Abstract
Objective
Among men who have sex with men (MSM), HIV sexual risk and poor self-care behavior is associated with syndemics, or co-occurring psychosocial problems. Though prior research has demonstrated an additive total effect of syndemics on HIV risk behavior and infection, mostly within cross-sectional designs, it is possible that these associations are not direct, but rather that syndemics disrupt relevant individual-level mediating psychological variables. One of the most common individual-level psychological variables that predicts health behavior generally, and HIV risk behavior specifically, is self-efficacy. This study sought to examine the potential effects of syndemics on condomless sex via condom-use self-efficacy as an intermediary variable.
Methods
In high-risk MSM (N=197), across three time points (baseline, 3-months, and 6-months) we used latent growth curve modeling to test the degree to which self-efficacy mediated the relationship between syndemics (heavy alcohol use, substance use disorder, sexual compulsivity, depression, social anxiety, intimate partner violence, childhood sexual abuse) and condomless anal sex.
Results
The baseline analyses were consistent with an indirect effect of the association between syndemics and condomless sex through self-efficacy. Prospective longitudinal mediation was partially supported such that baseline syndemics were associated with lower baseline self-efficacy, which in turn predicted higher increases in condomless anal sex across time.
Conclusions
These findings provide preliminary evidence (due to the partial support for the longitudinal model) that syndemics themselves may not be directly causal in their association with condomless sex, but the association may be through modifiable social-cognitive mechanisms such as condom self-efficacy.
Keywords: Men who have sex with men (MSM), syndemics, self-efficacy, HIV risk, sex
INTRODUCTION
Men who have sex with men (MSM) are the group with the greatest HIV risk in the U.S., with recent estimates that MSM are 83 times more likely than exclusively heterosexual men to be diagnosed with HIV in their lifetimes (Centers for Disease Control and Prevention, 2016). Syndemics are multiple, comorbid psychosocial conditions (e.g., substance use, depression, intimate partner violence, childhood sexual abuse, post-traumatic stress disorder, etc.) that interact to create increased risk for adverse behavioral outcomes (Singer, 1994; Stall, Friedman, & Catania, 2008). The theory of syndemic production among MSM posits that throughout development, sexual minority men develop, since childhood, certain vulnerabilities that can be associated with increased risk for experiencing psychosocial problems, including vulnerability to childhood sexual abuse, depression, and substance use (Stall, Friedman, & Catania, 2008). Moreover, once an individual experiences one of these psychosocial conditions, he or she is at greater risk of developing other psychosocial conditions, or syndemics (e.g., Kessler et al., 2005). Importantly, the presence of these psychosocial conditions that comprise syndemics may cause decreased self-efficacy (Corrigan & Watson, 2002), which may be an important variable related to perpetuating the synergistic effects of syndemics and to poorer health outcomes. Indeed, syndemics conditions are associated with each other and with physical health problems (Stall et al., 2008; Safren, Reisner, Herrick, Mimiaga, & Stall, 2010; Stall et al., 2003).
Many of the existing studies of syndemics in MSM are cross-sectional (Hirshfield et al., 2015; Mustanski et al., 2007; Parsons et al., 2012; Stall et al., 2003) and generally have found that, in different age groups and geographic settings, the number of syndemics are additively and directly associated with condomless anal sex or HIV incidence. Because of the cross-sectional nature of many of the studies, they reveal that the risk occurs within the context of these problems, but do not demonstrate temporality. An emerging second set of studies of syndemics in MSM are longitudinal in design, which allows the examination of temporality, and therefore stronger evidence for possible causality. Mimiaga et al. (2015) examined 4,295 HIV-negative MSM in six U.S. cities over 4 years, as part of a larger psychosocial intervention (Project EXPLORE; Koblin, Chesney, Coates, & EXPLORE Study Team, 2004). The results of this study found that syndemics were additively associated with high-risk sexual behavior and HIV seroconversion over time (Mimiaga, O’Cleirigh, et al., 2015). In another longitudinal study, Guadamuz et al. (2014) explored the relationship between syndemics and HIV incidence and prevalence in 1,292 Thai MSM over a maximum of 3.8 years. This study also found that greater numbers of syndemics at baseline were additively associated higher levels of condomless sex and greater HIV incidence. Both the cross-sectional and the longitudinal studies reviewed above examine direct effects of syndemics on sexual risk or HIV acquisition, but have not examined potential mediators or intermediary variables.
