Abstract
Objective
This study aimed to examine implementation feasibility and initial treatment outcomes of a behavioral activation based treatment for adolescent depression, the Adolescent Behavioral Activation Program (A-BAP).
Method
A randomized, controlled trial was conducted with 60 clinically referred adolescents with a depressive disorder who were randomized to receive either 14 sessions of A-BAP or uncontrolled evidenced-based practice for depression (EBP-D). The urban sample was 64% female, predominantly Non-Hispanic White (67%) and had an average age of 14.9 years. Measures of depression, global functioning, activation and avoidance were obtained through clinical interviews and/or through parent and adolescent self-report at pre-intervention and end of intervention.
Results
Intent-to-treat linear mixed effects modeling and logistic regression analysis revealed that both conditions produced statistically significant improvement from pre- to end of treatment in depression, global functioning and activation and avoidance. There were no significant differences across treatment conditions.
Conclusions
These findings provide the first step in establishing the efficacy of BA as a treatment for adolescent depression and support the need for ongoing research on BA as a way to enhance the strategies available for treatment of depression in this population.
Keywords: Depression, Treatment, Randomized Controlled Trial
Depression during adolescence is a major public health problem (Lopez, Mathers, Ezzati, Jamison, & Murray, 2006). It is prevalent and associated with high rates of relapse during adolescence and recurrence during adulthood (Costello, Egger, & Angold, 2005; Dunn & Goodyer, 2006; Goodyer, Herbert, Tamplin, & Altham, 2000; Hankin et al., 1998; Lewinsohn, Rohde, Seeley, Klein, & Gotlib, 2000). Depression during adolescence is also linked with increased risk of impaired academic performance, poor peer and family relationship quality, substance abuse, and suicidality (Copeland, Shanahan, Costello, & Angold, 2009; Esposito & Clum, 2002; Keenan-Miller, Hammen, & Brennan, 2007; Marmorstein, 2009; McCarty et al., 2012). These far reaching consequences underscore the importance of access to effective interventions to treat acute symptoms and reduce risk of relapse and recurrence. This paper describes the development and initial investigation of behavioral activation (BA) as a treatment for depression during adolescence.
Both cognitive behavioral therapy (CBT) and interpersonal therapy (IPT), adapted for use with adolescents, have demonstrated efficacy in the treatment of adolescent depression. However, effect sizes are modest (Weisz, McCarty, & Valeri, 2006) and residual symptoms remain problematic even among responders (Kennard et al., 2006; Kennard et al., 2009; Mufson, Dorta, Moreau, & Weissman, 2011; Mufson, Weissman, Moreau, & Garfinkel, 1999; Rosselló & Bernal, 1999; TADS Team, 2007). Furthermore, important subgroups of adolescents, such as those exposed to early life adversity, demonstrate poor response to existing treatments (Lewis et al., 2010; Nanni, Uher, & Danese, 2012).
Treatment response for depressed adolescents may be improved by targeting specific functional deficits unique to some adolescents who present with depressive symptoms (Forbes, 2009; Forbes et al., 2006). Neurodevelopmental data suggests that adolescents are vulnerable to increased sensitivity to social stressors, disruptions in reward processing, and the tendency to shut down or avoid emotional stimuli (Forbes, 2009; Forbes et al., 2006; Hare et al., 2008; Silk et al., 2007; Somerville, Hare, & Casey, 2011; Tottenham, Hare, & Casey, 2011). Reward processing deficits, a physiological change associated with risk for depression, may increase during adolescence because neural reward systems are still developing (Davey, Yucel, & Allen, 2008; Forbes, 2009). These research findings on disengagement and avoidance suggest that treatment for adolescent depression may need to target adolescents’ ability both to experience and respond to reward, and overcome avoidance (Forbes, 2009). This argument is underscored by recent findings that anhedonia is the strongest predictor, among all depressive symptoms, of increased time to remission and therefore represents an important treatment target (McMakin et al., 2012). Given that BA focuses on context, and targets environmental stressors such as social relationships, overcoming avoidance and increasing engagement with reinforcers within the environment, it may offer an important approach to the treatment of depressed adolescents.
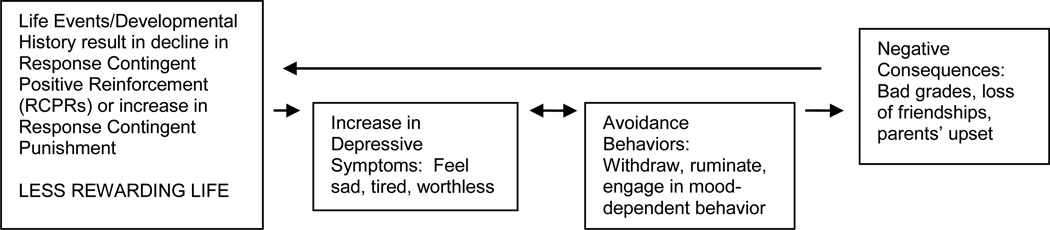
BA therapy is based on a functional analytic model of depression (see Figure 1) with two central assumptions (Ferster, 1973; Lewinsohn, 1974, 2001): 1) the experience of response contingent positive reinforcement is necessary to maintain normal mood; and 2) avoidance is common and serves as a barrier to engaging in antidepressant behavior that could naturally be positively reinforced. In this model, context is carefully assessed to determine factors that are contributing to and maintaining depressive behaviors and what behaviors/events are required to curtail it. Avoidance behavior often offers short-term symptom relief, but is maintained via negative reinforcement and contributes to the persistence of depression in the long run. While functional avoidance was recognized as central to depression in the early 1970s (Ferster, 1973), other treatments for depression have not identified avoidance as a primary treatment target, making the focus on avoidance in BA unique. CBT (Beck, Rush, Shaw, & Emery, 1979) includes an emphasis on scheduling pleasant and mastery activities, a form of behavioral activation, primarily as a foundation for cognitive interventions that focus on modifying distortions in thinking. In BA, activation differs from simple activity scheduling in that its focus centers on identifying behaviors that a) are important within the individual’s context, b) advance the individual’s goals and experience of mastery or pleasure, and c) counter avoidance. Although IPT (Mufson et al., 2011) may indirectly address avoidance with its attention to improving communication with important individuals in one’s life, overcoming avoidance is not a core treatment target. Studies with adults have suggested that BA is an efficacious treatment for depression (Dimidjian et al., 2006), with positive results across multiple patient populations, settings, and delivery formats (Dimidjian, Barrera, Martell, Muñoz, & Lewinsohn, 2011).
Figure 1.
Behavioral Activation Model of Depression
Preliminary findings suggest that the BA approach also holds promise as an effective treatment for adolescent depression (Chu, Colognori, Weissman, & Bannon, 2009; Jacob, Keeley, Ritschel, & Craighead, 2013; Ritschel, Ramirez, Jones & Craighead, 2011). Our study extended this research with a pilot randomized trial comparing the Adolescent Behavioral Activation Program (A-BAP) to evidence based practice for depression (EBP-D) within a university hospital based community mental health clinic. We addressed three specific aims. First, determine the feasibility of: a) adequate participant recruitment and enrollment; b) successful randomization across treatment conditions; and c) retention of participants during treatment and follow-up. Second, establish “proof of concept” by determining if the BA approach was associated with clinically meaningful reductions in depressive symptoms and improvements in global functioning that were comparable to a stringent comparison condition. We anticipated that youth in the BA condition would demonstrate a significant reduction in depressive symptoms on the Children’s Depression Rating Scale-Revised (CDRS-R; Poznanski & Mokros, 2001) and scores of 1–2 on the Clinical Global Impression Improvement Scale (CGI; Guy, 1976) and that such gains would be at least as good as those in EBP-D. Thus in this context, findings consistent with the null hypothesis (BA = EBP-D) would be acceptable and support further research. Our third specific aim was to conduct an initial exploration of change in activation and avoidance (potential mediators of change in the BA model.
