Abstract
Purpose:
We investigated the impact of elements of a workplace culture of health (COH) on employees’ perceptions of employer support for health and lifestyle risk.
Design:
We used 2013 and 2015 survey data from the National Healthy Worksite Program, a Centers for Disease Control and Prevention (CDC)-led initiative to help workplaces implement health-promoting interventions.
Setting:
Forty-one employers completed the CDC Worksite Health Scorecard to document organizational changes.
Participants:
Eight hundred twenty-five employees provided data to evaluate changes in their health and attitudes.
Measures:
We defined elements of a COH as environmental, policy, and programmatic supports; leadership and coworker support; employee engagement (motivational interventions); and strategic communication. Outcomes included scores of employees’ perceptions of employer support for health and lifestyle risk derived from self-reported physical activity, nutrition, and tobacco use.
Analysis:
We estimated effects using multilevel regression models.
Results:
At the employee level and across time, regression coefficients show positive associations between leadership support, coworker support, employee engagement, and perceived support for health (P < .05). Coefficients suggest a marginally significant negative association between lifestyle risk and the presence of environmental and policy supports (P < .10) and significant associations with leadership support in 2015 only (P < .05).
Conclusion:
Relational elements of COH (leadership and coworker support) tend to be associated with perceived support for health, while workplace elements (environmental and policy supports) are more associated with lifestyle risk. Employers need to confront relational and workplace elements together to build a COH.
Keywords: culture of health, workplace health promotion, workplace interventions, perceived support, lifestyle risk
Purpose
Over the past several decades, employers have increasingly established worksite-based health promotion programs (WHPPs) to reduce rising health-care costs, attract and retain talent, and improve employees’ quality of life.1 Worksite-based health promotion programs typically entail an assessment of employee health, personalized feedback on how employees can improve their health, and the provision of resources and programming designed to promote wellness.2 Evidence suggests WHPPs yield positive outcomes for employers and employees when properly executed.3,4 Worksite-based health promotion programs lead employees to adopt healthier behaviors, reduce rates of chronic disease, control employers’ health-care spending, and minimize absenteeism.2,5–8
As WHPPs continue to grow in popularity, researchers stress that employers must be realistic about the outcomes they can expect from their WHPPs.3 Employers should not simply introduce random interventions and expect improvements in health outcomes or cost reductions.3 Instead, they must strive to build a culture of health (COH)—an environment that “places value on and is conducive to employee health and well-being.”9(p17) As the name implies, a concern for employee health must permeate all aspects of an organization and its corporate identity.10
The literature points to several elements of the workplace COH as important, although it is unclear which elements are most essential for improving employee outcomes. One of the most frequently cited elements is strong leadership support throughout the organization.1 Senior managers’ roles entail creating the vision and values of an organization and allocating resources for organizational activities.10–12 Their positions give them power to prioritize employee well-being and ensure resources, such as providing and sustaining budgets and staffing for WHPPs.9 Successful WHPPs exhibit significant leadership participation and engagement,13 which was described as “critical” to effective programming by a National Institute of Occupational Safety and Health committee comprised of WHPP experts.14 Middle managers also play a key role in establishing a COH, as they serve as the face of the organization among many employees.14,15 Middle managers act as gatekeepers, communicating organizational values in the level of concern they demonstrate for their staff and the opportunities and encouragement they provide for employees to engage in health-promoting behavior, such as physical activity classes or stress management.9
Coworker support may shape employee health behavior and perceptions of organizational support for health. Coworkers further encourage healthy behavior or conversely can contribute to performance pressures that threaten health.16 For instance, research suggests exercise and nutritional behaviors of coworkers are associated with employees’ own behaviors.17,18 Employees’ relationships with coworkers also provide social support, which is associated with healthy lifestyles.19
In addition to social support, workplace supports reflect an organization’s investment in a COH. Perhaps, most basically, workplaces can offer information or tools at key decisionmaking points that help employees adopt healthy behaviors. Such environmental supports include labeling healthy food options in cafeterias and vending machines, posting signs that encourage workers to take the stairs instead of the elevator, and providing or subsidizing fitness facilities and equipment.1,7,9,20 Environmental supports can be buttressed with programmatic supports that help engage workers in health-promoting activities after assessing their health needs.2,4 Such activities include health screenings, educational sessions, and self-management programs designed to encourage healthy lifestyles. Employers can also show their commitment to wellness by employing policy supports, such as enforcing a tobacco-free campus. Policy supports tell employees that wellness is a significant concern for employers. Research suggests that best practices for WHPPs are integrated into organizational missions and business practices, reflected in organizational goals, and tied to health coverage policies and related discounts in premiums.1,13
Finally, a COH cannot be established without efforts to engage employees. Employee engagement is achieved when employees participate in and take ownership of WHPPs. Engagement can be encouraged with incentives, competitions, and participation in wellness planning.9,10,12,14 Organizations with strong WHPPs market their programs and make them relevant to employees’ needs through strategic communication.4,14 Strategic communication builds employee enthusiasm through personal success stories, tailored messaging to reach specific segments of the workforce, and using champions who advocate for the program.9,12,20
Culture of health advocates stress that worker involvement in WHPPs depends on workers’ belief that their employers care about their well-being.9 Social scientists have explained this belief with the concept of perceived organizational support.15,21 If employees think their employer is only interested in reducing staff health-care costs, they may feel resentful and not participate in the WHPP.22,23 If, on the other hand, workers think their employers genuinely care about their health and well-being, employees will feel more motivated to participate and adopt behaviors that benefit them and the organization at large.9 Research is limited on worker health and perceived organizational support,21 but some evidence hints at an association. For instance, in a study of hospital workers, Lemon and colleagues found that greater perceived support for health was associated with lower body mass index, improved nutrition, and increased physical activity.17
More research is needed to identify the essential elements of a COH for improving employee outcomes,3 particularly outcomes most closely associated with well-being and quality of life. This article contributes to the literature by investigating the following research questions:
Are organizational elements of a COH associated with perceived organizational support for health and lifestyle risk?
If so, which organizational elements of a COH are most strongly associated with perceived organizational support and lifestyle risk?
