Abstract
Introduction
Uncontrolled family factors may bias the estimation of the association between maternal smoking during pregnancy and offspring BMI. The objective was to assess if there is an association between maternal smoking during pregnancy and offspring BMI z-score independent of factors in the siblings’ shared environment, and if such association is linear.
Methods
We performed an individual patient data meta-analysis using five studies providing sibling data (45299 children from 14231 families). In a multi-level model, separating within-family and between-family effects and with random intercept for families, we analyzed the dose-response association between maternal number of cigarettes per day during pregnancy and offspring’s BMI z-score using B-splines to allow for non-linear associations.
Results
A linear within-family effect for number of cigarettes smoked in the range from 1-30 cigarettes per day on the offspring’s BMI z-score was observed. Each additional cigarette per day between sibling pregnancies resulted in an increase in BMI z-score of 0.007 (95%-CI=[0.006-0.009]). A between family-effect emerged only with doses ≥25 cigarettes per day.
Conclusions
The number of cigarettes mothers smoke per day during pregnancy is positively associated with offspring BMI z-score even among siblings, suggesting that the association is not entirely explained by confounding by family factors.
Keywords: offspring, smoking, siblings, family factors
INTRODUCTION
A number of early-life determinants of overweight and obesity have described.1 A role for maternal smoking in pregnancy in causing childhood obesity might appear surprising, since offspring of smoking mothers have a lower birth weight than those of non-smoking mothers.2 A number of studies, however, reported such associations with overweight even beyond childhood3 and a consistent association between maternal smoking during pregnancy and offspring overweight was confirmed in a number of meta-analyses .4–7 These meta-analyses based on observational studies, however, may be fraught with bias because of the inherent limitation of observational studies. Even if a wide range of confounders has been considered residual confounding due to unmeasured covariate cannot be excluded. Smoking, particularly during pregnancy, continues to be patterned by social and economic circumstances that have strong associations with child growth issue.8–11 Comparisons of outcomes between children born into the same family control for shared family factors by design without specifying and accurately measuring the wide range of potential confounding factors shared by siblings.12–14
In addition to the problem of causal inference, another unresolved issue concerning the hypothesized effects of maternal smoking during pregnancy on offspring overweight is whether or not the effect is linear - increasing with the number of cigarettes smoked - or in some fashion non-linear. In order to evaluate the linearity of the effect across the distribution of the number of cigarettes smoked, splines can be applied to uncover, rather than impose, the correct function form.
We conducted an Individual Patient Data (IPD) meta-analysis of the within-family association between maternal smoking during pregnancy and offspring overweight. In a two-step approach we first attempted to identify all studies on childhood overweight by number of cigarettes smoked by mothers during pregnancy in a systematic review. Studies reporting the association for more than one child per family were eligible to be included in this IPD study. We addressed the following research questions: Is there an association between maternal smoking during pregnancy and offspring BMI z-score independent of factors in the siblings’ shared environment, and is such association linear?
METHODS
Study Design and Population
We performed an IPD meta-analysis on the linearity of the effects of maternal smoking during pregnancy and offspring body mass index (BMI) for sibling data. Potentially eligible studies for the IPD meta-analysis were identified in a systematic literature search using the following search terms: (offspring OR children OR toddlers OR child OR infant OR adolescent* OR adult*) AND (overweight OR obesity OR obese OR adipose OR adiposity) AND (maternal smoking during pregnancy OR maternal smoking in pregnancy OR mother smoked during pregnancy OR mother smoked in pregnancy OR in utero nicotine exposure OR in utero exposure OR nicotine exposure during pregnancy OR nicotine exposure in pregnancy OR cigarettes during pregnancy OR cigarettes in pregnancy) AND (dose-response OR dose-effect OR dose OR amount of cigarettes OR number of cigarettes OR volume of cigarettes OR volume of nicotine). The literature search was performed independently by two investigators (CS and RvK).
