Abstract
Background
Malaria is a leading cause of paediatric morbidity and mortality in Uganda. More than half of febrile children in rural areas initially seek care at private clinics and drug shops. These shops are generally unregulated and the quality of clinical care is variable, with the potential for misdiagnosis and the development of drug resistance. There is thus an urgent need to identify rural drug shops and coordinate their malaria treatment efforts with those of the public sector. The objective of the study was to identify all drug shops in the Bugoye sub-county of Western Uganda and assess their anti-malarial dispensing practices.
Methods
This study is a cross-sectional survey of drug shops in a rural sub-county of Western Uganda. In the first phase, shop locations, licensing and shopkeeper’s qualifications, and supply and pricing of anti-malarials were characterized. In the second phase, the proportion of anti-malarials dispensed by private drug shops was compared to public health facilities.
Results
A total of 48 drug shops were identified. Only one drug shop (1 of 48, 2%) was licensed with the sub-county’s records office. The drug shops stocked a variety of anti-malarials, including first-line therapies and less effective agents (e.g., sulfadoxine/pyrimethamine). Almost all drug shops (45 of 48, 94%) provided parenteral anti-malarials. Of the 3900 individuals who received anti-malarials during the study, 2080 (53.3%) purchased anti-malarials through the private sector compared to 1820 (46.7%) who obtained anti-malarials through the public sector. Drug shops were the primary source of parenteral anti-malarials. Inadequate dosing of anti-malarials was more common in drug shops.
Conclusions
Drug shops are major sources of parenteral anti-malarials, which should be reserved for cases of severe malaria. Strengthening malaria case management and incorporating drug shops in future interventions is necessary to optimize malaria control efforts in the sub-county, and in similarly endemic regions.
Electronic supplementary material
The online version of this article (10.1186/s12936-018-2454-7) contains supplementary material, which is available to authorized users.
Keywords: Malaria, Health-seeking behaviors, Private sector, Anti-malarials, Parenteral drugs
Background
Approximately 30–50% of outpatient visits to public healthcare facilities in Uganda are related to malaria, which remains a leading cause of paediatric morbidity and mortality [1, 2]. However, the private sector is also an important source of anti-malarials in rural Uganda, where geographic factors such as distance to health centres and weak transportation networks can limit access to medical care [2–6]. More than half of febrile children in rural areas initially seek care at private drug shops, which are often unregistered, unregulated, and operated by individuals with limited formal clinical training [7–13]. A census of drug shops in rural Uganda found that 77% were unlicensed [8] and a national survey that tracked anti-malarial dispensation in Uganda’s private sector found that 20.0% of drug shops sold parenteral anti-malarials, a practice that is contrary to the policies of Uganda’s Ministry of Health [14].
Drug shops have also been found to market expired and/or ineffective anti-malarials despite the availability of efficacious first-line therapies, a practice that may result in adverse clinical outcomes [15–18]. One study found that licensed rural drug shops provided appropriate malaria treatments to only 10% of febrile children [7], and another study demonstrated that initially seeking care at a drug shop was a significant risk factor for severe malaria in Ugandan children [19]. These factors contribute to the highly variable quality of malaria case management in drug shops [7, 17, 19–22].
Drug shops do have several advantages compared to public facilities, especially in a rural context. They are generally more accessible due to their proximity to village population centres, shorter waiting times, and more flexible hours of operation. They are also less prone to drug stock-outs [23–27]. When provided with training in basic case management practices, drug shops increased patient access to appropriate care [10, 28, 29]. Thus, there is an urgent need to identify rural drug shops, evaluate current practices, and coordinate malaria treatment efforts with national guidelines and priorities.
This study was a cross-sectional survey examining the characteristics of drug shops in Bugoye sub-county, a rural area of highland western Uganda whose private sector has never been assessed. The objective of the study was to identify all drug shops in the sub-county and assess their anti-malarial dispensing practices in comparison to neighboring public health facilities.
Methods
Study setting
The study was conducted in Bugoye sub-county, Kasese District, Western Uganda (Fig. 1). The highland terrain, with elevations ranging from 1000 to 1800 m, is home to approximately 35,000 residents [30, 31]. Bugoye’s climate allows for year-round malaria transmission interspersed with semi-annual transmission peaks after the rainy seasons [30]. Recent surveys suggest that malaria transmission in the region is declining, evidenced by a parasite prevalence of 48.4% in 2009 compared to 17.6% in 2014 [2, 32]. Bugoye sub-county’s health system is divided into public and private health facilities.
