Abstract
Patient: Female, 44
Final Diagnosis: Coronary artery dissection
Symptoms: Chest pain
Medication: —
Clinical Procedure: Coronary angiography • CT scan • transthoracic echocardiography • urgent cesarean delivery
Specialty: Cardiology
Objective:
Rare disease
Background:
Spontaneous coronary artery dissection is the most common etiology of pregnancy-associated myocardial infarction. It is characterized by high rates of maternal morbidity and mortality and may cause fetal complications and death as well.
Case Report:
A 44-year-old female (G2P1) suffered from pregnancy-related spontaneous coronary artery dissection with dissection of distal left anterior descending coronary artery. The patient was hemodynamically stable and did not required revascularization, but signs of fetal distress were detected and thus an urgent cesarean delivery was performed. This emergency procedure was undertaken in the catheterization laboratory (Cath-Lab) right after coronary angiography, thanks to a multidisciplinary team. Health conditions of the newborn were good. The patient instead suffered from a recurrence of spontaneous coronary artery dissection 6 days later, complicated by left ventricular apical thrombus and epistenocardial pericarditis. The dissection self-healed in 1 month.
Conclusions:
Careful evaluation of pregnancy-related spontaneous coronary artery dissection is needed to assess and manage both maternal and fetal complications. Under specific circumstances, a cesarean delivery may be required and be even performed in the Cath-Lab after coronary catheterization.
MeSH Keywords: Acute Coronary Syndrome, Coronary Artery Disease, Dissection, Pregnancy Complications
Background
Spontaneous coronary artery dissection (SCAD) is an important cause of acute coronary syndrome (ACS) in young patients without atherosclerotic coronary artery disease and represents the most common etiology of pregnancy-associated myocardial infarction [1,2]. Pathophysiology and optimal treatment of SCAD are both uncertain. High rates of complication and mortality have been reported for pregnancy-associated SCAD (P-SCAD)
We present a case of P-SCAD complicated by fetal distress which required an urgent cesarean delivery in the catheterization laboratory (Cath-Lab).
Case Report
A 44-year-old female, G2P1 (gravida 2 para 1), previously fit and well, at the 37th week of pregnancy presented at the gynecological emergency department complaining of sudden onset of severe chest pain spreading to the left arm.
At admission, her electrocardiography (ECG) showed ST segment elevation in the antero-lateral leads, compatible with anterior ST segment elevation myocardial infraction (STEMI) (Figure 1).
Figure 1.
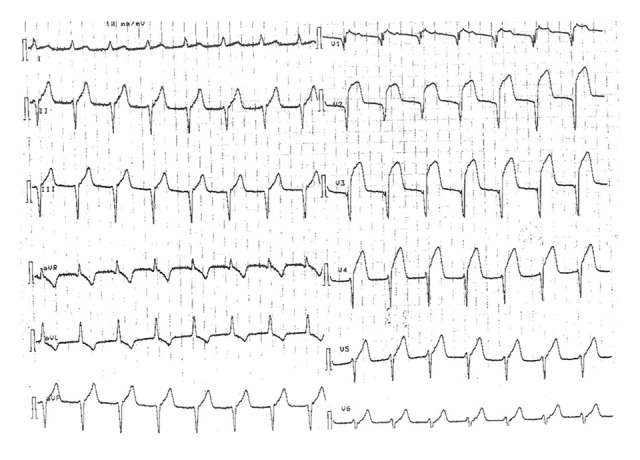
Electrocardiography at admission. ST-segment elevation in anterior leads. ESAOTE P8000.
The patient was therefore moved into the coronary intensive care unit.
Cardiac and thoracic examinations were unremarkable, but precocious signs of fetal distress were detected. The fetal heart rate was below 110 bpm, with evidence of frequent and irregular uterine contractions. Given concurrent maternal emergency and fetal distress, a multidisciplinary team (cardiologists, anesthetists and gynecologists) evaluated the case and decided to quickly assess cardiac status of the patient to consider whether and where to perform delivery.