All studies published before May 2015 that included data on the number of cigarettes mothers smoked during pregnancy and the BMI of children were considered for inclusion in our analysis. We excluded studies if the publication language was neither English nor German, or if the study population was already reported in another included study.
Authors of all studies reporting BMI and doses for maternal smoking during pregnancy were contacted and data collected. In a second step, these datasets were scanned for sibling data. If it was unclear whether sibling data was included in these dataset (in case of absence of a family or mother ID), authors were contacted again. Multiples and children with missing information on BMI or maternal number of cigarettes smoked during their pregnancy were excluded.
We additionally performed a plausibility analysis regarding the main outcome BMI z-score and excluded children with BMI z-scores <-4 or >4 from the analysis.
Data collection, merging and analysis was finished in May 2017. The study was approved by the Ethics Committee of the LMU Munich (UE Nr. 024-14). It is registered at PROSPERO international register of systematic reviews with registration number CRD4201502475. For all included studies, individual ethical approvals are documented in the respective original publications.
Study quality assessment
Study quality was assessed based on the quality assessment criteria for observational cohort and cross-sectional studies of the National Institute of Health (http://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/cohort). Eight questions out of 14 were appropriate for this analysis. We excluded questions regarding sample size/power estimate, sufficient timeframe to observe effect, different levels for exposure, quality of exposure measure, several measures of exposure and adjustment for confounding variables, as the answers were obvious, or they were already considered in the inclusion criteria (Table S1). Quality assessment was conducted independently by two investigators (RvK and LA) with each study rated as poor, fair, or good by mutual agreement.
Statistical Methods
In an initial analysis, mixed-effect regression models with random intercept for each family were used to analyze the association between the number of cigarettes mothers smoked during pregnancy and children’s BMI z-score (according to the WHO Child Growth Standards15). To identify the within-family and the between-family effect of maternal number of cigarettes smoked during pregnancy on BMI z-score (i.e., the effect that is independent of shared confounding influences), a term for the average number of cigarettes smoked across pregnancies was added to the model.16,17 In three studies multiple measures for the number of cigarettes at different stages of one pregnancy were given. Then the maximum number of cigarettes at any time point was used.3,8,18 The number of potential confounders to be included in the models of the IPD analysis was limited. We could only use potential confounders reported in most studies.
We considered a) maternal weight status (underweight (BMI<18 kg/m2), overweight (25 kg/m2≤ BMI<30 kg/m2), obese (BMI≥30 kg/m2) or normal weight (18 kg/m2≤ BMI<25 kg/m2;)) (if available pre-pregnancy weight before each respective pregnancy; if not available, then maternal weight at assessment of each child’s BMI assessment was used); b) breastfeeding (for at least one month if available, else ever breastfeeding) (yes vs. no) after the respective pregnancy; c) maternal education attained at the onset of the respective pregnancy (at least high school completed or 10 years of school education vs. no high school completed or less than 10 years of school education) as potential confounders. To take variations between studies into account a categorical indicator of study number was added as an additional covariate.
We also considered size at birth including small for gestational age (SGA; weight <10th percentile) or large for gestational age (LGA; weight >90th percentile) with reference to appropriate for gestational age (AGA; weight for gestational age between 10th and 90th percentile) as defined in the original studies or applying country specific percentiles if not reported, and preterm delivery (<37 weeks of gestation) in a sensitivity analysis. Models with adjustment for SGA, LGA and preterm delivery were provided as supplementary material. These models give the direct effect of smoking on BMI z-score (beyond the effects working through SGA, LGA or preterm delivery). For the main analysis, however, we provided the best estimate of the overall causal effect of maternal smoking, namely the effect of a hypothetical intervention reducing maternal smoking on offspring overweight/obesity, without adjustment for covariates likely to be in the causal pathway.
