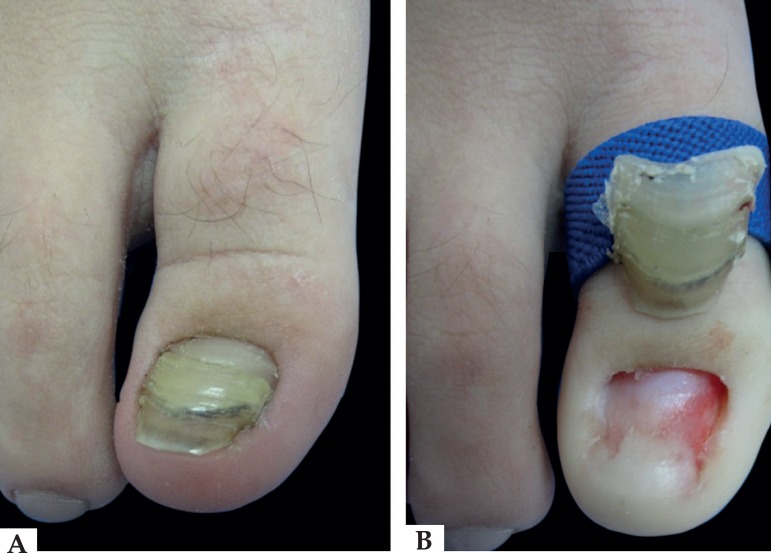
Proximal avulsion of the nail normally remains the treatment of choice for retronychia, besides confirming the diagnosis (Figure 6). The avulsed nail plate is proximally thickened and often presents two or more layers when viewed proximally. The procedure allows rapid treatment and pain relief. Conservative treatment such as taping, orthosis, and topical steroids may be helpful in early stages.4-6 Up to 16% of cases may recur.6 Permanent postsurgical nail dystrophy is unusual.4,12 Postoperative retraction of the nail bed with pincer nail and micronychia has been reported.6 After total avulsion of the nail, loss of counterpressure induced by the disappearance of the nail plate allows dorsal expansion of the distal pulp and may promote distal embedding with subsequent hyperkeratotic reaction.17 Conservative treatment to reduce the hyperkeratosis in front of the distal nail by using 50% urea occlusive dressing at night and debridement of hyperkeratosis with a scalpel blade is indicated. Massaging in the distal-plantar direction is recommended. Consistent taping is a valuable alternative. In the presence of severe pain, surgery is mandatory to free the distal edge of the plate (Dubois or Super "U" techniques). To prevent such a complication, an acrylic nail can be attached to the newly growing nail when it has reached one-third of its length. However, the upward force exerted by the pulp during gait often detaches the artificial nail.17 Patient education focusing on the importance of properly fitting footwear is important to prevent future trauma to the involved nail plate and matrix.11
Figure 6.
A - Preoperative view. B - After proximal avulsion of the nail
CONCLUSION
In the presence of posttraumatic proximal paronychia, xanthonychia, and disruption of linear nail plate growth, the diagnosis of retronychia should be considered. Knowledge of the condition allows appropriate and early treatment and avoids possible complications.
Footnotes
Work conducted at the Hospital do Servidor Público Municipal de São Paulo, São Paulo (SP), Brazil.
Conflict of interest: None.