Based on the literature, we hypothesized that all elements of the COH would have a direct, positive effect on perceived organizational support for health and a negative effect on lifestyle risk among employees who participated in Centers for Disease Control and Prevention’s (CDC)’s National Healthy Worksite Program (NHWP). Because managers have the greatest power to define organizational culture, the authors predicted that leadership support would be more strongly associated with perceived organizational support for health and lifestyle risk than other elements of the COH.24
Methods
Design
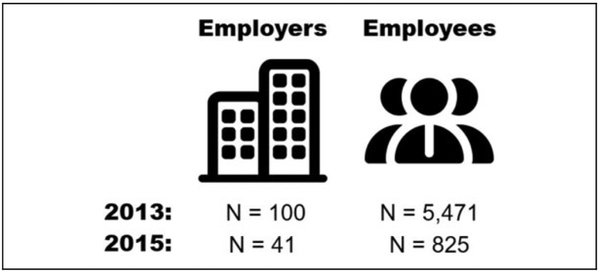
Data were collected in 2013 and 2015 as part of the evaluation of the CDC’s NHWP.25 The program was designed to help 100 participating employers from 8 communities in the United States carry out interventions to reduce rates of chronic disease. CDC recruited employers based on county- level outcomes and risk factor data, access to community resources and organizations, local health disparities, and diversity with respect to urban/rural locality, industry, and employee demographics. Participation required employers to evaluate their health promotion offerings and target highimpact strategies to improve those offerings using CDC’s Worksite Health ScoreCard (hereafter HSC), a publicly accessible assessment tool (see https://www.cdc.gov/workplacehealthpromotion/initiatives/healthscorecard/index.html). CDC supported employers who committed to improving their programs using training and technical assistance. In addition to employer-level data collection, 5741 employees from participating employers completed baseline biometric screenings and surveys on their health status and behavior. From this original sample, 41 (41%) employers and 825 (14.3%) employees completed follow-up data collection 18 months after baseline (see Figure 1). We have restricted the data for this article to include only those employers and employees with data at both time points to evaluate relationships before and after employers developed their WHPPs. Among these 41 employers, we also ran a sensitivity analysis to determine whether the relationships identified at baseline differed between the employees with data at both time points and the employees who participated at baseline only (N = 1760; see Appendix A).
Figure 1.
Study Design. Icons made by Freepik from www.flaticon.com.
Sample
RTI International’s institutional review board reviewed the study and deemed it exempt from institutional review because it was categorized as a program evaluation. Employees gave their informed consent to participate before providing responses to each data collection instrument. Table 1 provides descriptive data on the employers who participated in data collection at both baseline (2013) and follow-up (2015). As shown, most employers (n ¼ 29) had fewer than 250 workers. Employers were spread across different counties and regions, with most in Kern County, California (n = 9), Marion County, Indiana (n = 8), and Philadelphia County, Pennsylvania (n = 8). Although similarly diverse with respect to industry, most of the employers were in health care and social assistance (n = 14) or finance, insurance, and real estate (n = 11).
Table 1.
Size, Location, and Industry of Employers Participating in Baseline (2013) and Follow-Up (2015) Data Collection (N = 41).
| n | |
|---|---|
| Employer size | |
| 1–49 | 7 |
| 50–99 | 8 |
| 100–249 | 14 |
| 250–499 | 8 |
| 500+ | 4 |
| Community/county | |
| Buchanan, Missouri (St Joseph) | 5 |
| Harris, Texas (Houston) | 1 |
| Kern, California (Bakersfield) | 9 |
| Marion, Indiana (Indianapolis) | 8 |
| Philadelphia, Pennsylvania (Philadelphia) | 8 |
| Pierce, Washington (Tacoma) | 6 |
| Shelby, Tennessee (Memphis) | 4 |
| Industry sector | |
| Health care and social assistance | 14 |
| Finance, insurance, and real estate | 11 |
| Manufacturing | 5 |
| Public administration | 4 |
| Professional, scientific, and technical services | 3 |
| Retail and wholesale | 1 |
| Construction | 1 |
| Other | 2 |
Table 2 displays employee characteristics at follow-up (2015). Employees had a mean age of 46.9 years. The majority were female (73.9%), white (76.2%), and non-Hispanic (91.4%). Just over half (57.8%) of the employees were college graduates. In 2015, a little more than half (54.0%) of the participants had no supervisory responsibility, 18.4% had team leader or supervisory roles, and 27.6% had managerial or executive positions.
Table 2.
Characteristics of Employees Participating in Baseline (2013) and Follow-Up (2015) Data Collection (N = 825) at Follow-Up.
| Mean/% (SD) | |
|---|---|
| Mean age (SD) | 46.9(11.9) |
| % Female | 73.9 |
| Race | |
| % Asian | 4.9 |
| % Black/African American | 15.8 |
| % White | 76.2 |
| % Other/multiracial | 3.0 |
| % Hispanic ethnicity | 8.6 |
| Education | |
| % High school or less | 11.0 |
| % Some college | 31.2 |
| % College degree or higher | 57.8 |
| Organizational role | |
| % No supervisory responsibility | 54.0 |
| % Team leader/supervisor | 18.4 |
| % Manager/executive | 27.6 |
Abbreviation: SD, standard deviation.
Measures
Key elements include employer and employee measures of the COH as shown in Table 3. We defined these elements using the scholarly literature and CDC definitions26 as follows: Environmental supports are structural and physical factors at and near the work site that help protect and improve employee health by making healthyoptions available. Policy supports reflect worksite policies, statements, and elements of the compensation package that promote employee health. Programmatic supports include opportunities and supports, such as assessments and health education activities, promoted by the work site that assist employees to begin, change, or maintain healthy behaviors. Leadership support captures supervisory and managerial investment in employee health, whereas coworker support is affirming coworker relationships, including concern for colleague’s health. Employee engagement is efforts, such as incentives and team competitions that motivate workers to participate in WHPPs. Finally, strategic communication includes marketing strategies and messages to support health promotion programs.
Table 3.
Elements of the Workplace Culture of Health.a
| Environmental supports: structural and physical factors at and near the work site that help improve employee health by making healthy options available | |
Employer-level (HSC) measures:
|
|
| Policy supports: work-site policies, statements, and elements of the compensation package that promote employee health | |
Employer-level (HSC) measures:
|
|
| Programmatic supports: opportunities and supports promoted by the work site that assist employees to begin, change, or maintain health behaviors | |
Employer-level (HSC) measures:
|
|
| Leadership support: supervisory and managerial concern for employee health | |
Employer-level (HSC) measures:
|
Employee-level (self-perception) measures:
|
| Coworker support: establishment of affirming coworker relationships, including concern for colleagues’ health | |
Employer-level (HSC) measure:
|
Employee-level (self-perception) measures:
|
| Employee engagement: an organization’s efforts to motivate workers to take advantage of health-promoting resources and programming | |
Employer-level (HSC) measures:
|
Employee-level (self-perception) measure:
|
| Strategic communication: Communication and messaging designed to market program offerings | |
Employer-level (HSC) measures:
|
|
Abbreviation: HSC, Health ScoreCard.