To investigate non-linear associations between number of cigarettes and offspring BMI z-score, B-splines (numeric functions that are piecewise-defined by polynomials with a high degree of smoothness at the places where the polynomial pieces connect) were used in our main analysis to model both the within-family and between-family effects of maternal smoking.19 All analyses were implemented using the R package ‘lme4’.20
Missing values for the potential confounding variables were imputed by a single multiple imputation step (PROC MI, SAS, V.9.4).21 The imputation model included the exposure, the confounders, and study (as categorical variable). As the percentage of missing values was small and the sample size large we did not correct the analysis results by applying Rubin’s rules.22
RESULTS
Five studies reporting sibling data could be included in the IPD meta-analysis.3,8,18,23,24 The detailed steps of the systematic literature search are depicted in Figure 1.
Figure 1.
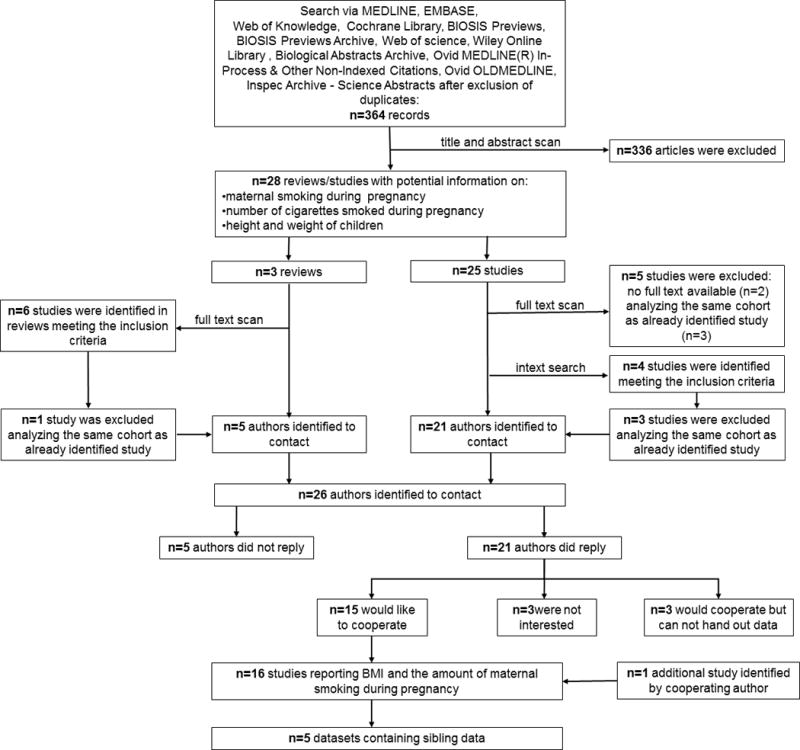
Flow chart displaying the process of literature search and study selection
Figure 2 depicts the flow chart of exclusions on the individual level in the five studies providing sibling data. For final analysis we considered data on 45 299 children from 14 231 families with at least two children in the dataset. The number of siblings per family ranged from two to sixteen children, but was two in most cases two (N=10 576 families).
Figure 2.
