Abstract
This chapter examines attitudes toward condom use in a national random sample of 332 MSM who use the Internet to seek men with whom they can engage in unprotected sex. Data collection was conducted via telephone interviews between January 2008 and May 2009. The following three research questions were addressed: 1) How do these men feel about using condoms, both ideologically and personally? 2) How do condom use attitudes relate to actual HIV risk behavior practices? 3) What factors underlie men’s attitudes toward condom use? The findings indicated that men held weakly-positive attitudes toward condom use overall, but were noticeably more negative in their attitudes regarding the personal use of condoms. Condom use attitudes were related consistently and inversely to involvement in HIV risk practices. In both multivariate and structural equation analyses, men’s condom-related attitudes were the single strongest factor associated with their involvement in risky sex. A number of factors were found to be correlated with more favorable attitudes toward condom use. These were: caring about potential sex partners’ HIV serostatus, experiencing fewer drug-related problems, having a lower level of educational attainment, not preferring to have “wild” or “uninhibited” sex, higher self-esteem, being African American, and not perceiving great accuracy in the information that sex partners supply verbally about their HIV serostatus.
Introduction
Men who have sex with men (MSM) represent one of the groups considered most at risk for the sexual transmission of HIV, at least in part due to their comparatively high risk per exposure via anal sex. The risk per exposure is estimated to be 1.00% for receptive anal sex and 0.06% for insertive anal sex as compared to 0.01–0.32% for receptive vaginal sex and 0.01–0.10% for insertive vaginal sex [1]. As condoms represent an effective method of HIV prevention, extensive efforts have been made by researchers to understand condom use attitudes in a variety of populations and to promote consistent condom use. In the United States, recent research shows that among MSM, increases in safer sex fatigue are associated with increases in the number of partners with whom they reported engaging in unprotected sex [2]. Surprisingly, there has been limited research addressing condom-related attitudes among MSM in the United States. A few studies, however, have examined condom attitudes and behavior in subpopulations of MSM, such as African American MSM [3,4], Latino MSM [5], and methamphetamine-using HIV-positive MSM [6]. These studies have shown that, among African American MSM, stronger peer condom use norms were associated with a lower frequency of risk behavior involvement [3] and lesser involvement in HIV risk behavior was associated with the perception of social norms that support condom use [4]. In a sample of Latino MSM, participants most commonly cited pleasure as the reason for a lack of condom use [5]. In a sample of methamphetamine-using HIV-positive MSM, researchers found that among men with negative attitudes about condoms, there was an association between methamphetamine use frequency and unprotected sex [6].
Although condoms are highly effective for HIV prevention when used correctly, research has shown that most individuals do not use condoms consistently [7], and others intentionally seek partners for unprotected sex. Previous research indicates a variety of factors associated with the motivation among MSM for barebacking (that is, the intentional practice of engaging in unprotected anal intercourse) [8]. These factors include the desire to: cope with psychosocial vulnerabilities [9], create intimacy with partners [9], exchange semen [10], maximize physical and/or emotional pleasure [11], and overcome social isolation [12]. Research efforts are underway to develop alternative methods of HIV prevention that are acceptable among MSM [13]. Condoms are currently the best known strategy for HIV prevention during sexual contact. Therefore, understanding the condom-related attitudes and behavior of men who seek other men for unprotected sexual contact is an important part of strategizing ways in which this subpopulation of MSM can increase safety and health by preventing HIV infection. As we previously noted, though, little has been written about condom-related attitudes among MSM, especially with regard to specific attitudes about particular aspects of condom use (e.g., perceived inconvenience, embarrassment regarding use, discomfort, etc.). Most of the published studies have reported, simply, that negative attitudes toward condoms were associated with greater involvement in risky practices [14].
Recent research has examined the use of the Internet among MSM for meeting potential sex partners, typically finding that this practice is associated with a variety of HIV risk behaviors. For example, one recent study [15] showed that 40% of MSM Internet users acknowledged engaging in unprotected anal sex. Similarly, in a study comparing self-identified barebackers and non-barebackers, barebackers were more likely to spend more time on the Internet looking for potential sex partners [16]. Furthermore, researchers have found that men who seek sex online report more unprotected sex and sexually transmitted infections compared to their peers who do not use the Internet to identify sex partners [17, 18]. In a study that examined online ads and profiles on MSM-oriented unprotected sex-focused websites, the rates of advertised high-risk sexual behaviors were very high, including oral sex with ejaculation in the mouth (88.0% receptive, 77.4% insertive), anal sex with ejaculation in the anus (79.7% insertive, 69.4% receptive), multiple partner sex (77.9%), and felching (16.5%) [19]. Evidence shows increasing numbers of young MSM who meet their first sexual partner online [20]. In another sample of MSM who use the Internet, guessing the HIV serostatus of the sexual partner, as compared to checking the online profile and pre- and post-sex discussions, was associated with higher levels of unprotected anal sex [21].
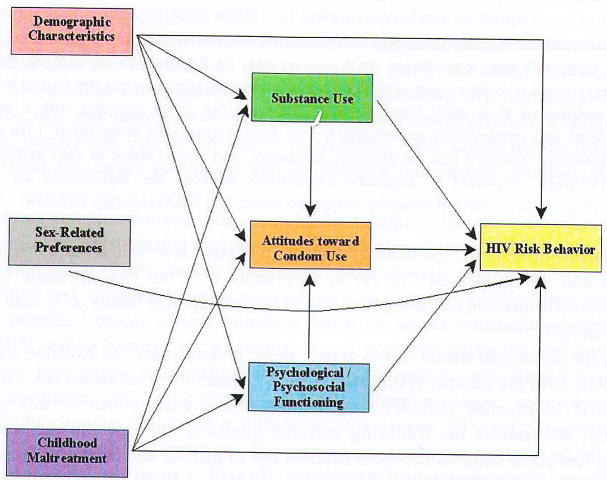
In the present paper, a structural approach is used to develop a better understanding of how attitudes toward condom use are related to HIV risk taking in a sample of men who use the Internet specifically to find other men with whom they can engage in unprotected sex. Based on previously published studies, the conceptual model depicted in Figure 1 was examined. In this model, attitudes toward condom use are conceptualized as an endogenous measure–that is, both as an independent variable, contributing to the understanding of men’s involvement in risky behaviors, and as a dependent variable, varying based upon the effects of numerous other types of measures. As the conceptual model shows, condom-related attitudes are one of six types of influences hypothesized to affect men’s HIV risk practices. The others are demographic variables (e.g., race/ethnicity, age, HIV serostatus), sex-related behavioral preferences (e.g., self-identification as a sexual “top” versus a “bottom,” preferring to have sex that is “wild” or “uninhibited”), substance use/abuse, childhood maltreatment experiences, and psychological/psychosocial functioning (e.g., depression, self-esteem, impulsivity).