Development of the A-BAP Intervention with Adolescents
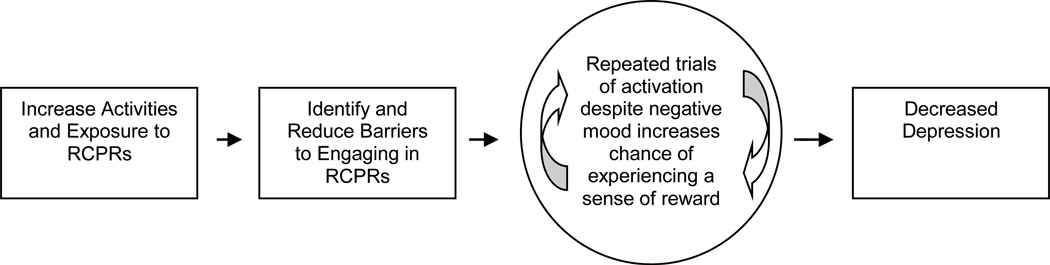
Based on open trial pilot testing with eight depressed adolescents, we developed a 12-week, 14-session treatment program for depressed youth aged 12–18. This program tested a proposed model of change for adolescents diagnosed with depression, as outlined in Figure 2, which posits that: a) as barriers to activation are identified and addressed, the adolescent’s ability to fully engage in activities and experience response contingent, positive reinforcement (RCPR) will be enhanced, b) repeated trials of activation, despite negative mood, will increase the likelihood that these activities will be experienced as positively reinforcing, and c) when activities are experienced as contingently positively reinforced, this in turn will lead to improved depressive symptoms. We designed our approach to include intervention components (e.g., activities designed to promote competence, psychoeducation regarding depression, outline of details of treatment, self-monitoring of moods and behaviors, etc.) that have been found to be elements in beneficial treatments (McCarty & Weisz, 2007).
Figure 2.
Proposed Behavioral Activation Model of Change
Method
Participants
Participants were recruited from a major metropolitan area on the West Coast via a hospital-based mental health clinic, referrals from primary care and/or mental health care providers, and flyers placed in health clinics and school newspapers. Inclusion criteria included: a) age 12–18 with one parent/guardian willing to participate; b) primary DSM-IV diagnosis of Major Depression, Depression Not Otherwise Specified, or Dysthymia, or a raw score of 45 (T-score of 65) or greater on the CDRS-R; c) self-report score of 11 or greater on the Short Moods and Feelings Questionnaire (SMFQ; Angold et al., 1995) at the start of treatment; and d) willingness to be randomized to treatment condition. Exclusion criteria included: inability to complete study questionnaires, psychotic or manic symptoms, acute substance use, suicidality requiring immediate, intensive treatment, and/or acute medical illness. Youth who met inclusion criteria, but were taking stimulant medications for ADHD or were on a stable antidepressant medication regimen were included. The study was approved by the Institutional Review Board (IRB), and all participants including a parent/guardian completed and signed IRB approved assent/consent forms before beginning the initial evaluation process. Youth who were eligible and gave assent, completed a clinic-based, comprehensive intake evaluation. Youth who were ineligible or declined participation in the study were offered treatment referrals outside the study. The study was registered with clinicaltrials.gov (ID number NCT01137149).
Procedures
Enrolled participants (N = 60) were randomly assigned to BA (n = 35) or EBP-D (n = 25). A computerized program was used to randomly assign participants to treatment group. This program used a stratified randomization scheme, where randomization was stratified based on age (categorically 11–14 yrs of age, 15–18 years of age) and gender with weighting to allow for greater inclusion in the BA group. Youth participants received a $25 incentive for completing the baseline and end-of-treatment assessment batteries. In each treatment condition, participants received up to 14 sessions of therapy over the course of a 12-week period.
A-BAP intervention
Our modification of BA for use with depressed adolescents can best be conceptualized as a behavioral treatment based on a functional conceptualization of each individual case. In an effort to adequately engage adolescents in treatment, the program utilized a structured psychoeducational format early in the treatment process, with a more flexible approach as treatment progressed. Treatment began with two sessions devoted to reviewing the assessment-based case conceptualization and introducing the BA model to the adolescent alone and then in the second session with the adolescent and parent together, followed by a series of sessions introducing particular skills (see Table 1). Four additional sessions were scheduled, either as needed to extend the skill modules or after introduction of all the skills, to allow for individualized practice and application. The treatment ended with two sessions devoted to termination and relapse prevention. Although treatment was structured to follow the order seen in Table 1, therapists had the discretion to tailor the sequence as appropriate to the adolescent’s needs. Functional analysis of behavior was introduced in the “Getting Active” sessions. As part of this functional analysis the role of reinforcement in maintaining behavior, including the importance of evaluating the payoff versus the price of behavior choices while considering both short- and long-term consequences of behavioral choices, was introduced. For the associated homework or practice, each adolescent was asked to identify at least one behavior/activity that they associated with feeling less depressed, structure time to engage in this over the week, and monitor the effect on his/her mood. In the core skills sessions, each skill was introduced using structured materials that built on and integrated examples drawn from each adolescent’s unique circumstances and priorities. Adolescents were encouraged to identify their own issues and actively engage in elucidating how each skill applied to their situation. Role-playing was used in some cases, while in all cases the skills were presented in the context of an example from the adolescent’s life. Homework or practice, assigned in each session, reflected the material covered in the session and included: monitoring behaviors and their association with mood, taking steps toward goals, identifying barriers, and testing out strategies to overcome avoidance and other barriers. In the less structured sessions each adolescent identified the key area(s) he or she wanted to work on (e.g., spending more time with friends), and with the therapist’s guidance employed skills from prior sessions to address the identified problem or reach the adolescent’s goal. Guidelines for each session are summarized in a treatment manual that is available from the authors.
Table 1.
Content of BA Sessions
| Sessions | Content Areas | Specific Topics |
|---|---|---|
| 1–2 | Case Conceptualization and Introduction to BA Model |
Introduction to the BA Model (“Getting Started”) |
| 3–4 | Activation & Goal-Directed Behavior |
|
| 5–8 | Core Skills |
|
| 9–12 | Practice and Application | All of the above |
| 13–14 | Relapse Prevention and Termination |
|
Parents participated in at least two of the BA sessions. This allowed: a) parents an opportunity to provide the therapist with their perspective on the adolescent’s depression; b) adolescents an opportunity to describe the behavioral model used in therapy to the parent as a means of consolidating the adolescent’s grounding in the model; and c) parents an opportunity to get “on board” with the adolescent’s work in BA such that they could reinforce appropriate behaviors and support therapeutic strategies and gains.
Evidence Based Practice for Depression (EBP-D)
Our comparison condition represents standard care offered in an academically affiliated outpatient clinic setting. EBP-D relied on a Cognitive Behavioral Therapy (CBT) approach in most cases (n = 21), and an Interpersonal Therapy for Adolescents (IPT-A) approach in a smaller subset of cases (n = 4). Although no specified manual was prescribed, all therapists had prior formal training in one or both of these therapeutic techniques, and routinely employed one of these therapies as part of their standard care. Therapists were chosen to participate based on experience in providing these treatments. To ensure consistent dose of treatment between conditions, the study provided up to 14 sessions of therapy. Both patient and therapist were aware of this at the start of therapy and planned treatment accordingly.
EBP-D therapists had the option to include parents in treatment “as needed,” but could not engage parents in independent treatments (e.g., initiating an additional parent training protocol, working with parents on individual adult/parent treatment issues). Therapists, in both conditions, also had the option to offer a limited number of additional sessions, if needed, to allow for a smooth termination of treatment.
Therapists
Therapists provided treatment in either A-BAP or EBP-D, but not both, so as not to bias results. A-BAP therapists included two postdoctoral fellows, two faculty/staff psychologists, and one MSW; four women and one man, one was Asian-American and the remaining were European-American. A larger cadre of therapists delivered the EBP-D intervention, including one advanced level graduate student, three postdoctoral fellows, four faculty/staff psychologists, one faculty/staff psychiatrist, and one MSW. In this group four were men, and all were European-American. The BA therapists completed a one-day training program and then met weekly for group supervision throughout the study. The EBP-D therapists were recruited from the general clinic staff and did not receive additional study training. Because of clinic space limitations, most treatment sessions took place in a research center outside the clinic. Scheduling for this space precluded overlap of therapists from different treatment arms and none of the clients were included in discussions at care conferences. For the EBP-D condition one of the faculty psychologists participating in that condition was available to clinicians for case consultation and guidance as needed. All participating therapists were asked to refrain from cross–condition discussion, which was easily accomplished since most therapists did not have overlapping clinical days. The postdoctoral fellows in both conditions came from varied academic training programs although all had completed their internship training within the affiliated university program but not in the same year.