Echocardiography detected akinesia of the anterior septum and of the apex, with moderate impairment of left ventricular systolic function with ejection fraction estimated at 45%.
An urgent coronary angiography was performed but identified only an irregularity of the distal left anterior descending (LAD) coronary artery, without critical stenosis. No intravascular optical coherence tomography (OCT) or intravascular ultrasound (IVUS) study was performed (Figure 2).
Figure 2.
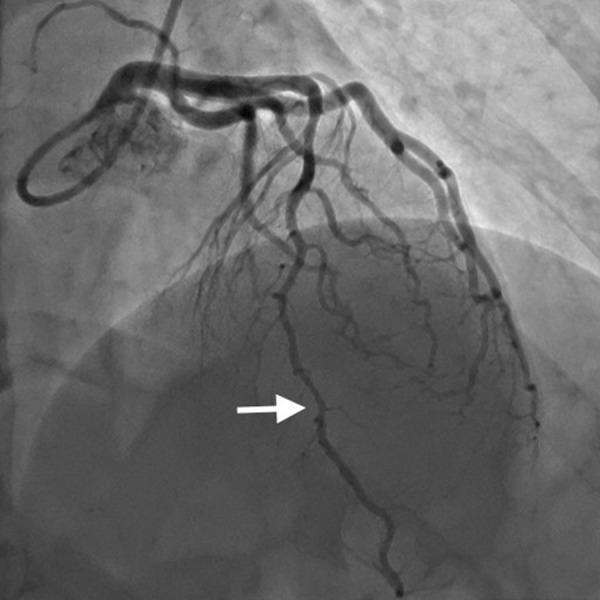
First coronary angiography (at admission) RAO cranial view showing only an irregularity of distal left anterior descending without critical stenosis, TIMI flow 3. Toshiba INFINIX.
Though coronary revascularization was not needed, clinical conditions of the patient were not reassuring. Yet, she was hemodynamically stable, although her systolic function was slightly reduced and there was a worsening of her cardiac status that could not be excluded at the time. Given the early signs of fetal distress and the final week of pregnancy, the multidisciplinary team decided to perform an urgent caesarean delivery in the Cath-Lab.
The newborn was healthy and in good condition. He was moved to the Department of Neonatology for continuation of care, while the patient, who at the time asymptomatic, was moved back into the intensive care unit.
The peak of cardiac troponin I was 72 ug/L (normal value <0.1 ug/L); serial ECGs showed an ischemic evolution with negative T waves in the anterior leads.
After 6 days of clinical wellness, the patient suffered again with chest pain, with ECG signs of ST segment elevation in the same leads of the first episode. No signs of hypoperfusion or major arrhythmias were present.
A second urgent coronary angiography was therefore performed, showing a sub-occlusive spontaneous dissection of the LAD, extending from the mid-proximal to the distal section with intimal flap and arterial wall hematoma (Figure 3). The second peak of cardiac troponin I was 40 ug/L.
Figure 3.
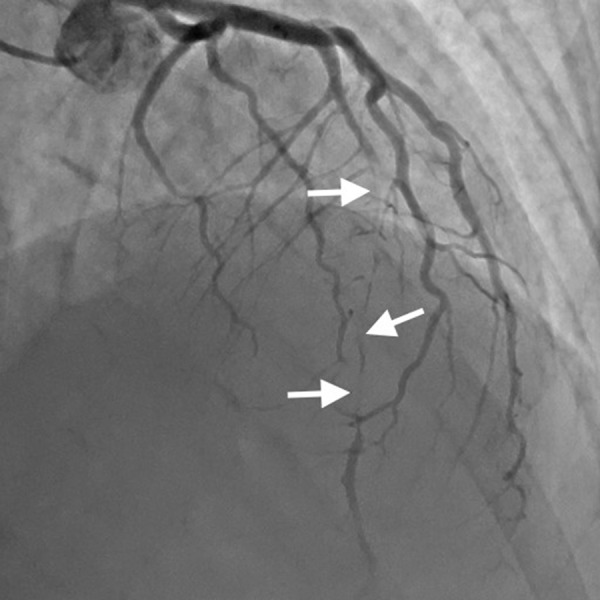
Second coronary angiography (6 days later) RAO cranial view showing extensive left anterior descending dissection starting from mid-proximal segment, involving diagonal branches. TIMI flow 1.