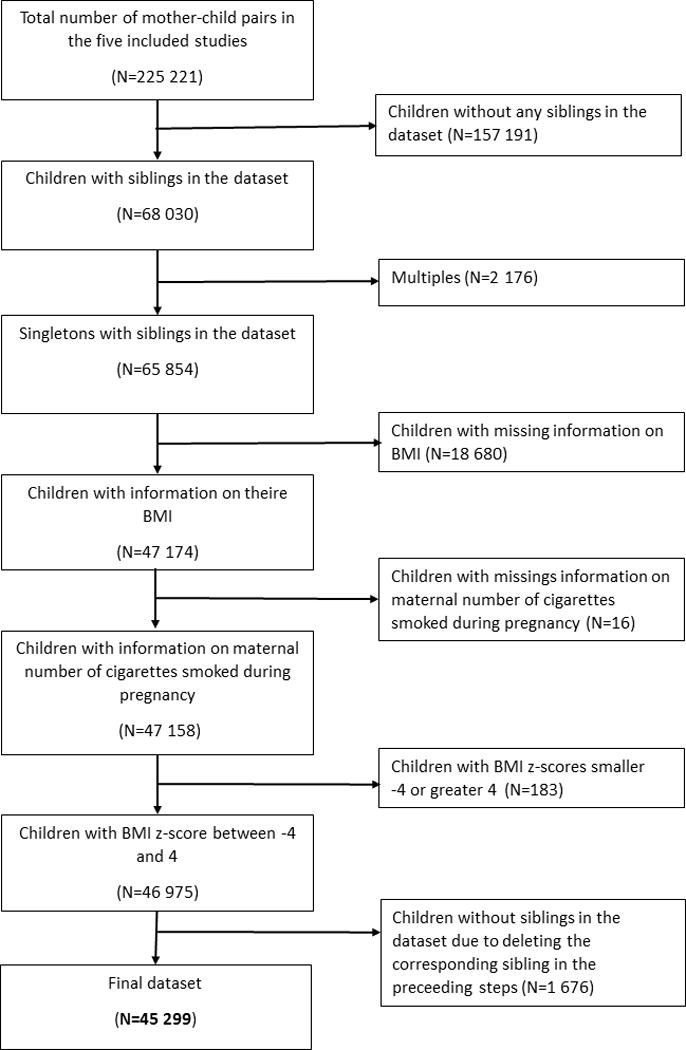
Flow chart of depicting exclusion of the individual children from the five studies providing information on siblings
A description of the five studies included in the meta-analysis is provided in Table S2: The number of participants provided in each study varied between 36 and 24 476. Four studies provided information about maternal weight before the respective pregnancy and one study only at assessment of the child’s BMI. Information on breastfeeding in the respective pregnancy was provided in four out of five studies. Data about maternal education at the respective pregnancy was reported in four out of five studies. Study quality was good for all included studies (Table S3).
Table 1 shows the characteristics of the study participants. The mean age of the included children was 5.6 years with a range between two and 19 years. The mean BMI z-score was 0.36. There was equal distribution of boys and girls. The proportion of offspring with overweight and obesity was 11.0% and 3.8% respectively. 34.2% of the children were breastfed. The proportion of mothers with overweight and obesity was 20.5%, and 14.7% respectively. 50.0% of the mothers had 10 years or more of school education. Thirty three percent of the mothers (N=14956) smoked with a mean number of 13.3 cigarettes per day.
Table 1.
Study participant characteristics and distributions of relevant co-variates
| Study Participant Characteristics | Mean (SD) respectively % (absolute number) |
|
|---|---|---|
| Child Age (in years) | 5.61 (2.37) | |
| Child BMI z-score | 0.36 (1.08) | |
| Average nr of Cigarettes/Day during Pregnancy among smokers | 13.33 (10.44) | |
| Sex | male | 49.94 (22624) |
| female | 50.06 (22675) | |
| Child Weight Status | Normal Weight | 85.17 (38580) |
| Overweight | 11.01(4989) | |
| Obese | 3.82 (1730) | |
| Breastfeeding | Yes | 34.2 (29804) |
| No | 65.8 (15495) | |
| Birth Weight for Gestational Age* | Normal | 73.28 (33189) |
| Small | 16.75 (7591) | |
| Large | 9.97 (4519) | |
| Preterm (<37 weeks) | Yes | 10.09 (4574) |
| No | 89.91 (40725) | |
| Maternal BMI | Normal Weight | 57.41 (26003) |
| Underweight | 7.37 (3342) | |
| Overweight | 20.49 (9281) | |
| Obese | 14.71(6673) | |
| Maternal Smoking Status | Yes | 33.02 (14956) |
| No | 66.98 (30343) | |
| Maternal Education | 10 or more years of schooling | 50.00(23569) |
| Less than 10 years of schooling | 50.00 (21730) | |
Birth weight for gestational age applying country specific percentiles defined as: Small, <10th percentile; Large, >90th percentile; Normal, between 10th and 90th percentile.