Assessments and Measures
Assessments were completed at baseline and end-of-treatment, with follow-up assessments conducted 6 and 12 months after study enrollment. All assessments examined psychiatric symptomatology, adaptive functioning, activation and avoidance, and academic, social and familial functioning. They were conducted by Independent Clinical Evaluators (ICEs) who were advanced level clinical psychology graduate students and naive to the adolescent’s treatment condition. ICEs completed a training program before administering diagnostic interviews which included: a) an orientation to the evaluation tools, b) the review and rating of two training interview tapes and one in-person interview conducted by the gold standard clinical evaluator (KS), and c) the administration of an interview that was co-rated by the gold-standard clinical evaluator to ensure appropriate reliability prior to independently conducting interviews. Inter-rater reliability at the diagnostic level was required to move into the role of an ICE. As the ICEs were only employed as part of this project, were not working in the clinic on a routine basis, and completed most evaluations after regular clinic hours or on weekends, they had little contact with the therapists in either condition.
Demographics
Participants completed a standard demographics form, and the Hollingshead Four Factor Index of Social Status (Hollingshead, 1975) was used to determine family composite social status. An education score (range 1 to 7), and an occupation score (range 1 to 9) was assigned for each parent/guardian based on information provided by the parent reporter. Education and occupation scores were weighted according to Hollingshead guidelines to obtain a single score for each parent/guardian (range 8 to 66). for families with multiple caregivers, scores for each were averaged to obtain a single socioeconomic status (SES) score.
Clinical symptoms
The Kiddie-SADS Diagnostic Interview (KSADS) (Kaufman et al., 1997), used to establish a diagnosis of depression, is a structured diagnostic interview with established reliability and validity. Selected modules of the KSADS were used to assess depression disorders, Mania, Oppositional Defiant Disorder, Generalized Anxiety Disorder, Overanxious Disorder, and Conduct Disorder.
The Children’s Depression Rating Scale-Revised (CDRS-R; Poznanski & Mokros, 2001) was utilized to assess level of depressive symptomatology. The CDRS-R is a semi-structured interview-based measure modeled on the adult Hamilton Rating Scale for Depression, and has been found to be a sensitive and reliable severity measure of depression in youth (Poznanski & Mokros, 2001). ICEs administered the 17-item scale to both the adolescent and the parent. Item values range from 1 to 5 or 1 to 7, with higher scores reflecting more clinically significant difficulties. A raw score at or above 45 (T-score at or above 65) indicates a likely depressive disorder.
The Clinical Global Impressions/Improvement scale (CGI; Guy, 1976) was used to assess the level of symptom severity at intake and end of treatment. Scores on the CGI range from 1–7, with lower scores denoting less severity/better outcome. The CGI measure has been widely utilized in a number of treatment outcome studies with adolescents (e.g., Mufson et al., 2004; TADS Team, 2004) to assess treatment response with improvement scores of 1 (very much improved) or 2 (much improved) indicating positive response to treatment.
The Short Mood and Feelings Questionnaire (SMFQ; Angold et al., 1995) was used to index self-reported distress, including depressive thoughts, feelings, and behaviors. Items are each scored on a 3-point scale: not true, sometimes true, and true. The 13-item measure has high internal consistency and has been noted to successfully distinguish between children and adolescents with and without depressive disorders (Angold et al., 1995). In the current sample, internal consistency was high (pre-treatment α = .84, end of-treatment α = .95). For inclusion in this study, a categorical cutoff score of 11 was utilized as an indication of significant depressive symptomatology. This cut-off, utilizing adolescent report only was selected based on findings from large scale epidemiological studies (Angold, Erkanli, Silberg, Eaves & Costello, 2002; McKenzie et al., 2011; Patton et al., 2008). One additional question was added to the SMFQ, but not to the overall score, to track level of suicide risk.
The Multidimensional Anxiety Scale for Children (MASC; March, Parker, Sullivan, Stallings, & Conners, 1997) is a self-report questionnaire used to assess the nature and severity of anxiety symptoms. Widely utilized and with adequate psychometric properties (March et al., 1997), the MASC is normed for age and gender, and yields raw and T-scores. Administered at pre-treatment, the MASC Anxiety Disorder Index demonstrated adequate internal consistency (α = .62).
Behavioral function
The Children’s Global Assessment Scale (C-GAS; Shaffer et al., 1983) was administered by ICEs to assess adolescent global functioning and general symptom severity. Based on the adult GAS and modified by Shaffer and colleagues (1983) for use with children and adolescents, the C-GAS is rated on a scale of 0 (poor) to 100 (excellent) and has been shown to have good psychometric properties.
The Behavioral Activation for Depression Scale (BADS; Kanter, Mulick, Busch, Berlin, & Martell, 2007; Kanter, Rusch, Busch, & Sedivy, 2009) is a 25-item self-report measure designed to track changes in proposed mediators of BA: activation and avoidance. The BADS has four subscales, two of which were analyzed in the current study: Activation (focused, goal-directed activation and completion of scheduled activities) and Avoidance/Rumination (avoidance of negative aversive states and engaging in rumination rather than active problem solving). The BADS has been found to have good factor structure, internal consistency, and test-retest reliability (Kanter et al., 2007). In the current study, the BADS demonstrated good overall internal consistency (pre-treatment α = .88; end of treatment α = .91), as well as adequate to good reliability for the subscales examined (Activation: pre-treatment α = .78; end of treatment α = .77; Avoidance/Rumination: pre-treatment α = .84; end of treatment α = .87).
Adherence
BA adherence was rated from video recordings using items based on the Collaborative Study Psychotherapy Rating Scale (Form 6) (CSPRS-6; Evans, Piasecki, Kriss, & Hollon, 1984) and consistent with the Quality of Behavioral Activation Scale (Q-BAS; Dimidjian, Hubley, Martell & Herman-Dunn, in preparation). Items were rated on a 7-point scale (higher ratings indicating greater adherence to BA) and included: sets and follows agenda, maintains an activation focus, reviews homework, assigns homework, attends to client understanding, plans for preventing relapse, assesses cues and consequences of behavior, discusses client avoidance, assesses behavioral patterns, identifies desired behavioral changes, generates or evaluates solutions, provides education about activation principles, encourages self-monitoring, increases pleasure and mastery, schedules activities, structures activities, manipulates behavior via cues or consequences, teaches skills, elicits client practicing new behavior in session, and reestablishes routines.
A team of four raters, including three undergraduate students and one advanced graduate student, underwent approximately 20 hours of training, which involved an orientation to fidelity monitoring, reviewing instructions for rating BA adherence, and two five-hour didactic training sessions that included discussion forums and supervised group practice. Raters were naïve to treatment assignment, session number, and all study hypotheses. All ratings were completed while watching a video recording of the session. Each rater watched and rated each session independently, and met bi-weekly to review sessions jointly rated by all raters. A total of 44 sessions was randomly selected from sessions 3–11 for each patient (n=28 for BA and n=16 for EBP-D). Reliability was calculated based on 14 sessions rated jointly by two raters, and using Shrout and Fleiss’s (1979) fixed effects model, intraclass correlation coefficients (ICCs) were computed, yielding an ICC of .61. BA therapists received significantly higher ratings of adherence to BA (65.47, SD = 14.73) than EBP-D therapists (53.55, SD = 10.37), t(1,42) = 2.85, p = .007 suggesting adequate to strong adherence to the BA model.
Data Management and Analyses
Power calculations were done prior to initiating the study to determine necessary sample size. Given the fact that the BA treatment approach had never been applied to this specific population, power calculations were estimated approximations based on available adolescent treatment studies. Examining studies of CBT and IPT utilizing a “diagnosed” sample of adolescents, effect sizes were reported to range from -.07 to 2.02 (Weisz et al., 2006). Assuming a large effect size of .8 based on these studies, we determined that a proposed sample size of 25 and 25 for the two groups would provide adequate power of 80.1% to yield a statistically significant result, which was in the middle of the above range.