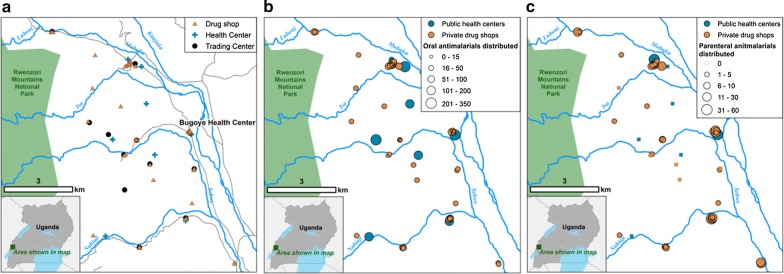
Fig. 1.
Map depicting the locations of public sector health centres and private sector drug shops in Bugoye sub-county (a), with number of patients receiving oral anti-malarials during the study period (b), and number of patients receiving parenteral anti-malarials during the study period (c)
Public health facilities
The sub-county’s primary public health facility is the Bugoye Level III health centre (BHC), which houses an inpatient ward where parenteral medications are administered, an outpatient ward where oral medications are dispensed, and a laboratory that conducts point-of-care diagnostics including malaria rapid diagnostic tests (RDTs) and light microscopy. There are Level II Health Centres in each of the six parishes that offer basic outpatient services. There are two community health workers termed village health teams (VHTs) in each of the sub-county’s 36 villages that are trained in integrated community case management (iCCM), perform RDTs, and dispense oral medications to children < 5 years of age suffering from uncomplicated pneumonia, diarrhoea, and malaria [33]. There is one public–private Level III Health Centre operated jointly by the Ugandan Ministry of Health and the Rwenzori Mountaineering Services (RMS), which houses a public outpatient ward and a private inpatient ward that provide services comparable to BHC. Remote villages were defined as those at least 3 km from BHC.
Private health facilities
To our knowledge, drug shops (i.e., privately owned small businesses that sell pharmaceutical products) comprise the entirety of the sub-county’s private health facilities.
Study design
This study was a two-phase, cross-sectional survey of drug shops in Bugoye sub-county. In the first phase, shop locations, self-reported licensing status and shopkeeper’s qualifications, and supply and pricing of anti-malarials were recorded. In the second phase, the number of anti-malarials dispensed by private drug shops was compared to public health facilities.
Phase 1: initial survey of drug shops
The locations of shops in the sub-county were identified with the assistance of local leaders and VHTs. Study staff visited all villages at least twice to ensure that no shops were missed. At the initial visit, the following information was collected on a questionnaire (Additional file 1): the village and shop names, GIS coordinates, self-reported licensing status, and shopkeeper’s credentials. The following information was recorded for each anti-malarial available at a shop: the drug’s trade name, manufacturer’s country of origin, formulation and route of administration, price for an adult and paediatric course (in Ugandan shillings), expiration date, and the shop’s current drug supply. Study staff also determined the availability and cost of malaria RDTs and asked about the shop’s primary resupply source. The names of shops that claimed to be licensed were compared to a list of licensed drug shops maintained by BHC.
Phase 2: tracking anti-malarial dispensation in drug shops and health centres
After completing the initial visit questionnaire, a form was provided to each shopkeeper (Additional file 2) along with instructions to record anti-malarial sales for 1 month beginning on 1 August 2017. For every anti-malarial sold, shopkeepers recorded the following information: date of sale, the purchaser’s gender, age, and village of residence, the drug name, units dispensed (recorded in tablets/bottles/ampules), and the remaining stock. Shopkeepers were instructed to return the questionnaire to BHC after 31 August 2017.
Over the same period, the following information on anti-malarial dispensation was extracted from the clinical registers of all public health facilities in the sub-county: date of encounter, patient’s gender, age, village of residence, and type and dose of anti-malarial dispensed. Records of children < 5 years of age seen by VHTs conducting integrated management of childhood illness (IMCI) were collated separately by BHC staff and shared with study staff. Anti-malarial tracking forms were not provided to public facilities as records were abstracted from existing registers.
Anti-malarial drug courses
The definition of a course of anti-malarials was based on WHO guidelines [34]. For example, a course of oral artemether/lumefantrine (AL) for an adult > 35 kg consists of 24 tablets (each containing 20 mg artemether and 120 mg lumefantrine), with 4 tablets as a single initial dose, followed by 4 tablets after 8 h, then 4 tablets twice a day (AM and PM) for the following 2 days. For an adult > 35 kg, a course of parenteral artesunate consists of six 60 mg ampules reconstituted in 5% sodium bicarbonate and diluted in 5% (w/v) glucose. A loading dose of 2 mg/kg is followed by 1 mg/kg after 4 and 24 h; subsequently, a dose of 1 mg/kg is given daily until the patient can tolerate oral therapy [34].
Statistical analysis
Data were entered into Microsoft Excel, version 15.33 (Microsoft, Redmond, WA) and analyzed with Stata, version 15.1 (Stata Corp., College Station, TX). A map of all health facilities was created using ArcGIS, version 10.4.1 (ESRI, Redlands, CA). The level of owner credentialing and self-reported licensing status with the sub-county’s records office were summarized, along with the availability, formulation, manufacturing origin, and median cost of each anti-malarial.