Figure 1.
Conceptual model.
To a great extent, this conceptual model owes its intellectual origins to the notion of syndemic and to Syndemics Theory. “Syndemic” refers to the tendency for multiple epidemics to co-occur and, in the process of affecting some of the same people, for the various maladies to interact with one another, with each one worsening the effects of the others [22,23]. Walkup et al [24] noted that health problems may be construed as syndemic when two or more conditions/afflictions are linked in such a manner that they interact synergistically, with each contributing to an excess burden of disease in a particular population. It is noteworthy that their work addresses the syndemic of HIV, substance abuse, and mental illness. A good example of how conditions may become syndemic is offered by Romero-Daza et al [25] in their study of sex work. The authors wrote:
Streetwalkers’ continuous exposure to violence, both as victims and as witnesses, often leaves them suffering from major emotional trauma. In the absence of adequate support services, women who have been victimized may turn to drug use in an attempt to deal with the harsh realities of their daily lives. In turn, the need for drugs, coupled with a lack of educational and employment opportunities, may lead women into prostitution. Life on the street increases women’s risk for physical, emotional, and sexual abuse as well as their risk for HIV/AIDS. Exposure to traumatic experiences deepens the dependence on drugs, completing a vicious cycle of violence, substance abuse, and AIDS risk (pp. 233–234)
A number of authors, particularly during the past few years, have written about syndemics and the Syndemics Theory, as they apply it to the HIV epidemic [23,25–27], including specific mention of the applicability of the concept and theory as to men who have sex with men [27].
Using the conceptual model shown above, in the present study, we examine a population of MSM who used the Internet specifically to find partners for unprotected sex. Our focus in this paper is to examine attitudes toward condom use among men in this population. Specifically, we address the following research questions: 1) How do members of this population feel about condom use–both condom use in general and condom use as it applies to the men themselves? 2) How, if at all, do condom-related attitudes relate to men’s involvement in HIV risk practices? 3) What factors are associated with having more favorable attitudes regarding condom use?
Our study
This chapter draws from data that were collected between January 2008 and May 2009 for The Bareback Project, a study funded by the National Institute on Drug Abuse. The study sample consisted of men who use the Internet specifically to find other men with whom they can engage in unprotected sex. Some of the 16 websites from which the sample of 332 men were recruited catered exclusively to unprotected sex (e.g., Bareback.com, RawLoads.com). Other websites used did not cater to unprotected sex exclusively but did make it possible for site users to identify which individuals were looking for unprotected sex (e.g., Men4SexNow.com, Squirt.org). Using the 16 websites, a national random sample of risk-seeking MSM was derived. Random selection was based on a combination of the first letter of the person’s online username, his race/ethnicity (as listed in his profile), and the day of recruitment. Men of color were oversampled, to ensure good representation of men belonging to racial minority groups and to facilitate the examination of racial differences in risk behaviors and risk-related preferences. Recruitment took place seven days a week, during all hours of the day and night, varying from week to week throughout the project, to maximize the representativeness of the research sample, in recognition of the fact that different people use the Internet at different times.
Initially, men were approached for participation either via instant message or email (much more commonly via email), depending upon the website used. Potential participants were provided with a brief overview of the study and informed consent-related information, and they were given the opportunity to ask questions about the study before deciding whether or not to participate. Potential participants were also provided with a website link to the project’s online home page, to offer additional information about the project and to help them feel secure in the legitimacy of the research endeavor. Interested men were scheduled for an interview soon after they expressed an interest in taking part in the study, typically within a few days. To maximize convenience for participants, interviews were conducted during all hours of the day and night, seven days a week, based on interviewer availability and participants’ preferences. All of the study’s interviewers were gay or lesbian, to engender credibility with the target population and to enhance participants’ comfort during the interviews.
Participants completed a one-time, confidential telephone interview addressing a wide array of topics. The questionnaire that was used was developed specifically for The Bareback Project. Many parts of the survey instrument were derived from standardized scales previously used and validated by other researchers. The interview covered such subjects as: degree of “outness,” perceived discrimination based on sexual orientation, general health practices, HIV testing history and serostatus, sexual practices (protected and unprotected) with partners met online and offline, risk-related preferences, risk-related hypothetical situations, substance use, drug-related problems, Internet usage, psychological and psychosocial functioning, childhood maltreatment experiences, HIV/AIDS knowledge, and some basic demographic information. The interviews lasted an average of 69 minutes (median = 63, s.d. = 20.1, range = 30–210). Participants who completed the interview were offered $35. Approval of the research protocol was given by the institutional review boards at Morgan State University (approval number 07/12-0145), where the principal investigator and one of the research assistants were affiliated, and George Mason University (approval number 5659), where the other research assistant was located.
Measures used
The principal variable of interest in this research is a 17-item scale pertaining to men’s attitudes toward condom use. Individual items were scored on a five-point Likert scale, and higher scores on the scale corresponded with more conducive attitudes toward condom use. The scale was derived from the work of Brown [28] and it was found to be highly reliable (Cronbach’s alpha = 0.91). Only items that were relevant to MSM and their sexual practices were used, so that the scale would be applicable to the study population.
For the second part of the analysis, examining the relationship between condom attitudes and risk practices, several HIV risk practice measures were examined, all using a past-30-day time frame of reference. These included: overall proportion of sex acts involving the use of condoms (a continuous measure based on responses to separate items inquiring about oral, anal, and vaginal sex), proportion of anal sex acts involving the use of condoms (a continuous measure derived from the variables just described), overall proportion of sex acts involving internal ejaculation (a continuous measure based on responses to separate items inquiring about where ejaculation occurred during oral, anal, and vaginal sex), proportion of anal sex acts involving internal ejaculation (a continuous measure derived from the items just described), having any sexual relations while under the influence of alcohol and/or other drugs (yes/no), number of male sex partners (continuous), number of times having “wild” or “uninhibited” sex (self-defined, continuous measure), and number of times having sex of any kind in a gay bath house or sex club (continuous). Men’s estimated total number of lifetime sex partners was also examined (continuous).