In assessing change over time, consistent with procedures used in the TADS Study (TADS Team, 2003, 2004, 2007), we followed the formula described by Rintelmann and colleagues (1996) to calculate improvement on the CDRS-R. This procedure corrects for the nonzero minimum score of the CDRS-R and, in turn is considered to be a more appropriate method for assessing change. Specifically, the formula used to calculate percent change was: ([baseline CDRS-R score – 17] – [endpoint CDRS-R score – 17])/(baseline CDRS-R score – 17). Descriptive statistics are used to report on feasibility of recruitment, randomization, and retention.
To compare changes in continuous outcomes from pre- to end of treatment, linear mixed effects models were used with intercepts allowed to vary across individual participants. As covariates, treatment condition (0: EBP-D, 1: BA), time (0: pre-treatment, 1: end of treatment), and their interaction were included in the statistical model. Improvement in CGI was modeled as a dichotomous variable. For analyses of this outcome, we used traditional logistic regression with randomized treatment group as the covariate. All analyses were conducted using an intent-to-treat design.
Under the assumption of missing-at-random, linear mixed effects models provide unbiased effects in the presence of missing data (Atkins, 2005). However, given that missing follow-up data varied by treatment condition, we also used a multiple imputation approach (Raghunathan, 2004). Ten imputed datasets were created for each outcome using the imputation by chained equations approach with predictors of the missing outcomes including baseline levels of the outcome and up to 3 other covariates found to be highly correlated with the outcome (Royston, 2005). The linear mixed models were run on each imputed dataset and results were combined across datasets to yield summary estimates and corresponding 95% confidence intervals and p-values according to Rubin’s rules (1987) that account for the uncertainty of the imputed values. Results using the multiply imputed data were similar to original models.
Results
Feasibility
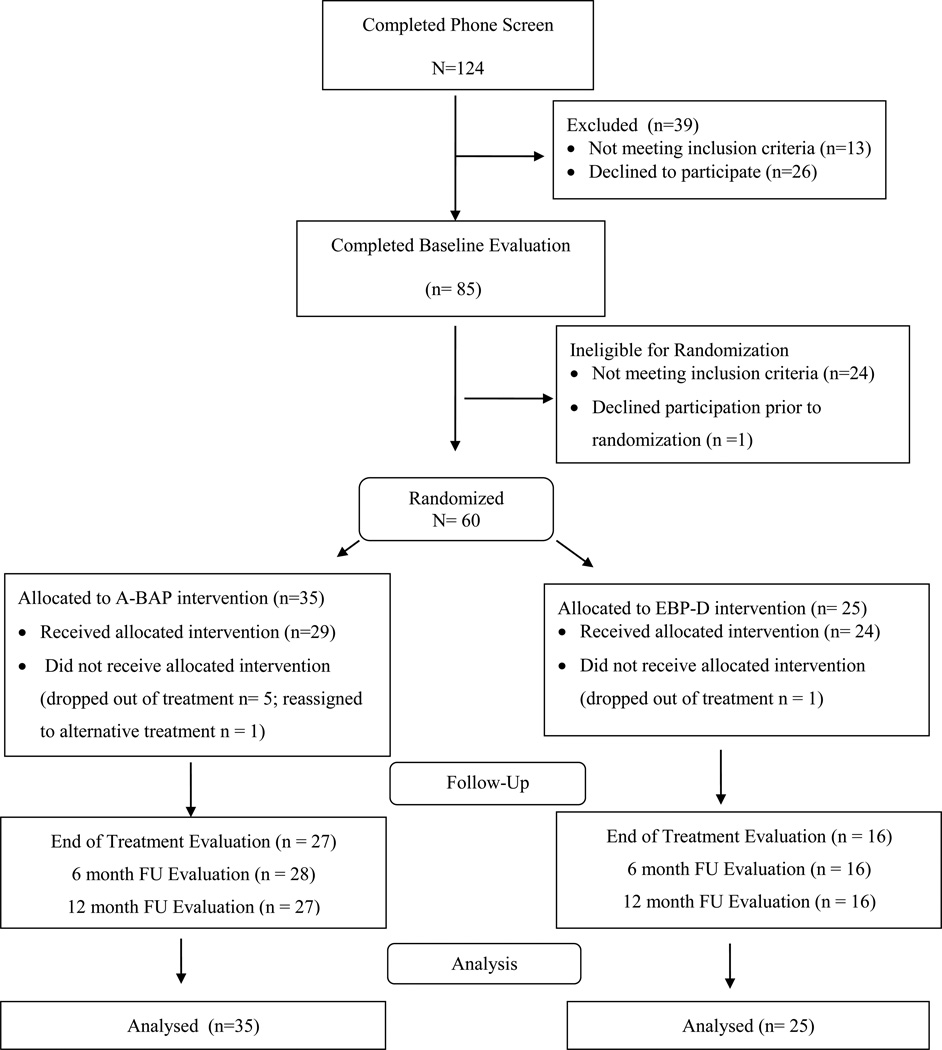
Participant recruitment, enrollment and randomization
As outlined in Figure 3, phone screens were conducted with 124 adolescents: 85 were eligible to participate in the intake evaluation, 13 were ineligible and 26 declined the offer to participate further. Reasons for ineligibility included insufficient reading ability (n = 1), subclinical depression (n = 2), depression secondary to an acute medical condition (n = 1), the absence of depression as the primary disorder, including presence of mania (n = 3), conduct disorder (n = 1) and Asperger’s disorder (n = 1), acute substance use (n = 3), and suicidality requiring immediate, intensive treatment (n = 1). The remaining 26 youth declined participation. Eighty-five cases participated in an in-person evaluation with an ICE resulting in the identification of 61 individuals who met all eligibility criteria. Reasons for ineligibility at intake included insufficient reading ability (n = 1), subclinical depression (n = 11), depression secondary to an acute medical condition (n = 1), the absence of depression as the primary disorder including primary diagnoses of bipolar disorder (n = 2), ODD or conduct disorder (n = 3), an eating disorder (n = 2) and PTSD (n = 1), Asperger’s disorder (n = 1) and suicidality requiring immediate, intensive treatment (n = 2). One potential participant declined and 60 agreed to be randomly assigned to BA or EBP-D.
Figure 3.
Recruitment Flow
As summarized in Table 2, the A-BAP and EBP-D groups did not differ at baseline in relation to gender, age, ethnicity, family socioeconomic status or scores on two measures of depression severity, the CDRS-R and the SMFQ. Participants had a mean age of 14.9 (SD = 1.53), and 63.7% were girls. Thirty-seven percent of those randomized to BA and 36% of those randomized to EBP-D were on antidepressant medication. One adolescent in each group was on both an antidepressant and a stimulant medication; two youth randomized to BA and one to EBP-D were on stimulant medications only.
Table 2.
Sample Characteristics at Baseline
| Total n = 60 |
BA n = 35 |
EBP-D n = 25 |
Statistic/pa | ||||
|---|---|---|---|---|---|---|---|
| Gender | N | % | N | % | N | % | X |
| Male | 22 | 36.7 | 13 | 37.1 | 9 | 36.0 | ns |
| Female | 38 | 63.3 | 22 | 62.9 | 16 | 64.0 | ns |
| Age | M 14.90 |
SD 1.53 |
M 15.17 |
SD 1.52 |
M 14.52 |
SD 1.48 |
F ns |
| Race/Ethnicity Non-Hispanic White |
N 40 |
% 66.7 |
N 23 |
% 65.7 |
N 17 |
% 68.0 |
X ns |
| Hollingshead | M 51.00 |
SD 12.65 |
M 52.64 |
SD 13.14 |
M 48.66 |
SD 11.75 |
F ns |
| CDRS-R | 57.70 | 10.39 | 57.60 | 11.80 | 57.84 | 8.26 | ns |
| SMFQ | 15.87 | 6.06 | 16.05 | 6.05 | 15.64 | 6.20 | ns |
Note. M = Mean; SD = Standard Deviation; CDRS-R = Children’s Depression Rating Scale-Revised; SMFQ = Short Moods and Feelings Questionnaire.
Fisher Exact or ANOVA tests were completed; no differences in means between demographic characteristic levels were statistically significant using a 0.05 alpha level.