Items abbreviated for display purposes.
Measures for environmental, policy, programmatic supports, and strategic communication are assessed at the employer level using only the HSC. In contrast, leadership support, coworker support, and employee engagement are measured at employer and employee levels using the HSC and employee surveys. Original measures of each element were standardized and averaged to compute a score. Higher scores reflect stronger evidence of each element, whereas lower scores reflect weaker evidence.
Outcomes examined include employee perceptions of organizational support for health and lifestyle risk. We determined perceptions of organizational support using a single employee rating ranging from 1 (extremely unsupportive) to 10 (extremely supportive). Lifestyle risk was also measured at the employee level, using an algorithm that accounts for participants’ self-reported nutrition, physical activity, and tobacco use (see Table 4). For nutrition, participants received between 0 and 10 points depending on whether their consumption of fried food, fruit, vegetables, whole grains, and nondiet soda met dietary guidelines for individuals of their sex, age, and physical activity level.27 Participants received 2 points for eating at least the minimum recommended servings of fruit, vegetables, and whole grains per week. Participants could also receive 2 points each for consuming little or no fried food and nondiet soda. For physical activity, participants received 0 to 10 points depending on how many minutes they were active, with more minutes corresponding to higher points. Participants received final lifestyle risk assignments of low, moderate, or high based on their total nutrition and physical activity points. If participants reported tobacco use, they automatically received a designation of high risk.
Table 4.
Lifestyle Risk Components, Indicators, Recommendations, and Scoring.
| Component/Risk Indicator | Recommendation | Scoring |
|---|---|---|
| Nutritiona | ||
| Fried food | ≤ 160–320 calories/week | 2 points |
| Fruit | ≥ 10.5–17.5 servings/week | 2 points |
| Vegetables | ≥ 14–28 servings/week | 2 points |
| Whole grains | ≥ 21–56 servings/week | 2 points |
| Nondiet soda | Less than 1 serving/week | 2 points |
| Moderate physical activityb | 150 minutes/week | |
| 1–29 minutes | 2 points | |
| 30–149 minutes | 4 points | |
| 150–199 minutes | 6 points | |
| 200–299 minutes | 8 points | |
| >300 minutes | 10 points | |
| Tobacco use | No tobacco use | High risk if any use |
| Lifestyle risk | - | |
| High | Take action | ≤ 5 total points or any tobacco use |
| Medium | Improve on | 6–14 total points |
| Low | Doing well | ≥ 15 total points |
Based on 2010 US dietary guidelines that depend on sex, age, and physical activity level.27
We standardized time spent engaging in physical activity of different intensities as follows: minutes of high-intensity activity ¼ minutes of moderate-intensity activity times 2. Adults aged 18 to 64 need 150 minutes of moderate intensity physical activity or 75 minutes of high-intensity physical activity per week.28
Analysis
Multilevel models were used to investigate associations between elements of the COH and perceived support and lifestyle risk. Multilevel models allow us to explain variation in employee outcomes using parameters assessed at different levels: employer attributes and employee perceptions. Employer effects capture the associations between culture and the average perceived support or lifestyle risk in a workplace. Employee effects reveal how much of the remaining variation—the deviation of individual workers from the average for the workplace—can be explained by the employee-level measures. Since environmental, policy, programmatic supports, and strategic communication contain employer measures only, there is no remaining employee variation in our predictors after the employer effects have been estimated. Thus, we estimate only employer effects for these 4 elements.
Multilevel modeling is uncommon in research on WHPPs (for an exception, see Terry et al29) but offers advantages over single-level modeling approaches. First, the use of multilevel modeling allows us to statistically link employees who share an employer. Acknowledging that employees of the same employer share more in common than employees spread across different employers is important. Regression techniques otherwise assume observations are independent. Violating the independence assumption heightens the risk for a type I error (ie, the researcher is more likely to infer an effect is significant when, in reality, it is not). Second, multilevel models prevent us from losing employee-level variation that would result from combining employee results. Employee variation is important to consider when examining the COH, as large differences among employees may themselves suggest fragmented efforts to develop a health-promoting culture.24
Third, estimating employer and employee effects empowers researchers, employers, and policy makers to make better decisions about what types of interventions are most likely to be effective for improving employee outcomes. Significant employer effects without corresponding employee effects suggest organizational initiatives may improve employee outcomes across a range of workers. But if effects are statistically significant among employees only, then specific types of workers (or work groups) may exhibit different outcomes, despite the presence of similar organizational interventions. If both types of effects are significant, employers may want to introduce universal investments in a COH while also making investments that target specific work groups.
We considered both employee- and employer-level controls. Since earlier studies indicate that workers’ responses to WHP interventions vary with worker characteristics,18,28 we controlled employee-level variables including age, gender, race, ethnicity, educational attainment, and hierarchical level in the company. Previous research also suggests small- and mediumsized organizations often struggle to implement and maintain WHPPs that are comprehensive enough to support changes in employee attitudes and behaviors, while other employer characteristics, for example, industry type, have less influence.30–32 Thus, we controlled for only 1 employer-level variable, namely, size, classified as small, medium, or large employer.
All analyses were conducted in SAS version 9.4 using proc mixed. Models employed maximum likelihood estimation, and fixed effects are reported. We show 2 sets of results for each outcome: estimates at baseline (2013) and estimates at follow-up (2015). The models are identical except that the baseline outcome is included as a covariate in the models predicting the outcome at follow-up. We also discuss the findings of our sensitivity analysis, which assessed employees from the 41 employers who participated in both baseline and follow-up. The sensitivity analysis allows us to investigate whether the relationships we identified at baseline differed between the employees with data at both time points and employees who participated at baseline only.
Results
Table 5 provides descriptive data on outcomes at baseline (2013) and follow-up (2015). Perceived organizational support did not change between baseline and follow-up, with a mean rating of 7.8 out of 10 at both time points. Lifestyle risk, however, improved significantly (P < .001) between 2013 and 2015. The proportion of participants assessed as high risk dropped from 57.0% to 43.2%, participants assessed as moderate risk increased from 38.4% to 49.7%, and participants assessed as low risk increased from 4.6% to 7.2%. Improvements in lifestyle risk were expected because of employers’ participation in the NHWP.
Table 5.