For the third part of the analysis, focusing on identifying the factors associated with better/worse attitudes toward condom use, a variety of factors in several domains were considered. The first consisted of demographic and background variables. These were: age (continuous), race/ethnicity (categorical), sexual orientation (gay versus bisexual), relationship status (involved versus not involved), educational attainment (continuous), and sexual role identity (top, versatile top, versatile, versatile bottom, bottom).
The second consisted of several HIV-related measures. These included: HIV serostatus (positive, negative, unknown), knowing anyone currently living with HIV or AIDS (two separate yes/no measures), the number of people known who died from AIDS (continuous), preferred HIV serostatus of sex partners (positive, negative, does not matter), perceived accuracy of HIV serostatus information provided verbally by sex partners (ordinal), and perceived accuracy of online HIV serostatus information (ordinal).
The third domain pertained to men’s risk-related preferences for sexual practices, including how rough they preferred their sex to be (continuous), how long they most liked their sexual sessions to last (continuous), how much they liked having sex in public venues (continuous), how much they liked having sex that was “wild” or “uninhibited” (continuous), and liking to have anonymous sex (yes/no).
The fourth domain pertained to substance use/abuse and included the following measures: currently a user of illegal drugs (yes/no), number of drug problems experienced (continuous), and total amount of illegal drug use (continuous measure of quantity × frequency of recent use, summed across nine drug types).
The final domain assessed psychological and psychosocial functioning. Measures examined were: self-esteem (using the Rosenberg self-esteem scale [29]; Cronbach’s alpha = 0.89), impulsivity (derived from the Barratt Impulsiveness Scale [30]; Cronbach’s alpha = 0.76), depression (using the CES-D [31]; Cronbach’s alpha = 0.93), optimism about the future (using the Life Orientation Test–Revised [32]; Cronbach’s alpha = 0.78), current life satisfaction (adapted from the Satisfaction with Life scale [33]; Cronbach’s alpha = 0.83), HIV/AIDS information burnout (derived from HIV Knowledge Questionnaire [34]; Cronbach’s alpha = 0.76), and childhood maltreatment experiences (separate measures for sexual abuse, physical abuse, emotional abuse, and neglect, taken from the Childhood Trauma Questionnaire [35]; Cronbach’s alpha = 0.94).
Analysis
Part 1 of the analysis, focusing on identifying men’s attitudes toward condom use, relied upon descriptive statistics. Part 2, examining the relationship between condom attitudes and involvement in risk practices, primarily used simple regression as the analytical strategy, as the independent variable and all but one of the dependent variables examined were continuous in nature. The one exception–whether or not the person had engaged in any recent sex while under the influence of alcohol and/or other drugs–was dichotomous, thereby making logistic regression the appropriate analytical tool.
Part 3, focusing on the factors associated with men’s condom-related attitudes, was undertaken in two steps. First, bivariate relationships were assessed for each of the independent variables outlined above and condom attitudes, using the latter as the dependent variable. Whenever the independent measure was dichotomous (e.g., sexual orientation, HIV-positive serostatus), Student’s t tests were used. Whenever the independent variable was continuous (e.g., educational attainment, self-esteem level), simple regression was used. Then, all items found to be related either significantly (p<.05) or marginally (.15>p>.05) to condom-related attitudes were entered into a multivariate equation, and then removed in stepwise fashion until a best fit model containing only statistically-significant measures remained.
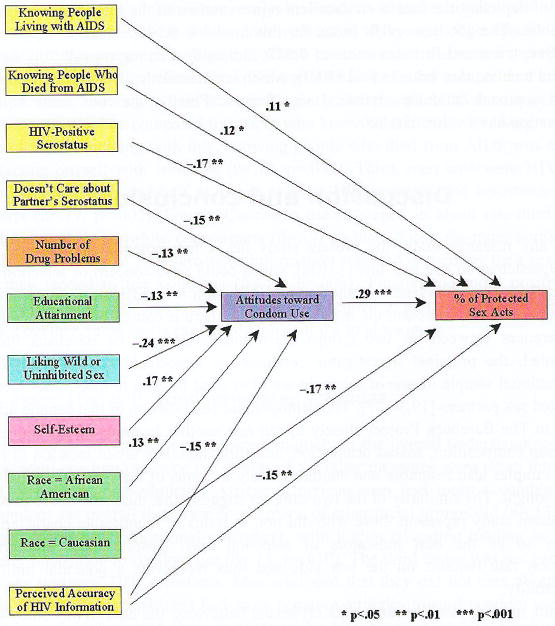
In Part 4, the relationships depicted in Figure 2 (which were the result of the Part 2 and Part 3 analysis) were subjected to a structural equation analysis to determine whether the way the relationships depicted there are an appropriate and effective representation of the study data. SAS’s PROC CALIS procedure was used to assess the overall fit of the model to the data. When we use this type of structural equation analysis, we look for several specific outcomes: (1) a goodness-of-fit index as close to 1.00 as possible, but no less than 0.90, (2) a Bentler-Bonett normed fit index value as close to 1.00 as possible, but no less than 0.90, (3) an overall chi-square value for the model that is statistically nonsignificant, preferably as far from attaining statistical significance as possible, and (4) a root mean square error approximation value as close to 0.00 as possible, but no greater than 0.05. If these conditions are met, then the relationships depicted are considered to indicate a good fit with the data.
Figure 2.
Condom-related attitudes and protected sex.
Throughout all of the analyses, results are reported as statistically significant whenever p<.05.
Our findings
In total, 332 men participated in the study. They ranged in age from 18 to 72 (mean = 43.7, s.d. = 11.2, median = 43.2). Racially, the sample is a fairly close approximation of the American population, with 74.1% being Caucasian, 9.0% each being African American and Latino, 5.1% self-identifying as biracial or multiracial, 2.4% being Asian, and 0.3% being Native American. The large majority of the men (89.5%) considered themselves to be gay and almost all of the rest (10.2%) said they were bisexual. On balance, men participating in The Bareback Project were fairly well-educated. About 1 man in 7 (14.5%) had completed no more than high school; 34.3% had some college experience without earning a college degree; 28.9% had a bachelor’s degree; and 22.3% were educated beyond the bachelor’s level. Slightly more than one-half of the men (59.0%) reported being HIV-positive; most of the rest (38.6%) were HIV-negative.