We employed common statistical tests to (1) compare patient populations receiving anti-malarials between the public and private sector, (2) explore the accuracy of AL dosing between the public and private sector, and (3) assess for significant differences in the rate of parenteral anti-malarial administration across the private sector. The demographic characteristics of patients presenting to private versus public health facilities were compared using Wilcoxon Rank Sum test for continuous variables (i.e., age) and Pearson’s Chi squared test for categorical variables.
The frequency of inadequate AL dose administration was explored in two groups: adults (defined as individuals ≥ 21 years of age with a weight assumed to be > 35 kg) and children (≤ 5 years of age with a weight assumed to be < 15 kg). AL was selected as a proxy for inadequate dosing because it is both the first-line therapy for uncomplicated malaria and the most commonly prescribed anti-malarial in the sub-county. Inadequate dosing was defined as the dispensation of < 6 AL tablets for children ≤ 5 years of age and < 24 tablets for adults ≥ 21 years of age. The proportion of inadequate dosing was compared between private and public facilities using Pearson’s Chi squared test.
Differences in the relative odds of parenteral anti-malarial administration across drug shops were examined using Poisson regression models. The outcome of interest was the route of administration (i.e., parenteral vs. oral) and the primary explanatory variable was individual drug shops, with BHC serving as the reference. Models were adjusted for age and reported as odds ratios (OR). For all statistical analyses, a resulting p-value of ≤ 0.05 was considered significant.
Results
Phase 1: initial survey of drug shops
Licensing and shopkeeper’s qualifications
A total of 48 drug shops were identified (Fig. 1a) and all shopkeepers consented to participate in the study. Only one shop (1 of 48, 2.1%) was licensed with the sub-county’s records office. Some shops (16 of 48, 33%) had more than one shopkeeper; most (48 of 67, 72%) identified themselves as nursing assistants, which in Uganda qualifies one to dispense medications under supervision.
Supply and pricing of anti-malarials
The drug shops stocked a variety of anti-malarials (Table 1). Nearly all shops (47 of 48, 98.0%) stocked AL at a median cost of $1.11 (IQR 1.11–1.28) for an adult course of 24 tablets. Quinine was available in tablet (43 of 48, 90%), syrup (48 of 48, 100%), and parenteral forms (45 of 48, 94%). Older agents like sulfadoxine/pyrimethamine (SP) that are no longer considered effective for the treatment of uncomplicated malaria [35] were also available in drug shop (42 of 48, 88.0%). In general, parenteral anti-malarials were more expensive, with an adult course of 6 ampules of parenteral artesunate (median cost $13.33, IQR 13.33–13.33) being the most expensive treatment. None of the anti-malarials examined on the initial visit were expired. All shops reported restocking supplies from pharmacies in Kasese Town, approximately 20 km to the south. All shops offered malaria RDTs for a median cost of $0.56 (IQR $0.56–$0.83).
Table 1.
Anti-malarial drugs available in drug shops in Bugoye sub-county
| Drug name | Formulation | Adult coursesa | Costb (median, IQR) | Drug shops (n, %) |
|---|---|---|---|---|
| Oral formulations | ||||
| Amodiaquine | Tablet | 9.5 (6 tablets) | 2.08 (1.46–2.78) | 6/48 (13) |
| Artemether | Tablet | 0 (12 tablets) | 1.81 (1.32–2.78) | 2/48 (4) |
| Artemether/lumefantrine | Tablet | 316.8 (24 tablets) | 1.11 (1.11–1.28) | 47/48 (98) |
| Chloroquine | Tablet | 6.1 (10 tablets) | 1.11 (0.83–1.11) | 4/48 (8) |
| Dihydroartemisinin/piperaquine | Tablet | 15.6 (9 tablets) | 4.17 (4.17–6.94) | 7/48 (15) |
| Quinine | Syrup | 99 (1 bottle) | 1.11 (1.11–1.39) | 48/48 (100) |
| Quinine | Tablet | 31.7 (30 tablets) | 2.50 (2.08–2.50) | 43/48 (90) |
| Sulfadoxine/pyrimethamine | Tablet | 243.8 (3 tablets) | 0.42 (0.42–0.54) | 42/48 (88) |
| Parenteral formulations | ||||
| Artemether | Parenteral | 6.5 (6 ampules) | 4.58 (3.13–8.33) | 9/48 (19) |
| Artesunate | Parenteral | 13.8 (6 ampules) | 13.33 (13.33–13.33) | 22/48 (46) |
| Quinine | Parenteral | 60.7 (3 ampules) | 8.06 (5.56–8.33) | 45/48 (94) |
aNumber (and definition) of adult courses available in all drug shops
bCost in US dollars of a single adult course of specified anti-malarial
Phase 2: tracking anti-malarial dispensation in drug shops and health centres
Completed tracking forms were received from all 48 drug shops. Of the 3900 individuals who received anti-malarials from private and public facilities during the study period, 2080 (53.3%) received anti-malarials through private facilities compared to 1820 (46.7%) who received anti-malarials through public facilities. Nearly all care on the weekends (503 of 515, 97.7%, Table 2) was provided by drug shops. Health centres were the primary source of AL, while drug shops dispensed more doses of every other type of anti-malarial, including less efficacious therapies such as SP and chloroquine (Table 3). All patients who received anti-malarials from a health centre had a positive RDT.