Descriptive Data for Outcomes Perceived Organizational Support for Health and Lifestyle Risk at Baseline (2013) and Follow-Up (2015) (N = 825).
| 2013% | 2015% | |
|---|---|---|
| Perceived organizational support for health | ||
| 1: Extremely unsupportive | 1.1 | 0.7 |
| 2 | 0.8 | 1.7 |
| 3 | 2.7 | 2.2 |
| 4 | 1.5 | 1.7 |
| 5 | 9.0 | 9.7 |
| 6 | 7.5 | 7.9 |
| 7 | 13.5 | 13.6 |
| 8 | 21.3 | 18.7 |
| 9 | 18.6 | 18.1 |
| 10: Extremely supportive | 24.1 | 25.5 |
| Mean (SD) | 7.8 (2.0) | 7.8(2.1) |
| Lifestyle risk | ||
| High | 57.0 | 43.2 |
| Medium | 38.4 | 49.7 |
| Low | 4.6 | 7.2 |
Abbreviation: SD, standard deviation.
Table 6 displays the results from models predicting perceived organizational support for health, first using baseline (2013) data and then using follow-up (2015) data. At baseline, we find statistically significant relationships (P < .05) between 4 of the 7 elements of culture and perceived support: leadership support, coworker support, employee engagement, and strategic communication. Consistent with our hypotheses, perceived support is positively associated with employer-level strategic communication, employee-level leadership support, and employee-level coworker support. Also, as expected, employee-level leadership support has a larger effect on perceived support than the other elements of culture. Inconsistent with our hypotheses, however, we find statistically significant negative relationships between leadership support and employee engagement at the employer level. Recall that employer-level effects can be thought of as representing how, across employers, average perceptions of culture relate to average levels of perceived support. The negative employer-level effects thus suggest that, across organizations, high levels of leadership support and employee engagement tend to co-occur with relatively low levels of perceived support for health. In contrast, employee-level effects help explain why individual employees’ perceptions of support vary within an organization. Our findings indicate that employees who reported the greatest leadership support and employee engagement within each employer’s workforce did, in fact, perceive greater support for their health. We offer possible explanations in the discussion section.
Table 6.
Perceived Organizational Support for Health Regressed on Elements of a Culture at Health, at Baseline (2013) and Follow-Up (2015).a
| 2013 (n = 765) | 2015 (n = 759) | |||
|---|---|---|---|---|
| Predictor | Estimate | P Value | Estimate | P Value |
| Intercept | 6.002 | <.001 | 4.618 | <.001 |
| Employer-level (HSC) measures | ||||
| Environmental supports | 0.049 | .899 | −0.083 | .760 |
| Policy supports | −0.526 | .138 | −0.338 | .252 |
| Programmatic supports | −0.138 | .561 | −0.025 | .932 |
| Leadership support | −1.738 | .002 | −0.541 | .241 |
| Coworker support | 0.211 | .568 | −0.330 | .356 |
| Employee engagement | −1.984 | .015 | −2.599 | <.001 |
| Strategic communication | 0.642 | .002 | −0.153 | .331 |
| Employee-level (self-perception) measures | ||||
| Leadership support | 3.305 | <.001 | 2.071 | <.001 |
| Coworker support | 0.422 | .009 | 0.385 | .004 |
| Employee engagement | 1.229 | .078 | 2.328 | <.001 |
| Employee & organizational characteristics | ||||
| Age | 0.009 | .085 | 0.007 | .158 |
| Male | 0.071 | .630 | 0.061 | .668 |
| Hispanic ethnicity | 0.229 | .368 | 0.085 | .750 |
| Race: black/African-American | 0.204 | .280 | 0.146 | .413 |
| Race: Asian | 0.576 | .038 | 0.328 | .216 |
| Race: other/multiracial | 0.672 | .024 | 0.312 | .344 |
| Education: less than high school | 0.276 | .185 | 0.253 | .221 |
| Education: some college | 0.056 | .686 | 0.324 | .017 |
| Hierarchical level: no supervisory authority | 0.406 | .006 | −0.102 | .474 |
| Hierarchical level: supervisory authority | 0.335 | .081 | −0.065 | .712 |
| Organization size: small | 0.953 | .003 | 0.007 | .158 |
| Organization size: mid | 0.768 | .010 | 0.061 | .668 |
| Baseline perceived organizational support for health | - | - | 0.316 | <.001 |
Abbreviation: HSC, Health ScoreCard.
Effects with P values less than .05 are set in bold type, and those with P values between 0.05 and 0.10 are italicized.
At follow-up (2015), employee-level perceived leadership support, coworker support, and employee engagement remain statistically significant predictors of perceived organizational support for health, whereas the effect for strategic communications was no longer significant. Both leadership and coworker support have significant positive effects among employees (P < .001 and P ¼ .004, respectively), which is consistent with hypotheses. As with the baseline models, however, the effects for employee engagement differ for employers and employees, with a negative employer association, and a positive employee association. Also, contrary to expectations, at the employee level, the employee engagement effect (2.328) is larger in magnitude than that for leadership support (2.071).
With respect to our control variables, relative to white race participants, Asian, and other race/multiracial participants perceive greater support at baseline (2013) only (P = .038 and P = .024, respectively). Participants with no supervisory responsibilities and those with some supervisory authority likewise perceive greater organizational support for their health than managers and executives at baseline only (P = .006 and P = .081, respectively). Participants with some college perceive greater support for their health than the college educated, just at follow-up (P = .017). Significant effects for organization size appear at baseline only. Employees of small- and mid-size organizations perceive greater support for their health than employees of large organizations (P = .003 and P = .010). Finally, as expected, baseline and follow-up perceptions of employer support for health are positively associated (P < .001).
Table 7 shows associations between the elements of culture and lifestyle risk, at baseline (2013) and follow-up (2015). In the baseline model, none of the elements of culture have a statistically significant association with lifestyle risk (P < .05). We find a marginally significant association between increases in policy supports and reduced lifestyle risk.
Table 7.