Despite the studies showing associations and direct effects of syndemics to HIV risk, to our knowledge, research has yet to address how syndemics impact HIV risk. It is likely that it is not simply the presence of the syndemic conditions alone, but rather that these syndemics influence other psychological variables that typically predict protective health behaviors. To address this question of how syndemics impact HIV risk, it is helpful to consult social-psychological conceptual models of behavior. For example, the Theory of Reasoned Action (Ajzen & Fishbein, 1980; Albarracín, Johnson, Fishbein, & Muellerleile, 2001; Fishbein & Ajzen, 1975) posits that subjective norms and attitudes influence one’s intention, which in turn influences future behavior. Another model, the Health Belief Model (Becker, 1974; Rosenstock, 1974), hypothesizes that one’s motivations, the value of illness threat reduction, and the probability that health-behavior will reduce the threat influence one’s likelihood of engaging in the health-behavior through demographic, structural, attitudes, medical interaction, and enabling factors. Additionally, Social Cognitive Theory (SCT), one of the most common social-psychological conceptual models, posits self-efficacy, the degree to which a person believes that they can succeed in using condoms in various sexual situations, as the primary proximal predictor of condom use (Bandura, 1994; Wulfert, Safren, Brown, & Wan, 1999; Wulfert & Wan, 1993, 1995).
SCT hypothesizes that sexual attitudes, negative expectancies, disease prevention, peer group comparison, and perceived vulnerability influence self-efficacy, which in turns predicts condom use (Wulfert & Wan, 1993). Prior research in gay men demonstrated that a substantial portion of the variance in condom use was predicted by conceptually analogous concepts across the aforementioned models, but self-efficacy significantly accounted for additional variance over and above these conceptually analogous variables (Wulfert, Wan, & Backus, 1996). Additionally, in one study (Wulfert & Wan 1995) three models were compared, the Health Belief Model, the Theory of Reasoned Action, and SCT (with self-efficacy as a key predictor), and found that the SCT model accounted for 79% of the variance, the most of the three, with the Health Belief Model predicting 28% of the variance in intentions to use condoms, and the Theory of Reasoned Action predicting 68% of the variance.
In addition, extant literature on various individual syndemic conditions suggests that condom use self-efficacy may mediate the relationship between such syndemic conditions and increased HIV risk via condomless sex. In MSM, with respect to depression, condom use self-efficacy has been shown to at least partially mediate the relationship between depression and sexual HIV risk behaviors (Alvy et al., 2011; Tucker et al., 2013). Similarly, research suggests that social anxiety is related to condomless anal sex, and that condom use self-efficacy is an important variable among MSM with social anxiety, who may fear negative evaluation regarding condom use-related behaviors (Hart & Heimberg, 2005). Additionally, the relationship between sexual compulsivity and substance use and HIV risk may also be mediated by self-efficacy (O’leary et al., 2005). Research has also shown that increased substance use is related to increased HIV risk and that this relationship is partially mediated by condom use self-efficacy (O’leary et al., 2005).
Taken together, the literature reviewed above suggests that the way in which syndemics affect health behaviors is via disrupting social-psychological variables proximal to health behaviors. One of the most commonly studied variable associated with is self-efficacy. Accordingly, the current study hypothesized that a social cognitive variable, self-efficacy, would mediate the additive effects of syndemics on an HIV risk indicator--condomless sex with casual partners, in MSM in the context of a longitudinal study.
METHODS
Participants
Participants (N with available data=197) for the current study were part of a larger longitudinal cohort aimed at identifying acute HIV infection using home rapid HIV testing at a community health center in New England with expertise in sexual and gender minority health (see also Blashill et al., 2016). To qualify, participants were required to be born male at birth (all participants identified as male gender as well), willing and able to provide written informed consent, be 18 years old or older, test HIV-negative at baseline via FDA approved rapid HIV testing, and self-report high risk for HIV-1 acquisition. High risk for HIV-1 acquisition was defined as any one of the following: At least one instance of no condom use during anal intercourse with an HIV-infected male partner or a male partner of unknown HIV status during the last 6 months; anal intercourse with more than 3 male sex partners during the last 6 months; exchange of money, gifts, shelter, or drugs for anal sex with a male partner during the last 6 months; or sex with a male partner and sexually transmitted infection (STI) diagnosis, during the last 6 months or at screening. Excluded participants were men currently using pre-exposure prophylaxis (PrEP) or planning to do so, those participating in an HIV vaccine trial or previous participation in HIV vaccine trial and receiving non-placebo. All participants completed an informed consent process, including signing a consent form, and all study procedures were approved and monitored by the institutional review board at Fenway Health.