Table 2.
Demographic characteristics of patients in the public and private sectors
| Public health centresa | Drug shopsb | p-value | |
|---|---|---|---|
| Patients (n, %) | 1531 (39.3) | 2080 (53.3) | – |
| Female (n, %) | 877 (57.3) | 1063 (53.3) | 0.018 |
| Age (median, IQR) | 16 (9–27) | 19 (9–30) | 0.004d |
| Age category (n, %) (years) | |||
| < 5 | 166 (10.9) | 306 (14.8) | < 0.001 |
| 5–12 | 366 (24.1) | 320 (15.5) | |
| > 12 | 989 (65.0) | 1443 (69.7) | |
| Villages with health centre | 685 (44.8) | 923 (44.7) | 0.97 |
| Remote villagesc | 295 (19.3) | 486 (23.6) | 0.002 |
| Weekend | 12 (0.8) | 503 (25.6) | < 0.001 |
aExcludes 289 (7.4%) patients < 5 years of age treated by VHTs
bIncludes the 45 patients seen at the private RMS Level III Health Centre
cDefined as villages at least 3 km from the Bugoye Level III Health Centre
dProbability obtained by comparison of medians using Mann–Whitney two sample test
Table 3.
Number of patients treated in the public sector versus the private sector
| Formulation | Anti-malarial | Patients treatedb (n, %) | |
|---|---|---|---|
| Public sector 1820 (46.7) |
Private sector 2080 (53.3) |
||
| Tablets | Amodiaquine | 0 | 0 |
| Artemether | 0 | 5 (0.2) | |
| Artemether/lumefantrine | 1715 (94.2) | 1029 (49.5) | |
| Chloroquine | 0 | 3 (0.1) | |
| Dihydroartemisinin/piperaquine | 0 | 19 (0.9) | |
| Quinine | 2 (0.1) | 169 (8.1) | |
| Sulfadoxine/pyrimethamine | 96 (5.3) | 341 (16.4) | |
| Parenteral | Artemether | 0 | 31 (1.5) |
| Artesunate | 47 (2.6) | 73 (3.5) | |
| Quinine | 12 (0.7) | 285 (13.7) | |
| Syrup | Quinine | 0 | 164 (7.9) |
| Rectal | Artesunate | 7 (0.4)a | 0 |
aAll seven individuals were children < 5 years of age treated by VHTs
bThe aggregate number of patients treated is less than the numbers reported in the table because some patients received more than one type of anti-malarial
Geographic characteristics of drug shops
Most shops distributing anti-malarials were located within 1 km of a health centre (Fig. 1b, c). Individuals from villages with a health centre were equally as likely to obtain anti-malarials from a drug shop as those from villages without a health centre (AOR 1.00, 95% CI 0.88–1.15, p = 0.97, Table 2). Conversely, individuals from remote villages furthest from BHC were more likely to obtain anti-malarials from drug shops (AOR 1.28, 95% CI 1.09–1.51, p = 0.002, Table 2).
Patient characteristics
Individuals receiving all types of anti-malarials from drug shops were slightly older than those that received all types of anti-malarials through health centres (median age 19 vs. 16 years, p = 0.004, Table 2). One half of individuals (165 of 329, 50.2%) treated with SP in drug shops were male, suggesting that intermittent treatment of malaria in pregnancy (IPTp) was not the rationale for selecting SP.
