Abstract
Objective
Epidemiologic analyses indicate a lack of association between body mass index (BMI: kg/m2) and mortality among Hispanic adults. Because BMI provides only a surrogate for the real variable of interest (adiposity), we evaluated associations between measures of body composition and mortality.
Methods
Using data from US-residing Mexican-Americans in the National Health and Nutrition Examination Survey (NHANES) III (n=4,480) and NHANES 1999–2010 (n=5,849), we examined the association between seven measures of body composition measured via anthropometry and bio-electrical impedance analysis (i.e., waist circumference, waist-to-height ratios (WHtR), skinfolds, lean mass, fat mass, percent body fat and BMI) and all-cause and cardiovascular and diabetes mortality. We conducted additional analyses stratified by gender.
Results
Waist circumference (hazard ratio [HR] 1.04, 95% Confidence Interval (CI): 1.01, 1.07) and WHtR (HR: 1.08, 95% CI: 1.03–1.14) were weakly associated with an increased all-cause mortality, while WHtR was associated with an increased risk of diabetes-related death (HR: 1.26, 95% CI: 1.07–1.49). In gender stratified analyses, we observed increases in risk of mortality in females who had increases in WHtR and waist circumference for all-cause mortality and cardiovascular deaths.
Conclusion
Waist circumference and WHtR were associated with increased risk of all-cause and diabetes-related mortality in US-residing Mexican-American adults.
Keywords: Hispanic, Mexican-Americans, mortality, obesity, diabetes, body composition
Introduction
The association between body mass index (BMI: kg/m2) and mortality has been frequently examined across gender, race and disease groups1–4. Since BMI does not take into account potential variability in the proportion and distribution of either fat mass or lean mass5, investigators have suggested that other measures of adiposity may provide more accurate estimates of the association between obesity and mortality6. These include measures derived from bioelectrical impedance analysis (BIA); anthropometrics (e.g. skinfold thickness, waist circumference, waist-to-height ratios and waist-to-hip ratios); and dual energy X-ray absorptiometry (DXA).
Although studies show that elevated BMI consistently associates with mortality in white and black populations4,7 it does not do so among Hispanic adults2,3. Studies have indicated that more precise measures of adiposity, such as ratio measures (e.g. waist-to-hip, waist-to-thigh, waist-to-height (WHtR)), may be stronger predictors of mortality6, diabetes8 and cardiovascular disease9 than BMI in whites and blacks, while lean mass has been shown to play a protective role in mortality risk1.
Ethnic and racial differences in body composition also facilitate the need to investigate different indices of adiposity. Hull et al10 examined the differences in fat-free mass index [FFMI: (fat free mass)/height2] between gender, age and ethnic groups and found that both male and female Hispanics had significantly higher FFMI values than whites and Asians but lower values than blacks. However, Aleman-Mateo et al11 found that total body and truncal body fat was higher and fat free lean mass was significantly lower in Mexican-Americans compared to their white and black counterparts. Given differences in body composition as a function of race/ethnicity as well as variation in findings of fat and lean mass distributions, using BMI as a proxy measure of obesity may not provide a precise estimate of the obesity-mortality association among Hispanics. Further, certain sub-groups of Hispanics, such as Mexican-Americans may exhibit different obesity-mortality associations.
Herein we examine the association between measures of body composition and all-cause, and cardiovascular and diabetes-related mortality among US-residing Mexican-American adults who participated in the National Health and Nutrition Examination Survey (NHANES) from 1988–1994 (NHANES III) and 1999–2010 (NHANES 1999–2010). We hypothesize that measures of adiposity such as waist circumference, WHtR, and percent body fat will associate with all-cause and cardiovascular and diabetes specific mortality among Mexican-Americans.
Methods
Data Source
We used data from the NHANES12, a program of surveys and physical examinations sponsored by the Centers for Disease Control and Prevention (CDC) and conducted for over 50 years in the United States designed to provide population estimates related to nutrition and health of US residents aged 2 months and older (age 0 and older since NHANES 1999). Two datasets were used: the NHANES III, conducted from 1988 to 1994 and the continuous NHANES, specifically data collected from 1999 to 2010. Publicly available mortality data has been probabilistically matched (to ensure anonymity) using the National Death Index to each participant through December 31, 201113. Data are publicly available from the CDC website12. This project was reviewed and declared exempt (i.e. the research conducted was less than minimal risk and used publically available de-identified data) by the University of Alabama at Birmingham Institutional Review Board.
Inclusion Criteria
Sampling of non-Mexican-American Hispanics participants was smaller than the US population in the design of the NHANES III and NHANES 1999–2007. Due to this, the National Centers for Health Statistics (NCHS)14 recommends limiting analyses to Mexican-Americans for NHANES prior to 2007 for precise estimates. Specific criteria for inclusion in the analyses were: (1) Mexican-American adults who were age 20 or older; (2) were not pregnant at the time of assessment (n=; (3) completed the physical examination and home questionnaire portions of the NHANES; and (4) were not missing mortality data. We identified n=11,051 (unweighted sample size) Mexican-American adults who were age 20 or older, and excluded n=303 (unweighted) pregnant females, n=410 (unweighted) that had some missing exam or questionnaire data, and n=9 (unweighted) missing mortality information, leaving an unweighted sample of n=10,329 participants for analysis.
Study Variables
Outcome variables
Survival time, with age as timescale (age in years), to all-cause, cardiovascular or diabetes related death or censoring (December 31, 2011) were the primary outcomes of interest, taking a classical approach account for competing risks by coding deaths due to the other causes as censored at the time of death for each cause-specific death. Cardiovascular deaths were defined using the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) codes I00–I09, I11, I13, I20–I51 and diabetes deaths using ICD-10 codes E10–E14.