Retention and characteristics of completers versus noncompleters
Of the 60 cases randomized, 53 completed the treatment protocol (88.3%) with 5 BA participants (14.1%) and 1 EBP-D participant (1.7%) dropping out of treatment. An additional BA participant was transferred to alternative care based on a decision made by the treatment team in concert with the patient and parent that depression was not the core problem and that the participant would be better served with a different form of treatment. Although higher, the drop-out rate for BA did not differ significantly from that in the EBP-D condition (p = .22, two-tailed Fisher’s exact test). Three participants dropped out secondary to transportation or unanticipated family factors (e.g., familial move) while two adolescents were unwilling to continue in treatment; four of the five who dropped out of BA did so within two sessions of initiating therapy.
Completers across both treatment groups averaged 13.77 sessions (SD = 1.74) whereas non-completers averaged 3.0 (SD = 2) sessions. Youth who completed the protocol were similar to those who did not on core demographic variables, including gender, age, race and ethnicity, SES, or on baseline depression (CDRS-R and SMFQ) or global functioning (CGAS). However, compared to youth who completed the protocol, youth who did not complete the protocol demonstrated significantly higher anxiety (MASC Anxiety Disorders Index (F (1, 54) = 5.10, p < .028). Of the 53 participants who completed treatment, the mean number of sessions attended for youth in the BA condition was slightly higher at 14.44 (SD = 1.78) as compared to 13.13 (SD = 1.30) for the EBP-D group (t(51) = 3.01, p = .004). All participants in both groups completed 10 or more sessions.
Follow-up assessments
Completion of the end of-treatment evaluations was non-significantly higher in BA (77%) than EBP-D (64%) (p = .38, two-tailed Fisher’s exact test). One BA participant and 8 EBP-D participants did not complete an end-of--treatment evaluation, but did complete one of the subsequent follow-up assessments. Of those who did not continue in active treatment, none were willing or able to complete any of the follow-up evaluations.
Symptom and Function Change
Linear mixed model analyses were used to examine changes (improvements) in clinical symptoms and behavioral function of each group from pre- to end of-treatment assessment within each treatment group (A-BAP and EBP-D) (Table 3). Both A-BAP and EBP-D treatment groups showed statistically significant improvements in their clinical symptoms. There was no evidence of statistically significant change over time in Activation, although Avoidance/Rumination significantly decreased over time in both conditions. There were no statistically significant interactions between treatment condition and time indicating that the changes in symptoms and function over time were not significantly different between A-BAP and EBP-D. Additionally, results from logistic regression of CGI Improvement between A-BAP and EBP-D were not statistically significant (OR=2.08 [95% CI 0.64, 6.74, p=0.220]), although both groups showed significant improvement over time.
Table 3.
Means, standard deviation of clinical symptoms and behavioral function outcomes and comparison of pre and end of treatment outcomes for BA and EBP-D conditions
| Measures | BA group (n=35) | EBP-D group (n=25) | P-value interactionb |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre treatment |
End of treatment |
Change from pre-to-posta |
Pre treatment |
End of treatment |
Change from pre-to-posta |
||||||
| Mean | (SD) | Mean | SD | β [95% CI] | Mean | SD | Mean | SD | β [95% CI] | ||
| CDRS-R | 57.6 | (11.8) | 40.2 | (13.9) | −18.6 [−23.2, −13.9] | 57.8 | (8.3) | 45.1 | (14.2) | −13.1 [−18.3, −7.8] | 0.12 |
| SMFQ | 16.1 | (6.1) | 6.3 | (7.4) | −9.6 [−12.3, −6.9] | 15.6 | (6.2) | 6.5 | (6.5) | −9.2 [−12.7, −5.8] | 0.53 |
| CGI Severity | 4.4 | (0.9) | 2.7 | (1.3) | −1.7 [−2.1, −1.3] | 4.7 | (0.6) | 2.8 | (1.2) | −1.9 [−2.5, −1.3] | 0.80 |
| CGAS | 48.9 | (8.9) | 68.8 | (11.7) | 19.9 [14.8, 25.0] | 50.4 | (7.9) | 67.3 | (12.8) | 16.1 [ 9.5, 22.7] | 0.38 |
| BADS Activation | 17.3 | (7.6) | 21.1 | (10.1) | 3.5 [−0.7, 7.7] | 15.5 | (9.9) | 20.1 | (12.1) | 4.8 [ −0.5, 10.2] | 0.87 |
| BADS Avoidance | 25.1 | (9.1) | 16.1 | (9.9) | −9.4 [−13.9, −4.8] | 21.0 | (10.3) | 16.9 | (11.6) | −9.8 [−15.7, −3.9] | 0.91 |
Note. CDRS-R = Children’s Depression Rating Scale-Revised; SMFQ = Short Moods and Feelings Questionnaire; CGI = Clinical Global Impression; CGAS = Children’s Global Assessment Scale; BADS = Behavioral Activation for Depression Scale.
Indicates the change in mental health outcomes from pre-to-end of treatment for each study group (BA and EBP-D) and are results from linear mixed models
p-value is the test that compares whether changes from pre-to-end of treatments are different between BA and EBP-D conditions
Categorical outcomes were operationalized according to CDRS-R categories in which raw scores of 45 to 55 are defined as “depressive disorder is likely to be confirmed”, 31 to 42 as “possible”, and 20 to 29 as “unlikely”. The mean CDRS-R score for the EBP-D participants who completed the end of treatment evaluation (45.05, SD 14.23) fell in the lower range of the “likely” depressive disorder category; 42% had a mean score of 40 or lower at the end of treatment, placing them in the “possible” or “unlikely” depressive disorder categories. Comparatively, the mean CDRS-R score for the A-BAP completers (40.18, SD 13.91) at the end of treatment fell in the “possible” depressive disorder range, with 76% (22 of 29) of treatment completers in the this group having a CDRS-R score of 40 or lower. Of the 27 who completed the BA treatment protocol and end of treatment assessment, 21 were rated as no longer meeting diagnostic criteria for depression (Major Depression, Depressive Disorder NOS, or Dysthymia) on the K-SADS at the end of the active treatment; six continued to meet criteria for a diagnosis of depression. End of treatment KSADS data were missing for two participants: one had a score of 5 on her final session SMFQ which is well below the clinical cut off of 11, while the other completed the 6 month follow-up evaluation and was rated as falling within the “depressive disorder likely” range on the CDRS-R. Of the EBP-D group, 16 completed the end of treatment assessment, four no longer met criteria for depression, seven were rated as improved but with residual symptoms, and three continued to meet diagnostic criteria for depression.
Discussion
The last decade has seen a renewed interest in use of behavioral approaches for the treatment of depressive disorders. Building on this interest and the promising preliminary open trial studies testing the BA approach with depressed adolescents (Chu et al., 2009; Jacob et al., 2013; Ritschel et al., 2011), this pilot study was conducted to assess the feasibility of using a BA approach to effectively treat depressive symptoms in adolescents as part of a treatment development process. Weisz and colleagues (2005) argue that treatments should be developed and tested through a sequence of studies designed to assure that developing treatments work with clinically referred individuals being treated in real-life practice conditions, provide evidence of the treatment’s nature, necessary and sufficient components, and explore moderators and mediators or change processes associated with treatment impact. This trial of A-BAP, as outlined above, focused on completing the first phases outlined in this treatment development model: a) manual development, b) efficacy testing under controlled conditions, c) testing and refinement with single cases in the field, and d) completion of a pilot randomized trial.
The results of the current pilot study provide support for both the feasibility and clinical importance of BA strategies in the treatment of adolescents struggling with depression and should encourage continuing research in this area. The goals of the study were to recruit, successfully randomize, retain and treat 50 participants with the additional goal of demonstrating a significant reduction in depressive symptoms over the course of treatment. Recruitment surpassed the initial target allowing us to follow 53 adolescents through the treatment. Overall retention through the treatment component of the study was 88%, which compares favorably to the retention rates at the end of 12 weeks of treatment reported in the TADS study (TADS Team, 2004). Although more participants randomized to the BA condition dropped out of treatment, factors unrelated to the nature of treatment (e.g. burden of a long commute to appointments; family moved out of the area, poor engagement with initial agreement based on need to appease their parents) were cited in all cases. Since it was made clear that the study was designed to test the BA approach, it is possible that these adolescents and their parents lacked confidence that BA would be effective and therefore left treatment, although this was not stated directly. Anxiety may have been a contributing factor as well since the youth who did not continue in treatment endorsed greater anxiety at baseline than those who completed treatment.