Attitudes toward condom use
Overall, men’s attitudes toward condom use were rather ambivalent, averaging 2.96 on a 1–5 scale (see Table 1). On the positive side, most study participants felt that men should not be embarrassed to suggest a condom (93.0%), that using a condom was not a reason for feeling embarrassment (83.0%), and that they would not object if one of their partners asked them to use a condom (61.8%).
Table 1.
Attitudes toward Condom Use
| Attitude Item | Percentage Disagreeing | Percentage Neutral | Percentage Agreeing |
|---|---|---|---|
| * In your opinion, condoms are too much trouble. | 31.8 | 19.4 | 48.8 |
| Condoms are unreliable. | 16.7 | 18.8 | 64.5 |
| * Condoms are pleasant to use | 74.6 | 15.2 | 10.3 |
| There is no reason why a man should be embarrassed to suggest a condom. | 3.3 | 3.6 | 93.0 |
| * You think that proper use of condoms can enhance sexual pleasure. | 63.9 | 16.7 | 19.4 |
| Many people make using condoms an erotic part of foreplay. | 35.5 | 27.6 | 37.0 |
| * You just don’t like the idea of using condoms. | 65.5 | 13.0 | 21.5 |
| * You think condoms look ridiculous. | 18.2 | 18.2 | 63.6 |
| Condoms are inconvenient. | 55.2 | 14.8 | 30.0 |
| You see no reason to be embarrassed by the use of condoms. | 8.2 | 8.8 | 83.0 |
| * Putting a condom on an erect penis can be a real sexual turn-on. | 63.9 | 15.2 | 20.9 |
| * Condoms are uncomfortable. | 57.3 | 13.9 | 28.8 |
| * Using a condom makes sex unenjoyable. | 47.0 | 18.5 | 34.5 |
| * You would avoid using condoms if at all possible. | 70.6 | 9.7 | 19.7 |
| Putting on a condom is an interruption of foreplay. | 50.6 | 16.1 | 33.3 |
| * There is no way that using a condom can be pleasant. | 25.5 | 18.2 | 56.4 |
| * You would have no objection if your partner suggested that you use a condom. | 29.1 | 9.1 | 61.8 |
Attitude toward personal condom use.
But on the negative side, most study participants felt that condoms were unreliable (64.5%), that they were not pleasant to use (74.6%), that their use could not enhance sexual pleasure (63.9%), that they looked ridiculous (63.6%), and that putting on a condom was a sexual turn-off (63.9%).
Nearly two-thirds of the men studied said that they simply do not like the idea of using condoms (65.5%) and even more of the men said that they would avoid using condoms if at all possible (70.6%).
As Table 1 also shows, if a differentiation is made between men’s attitudes toward condom use in general (that is, condom use as a concept, not applied to their specific behaviors) and their attitudes toward using condoms themselves (that is, attitudes toward personal condom use), a rather different picture emerges. Whereas men’s attitudes toward condom use in general were positive overall (mean score = 3.38), their attitudes toward personal condom use were noticeably more negative (mean score = 2.73).
Condom-related attitudes and behavioral risk
As expected, men’s attitudes toward condom use were related closely to their involvement in sexual risk practices (see Table 2). This was true for the global measure of condom-related attitudes and for the component measure of attitudes toward personal condom use. In every instance, more favorable attitudes toward condom use were associated with lesser involvement in risky sex. This was true for the overall proportion of all sex acts involving the use of condoms (p<.0001), the proportion of anal sex acts involving the use of condoms (p<.0001), the proportion of all sex acts involving internal ejaculation (p<.0001), the proportion of anal sex acts involving internal ejaculation (p<.0001), the likelihood that the person recently had engaged in any sex acts while under the influence of alcohol and/or other drugs (p=.0003), the number of sex partners that the person reported having had recently and during his lifetime (both p<.0001), the number of times recently having engaged in sex adjudged by the man himself to be “wild” or “uninhibited” (p=.0005), and the number of times recently having had sex in a place like a gay bath house or a sex club (p=.036).
Table 2.
Attitudes toward Condom Use and Involvement in Risky Sex
| Risk Behavior Measure | Overall Condom-Related Attitudes | Attitudes toward Personal Condom Use |
|---|---|---|
| % of protected sex acts | p<.0001 | p=.0005 |
| % of protected anal sex | p<.0001 | p<.0001 |
| % of sex acts with internal ejaculation | p<.0001 | p=.0014 |
| % of anal sex acts with internal ejaculation | p<.0001 | p=.0004 |
| had any sex while “under the influence” | p=.0003 | p=.0009 |
| number of recent sex partners | p<.0001 | p<.0001 |
| number of lifetime sex partners | p<.0001 | p=.0011 |
| number of times recently having “wild” or “uninhibited” sex | p=.0005 | p=.0006 |
| number of times recently having sex in a gay bath house or a sex club | p=.0356 | p=.0334 |
When examined via multivariate analysis, condom-related attitudes are the single strongest factor associated with men’s involvement in risky sex. One specific example demonstrating this is presented in Figure 2, where the outcome measure is the proportion of all sex acts involving the use of condoms. Six variables were found to be related uniquely to the equation. First, knowing people who are currently living with AIDS was associated with greater condom use when compared to people who knew no one currently living with AIDS (β=.11, p=.034). Coinciding with this, knowing people who died from AIDS was associated with protecting oneself with condoms (β=.12, p=.032). Third, men who were HIV-positive used condoms less than one-half as much as their HIV-negative and serostatus-unknown counterparts (β=.17, p=.002). Fourth, Caucasian men engaged in about one-third as much protected sex as their nonwhite counterparts (β=.17, p=.002). Fifth, the more confident men were in the truthfulness of HIV serostatus information supplied to them by their sex partners, the less they tended to use condoms (β=.15, p=.006). Finally, the more positive men’s attitudes toward using condoms were, the more they tended to practice protected sex (β=.29, p<.0001). Together, these items explained 23.8% of the total variance.