Predictor variables
Predictors of interest included six measures of body composition: (1) waist circumference (cm); (2) waist-to height ratio (WHtR); (3) sum of subscapular (mm) and triceps (mm) skinfolds; (4) lean mass (kg); (5) fat mass (kg); and (6) percent body fat collected via BIA (for the continuous NHANES we restricted the analysis of lean mass, fat mass and percent body fat to the NHANES 1999–2004 cycles since BIA was not collected in the 2005–2010 cycles). An additional model was fitted with BMI as a predictor. Waist circumference, weight, height and skinfold thickness were collected using standard equipment by trained NHANES staff based on uniform procedures described in The Anthropometric Standardization Reference Manual15. WHtR was calculated by dividing waist measurement in centimeters by height in centimeters. BMI was calculated as weight in kilograms divided by height in meters squared.
BIA was collected by placing electrodes on the participant’s right hand and right foot and administering a small electrical current, while additional electrodes placed on the right side of the body measured the resistance and reactance to the current 16. Resistance and reactance values are recorded and then converted to assess body composition values such as fat-free body mass and total body water using established formulas17.
Covariates
Covariates (age, gender and smoking status) were selected a priori and included potential confounders related to associations between mortality and body composition. Age was treated as a continuous variable in the model. Gender and smoking status were categorical, with smoking status classified as either “never smoker”, “former” or “current smoker”.
Statistical Analysis
Means, proportions and measures of variation were calculated, taking into account the complex, stratified sampling design used by NHANES by applying weights, strata, and sampling unit values to produce estimates of the national population. Hazard ratios [HRs] and 95% confidence intervals [95% CI] were calculated using Cox proportional hazards regression, with all-cause mortality, and cardiovascular and diabetes related mortality as the outcome and age at death or censor as the time scale18, for each measure of adiposity in separate models. Reference cut-off values for each anthropometric measure were computed by following the prevalence-matched approach similar to methods used by Flegal et al19. First, we calculated the proportion of adults in our sample that had a BMI ≤ 25 kg/m2 and a BMI > 25 kg/m2. Next, we looked at the distributions of each of the body composition measures and selected a cut-off that would yield the same proportion in our sample to match the distribution based on BMI. To assess nonlinearity of the continuous body composition measures, an additional analysis was conducted by entering quadratic terms into each of the models for each mortality outcome. We assessed the improvement (or the lack of improvement) in model fit using the Akaike information criterion (AIC) criterion. To control for varying times of entry into the study18, we left truncated the survival observation period for each participant at the age at survey. The age at survey was included as a covariate in the models, along with, as previously noted, gender and smoking status. Proportional hazard assumptions were assessed using weighted Schoenfeld residuals20 and weighted Kaplan-Meir curves and appeared reasonable for the covariates in the model. Due to established differences in body composition by gender, an additional stratified analysis was conducted by gender to ascertain any gender differences in the association between body composition/adiposity and mortality. We also conducted an additional analysis that estimated HRs based on 5-unit increment increases per body composition measure.
To compare the predictive ability of the models, a generalized R2 was calculated using methods described by O’Quigley et al21, where the Cox and Snell22 R2 is adjusted by the number of censored events as opposed to the overall sample size and is more appropriate when data is highly censored. Kent23 proposed the use of a “coefficient of explained randomness” in nonlinear models, such as the Cox proportional hazards model, which is comparable to explained variation in linear models and often referred to as a generalized or pseudo-R2. A higher number indicates a higher level of explained randomness (since these models are proportional) for that particular model. We used R version 3.4.0 and its library (‘survey’) to conduct all analyses.
Results
Descriptive statistics for the sample are presented in Table 1 (shown separately by dataset). There were 10,329 Mexican-American adults (unweighted sample size) included in the analysis, with a mean age of 38.7 (SD 14.2) at time of study participation and roughly 47% were female. After a mean follow up of 11.0 (SD 6.9) years, there were a total of 1423 unweighted deaths, of which 109 were cardiovascular related deaths and 107 were diabetes related deaths. Mean age at all-cause mortality was 64.7 years (SD 17.0); cardiovascular related mortality was 65.9 years (SD 19.6); and diabetes related mortality was 69.7 years (SD 12.7).
Table 1.
Description of the datasets and participant characteristics
| Characteristic | NHANES III | NHANES 1999–2010 |
|---|---|---|
| Dates of Study | 1988–1994 | 1999–2010 |
| Sample size for analysis d | 4480 | 5849 |
| Mean Age (years) (SE) c | 37.4 (14.4) | 39.5 (14.1) |
| Mean Mortality follow-up (years) (SE) c | 18.7 (4. 1) | 6.4 (3.3) |
| Female (%) c | 47.8 | 45.7 |
| No of Deaths (%) d | 999 (13.9) | 424 (3.4) |
| Mean BMI (SE) c | 27.4 (5.4) | 28.9 (5.9) |
| Mean waist circumference (cm) (SE) c | 92.4 (13.3) | 96.9 (13.9) |
| Mean WHtR (SE) c | 0.57 (0.08) | 0.59 (0.09) |
| Mean sum skinfoldsa (mm) (SE) c | 39.3 (15.8) | 38.7 (13.7) |
| Mean BIA % fat (SE) c | 31.6 (8.8) | 31.4 (10.6)b |
| Mean BIA Lean Mass (kg) (SE) c | 50.0 (10.8) | 52.0 (12.3)b |
| Mean BIA Fat Mass (kg) (SE) c | 23.6 (9.5) | 24.3 (10.8)b |
| Non-Smokers (%) c | 56.7 | 60.3 |
SE: Standard error; BMI: Body mass index (kg/m2); WHtR: waist-to-height ratio; BIA: bioelectrical impedance analysis
sum of subscapular and triceps
Bioelectrical impedance analysis was only collected from 1999–2004 in the NHANES. Mean values represent the 2995 Mexican-Americans that completed this measure.