Procedures
After a pre-screening procedure to assess initial eligibility, participants attended a baseline study visit that involved administration of the computer-assisted questionnaires and HIV counseling and testing. For the present analysis, all available data were used, and this included participants who had available data on the primary variables (and who did not drop out). Accordingly, the baseline n=197), 3-month n=145, and 6-month n=124. There were no significant differences between those who attended all visits and those who dropped out on study variables.
Measures
All measures, including general demographics, were assessed via computer assisted self-interview (CASI).
The number of psychosocial syndemics (alcohol use disorder, substance use disorder, sexual compulsivity, depression, social anxiety, intimate partner violence, childhood sexual abuse) experienced by each participant was assessed in the following way. If a participant endorsed experiencing or engaging in a syndemic indicator, it was coded 1, if not it was coded 0; and then the scores were summed. The syndemics utilized are described below, and were assessed at baseline.
Childhood sexual abuse (CSA) was assessed via three standard questions using the Finkelhor definition (Finkelhor, 1994). These questions assessed whether one ever had a wanted or unwanted, with or without contact, sexual experience with someone 5 or more years older when age 12 or younger, and/or with someone 10 or more years older when age 13–16 (Lenderking et al., 1997). An affirmative response to either was considered screening in for CSA.
Intimate partner violence
Intimate partner violence (IPV) was assessed via a 4-item measure adapted from the HPTN061 study (Williams et al., 2015). This measure assessed whether one has ever experienced emotional abuse, physical abuse, stalking, and/or sexual abuse from one’s intimate partner. Endorsing any one type of abuse was considered as meeting criteria for this syndemic.
Substance Use Disorder
The presence or absence of a substance use disorder was assessed via the MINI 6.0 (Sheehan & Lecrubier, 2010) questions for substance abuse or dependence. These questions map onto the DSM-IV criteria for substance abuse or dependence which were used as the cutoff (any 1 symptom=criteria for abuse).
Problematic Alcohol Use
The potential presence or absence of a potential alcohol use disorder (AUD) was assessed via the CAGE (Ewing, 1984), which is a self-report screening instrument to identify persons experiencing alcohol problems. Here participants responded yes or no to 4 items that assess for the presence of core symptoms of AUD. The CAGE has been shown to be a brief, but valid assessment of AUD, successfully discriminating between those with or without the disorder among various demographic groups (Buchsbaum, Buchanan, Centor, Schnoll, & Lawton, 1991; Bush, Shaw, Cleary, Delbanco, & Aronson, 1987; Knowlton, McCusker, Stoddard, Zapka, & Mayer, 1994; Mayfield, McLeod, & Hall, 1974), using the cut score of 2 which we employed in the present study. KR-20 for this measure was .78.
Sexual compulsivity
Sexual compulsivity was assessed by the Kalichman Sexual Compulsivity Scale (SCS; Kalichman et al., 1994), which is a 10-item measure of one’s ability to control sexual thoughts and behaviors. Participants indicated their responses on a 4-point scale in which responses range from 1 (not at all like me) to 4 (very much like me), and higher scores indicated an increased likelihood of sexual compulsivity. In the current study, we considered participants who reported a score of 20 or greater on the SCS as experiencing problematic levels of sexual compulsivity, as it indicates “mild” above on the scale. Chronbach’s alpha for this scale was .90 at baseline.
Depression
Depression was assessed via the 9-item depression severity scale of the Patient Health Questionnaire (PHQ-9; Spitzer, Kroenke, Williams, & and the Patient Health Questionnaire Primary Care Study Group, 1999), which is both a measure of diagnostic criteria and depression severity. Responses were indicated on a 4-point scale from 0 (not at all) to 3 (nearly every day). We used a score of 5 or above as the cut score, indicating mild (potentially clinically significant) depression or greater. Chronbach’s alpha at baseline was .91. Consideration was given to using a higher cutoff for more severe depression, however we used the cutoff of mild because a symptom of severe depression is loss of libido which would therefore inhibit sexual behavior.