Factors associated with condom-related attitudes
As Figure 2 shows, seven items contributed uniquely to the overall understanding of men’s attitudes toward condom use once the effects of the other measures were taken into account. The first factor was race/ethnicity. African American men had more favorable attitudes toward condom use overall than their counterparts of other racial groups did (β=.13, p=.008). The second factor was educational attainment, with higher education tending to be linked with greater opposition to condom use (β=.13, p=.010). The third factor was not caring about potential sex partners’ HIV serostatus. Men who said that they did not care about the HIV serostatus of potential sex partners had more negative attitudes toward condom use than did men who specifically wanted their partners to be HIV-positive or HIV-negative (β=.15, p=.004). The fourth contributing measure was the preference for “wild” or “uninhibited” sex. The more that men wanted their sex to be “wild” or “uninhibited,” the more negative their attitudes toward condoms were (β=.24, p<.0001). The fifth factor was the number of drug problems that men experienced, with a greater number of drug-related problems (i.e., abuse/dependency symptoms) being associated with more negative attitudes toward condom use (β=.13, p=.009). The sixth measure retained in the multivariate equation was the perceived accuracy of information provided by sex partners about their HIV serostatus. The more that men believed in the accuracy of what their sex partners told them about their HIV serostatus, the less favorably disposed they tended to be regarding condom use (β=.15, p=.004). Finally, level of self-esteem was found to be associated with men’s attitudes toward condom use, with better self-esteem corresponding to more favorable condom-related attitudes (β=.17, p=.001). Together, in the multivariate analysis, these items explained 21.9% of the total variance.
The overall role of condom-related attitudes
Figure 2 portrays the specific role played by men’s attitudes toward condom use when it comes to their involvement in protected sex. The structural equation analysis revealed that this way of depicting the data is an excellent representation of the interrelationships amongst the variables. The goodness-of-fit index for this model is 0.995, which is supported by the Bentler-Bonett normed fit index value of 0.977, indicating a strong overall “fit” for the data. The model’s chi-square value is 9.52 (10df), which is not statistically significant (p=.484) and does not approach attaining statistical significance. Finally, the root mean square error approximation has a value of 0.000.
Discussion and conclusion
As with any research study, the present study has a few potential limitations. First, the response/participation rate was low (<10%), which could raise concern of selection bias and, therefore, the representativeness of the sample. Although it is difficult to be certain that the men who participated represent the men who did not, there is compelling evidence to suggest that differences between the two groups are minimal. Before The Bareback Project was implemented, the principal investigator conducted a large-scale content analysis with a random national sample of one of the main websites used by men to meet other men seeking unprotected sex partners [19,36,37]. The demographic composition of that sample and the one obtained in The Bareback Project closely match one another in terms of age representation, racial group composition, sexual orientation, and rural/suburban/urban location of residence. The two samples also resemble one another closely in terms of the types of sexual practices that men sought. The similarity of the two samples suggests that men who chose to participate in the present study represent those who did not, in terms of identifiable characteristics that are likely to be the best indicators of selection bias. Despite these similarities, the participation rate remains on the low side and thus represents a potential limitation for generalizability.
Second, as with most research data on sexual behaviors, the data in this study are based on uncorroborated self-reports. Therefore, it is unknown whether participants underreported or overreported their involvement in risky behaviors. The self-reported data probably can be trusted, however, as noted by other authors of previous studies with similar populations [38]. This is particularly relevant for self-reported measures that involve relatively small occurrences (e.g., number of times having a particular kind of sex during the previous 30 days), which characterize the substantial majority of the data collected in this study [39]. Other researchers have also commented favorably on the reliability of self-reported information in their studies regarding topics such as condom use [40].
A third potential limitation is the possibility of recall bias. For most of the measures used, respondents were asked about their beliefs, attitudes, and behaviors during the past 30 days. This time frame was chosen specifically: 1) to incorporate a large enough time frame in order to facilitate meaningful variability from person to person, and 2) to minimize recall bias. Although the authors cannot determine the exact extent to which recall bias affected the data, other researchers who have used similar measures have reported that recall bias is sufficiently minimal and that its impact upon study findings is likely to be negligible [41]. This seems to be especially true when the recall period is small [42,43], as was the case for most of the main measures used in the present study.
Despite these potential limitations, the present authors believe that the current study has much to offer. As hypothesized, condom-related attitudes were associated (consistently and inversely) with men’s sexual risk practices. They were, in fact, the single strongest factor related to HIV risk identified in the structural equation model depicted in Figure 2. Reducing HIV risk in this population will depend heavily on finding ways to change how men feel about using condoms. The data indicate an important difference between men’s attitudes about condoms in general and their attitudes about using them personally. Although men in the sample had weakly-positive attitudes about condoms overall, their attitudes about using condoms themselves were considerably more negative. In other words, the men were not opposed to condoms ideologically; they simply preferred not to use condoms themselves.
Thus, intervention strategies must consider the question of how to make condoms more appealing and less unpleasant to men who prefer intentional condomless sex. Previous research suggests that highlighting the sexual/sensory aspects of condoms and eroticizing safer sex might help increase condom use among MSM [7]. Indeed, when asked in the present study how they felt about the statement, “Many people make using condoms an erotic part of foreplay,” men’s responses were very divided (see Table 1), suggesting the possibility of making inroads in this area. Specific strategies to eroticize safer sex for members of this target population need to be developed, implemented, and subsequently tested for effectiveness. A number of community-based HIV prevention, education, and intervention programs around the United States have offered workshops about eroticizing safer sex, in an effort to teach members of the MSM community about specific strategies that can be undertaken to make condom use and other safer sex strategies more palatable. Programs such as those offered by Gay Men’s Health Crisis in New York City [44], the Howard Brown Health Center in Chicago, and Project ARK in St. Louis are to be applauded, as are community-specific approaches such as AIDS Project Los Angeles’ Red Circle Project (targeting safer sex among Native Americans) and Bockting, Rosser, and Scheltema’s [45] program targeting safer sex among transgendered persons. Likewise, in recent years, websites dedicated to promoting erotic safer sex have begun to appear on the Internet, and we believe that they offer great promise in combating HIV risk-taking among MSM. An excellent example of this may be found on the Washington, DC-based group’s DCFukit website, at www.dcfukit.org. Finding innovative ways to eroticize safer sex may be an important approach to changing how MSM think about condom use, and that, in turn, is likely to be an effective way of reducing their involvement in risky sexual practices.
One approach to accomplishing this may be to develop Internet-based prevention and intervention programs targeting the MSM community, as recent evidence has suggested that this approach may be effective in decreasing risk in this population. For example, Bowen and colleagues [46,47] tested the feasibility, acceptability, and efficacy of an Internet-based HIV prevention intervention targeting MSM in rural communities. Their preliminary findings indicated community support for such an intervention, with MSM in the study reporting reduced anal sex and increased condom usage. Likewise, another Internet-based prevention intervention among MSM demonstrated reductions in sexual contact with partners who were HIV-positive or HIV-serostatus-unknown [48]. Internet-based prevention/intervention approaches may be particularly apropos with populations similar to that involved in the present study because these men were using the Internet actively to find partners for unsafe sex.