Weighted values
Un-weighted values
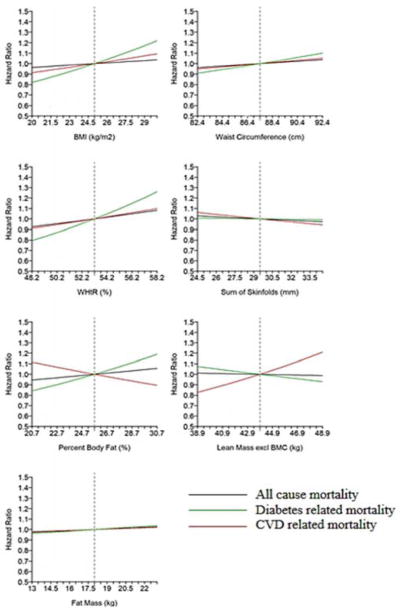
Plotted hazard ratios (HR) for all-cause mortality, cardiovascular and diabetes-related mortality by continuous body composition measure for the 1-unit linear models are presented in Figure 1. Estimates for the 1-unit linear and quadratic models for all-cause mortality, along with model fit statistics, are presented in supplementary table 1 with estimates for cardiovascular and diabetes related deaths presented in supplementary table 2. Overall, after adjusting for gender, smoking and waist circumference and age, WHtR associated with a slight increased risk of all-cause death among Mexican-American adults, while no other measure of body composition associated with an increased risk. No body composition measures associated with an increased risk of cardiovascular- related death. WHtR was associated with an increased risk of diabetes-related death.
Figure 1.
Plotted hazard ratios for all-cause, cardiovascular and diabetes related mortality by continuous body composition measure for Mexican-American adults in the NHANES III and NHANES 1999–2010, adjusted for age, gender and smoking status.
Table 2 presents HR mortality estimates for larger increases (which may translate into more clinical relevance) in the various body composition measures. As shown, it is estimated that Mexican-American adults have a 4% increased risk for all-cause mortality for each 5 cm increase in waist circumference and an 8% increased hazard of death per 5% (0.05) increment increase in WHtR. Sum of skinfolds, body fat percent, fat mass, lean mass and BMI did not associate significantly with all-cause mortality (HRs: 0.97–1.06). Mexican-American adults had a 26% increased risk of a diabetes related death per 5% (0.05) increment increase in WHtR while no measure of body composition associated significantly with cardiovascular related mortality.
Table 2.
Hazard ratios and 95% confidence interval for all-cause mortality by body composition measure in 5-unit increments for Mexican-American adults in the NHANES III and NHANES 1999–2010a
| Body Composition Measure | All-Cause Mortality | Cardiovascular Related Mortality | Diabetes Related Mortality | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Reference Values | No. of Events | HR (95% CI) | No. of Events | HR (95% CI) | No. of Events | HR (95% CI) | |
| BMI (per 5kg/m2) | 25.0 kg/m2 | 1423 | 1.04 (0.96–1.11) | 109 | 1.10 (0.88–1.36) | 107 | 1.23 (0.99–1.52) |
| Waist Circumference (per 5cm) | 87.4 cm | 1423 | 1.04 (1.01–1.07) | 109 | 1.05 (0.97–1.15) | 107 | 1.10 (0.99–1.22) |
| WHtR (per 0.05) | 0.53 | 1423 | 1.08 (1.03–1.14) | 109 | 1.09 (0.96–1.25) | 107 | 1.26 (1.07–1.49) |
| Sum of Skinfolds (per 5mm) | 29.5 mm | 1423 | 0.97 (0.94–1.00) | 109 | 0.95 (0.86–1.06) | 107 | 1.00 (0.88–1.15) |
| Percent Body Fat (per 5%) | 25.7% | 1423 | 1.06 (0.96–1.17) | 109 | 0.91 (0.70–1.18) | 107 | 1.20 (0.96–1.52) |
| Lean Mass (per 5kg) | 43.0 kg | 1423 | 0.99 (0.94–1.04) | 109 | 1.21 (1.00–1.47) | 107 | 0.92 (0.69–1.23) |
| Fat Mass (per 5kg) | 18.0 kg | 1423 | 1.03 (0.97–1.09) | 109 | 1.03 (0.84–1.27) | 107 | 1.05 (0.86–1.28) |
BMI: Body mass index (kg/m2); WHtR: waist-to-height ratio
Bolded text indicates significance at p<0.05.
Models adjusted for age, gender and smoking status. Separate models were estimated for each body composition measure.
Gender Specific Estimates
Since substantial gender differences in body composition exist, we conducted a stratified analysis by gender for both datasets (see Figure 2 and Table 3). Figure 2 plots the HRs for mortality by body composition measure on a continuous scale (per 1-unit increment) for males and females separately. Table 3 presents HR mortality estimates for 5-unit increases for each body composition measure for males and females.
Figure 2.