Social anxiety
Social anxiety was assessed via the Social Phobia Inventory (SPIN; Connor et al., 2000) which is a 17-item diagnostic screening measure of social anxiety that is also a measure of severity and is sensitive to change over time. Participants rate the presence and severity of core symptoms (e.g., avoidance, fear, and somatic discomfort) on a 5-point scale from 0 (not at all) to 4 (extremely). On the SPIN, participants who endorsed scores greater than or equal to 19 experience mild (potentially clinically significant) levels of social anxiety or greater. Chronbach’s alpha for this measure was .94. Similar to depression, we used “mild” because a symptom of more severe social anxiety is severe avoidance of social interactions, which would include sexual situations.
Condom-use self-efficacy
The mediator variable, condom-use self-efficacy, was assessed via a two-item measure (Wulfert et al., 1999) that questions one’s self-reported perceived ability to use a condom in sexual situations (e.g. “How sure are you of your ability to always use condoms”). Participants indicated their response on a 7-point scale ranging from 1 (very unsure) to 7 (very sure); and the two items were averaged, with higher scores therefore indicating greater self-efficacy. This measure has been shown to be a significant and robust predictor of condom use and condom use intentions in prior research (Wulfert et al., 1999; Wulfert and Wan, 1995). Reliability was estimated using the Spearman-Brown coefficient, which is appropriate for two-item measures (Eisinga, Grotenhuis, & Pelzer, 2013), at each time point, with values at .93 at baseline, .95 at 3-month, and .90 at 6-month. While other measures of self-efficacy were considered, this brief 2-item measure was chosen because it has been successful in our prior research, and appropriate for an observational study in terms of participant burden.
Condomless sex
The sexual risk outcome was condomless sex acts with casual partners in the past three months, which we had used in a prior analysis with this sample (Blashill et al., 2016). The rationale behind using condomless sex with casual partners as a “risky” event is because it is typically not possible to know with certainty a partner’s HIV status/viral load, PrEP use/adherence patterns, STI history compared to primary partners where there may be more of an opportunity to have repeated discussions over time and/or the ability to more comprehensively evaluate repeated conversations over time in the context of an enduring sexual relationship. This outcome variable is commonly used in recent epidemiological studies clinical trials involving sexual behavior of MSM (e.g., Millar, Starks, Grov, & Parsons, 2017; Mustanski, Feinstein, Madkins, Sullivan, & Swann, 2017; Shadaker, Magee, Paz-Bailey, Hoots, & NHBS Study Group, 2017).
Statistical Analysis
The number of syndemics experienced by each participant was summed and then categorized into four categories based on the distribution as done in prior research (e.g., Blashill et al., 2015; Stall et al., 2003): no syndemics (none), 1 syndemics, 2 syndemics, or 3 or more syndemics.
To analyze the effect of syndemics on the outcome, condomless sex, via self-efficacy, a parallel process latent growth curve model (e.g., Selig & Preacher, 2009) was employed via Mplus (v7.4). In this approach, baseline values of syndemics were modeled to predict both the intercept and slope of self-efficacy and intercept and slope of condomless anal sex. Intercepts were set at the baseline values and slopes represent linear change across the three time points (baseline, 3 month, and 6 month). Given that the outcome variable is count in nature, negative binomial regressions were used for pathways predicting condomless anal sex. Within Mplus, when the outcome variable is count, traditional model fit indices (e.g., CFI, TLI, RMSEA) are not available. To test cross-sectional mediation, paths were modeled with syndemics predicting the intercept of condomless anal sex through the intercept of self-efficacy. To test longitudinal mediation, paths were modeled with syndemics predicting the slope of condomless anal sex through the intercept and slope of self-efficacy. These analyses use all available data for modeling. Outliers were defined as z-score values +/− 3.3 SD from the mean, with nine outliers identified across the dataset. Outlier values were transformed to the next highest non-outlier value, to retain the rank order of the value. Because we did not hypothesize there would be differences in the associations among variables by demographic variables such as race/ethnicity, they are not included as covariates. However, sensitivity analyses were repeated with these as covariates. Additionally, all analyses were repeated with any condomless sex versus the a-priori outcome variable, condomless sex with casual partners, as an additional set of sensitivity analyses.