The present study also identified several specific factors that were associated with men’s attitudes toward condom use. We wish to discuss the implications of some of these findings. First, we discovered that men who said that they did not care whether their sex partners were HIV-positive or HIV-negative had more negative attitudes toward condom use overall than their counterparts who did care about their sex partners’ HIV serostatus. In other research as well, a partner’s indication of HIV serostatus has been shown to be linked to condom use attitudes and behaviors among MSM [5,49]. Intervention programs working with MSM need to emphasize the importance of considering one’s partners’ HIV serostatus as one makes decisions regarding the types of sexual behaviors in which one is/not willing to engage. Intervention messages need to emphasize the importance of considering condom use and other safer sex strategies for men who engage in sex with serodiscordant partners.
Along the same lines, the present study found that, the more accurate men perceived HIV information supplied by would-be sex partners to be, the more negative their condom-related attitudes tended to be. This finding suggests that men who ask their partners about their HIV serostatus prior to having sex are apt to rely upon that information, supplanting it for their general feelings about using condoms. If their partners tell them that they are HIV-negative, then our findings suggest that the men accept this verbal information and act accordingly. Although we believe that it is important to discuss sexual partners’ HIV serostatus, this strategy does not ensure protection from HIV transmission. HIV prevention strategies targeting MSM should, therefore, emphasize the importance of making decisions on the basis of personal safety and protection without relying primarily upon a partner’s word, especially if that partner is not well known by the individual in question.
This study also found that attitudes toward condom use were more positive among African American men than they were among men belonging to other racial/ethnic groups. This finding, coupled with the lower overall rates of condom use practiced by Caucasian men (see Figure 2), suggests a need to target Caucasian men in future prevention, education, and risk reduction intervention efforts. A number of published studies have reported on racial differences in HIV risk-taking among MSM [50–52], leading some authors to advocate culturally-specific targeted interventions. Our own research findings suggest a need to target Caucasian MSM, particularly those using the Internet to identify partners for unprotected sex, and to develop strategies that can be effective at modifying how these men feel about using condoms.
In conclusion, the present study found that attitudes toward condom use among MSM seeking partners for unprotected sex via the Internet are the single strongest factor associated with men’s involvement in risky sex. HIV risk reduction efforts need to find ways to change the way that men feel about using condoms. They need to change the prevalent notions that condoms are unpleasant to use, that they reduce sexual pleasure, that they interrupt foreplay, and that putting them on a sex partner cannot be an erotic act–all notions that were commonplace in the men participating in this study. It is important to bear in mind that condom use attitudes do not exist or develop in isolation. The factors that help shape them (which the present study’s findings suggest may be race/ethnicity, caring about sex partners’ HIV serostatus, educational attainment, substance use/abuse problems, and level of self-esteem) can lead researchers toward successful prevention intervention strategies.
Social science implications
Sexual behavior and sexual risk are social and/or interpersonal by nature and cannot be examined in a contextual vacuum. Although MSM were asked individually about their sexual behaviors and attitudes, sexual behaviors themselves take place in a complex social environment. Public health strategies can appear to be at odds with an individual’s choices when making personal decisions about sexual behavior. Social scientists strive to understand the social determinants of health in an effort to mitigate the impact of HIV/AIDS.
However, the importance of psychosocial functioning can, inadvertently, become secondary to disease prevention. Social scientists must seek ways to balance individuals’ sexual and psychosocial needs with the larger public’s health and safety. Understanding condom use attitudes and other psychosocial measures of functioning simultaneously can improve our ability to enhance individual-level and societal-level health and to address the needs of individuals more adequately. Condom use attitudes can offer clues about individuals’ choices according to their social, emotional, psychological, and sexual needs. These ways of examining risk behavior and HIV transmission prevention are not applicable exclusively to MSM seeking unprotected anal intercourse (UAI). Rather, they apply across populations and are particularly relevant for discussions about decision-making processes and models such as Empowerment Theory, the Theory of Reasoned Action, and the Health Belief Model. For MSM seeking UAI, the perceived benefits of having UAI outweigh the perceived risks.
Actively seeking unprotected sex indicates a tipping of the risk/benefit scales in favor of more risk, according to health researchers and prevention specialists [53]. However, ‘safe’ and ‘risk’ are subjective terms that are defined relatively, according to individuals’ needs, desires, and preferences. As social scientists, our goal is not to pathologize behaviors, such as actively seeking unprotected sex, as was the focus of this study of MSM. Instead, our efforts should include psychosocial factors and the social determinants of health that correlate with condom use and attitudes toward using condoms. Failing to do so would be a failure to understand individuals and groups comprehensively, particularly from a social science perspective on behavior that is social and/or interpersonal in nature. The findings of this study support the Health Belief Model in that MSM in the sample held beliefs about condom use that directly corresponded to their sexual risk practices. As noted, in order to promote health by reducing HIV transmission in this high-risk population, it is essential for men to change the way they view personal condom use. This, however, must be approached within the broader context of an individual’s needs and psychosocial health.
Acknowledgments
This research was supported by a grant from the National Institute on Drug Abuse (5R24DA019805). The authors wish to acknowledge, with gratitude, the contributions made to this study’s data collection and data entry/cleaning functions by Thomas P. Lambing.