Parenteral anti-malarial dispensation
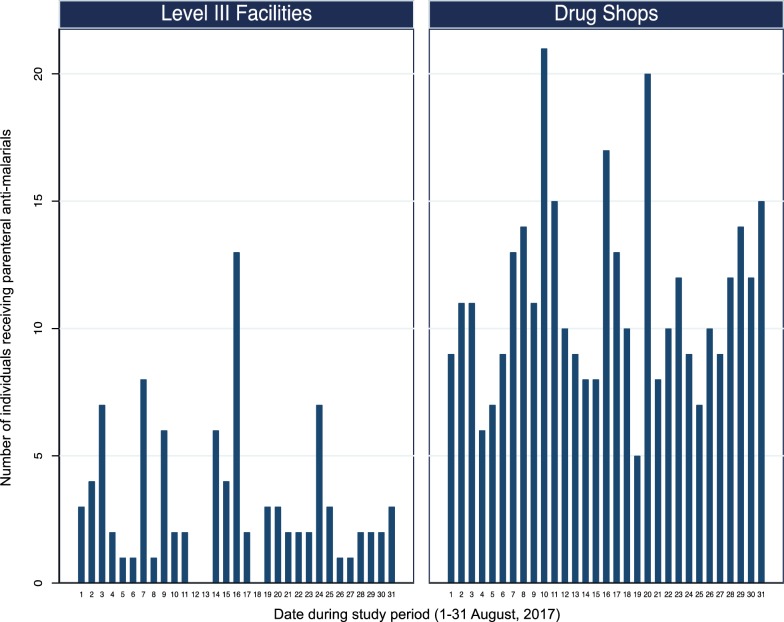
59 of 299 (19.7%) individuals treated for malaria at BHC received parenteral anti-malarials, consisting of either artesunate (47 of 59, 79.7%) or quinine (12 of 59, 20.3%). An additional 36 of 45 (80.0%) patients treated in the private inpatient ward of the RMS health centre received parenteral anti-malarials. All patients who received a course of parenteral anti-malarials at a Level III health centre also received a course of oral anti-malarials. Together, these two Level III facilities accounted for only 95 of the 448 (21.2%) individuals that received parenteral anti-malarials over the study period (Fig. 2).
Fig. 2.
Number of individuals receiving parenteral anti-malarial therapy at the Bugoye Level III Health Centre compared to private sector drug shops during the study period (1–31 August 2017)
In contrast, drug shops accounted for 353 of the 448 (78.8%) individuals that received parenteral anti-malarials over the study period (Fig. 2). The administration of parenteral anti-malarials in drug shops was common practice (Fig. 1c), with most shops (40 of 48, 83.4%) dispensing parenteral anti-malarials to at least one person over the study period. Quinine was the most frequently sold parenteral anti-malarial (251 of 353, 71.7%), followed by artesunate (71 of 353, 20.1%) and artemether (31 of 353, 8.9%). None of the patients who purchased parenteral anti-malarials from a shop purchased a concomitant course of oral anti-malarials. Five drug shops (5 of 48, 10.4%) accounted for 37.7% of individuals treated with parenteral anti-malarials in the private sector.
In the regression analysis, receiving care at drug shops was associated with significantly higher odds of parenteral anti-malarial use (AOR 5.05, 95% CI 3.80–6.72, p < 0.001) compared to BHC. At eight shops, the odds of parenteral anti-malarial sales were significantly higher (p < 0.05) or trended higher (p < 0.1) than that observed at BHC. Together, these eight shops accounted for 31.3% of individuals treated with parenteral anti-malarials in both the public and private sectors. Of these eight shops, four were in trading centres adjacent to BHC and two were near RMS.
Individuals receiving parenteral treatment in drug shops were on average 7.8 years older than those receiving treatment at BHC (22.7 vs. 15.0 years, p < 0.001). Similarly, children < 5 years of age presented less frequently to drug shops compared to BHC to receive parenteral therapy (30.8% vs. 69.2%, p < 0.001). There were no significant differences by gender.
Inadequate AL dosing in drug shops
Inadequate AL dosing among children was not observed in health centres (0 of 137 cases, 0.0%). However, inadequate AL dosing was relatively frequent in drug shops (11 of 94 cases, 11.7%). Inadequate AL dosing among adults was also more common at drug shops (65 of 410 cases, 15.9%) compared to health centres (8 of 526 cases, 1.5%, p < 0.001). There was no significant difference in the age of adults between private and public facilities (p = 0.80) that might explain the difference in AL dosing. Furthermore, adult women (who may weigh less than the 35-kg threshold for a 24 tablet AL course) comprised a higher, albeit non-significant, proportion of attendees at public compared to private health facilities (57.2 vs. 52.4, p = 0.14), which makes this unlikely to explain the observed differences.
Discussion
This study demonstrates that private sector drug shops are not only significant distributors of anti-malarials in a rural area of western Uganda, but also a major source of parenteral anti-malarials. Although Uganda’s National Drug Authority does not authorize drug shops to dispense parenteral medications, a 2015 national survey found that 20.0% of drug shops sold parenteral quinine and 10.9% sold parenteral artemether. Ultimately, 8.7% of patients received non-artemisinin therapies (i.e., parenteral/tablet/syrup quinine, SP tablets, or chloroquine tablets) and 3.9% of patients received an artemisinin monotherapy (i.e., parenteral artemether) during the national survey’s data collection period [14]. The present study found that both the percentage of drug shops selling parenteral anti-malarials and the percentage of patients receiving parenteral anti-malarials were greater than previously reported. Even shops located near Level III facilities had high rates of parenteral anti-malarial sales, indicating a strong preference for seeking care in the private sector.