Results
Participant demographics and baseline study data on syndemics are depicted in Table 1. On average, the participants were middle-aged, with almost three-quarters of the sample White, a quarter African American, and 15% Hispanic/Latino. All participants identified as male. In this sample, the frequency of syndemics was relatively high (see Table 2), and relatively equally distributed across the four categories. Accordingly, only 20% had no syndemic indicators, and almost 30% had three or more. Mean and standard deviation scores for self-efficacy and condomless sex variables are depicted in Table 3.
Table 1.
Selected Participant Demographics and Baseline Syndemics Scores
| Demographics | N (%) | |
|---|---|---|
| Ethnicity | ||
| Hispanic/Latino | 30 (15.2%) | |
| Non-Hispanic | 167 (84.8%) | |
| Race1 | ||
| Asian | 7 (2.1%) | |
| Black, African-American | 43 (20.9%) | |
| White | 139 (70.2%) | |
| Multi-racial/Other | 12 (7.9%) | |
| Sexual Orientation | ||
| Homosexual/Gay | 151 (76.6%) | |
| Bisexual | 37 (18.8%) | |
| Heterosexual/Straight | 5 (2.5%) | |
| Don’t Know | 1 (0.5%) | |
| Other | 3 (1.5%) | |
| Ever Received HIV Test (prior to this study) | ||
| Yes | 186 (94.4%) | |
| No | 11 (5.6%) | |
|
| ||
| M (SD) | ||
|
| ||
| Age (in years) | 37 (11.6) | |
|
| ||
| Syndemics | M (SD) | % pos |
|
| ||
| PHQ | 4.28 (5.13) | 21.6 |
| SPIN | 11.35 (12.86) | 8.5 |
| SC | 15.89 (5.50) | 21.5 |
| CAGE | .96 (1.29) | 29.4 |
| SU | 21 | |
| IPV | 50.5 | |
| CSA | 40.1 | |
Note.
The sums of the frequencies and percentages for categories of Race are greater than the total sample, and 100%, as participants were instructed to select all categories that apply and were therefore not mutually exclusive. PHQ=Patient Health Questionnaire, Depression.
SPIN=Social Phobia Inventory, SC=Sexual Compulsivity Scale, CAGE=Alcohol Screening, SU=Any Substance Use Diagnosis, IPV=Interpersonal Violence, CSA=Childhood Sexual Abuse
Table 2.
Frequency, Percent, and Cumulative Percent of Syndemics
| Syndemics Category | Frequency (n) | Percent (%) | Cumulative Percent (%) |
|---|---|---|---|
| .00 | 40 | 20.0 | 20.3 |
| 1.00 | 48 | 24.0 | 44.7 |
| 2.00 | 50 | 25.0 | 70.1 |
| 3.00 | 59 | 29.5 | 100.0 |
|
| |||
| Total | 197 | 98.5 | 100.0 |
Table 3.
Self-efficacy and Condomless Sex with Casual Partners over the Study Period
| Baseline M (SD) |
3-month M (SD) |
6-month M (SD) |
|
|---|---|---|---|
| Condomless Anal Sex | 4.07 (6.20) | 2.67 (4.12) | 2.55 (4.14) |
| Self-Efficacy | 4.74 (1.97) | 4.84 (2.07) | 4.86 (1.94) |
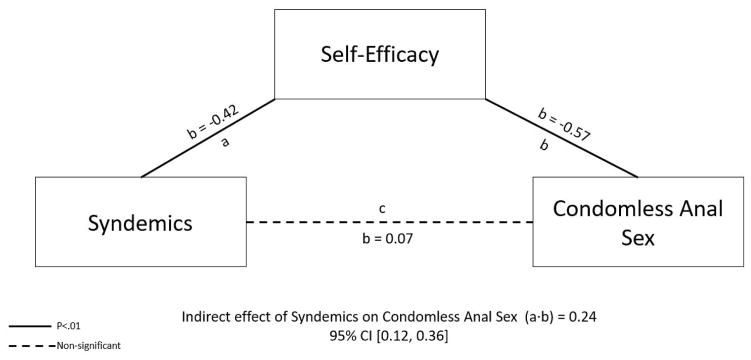
In the baseline data model (Figure 1), syndemics significantly predicted self-efficacy (b = −0.42, SE = 0.12, t = −3.75, p < .0001) but not condomless anal sex (b = 0.07, SE = 0.08, t = 0.81, p = .417), with greater endorsement of syndemic indicators predicting lower self-efficacy. Self-efficacy significantly predicted condomless anal sex (b = −0.57, SE = 0.08, t = −7.48, p < .0001, with lower self-efficacy predicting increased condomless anal sex. Accordingly, the indirect effect of syndemics to condomless anal sex through self-efficacy was also significant (b = 0.24, SE = 0.08, 95% CI: 0.12, 0.36, t = 3.17, p = .002), providing support for cross-sectional indirect effects of syndemics on condomless anal sex through its association with self-efficacy.