Given hemodynamical stability, the patient was treated conservatively with medical therapy.
The patient’s subsequent clinical course was complicated by an epistenocardial pericarditis and by left ventricular apical thrombus (Figure 4). A computed tomography (CT) study confirmed the spontaneous dissection of LAD, showing critical stenosis but without complete occlusion of the vessel and presence of apical ventricular thrombus (Figures 5, 6).
Figure 4.
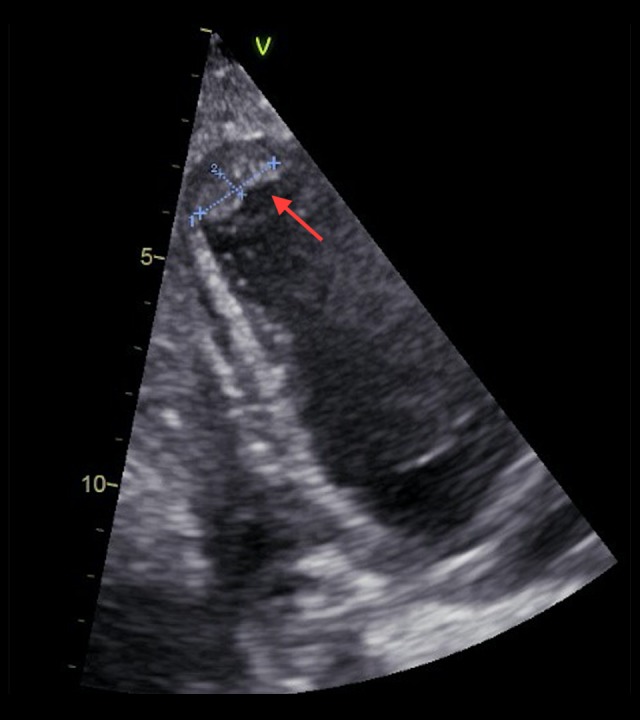
Transthoracic echocardiography (2-chamber-view) showing left ventricular apical akinesia with thrombus. GE E80 Ultrasound System.
Figure 5.
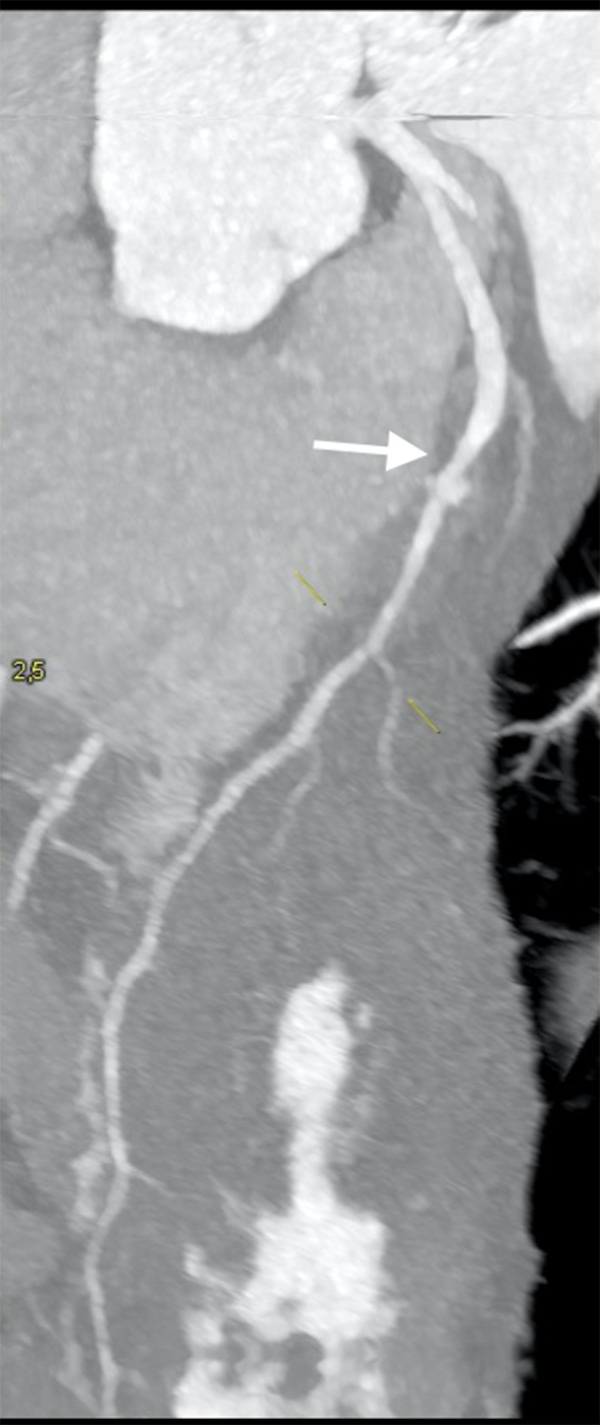
High resolution computer tomography image demonstrating left anterior descending dissection involving diagonal branches. Siemens SOMATOM High Definition AS.
Figure 6.
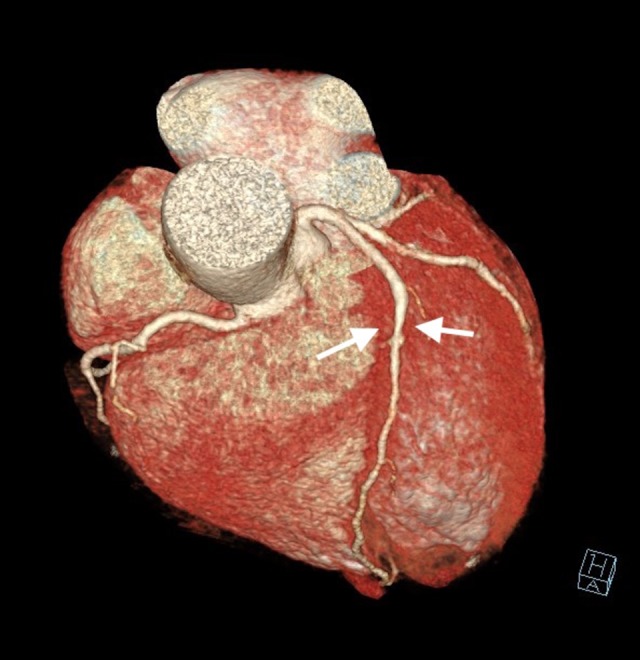
Computed tomography 3D-reconstruction demonstrating left anterior descending dissection involving diagonal branches. Siemens SOMATOM High Definition AS. Electrocardiography at admission.
Anticoagulation and anti-inflammatory therapy were started.
At discharge, after 30 days of hospital stay, the echocardiogram still showed moderate impairment of left ventricular systolic function (ejection fraction 45%) with akinesia of the anterior septum and of the apex, apical ventricular thrombus, and mild circumferential pericardial effusion.
One month later, the patient underwent a new study, revealing disappearance not only of the apical thrombus and the pericardial effusion, but also of the dissection of the entire LAD. At clinical evaluation, the patient reported improvement of symptoms (NYHA functional class I). Anticoagulation therapy was discontinued, even though the classical heart failure therapy was continued.