Several factors may account for increased utilization of drug shops in Bugoye sub-county. Long wait times at public health facilities, coupled with the convenience of seeking care in drug shops, likely led to increased acquisition of parenteral anti-malarials through the private sector. Patients may believe that parenteral anti-malarials are more efficacious than oral formulations, a perception that has been shown in other countries [36]. Furthermore, this study found that older patients were not only more likely to seek care in drug shops, but also more likely to purchase parenteral anti-malarials without an accompanying course of oral anti-malarials. On the other hand, paediatric patients were less likely to present to a shop and receive parenteral therapy. This could be because parents, concerned that their child might be suffering from severe malaria, seek formal treatment from a public facility staffed by more qualified personnel.
These results have important public health implications. In terms of patient safety, the dispensation of parenteral anti-malarials in drug shops raises concerns about safety practices, management of adverse drug effects, and possible dispensation of counterfeit drugs. In particular, parenteral quinine can have dangerous adverse effects if improperly administered. In terms of anti-malarial stewardship, all drug shops dispensed a course of parenteral anti-malarials without a concomitant course of oral anti-malarials, a practice that can lead to the development of drug resistance. Additionally, previous studies have found that initially seeking care at drug shops was a significant risk factor for severe malaria in Ugandan children, likely due to their provision of sub-optimal treatments and resultant disease progression [19, 37].
Several approaches could be taken to address these complex issues. A ban on parenteral anti-malarial dispensation in drug shops could be enforced, but may push sales further underground, where they will be even more difficult to regulate. Another option is a harm reduction approach, which could include more training for shopkeepers and more rigorous enforcement of licensing and RDT usage. The results of our analysis indicate that targeting a few high-volume drug shops could have an exponential impact on malaria case control.
This study has several methodological strengths, including its rigorous field practices identifying drug shops and its high response rate. This study also has some limitations. First, the data was drawn from clinic records in public facilities and from self-reported records in drug shops whose accuracy were not assessed. However, the rate of completeness was high and there is no reason to believe there were systemic issues in reporting. Second, study staff did not interview customers and thus can only speculate on the motivations driving their care-seeking behaviors. These behaviors can be examined in future qualitative studies. Third, this study did not track the degree of overlapping patient utilization of the public and private sector. Finally, RDT utilization in drug shops was not assessed and it is unknown whether the 2080 individuals that received anti-malarials through the private sector actually had clinical malaria. Regardless, these limitations do not diminish the striking finding that the majority of parenteral anti-malarials were dispensed through private drug shops.
Conclusions
Private sector drug shops in Bugoye sub-county distributed more than half of all anti-malarials during the study period and were the primary source of parenteral anti-malarials. There were several risks associated with seeking care in drug shops, including higher rates of inadequate anti-malarial dosing. Further studies are needed to assess the potential risks and benefits of incorporating drug shops as stakeholders in malaria case management in Uganda.
Additional files
Additional file 1. Initial visit questionnaire.
Additional file 2. Anti-malarial sales tracking form.
Authors’ contributions
LW and RMB designed the study, collected the data, and drafted the manuscript. RB and RM helped collect the data. CK helped with mapping. MN, EM, RR, and RS helped draft the manuscript. All authors read and approved the final manuscript.
Acknowledgements
We thank the drug shopkeepers in Bugoye sub-county for participating in the study and the clinical staff at BHC who supported the study. We also thank Drs. Jonathan Juliano and Steve Meshnick, who read drafts of the manuscript and provided constructive feedback.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets supporting the conclusions of this article are available on reasonable request from the authors.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Ethical approval was provided by the institutional review boards of the University of North Carolina, Chapel Hill and the Mbarara University of Science and Technology. Shopkeepers provided verbal consent to participate in the study. Individual informed written consent was not required due to the programmatic nature of data collection and retrospective review of data.
Funding
LW’s participation was funded by the Global Health Academic Concentration and the Global Health Institute (University of California, San Diego). RMB receives support from the National Institutes of Health (T32 AI007151). RS receives support from the National Institutes of Health (K23 MH111409).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Yeka A, Gasasira A, Mpimbaza A, Achan J, Nankabirwa J, Nsobya S, et al. Malaria in Uganda: challenges to control on the long road to elimination: I. Epidemiology and current control efforts. Acta Trop. 2012;121:184–195. doi: 10.1016/j.actatropica.2011.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Uganda Bureau of Statistics. Uganda Malaria Indicator Survey 2014–15. https://dhsprogram.com/pubs/pdf/MIS21/MIS21.pdf. Accessed 12 Nov 2017.
- 3.Ministry of Health. Health Sector Strategic Plan III 2010/11–2014/15. Kampala, Republic of Uganda. http://www.health.go.ug/docs/HSSP_III_2010.pdf. Accessed 12 Nov 2017.
- 4.United Nations Industrial Development Organization. Pharmaceutical Sector Profile: Uganda. http://www.unido.org/fileadmin/user_media/ Services/PSD/BEP/Uganda%20Pharma%20Sector%20Profile_TEGLO05015_ Ebook_.pdf. Accessed 12 Nov 2017.