Figure 1.
Cross sectional indirect effect of syndemics on condomless anal sex with casual partners though self-efficacy.
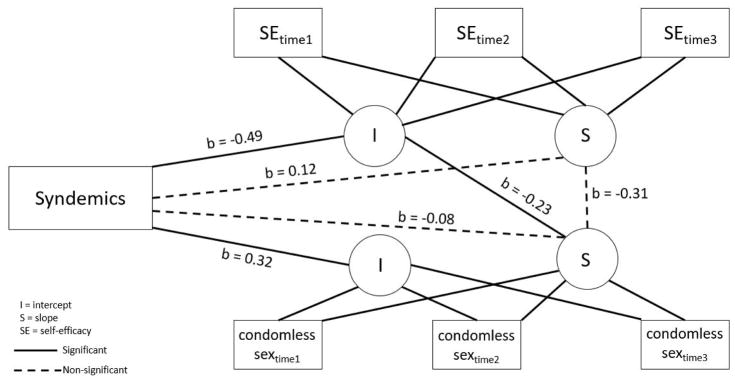
Over the course of the study, rates of condomless sex with casual partners significantly decreased (b = −.317, SE = .112, t = −2.83, p = .005; intercept = .66, SE= .123, t = 5.39, p < .0001) and self-efficacy scores were generally stable (b= −.013, SE = .084, t = −.153, p = .87, intercept = 4.73, SE = .141, t = 33.55, p < .0001). The indirect effect of syndemics on condomless sex through self-efficacy was partially supported by the longitudinal modeling (Figure 2). In support of the model, baseline syndemics significantly predicted the baseline (intercept) of self-efficacy (b = −0.49, SE = 0.12, t = −4.02, p < .0001), and the baseline (intercept) of condomless sex (b = 0.32, SE = 0.10, t = 3.13, p = .002). Baseline levels of self-efficacy (the intercept for self-efficacy) significantly predicted the slope of condomless anal sex (b = −0.23, SE = 0.07, t = −3.20, p = .001), with lower self-efficacy predicting increased condomless anal sex. Additionally, the indirect effect of baseline syndemics to the slope of condomless anal sex through the baseline (intercept) levels of self-efficacy was significant (b = 0.11, SE = 0.05, 95% CI: 0.04, 0.18, t = 2.47, p = .014). However, not supporting the model, the change (slope) in self-efficacy did not significantly predict the change (slope) in condomless sex (b = −0.31, SE = 0.41, t = −0.75, p = .46). Additionally, the indirect effect of syndemics to the slope of condomless anal sex through the slope of self-efficacy was not significant (b = −0.04, SE = 0.05, 95% CI: −0.13, 0.06, t = −0.67, p = .50).
Figure 2.
Longitudinal mediational effects of syndemics on condomless anal sex with casual partners through self-efficacy.
Sensitivity analyses with race/ethnicity as covariates were completed and the pattern of results was the same. Additionally, sensitivity analyses with any condomless sex (versus the a-priori variable, condomless sex with casual partners) both with and without race/ethnicity as covariates, also yielded a similar pattern of results.