Assuming a linear association for the number of cigarettes and offspring BMI z-score, an increase per cigarette of 0.007 (95% CI=0.006; 0.008) for the within-family effect and 0.000 (95% CI=-0.003; 0.003) for the between-family effect was observed.
When allowing also for non-linear association, the effect of maternal number of cigarettes smoked per day during pregnancy on offspring BMI z-score is displayed as two slopes (Figure 3). For the within-family effect, a linear increase up to about 30 cigarettes per day was observed with an effect of 0.22 (95% CI=0.18; 0.27) for 30 cigarettes per day compared to no cigarette smoked during pregnancy, indicating an increase per cigarette of 0.007 (95% CI=0.006; 0.009) in offspring BMI z-scores. For higher quantities of smoking a flattening of the effect was observed. There was no between-family effect (reflected in the average number of cigarettes smoked by the mother during all pregnancies) until number of cigarettes smoked was higher than about 25 cigarettes. For higher number of cigarettes there was an incremental effect. For example, an effect size of about 0.33 (95% CI=0.06; 0.60) for 40 cigarettes, indicating an increase of BMI z-score of 0.33 in families where mothers smoked 40 cigarettes per day averaged over all pregnancies compared to families where mothers smoked an average 0 to 25 cigarettes per day during all their pregnancies.
Figure 3.
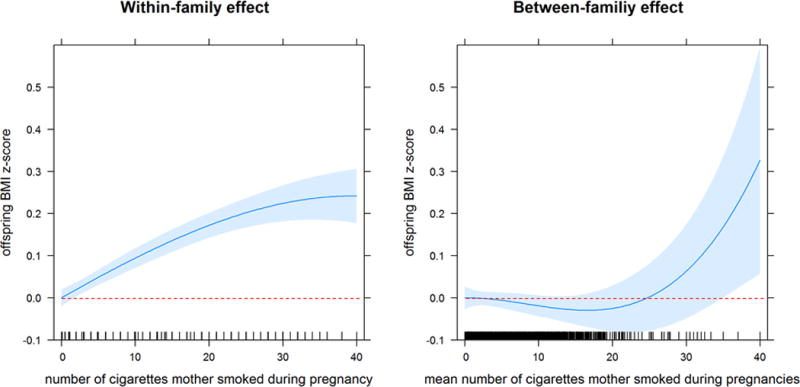
Within-family and between-family effect for number of cigarettes smoked during pregnancy on offspring BMI z-score in total sample
Adjustment for SGA, LGA and preterm delivery, covariates which might be in the causal pathway, did only marginally change the effect (Figure S1).
DISCUSSION
This meta-analysis finds a linear association between the number of cigarettes smoked during pregnancy and the BMI z-score in the offspring, which could not be explained by a number of possible confounders or residual confounding related to family factors shared by siblings. This within-family effect increased up to 30 cigarettes per day by 0.01 BMI z-scores per increment of one cigarette per day.
We identified only two studies that previously attempted to assess the association of maternal smoking during pregnancy with childhood overweight and BMI z-score controlled for family factors by examining siblings.8,9 In a Swedish cohort with sibling pairs, an analysis stratified by maternal smoking habits over the two pregnancies suggested confounding of the association by family factors.9 Analysis of the Collaborative Perinatal Project data with fixed effects models, however, showed an association independent of family factors.8 By including all studies identified in this IPD meta-analysis, our sample size was increased by a factor of two providing a larger dataset with information on the number of cigarettes smoked by the mother. Extension of Gilman et al.’s analysis in our dataset including data from three different countries yielded effect estimates with boundaries excluding the null.