Discussion
SCAD is defined as a spontaneous separation of the coronary artery wall, not iatrogenic nor related to trauma or atherosclerotic disease [3].
Two mechanisms for arterial wall separation in SCAD have been proposed. The first hypothesizes a tear in the inner layer of the vessel wall, with the formation of a false lumen. The second is thought to be due to the rupture of the vasa vasorum, creating an intramural hematoma. Accumulation of blood within the false lumen can compress the true lumen to varying degrees; anterograde and retrograde propagation may occur and be extensive, because of the weakening of the arterial wall architecture [4–6]. Several underlying predisposing conditions have been associated with SCAD such as systemic inflammatory diseases and connective tissue disorders. The most frequently reported is fibromuscular dysplasia [7–9].
During pregnancy, hormonal and hemodynamic changes may predispose a woman to SCAD.
High progesterone levels weaken the arterial media through alteration of the elastic fiber and mucopolysaccharide content, and impairment of collagen synthesis. Estrogens create a hypercoagulable state. Augmented cardiac output and circulatory volume increase shear stress, causing microstructural changes in vessels [10–12]. Multiple pregnancies may lead to chronic repetitive impairment of arterial wall integrity. Indeed, multiparous or multigravida women are at higher risk for SCAD [13,14].
Moreover, Valsalva-like increases in thoraco-abdominal pressure (such as the pregnant status) are known to be precipitating stressors which can trigger SCAD [8,13,15–17].
The true prevalence of SCAD in the general population is unknown due to significant under-diagnosis of this condition, although in recent case series, routine coronary angiography in patients presenting with ACS and a more diffuse availability and application of high-resolution intracoronary imaging resulted in an increase of diagnosis of up to 4% of ACS patients [18–22].
SCAD affects women in >90% of cases, with mean age ranging from 44 years to 55 years of age [7,8,23–26]. Although accounting for less than 5% of all SCAD cases [8,26,27], it is the most common cause of myocardial infarction in pregnant women, being diagnosed in more than 40% of pregnancy-associated myocardial infarction. P-SCAD occurs predominantly in the third trimester of pregnancy or in the first post-partum phase [7,21,25].
P-SCADs have been reported to have a more severe clinical presentation with frequent multivessel involvement [28]. Even long-term prognosis appears to be worse than non pregnancy-related SCAD (NP-SCAD), due to larger infarcts and lower discharge mean left ventricular ejection fraction [29].
We presented a case of P-SCAD occurring in a patient at the 37th week of pregnancy. She did not present any cardiovascular risk factor nor conditions predisposing to SCAD, except for pregnancy. During the first episode, she was hemodynamically stable, and the dissection was small and involved only the distal LAD. The case was then complicated by an early recurrence with extensive LAD dissection and left ventricular thrombus, but still the patient was stable and there was only a moderate impairment of the left ventricular systolic function.
The peculiarity of our case is that despite a benign presentation, not requiring any coronary intervention, early fetal distress occurred causing concern over the condition of the unborn infant.
In P-SCAD cases needing revascularization strategies, cesarean delivery is recommended before any other intervention [30]. Generally, in SCAD, revascularization is limited to cases of hemodynamical instability or involvement of left main coronary artery. Percutaneous coronary intervention and coronary artery bypass graft have both been used, but not routinely performed because of frequent occurrence of intervention failures or iatrogenic complications. Moreover, SCAD is known to self-heal in most cases [8,18,23,27,31–34]. Current opinion is that for cases of SCAD of larger proximal-mid arteries, an imaging follow-up (mostly with cardiac CT, a less invasive alternative to angiography) is recommended given the high-rate of self-healing of this condition [3]. Indeed, at 1-month follow-up for our patient, the dissection resolved spontaneously.
Our patient did not show characteristics requiring interventions. The multidisciplinary team considered that, given the maternal clinical circumstance and the time of pregnancy, an urgent cesarean delivery was the safest option. Indeed, the patient was hemodynamically stable but her clinical course could not be predicted with absolute accuracy, and might have become severe, as after an acute myocardial infarction. Notably, she suffered an early recurrence of SCAD, and we cannot exclude that if the delivery was not undertaken, that the infant outcome would have been good as well.