Plotted hazard ratios for all-cause, cardiovascular and diabetes related mortality by continuous body composition measure for Mexican-American adults in the NHANES III and NHANES 1999–2010 for linear models by gender, adjusted for age and smoking status.
Table 3.
Hazard ratios and 95% confidence interval for mortality by body composition measure in 5-unit increments for Mexican-American adults in the NHANES III and NHANES 1999–2010 by gendera
| Males | All-Cause Mortality | Cardiovascular Related Mortality | Diabetes Related Mortality | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Body Composition Measure | Reference Values | No. of Events | HR (95% CI) | No. of Events | HR (95% CI) | No. of Events | HR (95% CI) |
| BMI (per 5kg/m2) | 25.0 kg/m2 | 818 | 0.99 (0.88–1.10) | 60 | 0.69 (0.48–0.98) | 52 | 1.35 (0.90–2.01) |
| Waist Circumference (per 5cm) | 89.0 cm | 818 | 1.02 (0.98–1.06) | 60 | 0.94 (0.82–1.07) | 52 | 1.12 (0.96–1.31) |
| WHtR (per 0.05) | 0.53 | 818 | 1.05 (0.97–1.12) | 60 | 0.84 (0.66–1.06) | 52 | 1.26 (0.96–1.66) |
| Sum of Skinfolds (per 5mm) | 25.6 mm | 818 | 0.96 (0.92–1.00) | 60 | 0.79 (0.66–0.95) | 52 | 1.14 (0.97–1.34) |
| Percent Body Fat (per 5%) | 22.5% | 818 | 1.02 (0.91–1.14) | 60 | 0.70 (0.53–0.93) | 52 | 1.17 (0.78–1.76) |
| Lean Mass (per 5kg) | 52.2 kg | 818 | 0.99 (0.93–1.06) | 60 | 1.05 (0.82–1.33) | 52 | 1.07 (0.84–1.36) |
| Fat Mass (per 5kg) | 15.8 kg | 818 | 1.02 (0.94–1.10) | 60 | 0.75 (0.58–0.97) | 52 | 1.19 (0.87–1.63) |
| Females | All-Cause Mortality | Cardiovascular Related Mortality | Diabetes Related Mortality | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Body Composition Measure | Reference Values | No. of Events | HR (95% CI) | No. of Events | HR (95% CI) | No. of Events | HR (95% CI) |
| BMI (per 5kg/m2) | 25.0 kg/m2 | 605 | 1.08 (0.99–1.18) | 49 | 1.37 (1.11–1.69) | 55 | 1.15 (0.94–1.42) |
| Waist Circumference (per 5cm) | 84.9 cm | 605 | 1.06 (1.01–1.10) | 49 | 1.15 (1.05–1.26) | 55 | 1.08 (0.97–1.21) |
| WHtR (per 0.05) | 0.54 | 605 | 1.11 (1.04–1.18) | 49 | 1.26 (1.10–1.44) | 55 | 1.24 (1.05–1.48) |
| Sum of Skinfolds (per 5mm) | 38.8 mm | 605 | 0.99 (0.95–1.03) | 49 | 1.10 (0.95–1.27) | 55 | 0.91 (0.80–1.03) |
| Percent Body Fat (per 5%) | 35.8% | 605 | 1.11 (0.98–1.25) | 49 | 1.13 (0.78–1.63) | 55 | 1.22 (0.89–1.69) |
| Lean Mass (per 5kg) | 38.0 kg | 605 | 0.97 (0.88–1.06) | 49 | 1.58 (1.21–2.08) | 55 | 0.61 (0.32–1.17) |
| Fat Mass (per 5kg) | 21.8 kg | 605 | 1.04 (0.98–1.10) | 49 | 1.18 (0.96–1.46) | 55 | 0.97 (0.77–1.21) |
BMI: Body mass index (kg/m2); WHtR: waist-to-height ratio
Bolded text indicates significance at p<0.05.
Models adjusted for age and smoking status. Separate models were estimated for each body composition measure.
There were no significant associations between body composition and all-cause and diabetes related mortality in Mexican-American male participants. However, per 5-unit increases in BMI, sum of skinfolds, percent body fat, and fat mass, males had reduced risk of cardiovascular related mortality. For every 5-unit increase in waist circumference, Mexican-American females had an increased risk of all-cause mortality (HR: 1.06, 95% CI: 1.01–1.10) while a 5-unit climb in WHtR increased the risk of all-cause and diabetes related mortality (HR: 1.11, 95% CI: 1.04–1.18 and HR: 1.24, 95% CI: 1.05–1.48, respectively). Interestingly, Mexican-American females that had increases in BMI (HR: 1.37, 95% CI: 1.11–1.69) waist circumference (HR: 1.15, 95% CI: 1.05–1.26), WHtR (HR: 1.26, 95% CI: 1.10–1.44), and lean mass (HR: 1.58, 95% CI: 1.21–2.08) exhibited an increased risk in cardiovascular related mortality.
Non-Linearity and Model Fit Statistics
Akaike information criterion (AIC) values for both the linear and quadratic models are presented in supplementary tables. For all-cause mortality, the AIC values were not markedly different between the linear and quadratic models, however, values were lower for the linear models for all body composition predictors except percent body fat. For cardiovascular related mortality, the AIC values for the linear models were better for most predictors, except sum of skinfolds. Similarly, for diabetes-related mortality, the AIC values for the linear models were better for all of the predictors except lean body mass.