In addition to the large sample size, another strength of the study is the dose-response analysis using B-splines to allow also for non-linear associations. To account for family factors, a mixed-effects regression model was applied including all available sibling data. A linear association for doses up to 30 cigarettes per day with an increase of the offspring’s BMI z-score of 0.01 per cigarette was observed. The within family effect is linear starting at one cigarette per day, indicating that among smoking mothers every additional cigarette may matter. This stands in accordance with results from the only two other studies examining dose-response by cigarettes without building dose categories.25,26 These studies, however, used risk for overweight/obesity as outcome rather than continuous BMI z-score, hence effect sizes are not directly comparable.
The advantage of using this approach to account for family factors is that within-family and between-family effects are separated.16 The within-family effect includes all family factors shared between siblings that can neither be specified nor quantified. Conventional adjustment can only be performed for measured covariates. Control for unmeasured genetic factors is achieved in the model estimate for the between-family impact on smoking unless one of the siblings compared had been conceived out of wedlock or other forms of family partnership. Our sibling analysis similarly controls for unmeasured shared lifestyle factors. Adjustment for ‘maternal factors’ like maternal weight category, which may change in between pregnancies, was additionally preformed to account for maternal weight related differences in the intra-uterine milieu. Breastfeeding, which may vary between siblings was included as a potential confounder in all models. Unfortunately we had no information on diet and physical activity in the children which might be in the causal pathway. Several elements of diet and lifestyle are likely to be included in the between-family effect, since important risk factors for childhood obesity like fast food consumption, breakfast and sedentary behavior have been shown to be correlated between siblings.27
A limitation of the study might be, that it is still underpowered. In 19 630 of the in total 45 570 included mother-child pairs, there was no change in smoking behavior between pregnancies (18 525 children were from non-smoking families, and for 1 105 children mothers reported to smoke exactly the same number of cigarettes during all their pregnancies) leaving only 25 940 informative mother-child pairs with a change in smoking behavior for our analysis. Nevertheless, a linear increase of the BMI z-score by number of cigarettes smoked per day with a positive confidence limit was found. Unfortunately, we could not assess potential effect modification by age in this study population, because the majority of children was in preschool age. Further, if there are unmeasured factors that caused women to change their smoking behaviors, and these have associations with child development and BMI, this could bias results.
The innovation in applying this approach is that both the within-family and between-family effects of the number of cigarettes smoked on the BMI z-score are modeled using B-splines allowing for non-linear associations. Applying this innovative approach we were able to assess the nature of the dose dependency of maternal smoking and later BMI z-scores in the offspring with adjustment for unmeasured family factors and a range of potential confounders not captured by the within family factor.
By definition empirical data cannot prove causal relationship between maternal smoking in pregnancy and higher BMI z-scores later in the offspring. Compared to previous studies, these findings, however, increase the probability of a causal relationship by demonstrating a linear dose effect and after adjustment for within-family factors which cannot be included in conventional models. The observed stable postnatal changes in the AHRR gene methylation profile in offspring exposed to maternal smoking in pregnancy might provide a mechanism for long term changes in homeostasis of the body composition related to maternal smoking.28
CONCLUSION
The number of cigarettes mothers smoke per day during pregnancy is positively associated with offspring BMI z-score after adjustment for a number of measurable confounders and residual confounding related to shared lifestyle among siblings. A linear increase for doses up to 30 cigarettes per day was observed, indicating that among smoking mothers every additional cigarette may matter. These findings have implications for counselling women planning pregnancy or already pregnant. Since there is no threshold for the impact of maternal smoking of their children’s BMI there is no safe number of cigarettes during pregnancy with respect to the risk for higher BMI z-scores.
Supplementary Material
Figure S1: Within-family and between-family effect for number of cigarettes smoked during pregnancy on offspring BMI z-score when adjusted for SGA, LGA and preterm delivery
Acknowledgments
We would like to thank the participating families of all studies for the use of data.