A rigorous approach was taken in this study to test the BA treatment model. The BA approach was assessed with clinically referred individuals who were treated by practicing clinicians in an academic outpatient clinic that serves as a regional community mental health clinic. Furthermore BA was evaluated in comparison to a strong treatment comparison condition in which skilled therapists provided either CBT or IPT based care. Related to this, we anticipated that there would be a positive response to treatment in the control (EBP-D) condition, and this held true. However, more importantly for this study, the pilot accomplished the goal of demonstrating that an adequate treatment response could be obtained using the BA approach. Youth in the BA group demonstrated statistically significant improvement from pre- to end of treatment as reflected in the primary outcome measure, the CDRS-R scores, as well as in CGI and CGAS ratings and SMFQ self-report scores. All pre- to end of treatment outcomes fell within the 95% confidence interval suggesting that the estimates of change were reliable, but given the level of variance on some outcome measures estimates may not be as precise as might be obtained with a larger sample. Furthermore while not all participants met criteria for remission of depression at the end of treatment, diagnostic data was available for 27 of the 29 participants who completed the BA treatment and 78% of these no longer met diagnostic criteria for depression.
This pilot study also included an initial test of the BA model by exploring increased activation and reduced avoidance as potential mediators of clinical response. While it was premature to actually test a mediation model given the small sample size and preliminary nature of this study, we did find positive change on the Activation, and significant improvement on the Avoidance subscale of the BADS for both treatment groups. It is unclear why A-BAP exposed youth did not show greater changes than controls in this targeted area. As sustained, observable behavioral changes take time, however, it is possible that between group changes will emerge over time. Further research with larger sample sizes, will be needed to determine whether increased activation and decreased avoidance serve as mechanisms for change in depression across therapeutic approaches, or if cognitive or social support factors contribute differentially to change for youth exposed to BA, CBT or IPT interventions.
While this study provides initial support for the value of ongoing investigation of the use of a BA approach to treat depression among adolescents, a number of additional issues need to be taken into consideration. This was a small pilot study that was not adequately powered to fully test the BA model or generate an effect size to evaluate change. At the initiation of this study, the literature supported the assumption of a large effect size (0.8) which determined our sample size. Recent studies have, however, found more modest effect sizes, underscoring the need for significantly larger samples (e.g. 180 to 200) to detect differences between treatment conditions.
Additional limitations include the fact that the sample was majority white and female which could limit the generalizability of the findings to more diverse groups. Also the reliability of the Independent Clinical Evaluators was based on initial training only without ongoing adherence ratings as well as the fact that changes in medication usage during the trial was not controlled. Another limitation was the poor compliance with follow-up observed in the EBP-D group. While we were able to accommodate for this in the data analyses, it suggests that these participants/families were less engaged in the overall research project, perhaps assuming that their input was less valuable or needed since they were not randomized to the condition being “tested”. EBP-D participants were exposed to general evidence based treatment approaches, therapists in this condition were not asked to follow a standard treatment manual or given specific guidelines such that the quality and content of intervention in this condition was not controlled. While an in-depth review of the quality of EBP-D in this pilot is beyond the scope of this paper, we do know that participants in our treatment groups were similar in the severity of depression, sessions completed, and that therapists in both conditions were well trained in the approaches offered. However, the preliminary analyses of treatment fidelity reported here represent an additional limitation and underscore the need for a comprehensive comparison of both treatment conditions, including more precise specification of the nature of EBP-D.
Finally, it is important to consider the need for the development of an alternative approach for the treatment of depression in adolescents given the evidence in support of both CBT and IPT, particularly in combination with an antidepressant medication. While many youth find CBT, IPT, and medication, alone and in combination, to be effective treatments, others do not achieve remission of depression and rates of relapse remain high (Curry et al., 2011; Emslie et al., 2008). Furthermore, important subgroups of depressed adolescents such as those who have been exposed to maltreatment earlier in childhood are not responsive to these treatment approaches (Nanni et al., 2012). Thus, innovative treatment development remains critical. The preliminary findings outlined in this paper suggest that further development and testing of BA strategies could enhance the armamentarium of effective approaches in the field. BA expands upon the activation and pleasant events scheduling that is already included as an initial or elective component of most CBT approaches adapted for adolescents (Brent & Poling, 1997; Clarke, DeBar, Ludman, Asarnow, & Jaycox, 2002). Many of these programs also build in the option of using only the activation/pleasant events module in recognition that this may be sufficient to effect change for a subset of depressed youth (Clarke et al., 2002). Moreover, BA employs functional analysis to address issues that get in the way of change, and focuses on overcoming avoidance, both of which are factors that may boost and maintain treatment response. Furthermore BA offers a set of behaviorally focused strategies that may be more acceptable, at least as a starting point, for some adolescents. However, additional research is needed to allow us to tailor treatment approach to the needs of the individual adolescent. Younger adolescents without the maturity needed to effectively engage in cognitive restructuring (Herrington et al., 2013; Frankel et al., 2013), youth who have been exposed to early abuse with residual deficits in executive functioning and decreased sensitivity to reward anticipation (DePrince, Weinzierl, & Combs, 2009; Gould et al., 2012; Pechtel & Pizzagalli, 2011; Rao et al., 2010), and youth who are less open to “talking therapy” may be more responsive to a BA approach. BA strategies, once they are more thoroughly evaluated, may be most useful as a first option in a stepped model of care or as components in a modular approach to treatment of depression, allowing the therapist to draw on evidence-based elements of BA, CBT and IPT as needed to provide individually tailored care. Further research is needed to determine whether there are subgroups of youth that might respond better to one or the other type of treatment.
In closing, this study, although limited in size and scope, provides a first step in establishing the efficacy of BA strategies as either a stand alone, or a component of, treatment for adolescent depression. The findings summarized in this paper, coupled with the significant effect of BA in the treatment of adult depression and the promising data from other preliminary studies with adolescents, supports the need for ongoing work to establish the efficacy of BA strategies as part of a larger effort to improve our ability to effectively manage depression in young people.
Contributor Information
Gretchen Gudmundsen, University of Washington Psychiatry & Behavioral Sciences, 1959 NE Pacific St Box 356560, Seattle, WA 98195.
Elizabeth McCauley, University of Washington, Seattle, WA.
Kelly Schloredt, Seattle Children’s Hospital, 4800 Sand Point Way NE, Seattle, WA 98105.
Christopher Martell, University of Washington Psychiatry & Behavioral Sciences, 1959 NE Pacific St Box 356560, Seattle, WA 98195.
Isaac Rhew, University of Washington, 1100 NE 45th St, Seattle, WA 98105.
Samuel Hubley, University of Colorado School of Medicine, Mail Stop F496 Academic Office 1, 12631 E 17th Ave, Aurora, CO 80045.
Sona Dimidjian, University of Colorado at Boulder, 345 UCB, Boulder, CO 80309-0345.
References
- Angold A, Costello EJ, Messer SC, Pickles A, Winder F, Silver D. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. International Journal of Methods in Psychiatric Research. 1995;5:237–249. [Google Scholar]
- Angold A, Erkanli A, Silberg J, Eaves L, Costello EJ. Depression scale scores in 8–17-year-olds: effects of age and gender. Journal of Child Psychology and Psychiatry. 2002;43(8):1052–1063. doi: 10.1111/1469-7610.00232. [DOI] [PubMed] [Google Scholar]
- Atkins DC. Using multilevel models to analyze couple and family treatment data: basic and advanced issues. Journal of Family Psychology. 2005;19(1):98–110. doi: 10.1037/0893-3200.19.1.98. [DOI] [PubMed] [Google Scholar]
- Beck AT, Rush JA, Shaw BF, Emery G. Cognitive therapy of depression. New York: Guilford; 1979. [Google Scholar]
- Brent DA, Poling K. Cognitive therapy treatment manual for depressed and suicidal youth. Pittsburgh, PA: University of Pittsburgh Health System Services for Teens At Risk; 1997. [Google Scholar]
- Chu BC, Colognori D, Weissman AS, Bannon K. An initial description and pilot of group behavioral activation therapy for anxious and depressed youth. Cognitive and Behavioral Practice. 2009;16:408–419. [Google Scholar]
- Clarke G, DeBar L, Ludman E, Asarnow J, Jaycox L. STEADY Project intervention manual: Collaborative care, cognitive-behavioral program for depressed youth in a primary care setting. 2002 Retrieved from http://www.in.gov/idoc/files/STEADY_project_Intervention1.pdf.