Discussion
Using cross-sectional data, the findings of this study provide support for condom use self-efficacy as an intermediary variable between syndemics (alcohol use disorder, substance use disorder, sexual compulsivity, depression, social anxiety, intimate partner violence, childhood sexual abuse) and condomless sex using cross-sectional data in MSM with a history of HIV acquisition risk behavior. However, in longitudinal models, the data only partially supported a mediational model. The present study sought to extend the literature on syndemics and HIV risk in men who have sex with men by hypothesizing that the effect of syndemics on HIV risk is not direct. Prior studies of syndemics on risk (e.g., Guadamuz et al., 2014; Mimiaga, Biello, et al., 2015; Mimiaga, O’Cleirigh, et al., 2015; Mustanski et al., 2007; Parsons et al., 2012; Safren et al., 2011; Safren, Reisner, et al., 2010; Stall et al., 2003) have not tested mediators, and many have been cross-sectional in design (e.g., Hirshfield et al., 2015; Mimiaga, Biello, et al., 2015; Mustanski et al., 2007; Parsons et al., 2012; Stall et al., 2003). In the present study, we used a well-studied variable typically associated with health behavior, self-efficacy, as a possible intermediary variable between syndemics and condomless sex with casual partners, both cross-sectionally and via longitudinal modeling, in a high-risk sample of MSM. We found that the cross-sectional analyses supported the indirect effect of syndemics on condomless sex through lowered condom-use self-efficacy. The longitudinal model was partially supported, with syndemics being associated with baseline levels of condomless sex and baseline levels of condom-use self-efficacy, the effect of baseline self-efficacy being associated with change (slope) in condomless sex over three time-points, and the indirect effect of syndemics on change (slope) in condomless sex over time being through its effect on baseline self-efficacy. A fully longitudinal model was not supported because changes in self-efficacy were not associated with changes in condomless sex over time, and, subsequently, the indirect effect of syndemics on changes in self-efficacy was not associated with changes in condomless sex. These results speak to the importance of examining potential psychological variables that are affected by increasing numbers of syndemics that individuals at high risk for HIV may experience, and examining ways in which interventions can directly address the variables proximal to HIV risk within the context of psychosocial problems.
As primary and secondary HIV prevention efforts maintain their focus on treatment as prevention and on pre-exposure prophylaxis the usefulness of the self-efficacy construct will be apparent in a wider range of health behaviors than just condom use. Behavioral and cognitive-behavioral intentions may well benefit by specifying self-efficacy among their treatment targets to increase our ability to impact important health behaviors including medication adherence or engagement in care for HIV prevention or treatment.
There are several possible explanations for the pattern of results obtained in the study. First, it is possible that other mediators exist, particularly for the population of high-risk MSM that were not measured in the present analysis. While low condom-use self-efficacy is a well-studied predictor of condomless sex, other psychological variables associated with condomless sex include low motivation for change, norms about using condoms, attitudes about condoms, and perceptions of the benefits and barriers (e.g. pleasure reduction) of condom use (Mimiaga, Reisner, Reilly, Soroudi, & Safren, 2009; Wulfert, Wan, & Backus, 1996). The results of the present study can be used to potentially inform future research on other possible mediators of the now well-established link between syndemics and HIV related health behaviors. This could be done by conducting similar analyses, but with mediators from other models to determine what specific social psychological variables might be most important either on their own or in combination with self-efficacy in mediating this relationship. It is also possible that sample characteristics contributed to the results in that participants were enrolled due to high levels of HIV risk, and conducting home HIV testing every 2 weeks, potentially affecting the salience of HIV and their behavior, and thus mitigating the true observational nature of the investigation.
Limitations of the present study therefore include the sample and the possible effect of home testing on HIV risk behavior and the psychological and syndemic variables impact on HIV risk behavior. Again, this might affect the salience of HIV risk, and therefore the relationships examined. Additional limitations include the relative homogeneity of the sample and the lack of long-term follow-up assessments. Our assessments were limited to a span of 6 months, and thus it is possible that varied effects could emerge when modeling longer periods of time. Related, with only three time points, non-linear effects of time could not be explored, and with longer periods alternative models could be examined. Additionally, the study was conducted while pre-exposure prophylaxis (PrEP) was becoming more established and, although participants were not taking PrEP, there may be changes in the associations of these variables to HIV risk now defined as condomless sex with potentially HIV positive unsuppressed or unknown status partners when not taking PrEP. There was attrition, particularly from the second to the third assessment point. Despite the analyses using all available data, it is possible that this could affect the outcomes. Finally, future analyses could be aimed at the degree to which different syndemics are more or less predictive of self-efficacy or of, eventually, HIV risk; and should examine how different syndemics themselves might group together.