This work was supported by the Deutschen Forschungsgesellschaft (German Research Foundation, DFG) [KR 1926/9-1, KU1443/4-1]. Dr. Gilman’s contribution was supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC.
Financial disclosure statement:
Rüdiger von Kries has received funding from the Deutschen Forschungsgesellschaft (German Research Foundation, DFG) [KR 1926/9-1].
Dr. Gilman’s contribution was supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Footnotes
Conflict of Interest: All authors declare that they have no conflict of interest.
All other authors have no financial disclosures.
References
- 1.Monasta L, Batty G, Cattaneo A, et al. Early-life determinants of overweight and obesity: a review of systematic reviews. Obes Rev. 2010;11:695–708. doi: 10.1111/j.1467-789X.2010.00735.x. [DOI] [PubMed] [Google Scholar]
- 2.Harrod CS, Reynolds RM, Chasan-Taber L, et al. Quantity and timing of maternal prenatal smoking on neonatal body composition: the Healthy Start study. J Pediatr. 2014;165:707–712. doi: 10.1016/j.jpeds.2014.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Syme C, Abrahamowicz M, Mahboubi A, et al. Prenatal exposure to maternal cigarette smoking and accumulation of intra-abdominal fat during adolescence. Obes Silver Spring. 2010;18:1021–1025. doi: 10.1038/oby.2009.354. [DOI] [PubMed] [Google Scholar]
- 4.Rayfield S, Plugge E. Systematic review and meta-analysis of the association between maternal smoking in pregnancy and childhood overweight and obesity. J Epidemiol Community Health. 2016;71:162–173. doi: 10.1136/jech-2016-207376. [DOI] [PubMed] [Google Scholar]
- 5.Riedel C, Schönberger K, Yang S, et al. Parental Smoking and Childhood Obesity: Higher Effect Estimates for Maternal Smoking in Pregnancy Compared to Paternal Smoking - A Meta-Analysis. Int J Epidemiol. 2014;43:1593–606. doi: 10.1093/ije/dyu150. [DOI] [PubMed] [Google Scholar]
- 6.Oken E, Levitan EB, Gillman MW. Maternal smoking during pregnancy and child overweight: systematic review and meta-analysis. Int J Obes. 2008;32:201–210. doi: 10.1038/sj.ijo.0803760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ino T. Maternal smoking during pregnancy and offspring obesity: meta-analysis. Pediatr Int. 2010;52:94–99. doi: 10.1111/j.1442-200X.2009.02883.x. [DOI] [PubMed] [Google Scholar]
- 8.Gilman SE, Gardener H, Buka SL. Maternal smoking during pregnancy and children’s cognitive and physical development: a causal risk factor? Am J Epidemiol. 2008;168:522–531. doi: 10.1093/aje/kwn175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Iliadou AN, Koupil I, Villamor E, et al. Familial factors confound the association between maternal smoking during pregnancy and young adult offspring overweight. Int J Epidemiol. 2010;39:1193–1202. doi: 10.1093/ije/dyq064. [DOI] [PubMed] [Google Scholar]
- 10.Raum E, Kupper-Nybelen J, Lamerz A, Hebebrand J, Herpertz-Dahlmann B, Brenner H. Tobacco smoke exposure before, during, and after pregnancy and risk of overweight at age 6. Obes Silver Spring. 2011;19:2411–2417. doi: 10.1038/oby.2011.129. [DOI] [PubMed] [Google Scholar]
- 11.Yang S, Decker A, Kramer MS. Exposure to parental smoking and child growth and development: a cohort study. BMC Pediatr. 2013;13:104. doi: 10.1186/1471-2431-13-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Donovan SJ, Susser E. Commentary: Advent of sibling designs. Int J Epidemiol. 2011;40:345–349. doi: 10.1093/ije/dyr057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Susser E, Eide MG, Begg M. Invited commentary: The use of sibship studies to detect familial confounding. Am J Epidemiol. 2010;172:537–539. doi: 10.1093/aje/kwq196. [DOI] [PubMed] [Google Scholar]