Lifestyle Risk Regressed on Elements of a Culture at Health, at Baseline (2013) and Follow-Up (2015).a
| 2013 (n = 770) | 2015 (n = 771) | |||
|---|---|---|---|---|
| Predictor | Estimate | P Value | Estimate | P Value |
| Intercept | 2.396 | <.00l | 1.523 | <.00l |
| Employer-level (HSC) measures | ||||
| Environmental supports (employer-level) | −0.123 | .230 | −0.122 | .099 |
| Policy supports (employer-level) | −0.144 | .092 | −0.085 | .276 |
| Programmatic supports (employer-level) | 0.055 | .362 | 0.017 | .825 |
| Leadership support (employer-level) | −0.165 | .242 | 0.366 | .010 |
| Coworker support (employer-level) | −0.007 | .947 | −0.076 | .455 |
| Employee engagement (employer-level) | 0.021 | .934 | −0.175 | .390 |
| Strategic communication (employer-level) | 0.017 | .723 | 0.068 | .127 |
| Employee-level (self-perception) measures | ||||
| Leadership support (employee-level) | 0.047 | .629 | −0.261 | .003 |
| Coworker support (employee-level) | −0.025 | .653 | 0.076 | .103 |
| Employee engagement (employee-level) | 0.143 | .551 | 0.088 | .641 |
| Employee and organizational characteristics | ||||
| Age | 0.001 | .571 | −0.002 | .218 |
| Male | 0.132 | .008 | 0.077 | .117 |
| Hispanic ethnicity | 0.095 | .262 | −0.141 | .125 |
| Race: black/African American | 0.186 | .003 | 0.086 | .154 |
| Race: Asian | 0.082 | .391 | −0.079 | .401 |
| Race: other/multiracial | −0.074 | .473 | 0.270 | .023 |
| Education: less than high school | 0.261 | <.00l | 0.163 | .021 |
| Education: some college | 0.213 | <.001 | 0.127 | .008 |
| Hierarchical level: no supervisory authority | −0.070 | .169 | −0.042 | .402 |
| Hierarchical level: supervisory authority | −0.038 | .560 | −0.050 | .416 |
| Organization size: small | −0.033 | .658 | 0.093 | .146 |
| Organization size: mid | −0.046 | .523 | −0.010 | .865 |
| Baseline lifestyle risk | - | - | 0.340 | <.00l |
Abbreviation: HSC, Health ScoreCard.
Effects with P values less than .05 are set in bold type, and those with P values between .05 and .10 are italicized.
At follow-up (2015), we find statistically significant (P < .05) or marginally significant (P < .10) associations between 2 elements of the COH and lifestyle risk: leadership support and environmental supports. At the employer level, environmental supports are marginally associated with lower average lifestyle risk (P = .099). Also, at the employer-level, leadership support is associated with a higher lifestyle risk profile (P = .010). At the employee level, leadership support is associated with lower levels of lifestyle risk (P =.003)— again reflecting a change in the direction of effects when contrasting employer and employee findings.
We also find associations between lifestyle risk and gender, race, education, and baseline lifestyle risk. Men show higher levels of lifestyle risk than women at baseline only (P=.008). Black/African American participants also exhibit higher risk than white participants at baseline (P = .003), and the same is true of other or multiracial participants at follow-up only (P ¼ .023). Participants with less than a college degree experience elevated lifestyle risk at both baseline and follow-up, although position in the hierarchy does not play a role. Finally, we identify a significant effect for baseline risk on risk at follow-up (P < .001).
Appendix Tables A1 and A2 contain the results of our sensitivity analysis. We examined whether our baseline model results changed if we ran them on the sample of employees who participated in baseline data collection only but worked for employers with data at both time points (N = 1760). Descriptive analyses (not shown) revealed that these”dropout” participants differed from the sample of employees with data at both time points with respect to gender, race, and hierarchical level (P < .05). They also exhibited higher levels of lifestyle risk (P < .001). As Table A1 shows, in our model predicting perceived organizational support for health, the statistically significant employee effect for coworker support and employer effect for strategic communication are absent among the dropouts, although a new marginally significant employer-level effect for coworker support appears. The marginally significant employee effect for employee engagement is also fully significant in the dropout model. Table A2 shows the results for lifestyle risk. The marginally significant effect for policy supports identified in the original model is absent in the dropout model, and new effects for employer-level leadership and coworker support manifest (P = .027 and P = .003).
Discussion
Social science research and health promotion practice show that WHPPs, which reflect a “COH” can improve a range of employer and employee outcomes.2–8 Best practices in WHPP development and application define COH as including leadership and coworker support; environmental, policy, and pro-grammatic supports; employee engagement; and strategic communication.9,10,12 Although the real-world practices associated with each element are well- defined, measuring culture—particularly its social elements—nonetheless remains a challenge.21,33–35 This article measures the elements of a COH and investigates their association with 2 employee outcomes: perceived organizational support for health and lifestyle risk. Our findings can help employers prioritize their WHPP investments, which well-meaning but resource-strapped organizations commonly struggle with.21,28
We expected that all elements of culture would affect perceived organizational support for health and lifestyle risk. Instead, we found that only leadership support predicted both outcomes. The consistent effects for leadership support reflect the critical role that leaders play in developing WHPPs, allocating resources that support the programs, creating opportunities to adopt a healthy lifestyle (ie, by providing time and flexibility to use programming), and modeling healthy behaviors with words and deeds.9,10,12,13 The consistent effects likewise back our contention that leadership support may be one of the most important and perhaps even an essential element for effective health promotion programs.
Although we found a greater number of statistically significant associations between leadership support and our outcomes than we identified for the remaining elements of culture, the employer and employee effects for leadership support sometimes went in opposite directions. We generally found a negative association between leadership support and our outcomes among employers and positive associations among employees. Rather than implying that high levels of leadership support caused worse outcomes, on average, these findings could suggest employers already had poor perceived support and lifestyle risk outcomes and were thus more likely than other workplaces to increase leadership support during the study (ie, a reverse causality argument—perhaps employers had more to gain). The anticipated effects among employees might also suggest that the WHPPs examined yielded the anticipated benefits only among a small subset of employees. The implication may be that employees’ different perceptions of leadership support result from differences across supervisors. Other research has suggested that supervisors play a key role in communicating organizational values.14,15
We find similarly opposing effects across levels for employee engagement in the perceived support models, but not in the lifestyle models. Opposing effects across levels could suggest that employee engagement improves perceived support, but workers vary widely in how they respond to engagement initiatives. Previous research shows the difficulty in motivating employees in WHPPs.36 In the absence of the other elements of culture, employers’ interventions to increase employee engagement (eg, through incentives, competitions) could also be perceived as coercive rather than caring.
At baseline and follow-up, we find coworker support positively associated with perceived organizational support for health but not lifestyle risk. We identify these effects among employees only, which suggests that coworker influences on perceived support vary across work groups and tend not to show up across the organization. Social support networks may be more effective when smaller and more intimate or they may be motivating for only certain types of workers. Employers interested in developing a COH should thus work to ensure that WHPP messaging reaches all parts of the organization. If certain work groups develop unhealthy subcultures, employers may tailor messages to the group or expend extra effort to involve its thought leaders. If other work groups seem particularly health affirming, management could showcase the groups as reflecting organizational values.
Strategic communication is positively associated with perceived organizational support for health at baseline only. We suspect that, for the employers we studied, strategic communication may have become less essential during the study than it is in a typical workplace because participation in the NHWP already had heightened employees’ awareness of health promotion activities.