To our knowledge, only one case of cesarean delivery in a Cath-Lab has been previously reported [35]. As for our case, it was not complicated, and the infant had a good clinical course. A multidisciplinary team composed of cardiologists, anesthetists, gynecologists, and an hemodynamist participated in the management of the patient. Collaboration among different specialties experts made possible the cesarean delivery and its good result in this unordinary setting of acute cardiovascular scenario.
Conclusions
Careful evaluation of this delicate condition is needed and active collaboration among specialty experts is advised to promptly assess and manage complicated conditions. Even in cases with a benign presentation, there may be major concern for the fetal status. Under accurate circumstances, cesarean deliveries may be performed in a Cath-Lab after coronary catheterization if needed, with optimal results.
Abbreviations:
- ACS
acute coronary syndrome;
- Cath-Lab
catheterization laboratory;
- CT
computed tomography;
- LAD
left anterior descending;
- NP-SCAD
non pregnancy-related SCAD;
- P-SCAD
peripartum spontaneous coronary artery dissection;
- SCAD
spontaneous coronary artery dissection
References:
- 1.Tweet MS, Hayes SN, Pitta SR, et al. Clinical features, management, and prognosis of spontaneous coronary artery dissection. Circulation. 2012;126:579–88. doi: 10.1161/CIRCULATIONAHA.112.105718. [DOI] [PubMed] [Google Scholar]
- 2.Elkayam U, Jalnapurkar S, Barakkat MN, et al. Pregnancy-associated acute myocardial infarction: A review of contemporary experience in 150 cases between 2006 and 2011. Circulation. 2014;129:1695–702. doi: 10.1161/CIRCULATIONAHA.113.002054. [DOI] [PubMed] [Google Scholar]
- 3.Saw J, Mancini GBJ, Humphries KH. Contemporary review on spontaneous coronary artery dissection. J Am Coll Cardiol. 2016;68(3):297–312. doi: 10.1016/j.jacc.2016.05.034. [DOI] [PubMed] [Google Scholar]
- 4.Maehara A, Mintz GS, Castagna MT, et al. Intravascular ultrasound assessment of spontaneous coronary artery dissection. Am J Cardiol. 2002;89:466–68. doi: 10.1016/s0002-9149(01)02272-x. [DOI] [PubMed] [Google Scholar]
- 5.Isner JM, Donaldson RF, Fortin AH, et al. Attenuation of the media of coronary arteries in advanced atherosclerosis. Am J Cardiol. 1986;58:937–39. doi: 10.1016/s0002-9149(86)80015-7. [DOI] [PubMed] [Google Scholar]
- 6.Saw J, Mancini GB, Humphries K, et al. Angiographic appearance of spontaneous coronary artery dissection with intramural hematoma proven on intracoronary imaging. Catheter Cardiovasc Interv. 2016;87:E54–61. doi: 10.1002/ccd.26022. [DOI] [PubMed] [Google Scholar]
- 7.Saw J, Ricci D, Starovoytov A, et al. Spontaneous coronary artery dissection: Prevalence of predisposing conditions including fibromuscular dysplasia in a tertiary center cohort. J Am Coll Cardiol Intv. 2013;6:44–52. doi: 10.1016/j.jcin.2012.08.017. [DOI] [PubMed] [Google Scholar]
- 8.Saw J, Aymong E, Sedlak T, et al. Spontaneous coronary artery dissection: Association with predisposing arteriopathies and precipitating stressors and cardiovascular outcomes. Circ Cardiovasc Interv. 2014;7:645–55. doi: 10.1161/CIRCINTERVENTIONS.114.001760. [DOI] [PubMed] [Google Scholar]