References
- 1.Levy JA. HIV and the pathogenesis of AIDS. 3. Washington, DC: ASM Press; 2007. [Google Scholar]
- 2.Ostrow DG, Silverberg MJ, Cook RL, Chmiel JS, Johnson L, Li X, Jacobson LP. Prospective study of attitudinal and relationship predictors of sexual risk in the Multicenter AIDS Cohort Study. AIDS Behav. 2008;12:127–38. doi: 10.1007/s10461-007-9223-x. [DOI] [PubMed] [Google Scholar]
- 3.Bakeman R, Peterson JL Community Intervention Trial for Youth Study Team. Do beliefs about HIV treatments affect peer norms and risky sexual behaviour among African-American men who have sex with men? Int J STD AIDS. 2007;18:105–8. doi: 10.1258/095646207779949637. [DOI] [PubMed] [Google Scholar]
- 4.Peterson JL, Rothenberg R, Kraft JM, Beeker C, Trotter R. Perceived condom norms and HIV risks among social and sexual networks of young African American men who have sex with men. Health Educ Res. 2009;24:119–27. doi: 10.1093/her/cyn003. [DOI] [PubMed] [Google Scholar]
- 5.Carballo-Diéguez A, Miner M, Dolezal C, Rosser BR, Jacoby S. Sexual negotiation, HIV-status disclosure, and sexual risk behavior among Latino men who use the Internet to seek sex with other men. Arch Sex Behav. 2006;35:473–81. doi: 10.1007/s10508-006-9078-7. [DOI] [PubMed] [Google Scholar]
- 6.Nakamura N, Mausbach BT, Ulibarri MD, Semple SJ, Patterson TL. Methamphetamine use, attitudes about condoms, and sexual risk behavior among HIV positive men who have sex with men. Arch Sex Behav. 2011;40:267–72. doi: 10.1007/s10508-009-9566-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scott-Sheldon LA, Marsh KL, Johnson BT, Glasford DE. Condoms + pleasure = safer sex? A missing addend in the safer sex message. AIDS Care. 2006;18:750–4. doi: 10.1080/09540120500411073. [DOI] [PubMed] [Google Scholar]
- 8.Neville S, Adams J. Condom use in men who have sex with men: A literature review. Contemp Nurse. 2009;33:130–9. doi: 10.5172/conu.2009.33.2.130. [DOI] [PubMed] [Google Scholar]
- 9.Bauermeister JA, Carballo-Diéguez A, Ventuneac A, Dolezal C. Assessing motivations to engage in intentional condomless anal intercourse in HIV risk contexts (“Bareback Sex”) among men who have sex with men. AIDS Educ Prev. 2009;21:156–68. doi: 10.1521/aeap.2009.21.2.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holmes D, Warner D. The anatomy of a forbidden desire: men, penetration and semen exchange. Nurs Inq. 2005;12:10–20. doi: 10.1111/j.1440-1800.2005.00252.x. [DOI] [PubMed] [Google Scholar]
- 11.Balán IC, Carballo-Diéguez A, Ventuneac A, Remien RH. Intentional condomless anal intercourse among Latino MSM who meet sexual partners on the Internet. AIDS Educ Prev. 2009;21:14–24. doi: 10.1521/aeap.2009.21.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carballo-Diéguez A, Bauermeister J. “Barebacking”: intentional condomless anal sex in HIV-risk contexts. Reasons for and against it. J Homosex. 2004;47:1–16. doi: 10.1300/J082v47n01_01. [DOI] [PubMed] [Google Scholar]
- 13.Nodin N, Carballo-Diéguez A, Ventuneac AM, Balan IC, Remien R. Knowledge and acceptability of alternative HIV prevention bio-medical products among MSM who bareback. AIDS Care. 2008;20:106–15. doi: 10.1080/09540120701449096. [DOI] [PubMed] [Google Scholar]
- 14.Whittier DK, StLawrence J, Seeley S. Sexual risk behavior of men who have sex with men: Comparison of behavior at home and at a gay resort. Arch Sex Behav. 2005;34:95–102. doi: 10.1007/s10508-005-1003-y. [DOI] [PubMed] [Google Scholar]
- 15.Berg RC. Barebacking among MSM Internet users. AIDS Behav. 2008;12:822–33. doi: 10.1007/s10461-007-9281-0. [DOI] [PubMed] [Google Scholar]
- 16.Grov C, DeBusk JA, Bimbi DS, Golub SA, Nanin JE, Parsons JT. Barebacking, the Internet, and harm reduction: an intercept survey with gay and bisexual men in Los Angeles and New York City. AIDS Behav. 2007;11:527–36. doi: 10.1007/s10461-007-9234-7. [DOI] [PubMed] [Google Scholar]
- 17.Liau A, Millett G, Marks G. Meta-analytic examination of online sex-seeking and sexual risk behavior among men who have sex with men. Sex Transm Dis. 2006;33:576–84. doi: 10.1097/01.olq.0000204710.35332.c5. [DOI] [PubMed] [Google Scholar]
- 18.McKirnan D, Houston E, Tolou-Shams M. Is the web the culprit? Cognitive escape and Internet sexual risk among gay and bisexual men. AIDS Behav. 2007;11:151–60. doi: 10.1007/s10461-006-9084-8. [DOI] [PubMed] [Google Scholar]
- 19.Klein H. HIV risk practices sought by men who have sex with other men, and who use Internet websites to identify potential sexual partners. Sex Health. 2008;5:243–50. doi: 10.1071/sh07051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bolding G, Davis M, Hart G, Sherr L, Elford J. Where young MSM meet their first sexual partner: The role of the Internet. AIDS Behav. 2007;11:522–6. doi: 10.1007/s10461-007-9224-9. [DOI] [PubMed] [Google Scholar]
- 21.Horvath KJ, Nygaard K, Rosser BRS. Ascertaining partner HIV status and its association with sexual risk behavior among Internet-using men who have sex with men. AIDS Behav. 2010;14:1376–83. doi: 10.1007/s10461-009-9633-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Singer M. Introduction to syndemics: A systems approach to public and community health. San Francisco, CA: Jossey-Bass; 2009. [Google Scholar]
- 23.Singer MC, Erickson PI, Badiane L, Diaz R, Ortiz D, Abraham T, Nicolaysen AM. Syndemics, sex and the city: Understanding sexually transmitted diseases in social and cultural context. Soc Sci Med. 2006;63:2010–21. doi: 10.1016/j.socscimed.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Walkup J, Blank MB, Gonzales JS, Safren S, Schwartz R, Brown L, Wilson I, Knowlton A, Lombard F, Grossman C, Lyda K, Schumacher JE. The impact of mental health and substance abuse factors on HIV prevention and treatment. J Acquir Immune Defic Syndr. 2008;47:S15–9. doi: 10.1097/QAI.0b013e3181605b26. [DOI] [PubMed] [Google Scholar]
- 25.Romero-Daza N, Weeks M, Singer M. “Nobody gives a damn if I live or die”: Violence, drugs, and street-level prostitution in inner-city Hartford, Connecticut. Med Anthropol. 2003;22:233–59. doi: 10.1080/01459740306770. [DOI] [PubMed] [Google Scholar]
- 26.Gielen AC, Ghandour RM, Burke JG, Mahoney P, McDonnell KA, O’Campo P. HIV/AIDS and intimate partner violence: Intersecting women’s health issues in the United States. Trauma Violence Abuse. 2007;8:178–98. doi: 10.1177/1524838007301476. [DOI] [PubMed] [Google Scholar]