We generally find fewer associations between the elements of culture and lifestyle risk than we identified for perceived organizational support for health. Recall that the employers we studied began the NHWP with limited WHPPs and were selected to participate based on poor community health. Despite the limited number of effects, we confirmed the hypothesized negative association between employee leadership support and lifestyle risk in our follow-up model and identified marginally significant associations between environmental and policy supports and risk. Environmental and policy supports reflect enduring structural changes that encourage workers to make healthier choices and reflect employer investment in worker health.1,7,9,13,20
The relationships between elements of culture and our baseline outcomes differed when we compared participants with data at both time points to the dropouts, highlighting considerations for researchers and employers. The dropouts were demographically distinct from the participants in the main analysis and exhibited higher lifestyle risk. Dropouts may have left the participating employers during the study, perhaps for health reasons, or refused to participate in follow-up data collection precisely because they lacked enthusiasm for the WHPP. These findings underscore a weakness of many studies examining WHPPs: The workers who volunteer to participate in research evaluating WHPPs may be the healthiest and most invested in programming. Restricting data collection to volunteers may therefore result in misleading conclusions about the impact of a COH for workers more generally. Our models also suggest that not all employees will respond to culture in the same way. Since employers and employees arguably stand to benefit the most from reaching the least healthy members of the workforce, employers should consider whether distinct approaches are warranted to reach high-risk employees.
Some of this study’s limitations are attributable to the available measures. With respect to the dependent variables, we used a single, nonvalidated indicator for the perceived support for health outcome. We also used self-report measures for lifestyle risk outcomes. Our measure of lifestyle risk is derived from nutrition, physical activity, and tobacco use, as these were focal outcomes in the context of the larger NHWP initiative. We acknowledge that other lifestyle practices considered by NHWP employers, such as alcohol use, stress management, and occupational safety habits, are important predictors of overall health. However, since the goal of the initiative was to decrease rates of chronic disease, we focused on physical health and deemphasized other health outcomes, such as emotional, social, intellectual, spiritual, and financial well-being. Nonetheless, the lifestyle behaviors measured affect a wide range of individual and comorbid conditions (eg, physical activity enhances mental and emotional health).
Our independent variables introduce further limitations. Responses to the predictor items from HSC (eg, demonstrate organizational commitment and support of work site health promotion at all levels of management) were provided by representatives from each work site and not externally audited. Further, we defined the elements of culture from the measures available to us and did not psychometrically validate our summary measures. For instance, we did not measure whether managers model healthy behaviors, which is commonly identified as an important indicator of leadership support for employee health.9 Although we had some data on resources important for multiple dimensions of health (eg, employer provision of medical coverage), our analyses excluded employee-level income and related benefits (eg, employee assistance programs and retirement accounts), occupational health and safety policies and practices, and the spatial configuration of the work environment. Despite these limitations, to our knowledge, no intentionally designed and validated measures have been established for measuring a workplace COH.
Other limitations result from the design of the NHWP itself. The employer sample, although selected to be diverse with respect to industry sector and size, was not representative. Employers were selected based on community need (ie, high disease burden), community infrastructure (eg, availability of community partners and resources), and employer capacity and need (ie, ability to commit staff and resources to the program and lack of an existing WHPP). Although study leaders strove to create diversity in employers’ industry sector and overrecruited small to mid-size employers, these results may not be generalizable to all employers, for example, large-sized employers. For the purposes of establishing causal associations between elements of a COH and employee health, researchers would ideally use randomized controlled trials that compare employee outcomes among work sites that attempt to establish a COH with similar employers who make no such attempts. Employees would also preferably be assigned to an intervention and control group so that the differences we identified between the baseline participants who did and did not participate in follow-up would not appear. For practical and ethical reasons, such studies are difficult to carry out. We hope our study inspires future research using a more rigorous yet feasible approach—perhaps entailing a pre- and postintervention comparison limited to the employees who participated in the WHPP, however defined.
All results considered together, we conclude that the most relational elements of culture—leadership support, coworker support, and employee engagement—matter most for changing how employees think and feel about the organization’s support for health. The benefits of the relational elements seem to show up not at the organizational level but among certain employees and perhaps within specific work groups. In contrast, sustainable institutional investments in environmental and policy supports could matter more for changing employees’ health risk behavior. Different associations between the elements of culture and our outcomes suggest a need to move beyond discussions of “best practices,” so employers can think critically about their WHPPs’ goals (ie, to improve attitudes, behavior, or both?) and how to best reach all members of the workforce.17
SO WHAT? Implications for Health Promotion Practitioners and Researchers
What is already known on this topic?
Worksite health-promotion programs (WHPPs) can improve a range of employee and employer outcomes when the programs reflect a culture of health (COH), which entails leadership and coworker support; environmental, policy and programmatic supports; employee engagement; and strategic communication.
What does this article add?
This study defines the elements of a COH using a diverse sample of work sites, aiming to improve their WHPPs. Leadership support predicts our outcomes more consistently than the other elements of culture. Perceived organizational support for health is most closely associated with relational aspects of culture that vary within organizations, including leadership support, coworker support, and employee engagement. Lifestyle risk is marginally associated with organization-wide environmental and policy supports.
What are the implications for health promotion practice or research?
Employers and their partners in health promotion can develop WHPPs with elements aligned to organizational interests and goals, targeting multiple dimensions of health and well-being. Employers also need to aim to reach their entire workforce with WHP programming using evidence-based interventions and validated measures that support a COH, and continuously evaluate whether the program is meeting employees’ needs.
Acknowledgments
We thank the employers who participated in the program and all of the employees who completed assessments. We also acknowledge the staff who provided technical assistance to employers and Joel Hampton who created the data set for our analyses.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was supported by US Department of Health and Human Services and Centers for Disease Control and Prevention (contract number 200-2008-27958).
Appendix A
Table A1.