Generalized R2
Results from the generalized R2 calculations are presented in the supplementary tables. For all-cause mortality, while the R2 for each of the seven models were similar in magnitude, the model with percent body fat as the outcome indicated the most randomness explained at about 5.2%. For cardiovascular-related mortality, lean mass explained the most randomness at 20.4% and for diabetes-related mortality, WHtR explained the most randomness at 12.2%. Of note, for all-cause mortality all other measures of body composition had higher R2 values than BMI. For cardiovascular and diabetes-related mortality models, most measures of body composition had more favorable R2 values than the BMI model.
Discussion
WHtR and waist circumference associated with a slight increased risk of all-cause mortality in Mexican-Americans in the NHANES III and NHANES 1999–2010, after controlling for age, gender and smoking status. We found no association with all-cause mortality for lean mass or any of the other adiposity measures, however, we did find associations between body composition measures and cardiovascular-related mortality in Mexican-American women in our stratified analysis. We also found that increases in WHtR associated with an increased risk of diabetes-related death overall and in women. Moreover, we found that including a non-linear term for each body composition model for each dataset did not alter our findings.
Our overall and female-specific findings of weak associations between increases in waist circumference and WHtR and all-cause mortality in Mexican Americans parallel those of Koster et al24 who examined the association between waist circumference and mortality in white, black and Hispanic adult’s age 50 to 71 years in the NIH-AARP Diet and Health Study. Using standard World Health Organization cut points, they observed a significant association with risk of death in Hispanic males that had a waist circumference > 102 cm (HR 1.38, 95% CI: 1.04, 1.82) and Hispanic females with a waist circumference > 88 cm (HR 1.74, 95% CI: 1.08, 2.08). In contrast, our study provides estimates of a larger sample of Hispanics not limited to an older age range. Our findings are also similar to Flegal and Graubard’s19 results using a heterogeneous population from the NHANES III.
Additional studies have found associations between waist circumference and WHtR and mortality in women25, black women26, non-Hispanic men and women24 and heterogeneous samples27. Kahn et al27 examined different measures of adiposity in a sample from the NHANES III and found that waist and WHtR associated with mortality in models adjusted for age, education, ancestry (white, black and Mexican American) and smoking. For the associations between waist circumference and mortality, males had a HR of 1.27 (95% CI: 1.08, 1.51) and females had a HR of 1.47 (95% CI: 1.29, 1.67). For WHtR, males exhibited a 33% increased risk of death per standard deviation change in ratio while females exhibited a 45% increased risk of mortality. Further, Katzmarzyk et al28 found that waist circumference and WHtR associated with mortality in adjusted models for whites and blacks in a longitudinal study of white and black men and women aged 18–89.
The lack of an association between other adiposity measures and all-cause mortality in this sample of Mexican-American adults is similar to previous findings in other ethnic populations examined using NHANES data. For instance, Navaneethan et al29 did not find associations between percent body fat and mortality in the NHANES 1999–2004. Moreover, while the results of this analysis, using more precise measures of adiposity and lean mass, confirm previous findings of an absence of a strong association between obesity (measured through BMI) and mortality in Hispanics2,3, they are in contrast to recent work from our group that found an increased risk of death in Mexican-Americans who were ≥ 35 kg/m2 at the time of study participation and reported a maximum lifetime weight of ≥ 35 kg/m2 (HR: 1.52, 95% CI 1.10–2.10)30.
WHtR associated with an increased risk of diabetes-related death for Mexican-Americans and specifically in Mexican-American women. To our knowledge, this is the first study to examine the association between different body composition measures and diabetes-related mortality specifically in Mexican-Americans. Our results are again similar to a recent study from our group that found that Mexican-Americans in the NHANES that had a maximum lifetime BMI of ≥ 30 kg/m2 (but lost weight over time) were at an increased risk of a diabetes-related death30. Further, there is evidence that adults with a BMI ≥ 35 kg/m2 in general are at a significantly increased risk of diabetes-related death31. Considering that, compared to non-Hispanics, Hispanics have an increased risk of diabetes-related death overall32, these results are cause for concern since obesity, particularly abdominal fat, may further increase the risk of diabetes-related deaths in Mexican-American adults.
In the analysis stratified by gender, while we did not find evidence of an association between body composition and increased risk of cardiovascular related deaths in Mexican-American men, we did find protective associations in BMI, percent body fat, skinfolds and fat mass (kg). These results are similar to previous work where individuals who were overweight (i.e. BMI 25.0–29.9 kg/m2) had decreased all-cause mortality among older Hispanics2, and decreased CVD-related mortality in the general population33, as well as in older individuals34 and other non-white populations35. Moreover, similar findings have been reported in individuals with known cardiovascular disease36,37 and there is evidence that Hispanics have lower rates of CVD mortality38. Although we did not limit our CVD model to individuals with known cardiovascular disease, individuals with CVD in our cohort may be influencing this association. Further investigation of these protective associations in Mexican-American men is warranted. Conversely, we found significant associations between increases in BMI, waist circumference, and WHtR and cardiovascular mortality in Mexican-American women, which is in line with previous studies in the general population19,39.
Interestingly, we found that increases in lean mass (kg) was associated with increased risk of CVD-related mortality in Mexican-American females. This finding is in contrast to other similar studies where increases in lean mass are protective. There is some evidence that lean individuals with hypertension have an increased risk of CVD mortality40,41 and not adjusting for individuals with CVD related chronic conditions in the current analysis may have affected the estimates. Additionally, estrogen, produced by fat cells42, has been shown to be protective against CVD in women43. Females with increases in lean mass may have decreases in fat mass resulting in less protection against CVD. We also observed that increases in lean mass trended towards an increased risk of diabetes death in men. Our findings are similar to those discussed by George et al44, who find that men with ‘lean diabetes’ have increases in overall mortality compared to obese diabetics. Lastly, the associations between lean mass and mortality may be different in this ethnic population, as seen in the BMI-mortality associations previously published2,3, warranting further investigations.