- 27.Mustanski B, Garofalo R, Herrick A, Donenberg G. Psychosocial health problems increase risk for HIV among urban young men who have sex with men: Preliminary evidence of a syndemic in need of attention. Ann Behav Med. 2007;34:37–45. doi: 10.1080/08836610701495268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brown IS. Development of a scale to measure attitude toward the condom as a method of birth control. J Sex Res. 1984;20:255–63. [Google Scholar]
- 29.Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- 30.Von Diemen L, Szobot CM, Kessler F, Pechansky F. Adaptation and construction of the Barratt Impulsiveness Scale BIS 11 to Brazilian Portuguese for use in adolescents. Rev Bras Psiquiatr. 2007;29:153–6. doi: 10.1590/s1516-44462006005000020. [DOI] [PubMed] [Google Scholar]
- 31.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 32.Scheier MF, Carver CS. Optimism, coping, and health: Assessment and implications of generalized outcome expectancies. Health Psychol. 1985;4:219–47. doi: 10.1037//0278-6133.4.3.219. [DOI] [PubMed] [Google Scholar]
- 33.Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. J Pers Assess. 1985;49:71–5. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- 34.Carey MP, Morrison-Beedy D, Johnson B. The HIV-Knowledge Questionnaire: Development and evaluation of a reliable, valid, and practical self-administered questionnaire. AIDS Behav. 1997;1:61–74. [Google Scholar]
- 35.Bernstein DP, Fink L. Childhood Trauma Questionnaire: A retrospective self-report manual. San Antonio, TX: Psychological Corporation; 1998. [Google Scholar]
- 36.Klein H. Differences in HIV risk practices sought by self-identified gay and bisexual men who use Internet websites to identify potential sexual partners. J Bisex. 2008;9:125–40. doi: 10.1080/15299710902881533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Klein H. Sexual orientation, drug use preference during sex, and HIV risk practices and preferences among men who specifically seek unprotected sex partners via the Internet. Int J Environ Res Publ Health. 2009;6:1620–35. doi: 10.3390/ijerph6051620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schrimshaw EW, Rosario M, Meyer-Bahlburg HFL, Scharf-Matlick AA. Test-retest reliability of self-reported sexual behavior, sexual orientation, and psychosexual milestones among gay, lesbian, and bisexual youths. Arch Sex Behav. 2006;35:225–34. doi: 10.1007/s10508-005-9006-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bogart LM, Walt LC, Pavlovic JD, Ober AJ, Brown N, Kalichman SC. Cognitive strategies affecting recall of sexual behavior among high-risk men and women. Health Psychol. 2007;26:787–93. doi: 10.1037/0278-6133.26.6.787. [DOI] [PubMed] [Google Scholar]
- 40.Morisky DE, Ang A, Sneed CD. Validating the effects of social desirability on self-reported condom use behavior among commercial sex workers. AIDS Educ Prev. 2002;14:351–60. doi: 10.1521/aeap.14.6.351.24078. [DOI] [PubMed] [Google Scholar]
- 41.Kauth MR, StLawrence JS, Kelly JA. Reliability of retrospective assessments of sexual HIV risk behavior: A comparison of biweekly, three-month, and twelve-month self-reports. AIDS Educ Prev. 1991;3:207–14. [PubMed] [Google Scholar]
- 42.Fenton KA, Johnson AM, McManus S, Erens B. Measuring sexual behaviour: Methodological challenges in survey research. Sex Transm Infect. 2001;77:84–92. doi: 10.1136/sti.77.2.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Weir SS, Roddy RE, Zekeng L, Ryan KA. Association between condom use and HIV infection: A randomised study of self reported condom use measures. J Epidemiol Community Health. 1999;53:417–22. doi: 10.1136/jech.53.7.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Palacios-Jimenez L, Shernoff M. Facilitator’s guide to eroticizing safer sex: A psychoeducational workshop approach to safer sex education. New York: Gay Men’s Health Crisis; 1986. [Google Scholar]
- 45.Bockting WO, Rosser BRS, Scheltema K. Transgender HIV prevention: Implementation and evaluation of a workshop. Health Educ Res. 1999;14:177–83. doi: 10.1093/her/14.2.177. [DOI] [PubMed] [Google Scholar]
- 46.Bowen AM, Horvath K, Williams ML. A randomized control trial of Internet-delivered HIV prevention targeting rural MSM. Health Educ Res. 2007;22:120–7. doi: 10.1093/her/cyl057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bowen AM, Williams ML, Daniel CM, Clayton S. Internet based HIV prevention research targeting rural MSM: Feasibility, acceptability, and preliminary efficacy. J Behav Med. 2008;31:463–77. doi: 10.1007/s10865-008-9171-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Carpenter KM, Stoner SA, Mikko AN, Dhanak LP, Parsons JT. Efficacy of a web-based intervention to reduce sexual risk in men who have sex with men. AIDS Behav. 2010;14:549–57. doi: 10.1007/s10461-009-9578-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Horvath KJ, Oakes JM, Rosser BR. Sexual negotiation and HIV serodisclosure among men who have sex with men with their online and offline partners. J Urban Health. 2008;85:744–58. doi: 10.1007/s11524-008-9299-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Millett GA, Flores SA, Peterson JL, Bakeman R. Explaining disparities in HIV infection among black and white men who have sex with men: A meta-analysis of HIV risk behaviors. AIDS. 2007;21:2083–91. doi: 10.1097/QAD.0b013e3282e9a64b. [DOI] [PubMed] [Google Scholar]
- 51.Mutchler MG, Bogart LM, Elliott MN, McKay T, Suttorp MJ, Schuster MA. Psychosocial correlates of unprotected sex without disclosure of HIV-positivity among African-American, Latino, and White men who have sex with men and women. Arch Sex Behav. 2008;37:736–47. doi: 10.1007/s10508-008-9363-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rhodes SD, Yee LJ, Hergenrather KC. A community-based rapid assessment of HIV behavioural risk disparities within a large sample of gay men in southeastern USA: A comparison of African American, Latino, and white men. AIDS Care. 2006;18:1018–24. doi: 10.1080/09540120600568731. [DOI] [PubMed] [Google Scholar]
- 53.Adam PC, Murphy DA, de Wit JB. When do online sexual fantasies become reality? The contribution of erotic chatting via the Internet to sexual risk-taking in gay and other men who have sex with men. Health Educ Res. 2011;26:506–15. doi: 10.1093/her/cyq085. [DOI] [PubMed] [Google Scholar]