- Copeland WE, Shanahan L, Costello EJ, Angold A. Childhood and adolescent psychiatric disorders as predictors of young adult disorders. Archives of General Psychiatry. 2009;66(7):764–772. doi: 10.1001/archgenpsychiatry.2009.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, Egger H, Angold A. 10-year research update review: The epidemiology of child and adolescent psychiatric disorders: I. Methods and public health burden. Journal of American Academy of Child and Adolescent Psychiatry. 2005;44(10):972–986. doi: 10.1097/01.chi.0000172552.41596.6f. [DOI] [PubMed] [Google Scholar]
- Curry J, Silva S, Rohde P, Ginsburg G, Kratochvil C, Simons A, March J. Recovery and recurrence following treatment for adolescent major depression. Archives of General Psychiatry. 2011;68(3):263. doi: 10.1001/archgenpsychiatry.2010.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davey CG, Yücel M, Allen NB. The emergence of depression in adolescence: Development of the prefrontal cortex and the representation of reward. Neuroscience & Biobehavioral Reviews. 2008;32(1):1–19. doi: 10.1016/j.neubiorev.2007.04.016. [DOI] [PubMed] [Google Scholar]
- DePrince AP, Weinzierl KM, Combs MD. Executive function performance and trauma exposure in a community sample of children. Child Abuse & Neglect. 2009;33(6):353–361. doi: 10.1016/j.chiabu.2008.08.002. [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Barrera M, Jr, Martell C, Muñoz RF, Lewinsohn PM. The origins and current status of behavioral activation treatments for depression. Annual Review of Clinical Psychology. 2011;7:1–38. doi: 10.1146/annurev-clinpsy-032210-104535. [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Hollon SD, Dobson KS, Schmaling KB, Kohlenberg RJ, Addis ME, Jacobson NS. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. Journal of Consulting and Clinical Psychology. 2006;74(4):658. doi: 10.1037/0022-006X.74.4.658. [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Hubley S, Martell C, Herman R, Dobson K. Quality of Behavioral Activation Scale. Boulder, Colorado: University of Colorado Boulder; (unpublished manuscript) [Google Scholar]
- Dunn V, Goodyer IM. Longitudinal investigation into childhood-an adolescence-onset depression: Psychiatric outcome in early adulthood. British Journal of Psychiatry. 2006;188:216–222. doi: 10.1192/bjp.188.3.216. [DOI] [PubMed] [Google Scholar]
- Emslie GJ, Kennard BD, Mayes TL, Nightingale-Teresi J, Carmody T, Hughes CW, Rintelmann JW. Fluoxetine versus placebo in preventing relapse of major depression in children and adolescents. The American Journal of Psychiatry. 2008;165(4):459. doi: 10.1176/appi.ajp.2007.07091453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esposito C, Clum GA. Psychiatric symptoms and their relation to suicidal ideation in a high risk adolescent community sample. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:44–51. doi: 10.1097/00004583-200201000-00010. [DOI] [PubMed] [Google Scholar]
- Evans MD, Piasecki JM, Kriss MR, Hollon SD. Raters manual for the collaborative study psychotherapy rating scale, form 6. Minneapolis: University of Minnesota and the St. Paul-Ramsey Medical Center; 1984. [Google Scholar]
- Ferster CB. A functional analysis of depression. American Psychologist. 1973;28:857–870. doi: 10.1037/h0035605. [DOI] [PubMed] [Google Scholar]
- Forbes EE. Where’s the fun in that? Broadening the focus on reward function in depression. Biological Psychiatry. 2009;66(3):199–200. doi: 10.1016/j.biopsych.2009.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes EE, Christopher May J, Siegle GJ, Ladouceur CD, Ryan ND, Carter CS, Dahl RE. Reward-related decision-making in pediatric major depressive disorder: an fMRI study. Journal of Child Psychology and Psychiatry. 2006;47(10):1031–1040. doi: 10.1111/j.1469-7610.2006.01673.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frankel SA, Herrington CG, Evans LD, Korelitz KE, Bauman JM, Garber J. Scientific reasoning development and learning cognitive behavioral therapy skills for depression in youth; Poster presented at the meeting of the Society for Research in Child Development; Seattle, WA. 2013. Apr, [Google Scholar]
- Goodyer IM, Herbert J, Tamplin A, Altham PME. First-episode major depression in adolescents: Affective, cognitive, and endocrine characteristics of risk status and predictors of onset. The British Journal of Psychiatry. 2000;176:142–149. doi: 10.1192/bjp.176.2.142. [DOI] [PubMed] [Google Scholar]
- Gould F, Clarke J, Heim C, Harvey PD, Majer M, Nemeroff CB. The effects of child abuse and neglect on cognitive functioning in adulthood. Journal of Psychiatric Research. 2012;46(4):500–506. doi: 10.1016/j.jpsychires.2012.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guy W. Early clinical drug evaluation unit (ECDEU) assessment manual for psychopharmacology (Rev.) (NIH Publication No. 76–338) Rockville, MD: US Department of Health, Education, and Welfare; 1976. [Google Scholar]
- Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE. Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10-year longitudinal study. Journal of Abnormal Psychology. 1998;107(1):128–140. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- Hare TA, Tottenham N, Galván A, Voss HU, Glover GH, Casey BJ. Biological substrates of emotional reactivity and regulation in adolescence during an emotional go-nogo task. Biological Psychiatry. 2008;63:927–934. doi: 10.1016/j.biopsych.2008.03.015015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrington CG, Frankel SA, Abernathy ET, Bauman JM, Hunt H, Korelitz KE, Garber J. Metacognitive development and learning cognitive behavioral therapy skills for depression in children and adolescents; Poster presented at the meeting of the Society for Research in Child Development; Seattle, WA. 2013. Apr, [Google Scholar]
- Hollingshead AB. Four factor index of social status. New Haven, CT: Unpublished manuscript, Yale University; 1975. [Google Scholar]
- Jacob M, L Keeley M, Ritschel L, Craighead WE. Behavioural activation for the treatment of low-income, African American adolescents with major depressive disorder: A case series. Clinical Psychology & Psychotherapy. 2013;20(1):87–96. doi: 10.1002/cpp.774. [DOI] [PubMed] [Google Scholar]
- Kanter JW, Mulick PS, Busch AM, Berlin KS, Martell CR. The behavioral activation for depression scale (BADS): psychometric properties and factor structure. Journal of Psychopathology and Behavioral Assessment. 2007;29(3):191–202. [Google Scholar]
- Kanter JW, Rusch LC, Busch AM, Sedivy SK. Validation of the Behavioral Activation for Depression Scale (BADS) in a community sample with elevated depressive symptoms. Journal of Psychopathology and Behavioral Assessment. 2009;31(1):36–42. [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao UMA, Flynn C, Moreci P, Ryan N. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(7):980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Keenan-Miller D, Hammen CL, Brennan PA. Health outcomes related to early adolescent depression. Journal of Adolescent Health. 2007;41(3):256–262. doi: 10.1016/j.jadohealth.2007.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennard BD, Clarke GN, Weersing VR, Asarnow JR, Shamseddeen W, Porta G, Brent DA. Effective components of TORDIA cognitive-behavioral therapy for adolescent depression: Preliminary findings. Journal of consulting and clinical psychology. 2009;77(6):1033. doi: 10.1037/a0017411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennard B, Silva S, Vitiello B, Curry J, Kratochvil C, Simons A, March J. Remission and residual symptoms after short-term treatment in the Treatment of Adolescents with Depression Study (TADS) Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45(12):1404–1411. doi: 10.1097/01.chi.0000242228.75516.21. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM. A behavioral approach to depression. In: Friedman RM, Katz MM, editors. The psychology of depression: Contemporary theory and research. New York: Wiley; 1974. pp. 157–185. [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR, Klein DN, Gotlib IH. Psychosocial functioning of young adults who have experienced and recovered from major depressive disorder during adolescence. Journal of Abnormal Psychology. 2000;112:353–363. doi: 10.1037/0021-843x.112.3.353. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM. Lewinsohn’s model of depression. In: Craighead WE, Nemeroff CB, editors. The Corsini encyclopedia of psychology and behavioral science. 3rd. New York: Wiley; 2001. pp. 442–444. [Google Scholar]