- 9.Kamran M, Guptan A, Bogal M. Spontaneous coronary artery dissection: Case series and review. J Invasive Cardiol. 2008;20:553–59. [PubMed] [Google Scholar]
- 10.Yip A, Saw J. Spontaneous coronary artery dissection – a review. Cardiovasc Diagn Ther. 2015;5:37–48. doi: 10.3978/j.issn.2223-3652.2015.01.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sheikh AS, O’Sullivan M. Pregnancy-related spontaneous coronary artery dissection: Two case reports and a comprehensive review of literature. Heart Views. 2012;13:53–65. doi: 10.4103/1995-705X.99229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Manalo-Estrella P, Barker AE. Histopathologic findings in human aortic media associated with pregnancy. Archiv Pathol. 1967;83:336–41. [PubMed] [Google Scholar]
- 13.Vijayaraghavan R, Verma S, Gupta N, et al. Pregnancy-related spontaneous coronary artery dissection. Circulation. 2014;130:1915–20. doi: 10.1161/CIRCULATIONAHA.114.011422. [DOI] [PubMed] [Google Scholar]
- 14.Koller PT, Cliffe CM, Ridley DJ. Immunosuppressive therapy for peripartum-type spontaneous coronary artery dissection: Case report and review. Clin Cardiol. 1998;21:40–46. doi: 10.1002/clc.4960210108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lempereur M, Grewal J, Saw J. Spontaneous coronary artery dissection associated with b-HCG injections and fibromuscular dysplasia. Can J Cardiol. 2014;30:464.e1–3. doi: 10.1016/j.cjca.2013.11.030. [DOI] [PubMed] [Google Scholar]
- 16.Sivam S, Yozghatlian V, Dentice R, et al. Spontaneous coronary artery dissection associated with coughing. J Cyst Fibros. 2014;13:235–37. doi: 10.1016/j.jcf.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 17.Keir ML, Dehghani P. Corticosteroids and spontaneous coronary artery dissection: A new predisposing factor? Can J Cardiol. 2016;32:395.e7–8. doi: 10.1016/j.cjca.2015.06.021. [DOI] [PubMed] [Google Scholar]
- 18.Saw J. Spontaneous coronary artery dissection. Can J Cardiol. 2013;29:1027–33. doi: 10.1016/j.cjca.2012.12.018. [DOI] [PubMed] [Google Scholar]
- 19.Vrints CJ. Spontaneous coronary artery dissection. Heart. 2010;96:801–8. doi: 10.1136/hrt.2008.162073. [DOI] [PubMed] [Google Scholar]
- 20.Poon K, Bell B, Raffel OC, et al. Spontaneous coronary artery dissection: Utility of intravascular ultrasound and optical coherence tomography during percutaneous coronary intervention. Circ Cardiovasc Interv. 2011;4:e5–7. doi: 10.1161/CIRCINTERVENTIONS.110.959593. [DOI] [PubMed] [Google Scholar]
- 21.Rashid HN, Wong DT, Wijesekera H, et al. Incidence and characterisation of spontaneous coronary artery dissection as a cause of acute coronary syndrome – a single-centre Australian experience. Int J Cardiol. 2016;202:336–38. doi: 10.1016/j.ijcard.2015.09.072. [DOI] [PubMed] [Google Scholar]
- 22.Nishiguchi T, Tanaka A, Ozaki Y, et al. Prevalence of spontaneous coronary artery dissection in patients with acute coronary syndrome. Eur Heart J Acute Cardiovasc Care. 2016;5:263–70. doi: 10.1177/2048872613504310. [DOI] [PubMed] [Google Scholar]
- 23.Tweet MS, Eleid MF, Best PJ, et al. Spontaneous coronary artery dissection: Revascularization versus conservative therapy. Circ Cardiovasc Interv. 2014;7:777–86. doi: 10.1161/CIRCINTERVENTIONS.114.001659. [DOI] [PubMed] [Google Scholar]