- 5.Ministry of Health. Report on updating of the 3 year rolling procurement plan for essential medicines and health supplies 2009/10–2011/12 including evaluation of 2008/2009. Kampala, Republic of Uganda. http://www.health.go.ug/docs/Report_April.pdf. Accessed 12 Nov 2017.
- 6.Lankowski AJ, Siedner MJ, Bangsberg DR, Tsai AC. Impact of geographic and transportation-related barriers on HIV outcomes in sub-Saharan Africa: a systematic review. AIDS Behav. 2014;18:1199–1223. doi: 10.1007/s10461-014-0729-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Awor P, Wamani H, Bwire G, Jagoe G, Peterson S. Private sector drug shops in integrated community case management of malaria, pneumonia, and diarrhea in children in Uganda. Am J Trop Med Hyg. 2012;87(5 Suppl):92–96. doi: 10.4269/ajtmh.2012.11-0791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Konde-Lule J, Gitta SN, Lindfors A, Okuonzi S, Onama VO, Forsberg BC. Private and public health care in rural areas of Uganda. BMC Int Health Hum Rights. 2010;10:29. doi: 10.1186/1472-698X-10-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rutebemberwa E, Pariyo G, Peterson S, Tomson G, Kallander K. Utilization of public or private health care providers by febrile children after user fee removal in Uganda. Malar J. 2009;8:45. doi: 10.1186/1475-2875-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Awor P, Wamani H, Tylleskar T, Jagoe G, Peterson S. Increased access to care and appropriateness of treatment at private sector drug shops with integrated management of malaria, pneumonia and diarrhoea: a quasi-experimental study in Uganda. PLoS ONE. 2014;9:e115440. doi: 10.1371/journal.pone.0115440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liow E, Kassam R, Sekiwunga R. Investigating unlicensed retail drug vendors’ preparedness and knowledge about malaria: an exploratory study in rural Uganda. Acta Trop. 2017;174:9–18. doi: 10.1016/j.actatropica.2017.06.008. [DOI] [PubMed] [Google Scholar]
- 12.Graham SM, English M, Hazir T, Enarson P, Duke T. Challenges to improving case management of childhood pneumonia at health facilities in resource-limited settings. Bull World Health Organ. 2008;86:349–355. doi: 10.2471/BLT.07.048512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buregyeya E, Rutebemberwa E, LaRussa P, Lal S, Clarke SE, Hansen KS, et al. Comparison of the capacity between public and private health facilities to manage under-five children with febrile illnesses in Uganda. Malar J. 2017;16:183. doi: 10.1186/s12936-017-1842-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaula H, Buyungo P, Opigo J. Private sector role, readiness and performance for malaria case management in Uganda, 2015. Malar J. 2017;16:219. doi: 10.1186/s12936-017-1824-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goodman C, Brieger W, Unwin A, Mills A, Meek S, Greer G. Medicine sellers and malaria treatment in sub-Saharan Africa: what do they do and how can their practice be improved? Am J Trop Med Hyg. 2007;77(6 Suppl):203–218. [PMC free article] [PubMed] [Google Scholar]
- 16.Ndyomugyenyi R, Neema S, Magnussen P. The use of formal and informal services for antenatal care and malaria treatment in rural Uganda. Health Policy Plan. 1998;13:94–102. doi: 10.1093/heapol/13.1.94. [DOI] [PubMed] [Google Scholar]
- 17.Wafula FN, Miriti EM, Goodman CA. Examining characteristics, knowledge and regulatory practices of specialized drug shops in sub-Saharan Africa: a systematic review of the literature. BMC Health Serv Res. 2012;12:223. doi: 10.1186/1472-6963-12-223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sudhinaraset M, Ingram M, Lofthouse HK, Montagu D. What is the role of informal healthcare providers in developing countries? A systematic review. PLoS One. 2013;8:e54978. doi: 10.1371/journal.pone.0054978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mpimbaza A, Ndeezi G, Katahoire A, Rosenthal PJ, Karamagi C. Demographic, socioeconomic, and geographic factors leading to severe malaria and delayed care seeking in Ugandan children: a case-control study. Am J Trop Med Hyg. 2017;97:1512–1523. doi: 10.4269/ajtmh.17-0056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tawfik Y, Nsungwa-Sabitii J, Greer G, Owor J, Kesande R, Prysor-Jones S. Negotiating improved case management of childhood illness with formal and informal private practitioners in Uganda. Trop Med Int Health. 2006;11:967–973. doi: 10.1111/j.1365-3156.2006.01622.x. [DOI] [PubMed] [Google Scholar]