- Lewis CC, Simons AD, Nguyen LJ, Murakami JL, Reid MW, Silva SG, March JS. Impact of childhood trauma on treatment outcome in the Treatment for Adolescents With Depression Study (TADS) Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(2):132–140. doi: 10.1097/00004583-201002000-00007. [DOI] [PubMed] [Google Scholar]
- Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. The Lancet. 2006;367(9524):1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- March JS, Parker JD, Sullivan K, Stallings P, Conners CK. The Multidimensional Anxiety Scale for Children (MASC): factor structure, reliability, and validity. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(4):554–565. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR. Longitudinal associations between alcohol problems and depressive symptoms: early adolescence through early adulthood. Alcoholism: Clinical and Experimental Research. 2009;33(1):49–59. doi: 10.1111/j.1530-0277.2008.00810.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarty CA, Weisz JR. Effects of psychotherapy for depression in children and adolescents: What we can (and can’t) learn from meta-analysis and component profiling. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46(7):879–886. doi: 10.1097/chi.0b013e31805467b3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarty CA, Wymbs BT, King KM, Mason WA, Stoep AV, McCauley E, Baer J. Developmental consistency in associations between depressive symptoms and alcohol use in early adolescence. Journal of Studies on Alcohol and Drugs. 2012;73(3):444. doi: 10.15288/jsad.2012.73.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenzie DP, Toumbourou JW, Forbes AB, Mackinnon AJ, McMorris BJ, Catalano RF, Patton GC. Predicting future depression in adolescents using the short mood and feelings questionnaire: a two-nation study. Journal of Affective Disorders. 2011;134(1):151–159. doi: 10.1016/j.jad.2011.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMakin DL, Olino TM, Porta G, Dietz LJ, Emslie G, Clarke G, Brent DA. Anhedonia predicts poorer recovery among youth with selective serotonin reuptake inhibitor treatment-resistant depression. Journal of the American Academy of Child & Adolescent Psychiatry. 2012;51(4):404–411. doi: 10.1016/j.jaac.2012.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mufson L, Dorta KP, Moreau D, Weissman MM. Interpersonal psychotherapy for depressed adolescents. New York: Guilford Press; 2011. [Google Scholar]
- Mufson L, Dorta KP, Wickramaratne P, Nomura Y, Olfson M, Weissman MM. A randomized effectiveness trial of interpersonal psychotherapy for depressed adolescents. Archives of General Psychiatry. 2004;61(6):577. doi: 10.1001/archpsyc.61.6.577. [DOI] [PubMed] [Google Scholar]
- Mufson L, Weissman MM, Moreau D, Garfinkel R. Efficacy of interpersonal psychotherapy for depressed adolescents. Archives of General Psychiatry. 1999;56(6):573. doi: 10.1001/archpsyc.56.6.573. [DOI] [PubMed] [Google Scholar]
- Nanni V, Uher R, Danese A. Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: a meta-analysis. American Journal of Psychiatry. 2012;169(2):141–151. doi: 10.1176/appi.ajp.2011.11020335. [DOI] [PubMed] [Google Scholar]
- Patton GC, Olsson C, Bond L, Toumbourou JW, Carlin JB, Hemphill SA, Catalano RF. Predicting female depression across puberty: a two-nation longitudinal study. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47(12):1424–1432. doi: 10.1097/CHI.0b013e3181886ebe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pechtel P, Pizzagalli DA. Effects of early life stress on cognitive and affective function: an integrated review of human literature. Psychopharmacology. 2011;214(1):55–70. doi: 10.1007/s00213-010-2009-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poznanski E, Mokros H. Children’s depression rating scale-revised (CDRS-R) Los Angeles, CA: Western Psychological Services; 2001. [Google Scholar]
- Raghunathan TE. What do we do with missing data? Some options for analysis of incomplete data. Annual Review of Public Health. 2004;25:99–117. doi: 10.1146/annurev.publhealth.25.102802.124410. [DOI] [PubMed] [Google Scholar]
- Rao U, Chen LA, Bidesi AS, Shad MU, Thomas MA, Hammen CL. Hippocampal changes associated with early-life adversity and vulnerability to depression. Biological Psychiatry. 2010;67(4):357–364. doi: 10.1016/j.biopsych.2009.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rintelmann JW, Emslie GJ, Rush AJ, Varghese T, Gullion CM, Kowatch RA, Hughes CW. The effects of extended evaluation on depressive symptoms in children and adolescents. Journal of affective disorders. 1996;41(2):149–156. doi: 10.1016/s0165-0327(96)00084-5. [DOI] [PubMed] [Google Scholar]
- Ritschel LA, Ramirez CL, Jones M, Craighead WE. Behavioral activation for depressed teens: A pilot study. Cognitive and Behavioral Practice. 2011;18(2):281–299. [Google Scholar]
- Rosselló J, Bernal G. The efficacy of cognitive-behavioral and interpersonal treatments for depression in Puerto Rican adolescents. Journal of Consulting and Clinical Psychology. 1999;67(5):734. doi: 10.1037//0022-006x.67.5.734. [DOI] [PubMed] [Google Scholar]
- Royston P. Multiple imputation of missing values: update of ice. Stata Journal. 2005;5(4):527. [Google Scholar]
- Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: J. Wiley & Sons; 1987. [Google Scholar]
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, Aluwahlia S. A children’s global assessment scale (CGAS) Archives of General Psychiatry. 1983;40(11):1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Fleiss JL. Intraclass correlations: Uses in assessing rater reliability. Psychological bulletin. 1979;86(2):420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- Silk JS, Dahl RE, Ryan ND, Forbes EE, Axelson DA, Birmaher B, Siegle GJ. Pupillary reactivity to emotional information in child and adolescent depression: links to clinical and ecological measures. The American Journal of Psychiatry. 2007;164(12):1873. doi: 10.1176/appi.ajp.2007.06111816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somerville LH, Hare T, Casey BJ. Frontostriatal maturation predicts cognitive control failure to appetitive cues in adolescents. Journal of Cognitive Neuroscience. 2011;23(9):2123–2134. doi: 10.1162/jocn.2010.21572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TADS (Treatment for Adolescents With Depression Study) Team. Treatment for Adolescents with Depression Study (TADS): rationale, design, and methods. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42(5):531–542. doi: 10.1097/01.CHI.0000046839.90931.0D. [DOI] [PubMed] [Google Scholar]
- TADS (Treatment for Adolescents with Depression Study) Team. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for adolescents with depression study (TADS) randomized controlled trial. Journal of the American Medical Association. 2004;292(7):807–820. doi: 10.1001/jama.292.7.807. [DOI] [PubMed] [Google Scholar]
- TADS (Treatment for Adolescents with Depression Study) Team. The Treatment for Adolescents with Depression Study (TADS): Long-term effectiveness and safety outcomes. Archives of General Psychiatry. 2007;64(10):1132–1144. doi: 10.1001/archpsyc.64.10.1132. [DOI] [PubMed] [Google Scholar]
- Tottenham N, Hare TA, Casey BJ. Behavioral assessment of emotion discrimination, emotion regulation, and cognitive control in childhood, adolescence, and adulthood. Frontiers in Psychology. 2011;2(39) doi: 10.3389/fpsyg.2011.00039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisz JR, Jensen AL, McLeod BD. Development and dissemination of child and adolescent psychotherapies: Milestones, methods, and a new deployment-focused model. In: Hibbs ED, Jensen PS, editors. Psychosocial treatments for child and adolescent disorders: Empirically-based approaches. 2nd. Washington, D.C: American Psychological Association; 2005. pp. 9–39. [Google Scholar]
- Weisz JR, McCarty CA, Valeri SM. Effects of psychotherapy for depression in children and adolescents: a meta-analysis. Psychological Bulletin. 2006;132(1):132. doi: 10.1037/0033-2909.132.1.132. [DOI] [PMC free article] [PubMed] [Google Scholar]