- 14.Lahey BB, D’Onofrio BM. All in the Family: Comparing Siblings to Test Causal Hypotheses Regarding Environmental Influences on Behavior. Curr Dir Psychol Sci. 2010;19:319–323. doi: 10.1177/0963721410383977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr Suppl. 2006;450:76–85. doi: 10.1111/j.1651-2227.2006.tb02378.x. [DOI] [PubMed] [Google Scholar]
- 16.Desai M, Begg MD. A Comparison of Regression Approaches for Analyzing Clustered Data. Am J Public Health. 2008;98:1425–1429. doi: 10.2105/AJPH.2006.108233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Begg MD, Parides MK. Separation of individual-level and cluster-level covariate effects in regression analysis of correlated data. Stat Med. 2003;22:2591–2602. doi: 10.1002/sim.1524. [DOI] [PubMed] [Google Scholar]
- 18.Sharma AJ, Cogswell ME, Li R. Dose-response associations between maternal smoking during pregnancy and subsequent childhood obesity: effect modification by maternal race/ethnicity in a low-income US cohort. Am J Epidemiol. 2008;168:995–1007. doi: 10.1093/aje/kwn223. [DOI] [PubMed] [Google Scholar]
- 19.Eilers PHC, Marx BD. Flexible smoothing with B -splines and penalties. Stat Sci. 1996;11:89–121. [Google Scholar]
- 20.Bates D, Mächler M, Bolker B, Walker S. Fitting Linear Mixed-Effects Models Using lme4. J Stat Softw. 2015;67:1–48. [Google Scholar]
- 21.Zhang Z. Missing data imputation: focusing on single imputation. Ann Transl Med. 2016;4:9. doi: 10.3978/j.issn.2305-5839.2015.12.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rubin DB. Multiple Imputation for Nonresponse in Surveys. Wiley-Interscience; Hoboken: 2004. [Google Scholar]
- 23.Grzeskowiak LE, Hodyl NA, Stark MJ, Morrison JL, Clifton VL. Association of early and late maternal smoking during pregnancy with offspring body mass index at 4 to 5 years of age. J Dev Orig Health Dis. 2015;6:485–492. doi: 10.1017/S2040174415007151. [DOI] [PubMed] [Google Scholar]
- 24.Oken E, Huh SY, Taveras EM, Rich-Edwards JW, Gillman MW. Associations of maternal prenatal smoking with child adiposity and blood pressure. Obes Res. 2005;13:2021–2028. doi: 10.1038/oby.2005.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gorog K, Pattenden S, Antova T, et al. Maternal smoking during pregnancy and childhood obesity: results from the CESAR Study. Matern Child Health J. 2011;15:985–992. doi: 10.1007/s10995-009-0543-5. [DOI] [PubMed] [Google Scholar]
- 26.Møller SE, Ajslev TA, Andersen CS, Dalgård C, Sørensen TIA. Risk of childhood overweight after exposure to tobacco smoking in prenatal and early postnatal life. PloS One. 2014;9:e109184. doi: 10.1371/journal.pone.0109184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Berge JM, Meyer C, MacLehose RF, Crichlow R, Neumark-Sztainer D. All in the Family: Correlations between Parents’ and Adolescent Siblings’ Weight and Weight-related Behaviors. Obes Silver Spring. 2015;23:833–839. doi: 10.1002/oby.21036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Macaulay E, Donovan E, Leask M, et al. The importance of early life in childhood obesity and related diseases: a report from the 2014 Gravida Strategic Summit. J Dev Orig Health Dis. 2014;5:398–407. doi: 10.1017/S2040174414000488. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1: Within-family and between-family effect for number of cigarettes smoked during pregnancy on offspring BMI z-score when adjusted for SGA, LGA and preterm delivery