- 24.Roura G, Ariza-Solé A, Rodriguez-Caballero IF, et al. Noninvasive follow-up of patients with spontaneous coronary artery dissection with CT angiography. JACC Cardiovasc Imaging. 2016;9(7):896–97. doi: 10.1016/j.jcmg.2015.06.011. [DOI] [PubMed] [Google Scholar]
- 25.Nakashima T, Noguchi T, Haruta S, et al. Prognostic impact of spontaneous coronary artery dissection in young female patients with acute myocardial infarction: A report from the Angina Pectoris-Myocardial Infarction Multicenter Investigators in Japan. Int J Cardiol. 2016;207:341–48. doi: 10.1016/j.ijcard.2016.01.188. [DOI] [PubMed] [Google Scholar]
- 26.Rogowski S, Maeder MT, Weilenmann D, et al. Spontaneous coronary artery dissection: Angiographic follow-up and long-term clinical outcome in a predominantly medically treated population. Catheter Cardiovasc Interv. 2017;89(1):59–68. doi: 10.1002/ccd.26383. [DOI] [PubMed] [Google Scholar]
- 27.Alfonso F, Paulo M, Lennie V, et al. Spontaneous coronary artery dissection: long-term follow-up of a large series of patients prospectively managed with a “conservative” therapeutic strategy. JACC Cardiovasc Interv. 2012;5(10):1062–70. doi: 10.1016/j.jcin.2012.06.014. [DOI] [PubMed] [Google Scholar]
- 28.Tweet MS, Hayes SN, Codsi E, et al. Spontaneous coronary artery dissection associated with pregnancy. J Am Coll Cardiol. 2017;70(4):426–35. doi: 10.1016/j.jacc.2017.05.055. [DOI] [PubMed] [Google Scholar]
- 29.Ito H, Taylor L, Bowman M, et al. Presentation and therapy of spontaneous coronary artery dissection and comparisons of postpartum versus nonpost-partum cases. Am J Cardiol. 2011;107:1590–66. doi: 10.1016/j.amjcard.2011.01.043. [DOI] [PubMed] [Google Scholar]
- 30.Havakuk O, Goland S, Mehra A, et al. Pregnancy and the risk of spontaneous coronary artery dissection: An analysis of 120 contemporary cases. Circ Cardiovasc Interv. 2017;10(3):e004941. doi: 10.1161/CIRCINTERVENTIONS.117.004941. pii. [DOI] [PubMed] [Google Scholar]
- 31.Lettieri C, Zavalloni D, Rossini R, et al. Management and long-term prognosis of spontaneous coronary artery dissection. Am J Cardiol. 2015;116:66–73. doi: 10.1016/j.amjcard.2015.03.039. [DOI] [PubMed] [Google Scholar]
- 32.Lempereur M, Fung A, Saw J. Stent malapposition with resorption of intramural hematoma with spontaneous coronary artery dissection. Cardiovasc Diagn Ther. 2015;5:323–29. doi: 10.3978/j.issn.2223-3652.2015.04.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Prakash R, Starovoytov A, Heydari M, et al. TCT-386: Iatrogenic catheter-induced dissection during angiography of patients with spontaneous coronary artery dissection. J Am Coll Cardiol. 2015;66(Suppl. B):B155–56. [Google Scholar]
- 34.Walsh SJ, Jokhi PP, Saw J. Successful per- cutaneous management of coronary dissection and extensive intramural haematoma associated with ST elevation MI. Acute Card Care. 2008;10:231–33. doi: 10.1080/17482940701802348. [DOI] [PubMed] [Google Scholar]
- 35.Sundaram V, Chaudhry SP, Reddy YN, et al. Emergent cesarean section in the catheterization laboratory for spontaneous coronary artery dissection. Am J Cardiol. 2015;115(12):1777–78. doi: 10.1016/j.amjcard.2015.03.027. [DOI] [PubMed] [Google Scholar]