Although the main aim of these analyses was to estimate associations between adiposity measures and mortality in Mexican-Americans, previous investigations have sought to understand whether different measures of adiposity better predict mortality than does BMI6,19,24,28. As an extension of this analysis, the body composition models (1-unit increment) were compared to a model with BMI by calculating a generalized R2. Although it is not a direct measure of the amount of variance explained in the model, the value of R2 increases when the predictors are strongly associated to the outcome. According to an O’Quigley et al21 simulation study, adjusting the Cox and Snell 22 formulas to account for the number of failures (deaths in our case) served as a stronger indicator of explained randomness in non-linear models. Using this statistic as a crude way of comparing the models, we found that most body composition measures had slightly higher R2 values than BMI, particularly in the all-cause mortality model, indicating that these adiposity measures may have better predictive ability than BMI when estimating the obesity-mortality association among Mexican Americans. This is consistent with previous studies 6,24. Our results also appear to be similar to Flegal et al19, who found that, in NHANES III, anthropometric measures of adiposity (i.e., waist circumference, hip circumference, sum of skinfolds and arm circumferences), ratio measures of adiposity (WHtR, waist to hip ratio), and percent body fat estimated from BIA were slightly associated with mortality but did not provide strikingly different results compared to the association observed between BMI and mortality.
It is important to acknowledge the limitations of these analyses. First, a limitation of all observational studies is that they show associations (or lack thereof) which may not necessarily indicate causation (or lack of causation). Second, our use of a generalized R2 to compare models is a crude measurement and the predictive ability of each model was not statistically compared to other models; rigorous analysis to compare the predictive ability of these models of adiposity (such as conducting sensitivity and specificity analyses) compared to BMI are warranted to understand which models are superior in Mexican-American samples. Third, we had to limit the models estimating percent body fat, and fat and lean mass via BIA to the NHANES III and NHANES 1999–2004 which did not allow us to include an additional six years of data for more precise estimates. Since we combined the NHANES III and NHANES 1999–2010 for analysis, we were limited to using BIA for body composition measures since body composition was not assessed using DXA in the NHANES III. Moreover, DXA is more accurate than BIA in measuring body composition and estimates should be interpreted with this limitation in mind45. Fourth, the NHANES 1999–2010 did not collect hip measurements, precluding us from looking at the association between waist-to-hip ratios and mortality. Previous studies19,25 have indicated associations between waist-to-hip ratio and mortality in other populations and would be useful to examine in a Hispanic population. Fifth, we did not adjust for other potential confounders that may influence the association between obesity and mortality, such as alcohol consumption, physical activity and socio-economic status, in order to preserve power. Sixth, although we used the largest set of available data involving Hispanic populations, there were relatively few deaths from CVD and diabetes. As such, the reliability of these estimates should be interpreted with caution. Lastly, we did not account for systematic measurement error in the various adiposity measures and thus risk estimates may be an underestimate of the actual risk (i.e. bring the results towards the null); interpretation of estimates should keep this limitation in mind.
Strengths of this study include that this analysis is the first to examine specific body composition measures in relation to all-cause and cardiovascular and diabetes-related mortality in Mexican-American adults. In addition, this analysis used a large sample size enabling the ability to yield precise estimates of the longitudinal association between measures of adiposity and mortality in this population. Further, this analysis used nationally representative data and incorporated sampling weights to produce population estimates. Moreover, we found evidence that confirms previous findings from our group that obesity associates with an increased risk of diabetes-related death in a Hispanic population.
Conclusion
To our knowledge, this is the first investigation of the association between body composition measures and mortality in a large nationally-representative cohort of US-residing Mexican-Americans. Overall we found only three modest associations between indices of body composition and all-cause and diabetes-related mortality. This suggests that obesity, whether assayed via BMI or measures of body composition, may not associate as strongly with mortality among Mexican-Americans as it does in other racial/ethnic groups. Further studies to understand the reasons for this are warranted.
Supplementary Material
What is already known about this subject?
There are consistent observed associations between increased body mass index (BMI: kg/m2) and mortality risk in white and black populations.
Although previous work indicates a lack of association between BMI and mortality in Hispanic adults, utilizing measures of body composition (e.g. waist circumference, waist-to-height ratio, skinfolds, percent body fat, lean mass and fat mass) as the predictor of interest may provide more insight into this association.
What does the current study add?
This is the first study to examine the association between measures of body composition and all-cause and cause-specific mortality in US-residing Mexican-American adults using two nationally representative datasets.
Increases in waist circumference and waist-to-height ratio were modestly associated with increased risk of all-cause mortality in Mexican American adults participating in the National Health and Nutrition Examination Survey.
Increases in waist-to-height ratio were associated with increased risk of diabetes related deaths in Mexican American adults participating in the National Health and Nutrition Examination Survey.
Acknowledgments
Funding Sources:
This work was supported in part by National Institutes of Health grant [grant number P30DK056336 to T.M.] and the funding provided by Lister Hill Center for Health Policy [to T.M.] at the University of Alabama at Birmingham.
Footnotes
Conflict of Interest:
The authors declared no conflicts of interest. The opinions expressed are those of the authors and not necessarily those of the NIH or any other organization with which the authors are affiliated.