- 21.Smith F. The quality of private pharmacy services in low and middle-income countries: a systematic review. Pharm World Sci. 2009;31:351–361. doi: 10.1007/s11096-009-9294-z. [DOI] [PubMed] [Google Scholar]
- 22.Bryce J, Victora CG. MCE-IMCI Technical Advisors. Ten methodological lessons from the multi-country evaluation of integrated Management of Childhood Illness. Health Policy Plan. 2005;20(Suppl 1):i94–i105. doi: 10.1093/heapol/czi056. [DOI] [PubMed] [Google Scholar]
- 23.Akol A, Chin-Quee D, Wamala-Mucheri P, Namwebya JH, Mercer SJ, Stanback J. Getting closer to people: family planning provision by drug shops in Uganda. Glob Health Sci Pract. 2014;2:472–481. doi: 10.9745/GHSP-D-14-00085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Williams HAHA, Jones COH. A critical review of behavioral issues related to malaria control in sub-Saharan Africa: what contributions have social scientists made? Soc Sci Med. 1982;2004(59):501–523. doi: 10.1016/j.socscimed.2003.11.010. [DOI] [PubMed] [Google Scholar]
- 25.Amin AA, Marsh V, Noor AM, Ochola SA, Snow RW. The use of formal and informal curative services in the management of paediatric fevers in four districts in Kenya. Trop Med Int Health. 2003;8:1143–1152. doi: 10.1046/j.1360-2276.2003.01140.x. [DOI] [PubMed] [Google Scholar]
- 26.Mills A, Brugha R, Hanson K, McPake B. What can be done about the private health sector in low-income countries? Bull World Health Organ. 2002;80:325–330. [PMC free article] [PubMed] [Google Scholar]
- 27.Mbonye AK, Bygbjerg IC, Magnussen P. Prevention and treatment practices and implications for malaria control in Mukono District Uganda. J Biosoc Sci. 2008;40:283–296. doi: 10.1017/S0021932007002398. [DOI] [PubMed] [Google Scholar]
- 28.Kitutu FE, Kalyango JN, Mayora C, Selling KE, Peterson S, Wamani H. Integrated community case management by drug sellers influences appropriate treatment of paediatric febrile illness in South Western Uganda: a quasi-experimental study. Malar J. 2017;16:425. doi: 10.1186/s12936-017-2072-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Awor P, Wamani H, Tylleskar T, Peterson S. Drug seller adherence to clinical protocols with integrated management of malaria, pneumonia and diarrhoea at drug shops in Uganda. Malar J. 2015;14:277. doi: 10.1186/s12936-015-0798-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Boyce R, Reyes R, Ntaro M, Mulogo E, Matte M, Boum Y, et al. Association between HRP-2/pLDH rapid diagnostic test band positivity and malaria-related anemia at a peripheral health facility in Western Uganda. J Glob Health. 2015;5:020402. doi: 10.7189/jogh.05.020402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Uganda Bureau of Statistics. National Population and Housing Census 2014 Sub-county Report, Uganda Western Region. http://www.ubos.org/onlinefiles/uploads/ubos/census_2014_regional_reports/revised/NPHC%202014-Subcounty%20Profile-Western%20Region-Final%2023MArch2017.pdf. Accessed 12 Nov 2017.
- 32.Uganda Bureau of Statistics. Uganda Malaria Indicator Survey 2009. https://dhsprogram.com/pubs/pdf/MIS6/MIS6.pdf. Accessed 12 Nov 2017.
- 33.English L, Miller JS, Mbusa R, Matte M, Kenney J, Bwambale S, et al. Monitoring iCCM referral systems: Bugoye Integrated Community Case Management Initiative (BIMI) in Uganda. Malar J. 2016;15:247. doi: 10.1186/s12936-016-1300-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.WHO. Guidelines for the treatment of malaria. 3rd ed. Geneva: World Health Organization; 2015. hpps.who.int/iris/bitstream/10665/162441/1/9789241549127_eng.pdf. Accessed 1 Aug 2018.
- 35.Nabyonga-Orem J, Ssengooba F, Macq J, Criel B. Malaria treatment policy change in Uganda: what role did evidence play? Malar J. 2014;13:345. doi: 10.1186/1475-2875-13-345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sundararajan R, Kalkonde Y, Gokhale C, Greenough PG, Bang A. Barriers to malaria control among marginalized tribal communities: a qualitative study. PLoS ONE. 2013;8:e81966. doi: 10.1371/journal.pone.0081966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sundararajan R, Mwanga-Amumpaire J, Adrama H, Tumuhairwe J, Mbabazi S, Mworozi K, et al. Sociocultural and structural factors contributing to delays in treatment for children with severe malaria: a qualitative study in southwestern Uganda. Am J Trop Med Hyg. 2015;92:933–940. doi: 10.4269/ajtmh.14-0784. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Initial visit questionnaire.
Additional file 2. Anti-malarial sales tracking form.
Data Availability Statement
The datasets supporting the conclusions of this article are available on reasonable request from the authors.