Perceived Organizational Support for Health Regressed on Elements of a Culture of Health at Baseline (2013), Participants With Data at Both Time Points Versus Dropouts With Baseline Data Only.a
| Matched (n = 765) | Dropouts From Continuing Employers (n = 1615) | |||
|---|---|---|---|---|
| Predictor | Estimate | P Value | Estimate | P Value |
| Intercept | 6.002 | <.001 | 6.524 | <.001 |
| Employer-level (HSC) measures | ||||
| Environmental supports (employer-level) | 0.049 | .899 | 0.246 | .611 |
| Policy supports (employer-level) | −0.526 | .138 | −0.607 | .171 |
| Programmatic supports (employer-level) | −0.138 | .561 | 0.128 | .672 |
| Leadership support (employer-level) | −1.738 | .002 | −1.461 | .009 |
| Coworker support (employer-level) | 0.211 | .568 | 0.775 | .079 |
| Employee engagement (employer-level) | −1.984 | .015 | −4.218 | <.001 |
| Strategic communication (employer-level) | 0.642 | .002 | 0.331 | .162 |
| Employee-level (self-perception) measures | ||||
| Leadership support (employee-level) | 3.305 | <.001 | 2.918 | <.001 |
| Coworker support (employee-level) | 0.422 | .009 | 0.181 | .113 |
| Employee engagement (employee-level) | 1.229 | .078 | 3.364 | <.001 |
| Employee and organizational characteristics | ||||
| Age | 0.009 | .085 | 0.008 | .035 |
| Male | 0.071 | .630 | 0.116 | .278 |
| Hispanic ethnicity | 0.229 | .368 | 0.088 | .639 |
| Race: black/African American | 0.204 | .280 | 0.052 | .667 |
| Race: Asian | 0.576 | .038 | 0.241 | .336 |
| Race: other/multiracial | 0.672 | .024 | 0.262 | .222 |
| Education: less than high school | 0.276 | .185 | 0.171 | .216 |
| Education: some college | 0.056 | .686 | 0.133 | .194 |
| Hierarchical level: no supervisory authority | 0.406 | .006 | 0.098 | .427 |
| Hierarchical level: supervisory authority | 0.335 | .081 | 0.154 | .284 |
| Organization size: small | 0.953 | .003 | 0.655 | .066 |
| Organization size: mid | 0.768 | .010 | 0.548 | .099 |
Abbreviation: HSC, Health ScoreCard
Effects with P values less than .05 are set in bold type, and those with P values between .05 and .10 are italicized.
Table A2.
Lifestyle Risk Regressed on Elements of a Culture at Health at Baseline (2013), Participants With Data at Both Time Points Versus Dropouts With Baseline Data Only.a
| Matched (n = 770) | Dropouts From Continuing Employers (n = 1628) | |||
|---|---|---|---|---|
| Predictor | Estimate | P Value | Estimate | P Value |
| Intercept | 2.396 | <.001 | 2.290 | <.001 |
| Employer-level (HSC) measures | ||||
| Environmental supports (employer-level) | −0.123 | .230 | −0.089 | .252 |
| Policy supports (employer-level) | −0.144 | .092 | −0.070 | .279 |
| Programmatic supports (employer-level) | 0.055 | .362 | 0.056 | .255 |
| Leadership support (employer-level) | −0.165 | .242 | 0.210 | .027 |
| Coworker support (employer-level) | −0.007 | .947 | −0.231 | .003 |
| Employee engagement (employer-level) | 0.021 | .934 | −0.004 | .980 |
| Strategic communication (employer-level) | 0.017 | .723 | 0.026 | .464 |
| Employee-level (self-perception) measures | ||||
| Leadership support (employee-level) | 0.047 | .629 | −0.031 | .612 |
| Coworker support (employee-level) | −0.025 | .653 | 0.002 | .962 |
| Employee engagement (employee-level) | 0.143 | .551 | −0.058 | .701 |
| Employee and organizational characteristics | ||||
| Age | 0.001 | .571 | 0.002 | .094 |
| Male | 0.132 | .008 | 0.004 | .888 |
| Hispanic ethnicity | 0.095 | .262 | −0.005 | .929 |
| Race: black/African American | 0.186 | .003 | 0.209 | <.001 |
| Race: Asian | 0.082 | .391 | 0.176 | .020 |
| Race: other/multiracial | −0.074 | .473 | 0.040 | .546 |
| Education: less than high school | 0.261 | <.001 | 0.230 | <.001 |
| Education: some college | 0.213 | <.001 | 0.198 | <.001 |
| Hierarchical level: no supervisory authority | −0.070 | .169 | 0.040 | .283 |
| Hierarchical level: supervisory authority | −0.038 | .560 | 0.034 | .443 |
| Organization size: small | −0.033 | .658 | 0.169 | .005 |
| Organization size: mid | −0.046 | .523 | 0.047 | .340 |
Abbreviation: HSC, Health ScoreCard.
Effects with P values less than .05 are set in bold type, and those with P values between .05 and .10 are italicized.
Footnotes
Authors’ Note
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Sparling PB. Worksite health promotion: principles, resources, and challenges. Prev Chronic Dis. 2009;7(1):A25 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2811520/. Accessed February 5, 2018. [PMC free article] [PubMed] [Google Scholar]
- 2.Soler RE, Leeks KD, Razi S, et al. A systematic review of selected interventions for worksite health promotion. The assessment of health risks with feedback. Am J Prev Med. 2010;38(2 Suppl): S237–S262. doi: 10.1016/j.amepre.2009.10.030. [DOI] [PubMed] [Google Scholar]
- 3.Goetzel RZ, Henke RM, Tabrizi M, et al. Do workplace health promotion (wellness) programs work? J Occup Environ Med. 2014;56(9):927–934. doi: 10.1097/JOM.0000000000000276. [DOI] [PubMed] [Google Scholar]
- 4.Terry PE, Seaverson ELD, Grossmeier J, Anderson DR. Association between nine quality components and superior worksite health management program results. J Occup Environ Med. 2008;50(6):633–641. doi: 10.1097/JOM.0b013e31817e7c1c. [DOI] [PubMed] [Google Scholar]
- 5.Chapman LS. Meta-evaluation of worksite health promotion economic return studies. Am J Health Promot. 2003;17(3):1–10. [DOI] [PubMed] [Google Scholar]
- 6.Baicker K, Cutler D, Song Z. Workplace wellness programs can generate savings. Health Aff (Millwood). 2010;29(2):304–311. doi: 10.1377/hlthaff.2009.0626. [DOI] [PubMed] [Google Scholar]
- 7.Kaspin LC, Gorman KM, Miller RM. Systematic review of employer-sponsored wellness strategies and their economic and health-related outcomes. Popul Health Manag. 2013;16(1):14–21. 8p. doi: 10.1089/pop.2012.0006. [DOI] [PubMed] [Google Scholar]
- 8.Goetzel RZ, Henke RM, Benevent R, et al. The predictive validity of the HERO scorecard in determining future health care cost and risk trends. J Occup Environ Med. 2014;52(2):136–144. [DOI] [PubMed] [Google Scholar]
- 9.Kent K, Goetzel RZ, Roemer EC, Prasad A, Freundlich N. Promoting healthy workplaces by building cultures of health and applying strategic communications. J Occup Environ Med. 2016;58(2):114–122. doi: 10.1097/JOM.0000000000000629. [DOI] [PubMed] [Google Scholar]