References
- 1.De Schutter A, Lavie CJ, Kachur S, Patel DA, Milani RV. Body composition and mortality in a large cohort with preserved ejection fraction: untangling the obesity paradox. Mayo Clin Proc. 2014;89(8):1072–1079. doi: 10.1016/j.mayocp.2014.04.025. [DOI] [PubMed] [Google Scholar]
- 2.Fontaine KR, McCubrey R, Mehta T, et al. Body mass index and mortality rate among Hispanic adults: a pooled analysis of multiple epidemiologic data sets. Int J Obes. 2012;36(8):1121–1126. doi: 10.1038/ijo.2011.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mehta T, McCubrey R, Pajewski NM, et al. Does obesity associate with mortality among Hispanic persons? Results from the National Health Interview Survey. Obesity. 2013;21(7):1474–1477. doi: 10.1002/oby.20105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whitlock G, Lewington S, Sherliker P, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–1096. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wellens RI, Roche AF, Khamis HJ, Jackson AS, Pollock ML, Siervogel RM. Relationships between the Body Mass Index and body composition. Obes Res. 1996;4(1):35–44. doi: 10.1002/j.1550-8528.1996.tb00510.x. [DOI] [PubMed] [Google Scholar]
- 6.Ashwell M, Mayhew L, Richardson J, Rickayzen B. Waist-to-Height Ratio Is More Predictive of Years of Life Lost than Body Mass Index. PLoS One. 2014;9(9):e103483. doi: 10.1371/journal.pone.0103483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berrington de Gonzalez A, Hartge P, Cerhan JR, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med. 2010;363(23):2211–2219. doi: 10.1056/NEJMoa1000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Folsom AR, Kushi LH, Anderson KE, et al. Associations of general and abdominal obesity with multiple health outcomes in older women: the Iowa Women’s Health Study. Arch Intern Med. 2000;160(14):2117–2128. doi: 10.1001/archinte.160.14.2117. [DOI] [PubMed] [Google Scholar]
- 9.Canoy D, Boekholdt SM, Wareham N, et al. Body fat distribution and risk of coronary heart disease in men and women in the European Prospective Investigation Into Cancer and Nutrition in Norfolk cohort: a population-based prospective study. Circulation. 2007;116(25):2933–2943. doi: 10.1161/CIRCULATIONAHA.106.673756. [DOI] [PubMed] [Google Scholar]
- 10.Hull HR, Thornton J, Wang J, et al. Fat-free mass index: changes and race/ethnic differences in adulthood. Int J Obes (Lond) 2011;35(1):121–127. doi: 10.1038/ijo.2010.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aleman Mateo H, Lee SY, Javed F, et al. Elderly Mexicans have less muscle and greater total and truncal fat compared to African-Americans and Caucasians with the same BMI. J Nutr Health Aging. 2009;13(10):919–923. doi: 10.1007/s12603-009-0252-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. [Accessed November 13, 2014];NHANES. http://www.cdc.gov/nchs/nhanes.htm.
- 13.Centers for Disease Control and Prevention. NCHS Surveys. 2011 Linked Mortality Files. [Accessed March 10, 2015];Public-Use Data Dictionary. http://www.cdc.gov/nchs/data/datalinkage/Public_use_Data_Dictionary_23_2015.pdf.
- 14.Johnson CL, Paulose-Ram R, Ogden CL, et al. National health and nutrition examination survey: analytic guidelines, 1999–2010. Vital and health statistics Series 2, Data evaluation and methods research. 2013;(161):1–24. [PubMed] [Google Scholar]
- 15.Lohman T, Roache A, Martorell R. Anthropometric standardization reference manual. 1988 [Google Scholar]
- 16.Centers for Disease Control and Prevention. [Accessed June 30, 2015]; http://wwwm.cdc.gov/Nchs/Nhanes/1999-2000/BIX.htm.
- 17.Chumlea WC, Guo SS, Kuczmarski RJ, et al. Body composition estimates from NHANES III bioelectrical impedance data. Int J Obes Relat Metab Disord. 2002;26(12):1596–1609. doi: 10.1038/sj.ijo.0802167. [DOI] [PubMed] [Google Scholar]
- 18.Pencina MJ, Larson MG, D’Agostino RB. Choice of time scale and its effect on significance of predictors in longitudinal studies. Stat Med. 2007;26(6):1343–1359. doi: 10.1002/sim.2699. [DOI] [PubMed] [Google Scholar]
- 19.Flegal KM, Graubard BI. Estimates of excess deaths associated with body mass index and other anthropometric variables. Am J Clin Nutr. 2009;89(4):1213–1219. doi: 10.3945/ajcn.2008.26698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grambsch PM, Therneau TM. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika. 1994;81(3):515–526. [Google Scholar]
- 21.O’Quigley J, Xu R, Stare J. Explained randomness in proportional hazards models. Stat Med. 2005;24(3):479–489. doi: 10.1002/sim.1946. [DOI] [PubMed] [Google Scholar]
- 22.Cox DR, Snell EJ. Analysis of binary data. Vol. 32. CRC Press; 1989. [Google Scholar]
- 23.Kent JT. Information gain and a general measure of correlation. Biometrika. 1983;70(1):163–173. [Google Scholar]
- 24.Koster A, Leitzmann MF, Schatzkin A, et al. Waist circumference and mortality. Am J Epidemiol. 2008;167(12):1465–1475. doi: 10.1093/aje/kwn079. [DOI] [PubMed] [Google Scholar]
- 25.Zhang C, Rexrode KM, van Dam RM, Li TY, Hu FB. Abdominal obesity and the risk of all-cause, cardiovascular, and cancer mortality: sixteen years of follow-up in US women. Circulation. 2008;117(13):1658–1667. doi: 10.1161/CIRCULATIONAHA.107.739714. [DOI] [PubMed] [Google Scholar]