AUTHORS'CONTRIBUTIONS
Cristina Diniz Borges Figueira de Mello
0000-0001-7199-8451
Design and planning of the study, Preparation and writing of the manuscript, Intellectual participation in propaedeutic and/or therapeutic conduct of studied cases
Milena da Rocha e Souza
0000-0002-0732-0432
Intellectual participation in propaedeutic and/or therapeutic conduct of studied cases, Critical review of the manuscript
Leandro Fonseca Noriega
0000-0002-2972-3718
Design and planning of the study, Critical review of the manuscript
Nilton Di Chiacchio
0000-0001-9536-2263
Approval of the final version of the manuscript, Design and planning of the study, Effective participation in research orientation, Critical review of the manuscript
REFERENCES
- 1.de Berker DAR, Rendall JRS. Retronychia-Proximal ingrowing nail. J Eur Acad Dermatol Venereol. 1999;12:S126–S126. [Google Scholar]
- 2.de Berker DA, Richert B, Duhard E, Piraccini BM, André J, Baran R. Retronychia: proximal ingrowing of the nail plate. J Am Acad Dermatol. 2008;58:978–983. doi: 10.1016/j.jaad.2008.01.013. [DOI] [PubMed] [Google Scholar]
- 3.Baumgartner M, Haneke E. Retronychia: diagnosis and treatment. Dermatol Surg. 2010;36:1610–1614. doi: 10.1111/j.1524-4725.2010.01693.x. [DOI] [PubMed] [Google Scholar]
- 4.Piraccini BM, Richert B, de Berker DA, Tengattini V, Sgubbi P, Patrizi A, et al. Retronychia in children, adolescents, and young adults: a case series. J Am Acad Dermatol. 2014;70:388–390. doi: 10.1016/j.jaad.2013.09.029. [DOI] [PubMed] [Google Scholar]
- 5.Ventura F, Correia O, Duarte AF, Barros AM, Haneke E. "Retronychia--clinical and pathophysiological aspects". J Eur Acad Dermatol Venereol. 2016;30:16–19. doi: 10.1111/jdv.13342. [DOI] [PubMed] [Google Scholar]
- 6.Gerard E, Prevezas C, Doutre MS, Beylot-Barry M, Cogrel O. Risk factors, clinical variants and therapeutic outcome of retronychia: a retrospective study of 18 patients. Eur J Dermatol. 2016;26:377–381. doi: 10.1684/ejd.2016.2774. [DOI] [PubMed] [Google Scholar]
- 7.Wortsman X, Calderon P, Baran R. Finger retronychias detected early by 3D ultrasound examination. J Eur Acad Dermatol Venereol. 2012;26:254–256. doi: 10.1111/j.1468-3083.2011.04068.x. [DOI] [PubMed] [Google Scholar]
- 8.Wortsman X, Wortsman J, Guerrero R, Soto R, Baran R. Anatomical changes in retronychia and onychomadesis detected using ultrasound. Dermatol Surg. 2010;36:1615–1620. doi: 10.1111/j.1524-4725.2010.01694.x. [DOI] [PubMed] [Google Scholar]
- 9.Cabete J, Lencastre A. Recognizing and treating retronychia. Int J Dermatol. 2015;54:e51–e52. doi: 10.1111/ijd.12635. [DOI] [PubMed] [Google Scholar]
- 10.Dahdah MJ, Kibbi AG, Ghosn S. Retronychia: report of two cases. J Am Acad Dermatol. 2008;58:1051–1053. doi: 10.1016/j.jaad.2007.12.038. [DOI] [PubMed] [Google Scholar]
- 11.Braswell MA, Daniel CR 3rd, Brodell RT. Beau lines, onychomadesis, and retronychia: A unifying hypothesis. J Am Acad Dermatol. 2015;73:849–855. doi: 10.1016/j.jaad.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 12.Fouilloux B. Retronychias. Presse Med. 2014;43:1223–1229. doi: 10.1016/j.lpm.2014.06.013. [DOI] [PubMed] [Google Scholar]
- 13.Reigneau M, Pouaha J, Truchetet F. Retronychia: four new cases. Eur J Dermatol. 2013;23:882–884. doi: 10.1684/ejd.2013.2226. [DOI] [PubMed] [Google Scholar]
- 14.Pizarro M, Pieressa N, Wortsman X. Posttraumatic Retronychia of the Foot with Clinical and Ultrasound Correlation. J Am Podiatr Med Assoc. 2017;107:253–256. doi: 10.7547/16-076. [DOI] [PubMed] [Google Scholar]
- 15.Chiheb S, Richert B, Belyamani S, Benchikhi H. Ingrown nail: A new cause of chronic perionyxis. Ann Dermatol Venereol. 2010;137:645–647. doi: 10.1016/j.annder.2010.06.020. [DOI] [PubMed] [Google Scholar]
- 16.Alonso-Pacheco ML, de Miguel-Mendieta E, Maseda-Pedrero R, Mayor-Arenal M. Retronychia: A Case Report Including Ultrasound Imaging and Surgical Treatment. Actas Dermosifiliogr. 2016;107:e33–e37. doi: 10.1016/j.ad.2015.06.018. [DOI] [PubMed] [Google Scholar]
- 17.Richert B. Surgery of the nail plate. In: Richert B, Di Chiacchio N, Haneke E, editors. Nail surgery. London: Healthcare; 2010. pp. 32–32. [Google Scholar]