- 10.Goetzel RZ, Shechter D, Ozminkowski RJ, Marmet PF, Tabrizi MJ, Roemer EC. Promising practices in employer health and productivity management efforts: findings from a benchmarking study. J Occup Environ Med. 2007;49(2):111–130. [DOI] [PubMed] [Google Scholar]
- 11.Schein EH. Organizational Culture and Leadership. San Francisco: Jossey-Bass; 2010. [Google Scholar]
- 12.Pronk N Best practice design principles of worksite health and wellness programs. ACSMs Health Fit J. 2014;18(1):42–46. [Google Scholar]
- 13.Goetzel RZ, Guindon AM, Turshen IJ, Ozminkowski RJ. Health and productivity management: establishing key performance measures, benchmarks, and best practices. J Occup Environ Med. 2001;43(1):10–17. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease Control (CDC). Essential Elements of Effective Workplace Programs and Policies for Improving Worker Health and Wellbeing. Atlanta, GA: Work Life A National Institute for Occupational Safety and Health Initiative; 2008. http://www.cdc.gov/niosh/docs/2010-140/pdfs/2010-140.pdf. Published October 2008. Accessed February 5, 2018. [Google Scholar]
- 15.Rhoades L, Eisenberger R. Perceived organizational support: a review of the literature. J Appl Psychol. 2002;87(4):698–714. doi: 10.1037/0021-9010.87.4.698. [DOI] [PubMed] [Google Scholar]
- 16.Michie S, Williams S. Reducing work related psychological Ill health and sickness absence: a systematic literature review. Occup Environ Med. 2003;60(1):3–9. doi: 10.1136/oem.60.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lemon SC, Zapka J, Li W, Estabrook B, Magner R, Rosal MC. Perceptions of worksite support and employee obesity, activity, and diet. Am J Health Behav. 2009;33(3):299–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tabak RG, Hipp JA, Marx CM, Brownson RC. Workplace social and organizational environments and healthy-weight behaviors. PLoS One. 2015;10(4):e0125424. doi: 10.1371/journal.pone.0125424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kelsey KS, Campbell MK, Tessaro I, et al. Social support and health behaviors among blue-collar women workers. Am J Health Behav. 2000;24(6):434–443. doi: 10.5993/AJHB.24.6.4. [DOI] [Google Scholar]
- 20.Goetzel RZ, Ozminkowski RJ. The health and cost benefits of work site health-promotion programs. Annu Rev Public Health. 2008;29(1):303–323. doi: 10.1146/annurev.publhealth.29.020907.090930. [DOI] [PubMed] [Google Scholar]
- 21.Terry PE, Eisenberger R, Shanock S. The art of health promotion. An interview on perceived organizational support and employee well-being with Drs. Robert Eisenberger and Linda Shanock. Am J Health Promot. 2014;29(1):TAHP2–TAHP7. [PubMed] [Google Scholar]
- 22.Zoller HM. Manufacturing health: employee perspectives on problematic outcomes in a workplace health promotion initiative. West J Commun. 2004;68(3):278–301. doi: 10.1080/10570310409374802. [DOI] [Google Scholar]
- 23.Berry L, Mirabito AM, Baun WB. What’s the hard return on employee wellness programs? Harv Bus Rev. December 2010. https://ssrn.com/abstract=2064874. Accessed February 5, 2018. [PubMed] [Google Scholar]
- 24.Peterson K, Rogers BME, Brosseau LM, et al. Differences in hospital managers’, unit managers’, and health care workers’ perceptions of the safety climate for respiratory protection. Workplace Health Saf. 2016;64(7):326–336. doi: 10.1177/2165079916640550.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lang J, Cluff L, Payne J, Matson-Koffman D, Hampton. The Centers for Disease Control and Prevention: Findings from the National Healthy Worksite Program. J Occup Environ Med. 2017; 59(7):631–641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Centers for Disease Control (CDC), Division of Population Health, National Center for Chronic Disease Prevention and Health Promotion. Workplace Health Model. http://www.cdc.gov/workplacehealthpromotion/model/index.html. Updated 2016. Accessed February 5, 2018.
- 27.U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2010. 7th ed. Washington, DC: Government Printing Office; 2010. [Google Scholar]
- 28.U.S. Centers for Disease Control and Prevention. How Much Physical Activity Do Adults Need?; 2015. https://www.cdc.gov/physicalactivity/basics/adults/index.htm. Accessed February 5, 2018.
- 29.Terry PE, Grossmeier J, Mangen DJ, Gingerich SB. Analyzing best practices in employee health management: how age, sex, and program components relate to employee engagement and health outcomes. J Occup Environ Med. 2013;55(4):378–392. doi: 10.1097/JOM.0b013e31828dca09. [DOI] [PubMed] [Google Scholar]
- 30.Hannon PA, Garson G, Harris JR, Hammerback K, Sopher CJ, Clegg-Thorp C. Workplace health promotion implementation, readiness, and capacity among mid-sized employers in low-wage industries: a national survey. J Occup Environ Med. 2012; 54(11):1337–1343. doi: 10.1097/JOM.0b013e3182717cf2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hannon PA, Harris JR, Sopher CJ, et al. Improving low-wage, midsized employers’ health promotion practices: a randomized controlled trial. Am J Prev Med. 2012;43(2):125–133. doi: 10.1016/j.amepre.2012.04.014. [DOI] [PubMed] [Google Scholar]
- 32.Linnan L, Bowling M, Childress J, et al. Results of the 2004 national worksite health promotion survey. Am J Public Health. 2008;98(8):1503–1509. doi: 10.2105/AJPH.2006.100313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Denison DR. What is the difference between organizational culture and organizational climate? A native’s point of view on a decade of paradigm wars. Acad Manage Rev. 1996;21(3): 619–654. doi: 10.2307/258997. [DOI] [Google Scholar]
- 34.DeJoy DM, Wilson MG, Goetzel RZ, et al. Development of the environmental assessment tool (EAT) to measure organizational physical and social support for worksite obesity prevention programs. J Occup Environ Med. 2008;50(2):126–137. doi: 10.1097/JOM.0b013e318161b42a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wilson MG, Dejoy DM, Vandenberg RJ, Richardson HA, McGrath AL. Work characteristics and employee health and well-being: test of a model of healthy work organization. J Occup Organ Psychol. 2004;77(4):565–588. [Google Scholar]
- 36.Person AL, Colby SE, Bulova JA, Eubanks JW. Barriers to participation in a worksite wellness program. Nutr Res Pract. 2010; 4(2):149–154. doi: 10.4162/nrp.2010.4.2.149. [DOI] [PMC free article] [PubMed] [Google Scholar]