- 26.Boggs DA, Rosenberg L, Cozier YC, et al. General and abdominal obesity and risk of death among black women. N Engl J Med. 2011;365(10):901–908. doi: 10.1056/NEJMoa1104119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kahn HS, Bullard KM, Barker LE, Imperatore G. Differences between adiposity indicators for predicting all-cause mortality in a representative sample of United States non-elderly adults. PLoS One. 2012;7(11):e50428. doi: 10.1371/journal.pone.0050428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Katzmarzyk PT, Mire E, Bray GA, Greenway FL, Heymsfield SB, Bouchard C. Anthropometric markers of obesity and mortality in white and African American adults: the pennington center longitudinal study. Obesity. 2013;21(5):1070–1075. doi: 10.1002/oby.20151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Navaneethan SD, Kirwan JP, Arrigain S, Schold JD. Adiposity measures, lean body mass, physical activity and mortality: NHANES 1999–2004. BMC Nephrol. 2014;15:108. doi: 10.1186/1471-2369-15-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Howell CR, Fontaine K, Ejima K, Ness KK, Cherrington A, Mehta T. Maximum Lifetime Body Mass Index and Mortality in Mexican American Adults: the National Health and Nutrition Examination Survey III (1988–1994) and NHANES 1999–2010. Prev Chronic Dis. 2017;14:E67. doi: 10.5888/pcd14.160588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rogers RG, Hummer RA, Krueger PM. The effect of obesity on overall, circulatory disease- and diabetes-specific mortality. J Biosoc Sci. 2003;35(1):107–129. [PubMed] [Google Scholar]
- 32.Kposowa AJ. Mortality from Diabetes by Hispanic Groups: Evidence from the US National Longitudinal Mortality Study. International Journal of Population Research. 2013;2013:12. [Google Scholar]
- 33.McGee DL The Diverse Populations Collaboration. Body mass index and mortality: a meta-analysis based on person-level data from twenty-six observational studies. Ann Epidemiol. 2005;15(2):87–97. doi: 10.1016/j.annepidem.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 34.Jiang J, Ahn J, Huang WY, Hayes RB. Association of obesity with cardiovascular disease mortality in the PLCO trial. Prev Med. 2013;57(1):60–64. doi: 10.1016/j.ypmed.2013.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Auyeung TW, Lee JS, Leung J, Kwok T, Leung PC, Woo J. Survival in older men may benefit from being slightly overweight and centrally obese--a 5-year follow-up study in 4,000 older adults using DXA. J Gerontol A Biol Sci Med Sci. 2010;65(1):99–104. doi: 10.1093/gerona/glp099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Banack HR, Kaufman JS. The obesity paradox: understanding the effect of obesity on mortality among individuals with cardiovascular disease. Preventive medicine. 2014;62:96–102. doi: 10.1016/j.ypmed.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 37.Romero-Corral A, Montori VM, Somers VK, et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet. 2006;368(9536):666–678. doi: 10.1016/S0140-6736(06)69251-9. [DOI] [PubMed] [Google Scholar]
- 38.Cortes-Bergoderi M, Goel K, Murad MH, et al. Cardiovascular mortality in Hispanics compared to non-Hispanic whites: a systematic review and meta-analysis of the Hispanic paradox. Eur J Intern Med. 2013;24(8):791–799. doi: 10.1016/j.ejim.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 39.Flegal KM, Graubard BI, Williamson DF, Gail MH. Cause-specific excess deaths associated with underweight, overweight, and obesity. Jama. 2007;298(17):2028–2037. doi: 10.1001/jama.298.17.2028. [DOI] [PubMed] [Google Scholar]
- 40.Carman WJ, Barrett-Connor E, Sowers M, Khaw KT. Higher risk of cardiovascular mortality among lean hypertensive individuals in Tecumseh, Michigan. Circulation. 1994;89(2):703–711. doi: 10.1161/01.cir.89.2.703. [DOI] [PubMed] [Google Scholar]
- 41.Colangelo LA, Vu TH, Szklo M, Burke GL, Sibley C, Liu K. Is the association of hypertension with cardiovascular events stronger among the lean and normal weight than among the overweight and obese? The multi-ethnic study of atherosclerosis. Hypertension. 2015;66(2):286–293. doi: 10.1161/HYPERTENSIONAHA.114.04863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Siiteri PK. Adipose tissue as a source of hormones. Am J Clin Nutr. 1987;45(1 Suppl):277–282. doi: 10.1093/ajcn/45.1.277. [DOI] [PubMed] [Google Scholar]
- 43.Rosano GM, Fini M. Postmenopausal women and cardiovascular risk: impact of hormone replacement therapy. Cardiol Rev. 2002;10(1):51–60. doi: 10.1097/00045415-200201000-00010. [DOI] [PubMed] [Google Scholar]
- 44.George AM, Jacob AG, Fogelfeld L. Lean diabetes mellitus: An emerging entity in the era of obesity. World Journal of Diabetes. 2015;6(4):613–620. doi: 10.4239/wjd.v6.i4.613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pateyjohns IR, Brinkworth GD, Buckley JD, Noakes M, Clifton PM. Comparison of three bioelectrical impedance methods with DXA in overweight and obese men. Obesity (Silver Spring) 2006;14(11):2064–2070. doi: 10.1038/oby.2006.241. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.