The present study, however, is the first in its kind in that it not only examined the potential intermediary effects of a psychological variable between syndemics and HIV risk behavior (in this case condomless anal sex with casual partners), but also that it did so in both cross-sectional and longitudinal analyses. It provides initial support for moving beyond examining simple direct effects of psychosocial syndemics on HIV risk to examining these effects via mediating psychological variables. The cross-sectional data supported our hypotheses, and the longitudinal model partially supported our hypothesis. As a first examination of mediators using a syndemic framework, conducting studies like this in different samples, potentially not specifically selected for HIV risk, and examining additional possible mediators, would provide further information about potential modifiable psychological variables that mediate the association of syndemics to HIV risk or, potentially, other negative health related-outcomes.
Acknowledgments
The project described was supported by P01AI074415 (Altfeld), an unrestricted research grant from Alere, Harvard University Center for AIDS Research 5P30AI060354. Some of the author time was supported by 9K24DA040489 (Safren), 7K23MH096647 (Blashill). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health, or any of the other funders.
Footnotes
Disclosures:
Dr. Safren receives royalties for book publications from Oxford University Press, Guilford Publications, and Humana Press (Springer).
References
- Bandura A. Social Cognitive Theory and Exercise of Control over HIV Infection. In: DiClemente RJ, Peterson JL, editors. Preventing AIDS: Theories and Methods of Behavioral Interventions. Boston, MA: Springer US; 1994. pp. 25–59. Retrieved from . [DOI] [Google Scholar]
- Blashill AJ, Bedoya CA, Mayer KH, O’Cleirigh C, Pinkston MM, Remmert JE, … Safren SA. Psychosocial Syndemics are Additively Associated with Worse ART Adherence in HIV-Infected Individuals. AIDS and Behavior. 2015;19(6):981–986. doi: 10.1007/s10461-014-0925-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blashill AJ, Tomassilli J, Biello K, O’Cleirigh C, Safren SA, Mayer KH. Body Dissatisfaction Among Sexual Minority Men: Psychological and Sexual Health Outcomes. Archives of Sexual Behavior. 2016;45(5):1241–1247. doi: 10.1007/s10508-015-0683-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchsbaum D, Buchanan R, Centor R, Schnoll S, Lawton M. Screening for alcohol abuse using cage scores and likelihood ratios. Annals of Internal Medicine. 1991;115(10):774–777. doi: 10.7326/0003-4819-115-10-774. [DOI] [PubMed] [Google Scholar]
- Bush B, Shaw S, Cleary P, Delbanco TL, Aronson MD. Screening for alcohol abuse using the CAGE questionnaire. The American Journal of Medicine. 1987;82(2):231–235. doi: 10.1016/0002-9343(87)90061-1. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Lifetime Risk of HIV Diagnosis by Transmission Group; Presented at the Conference on Retroviruses and Opportunistic Infections; Boston, MA. 2016. Retrieved from http://www.cdc.gov/nchhstp/newsroom/2016/croi-2016.html#Graphics2. [Google Scholar]
- Connor KM, Davidson JRT, Churchill LE, Sherwood A, Weisler RH, Foa E. Psychometric properties of the Social Phobia Inventory (SPIN) The British Journal of Psychiatry. 2000;176(4):379. doi: 10.1192/bjp.176.4.379. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Watson AC. The paradox of self-stigma and mental illness. Clinical Psychology: Science and Practice. 2002;9(1):35–53. [Google Scholar]
- Eisinga R, te Grotenhuis M, Pelzer B. The reliability of a two-item scale: Pearson, Cronbach, or Spearman-Brown? International Journal of Public Health. 2013;58(4):637–642. doi: 10.1007/s00038-012-0416-3. [DOI] [PubMed] [Google Scholar]
- Ewing JA. Detecting alcoholism: The cage questionnaire. JAMA. 1984;252(14):1905–1907. doi: 10.1001/jama.1984.03350140051025. [DOI] [PubMed] [Google Scholar]
- Finkelhor D. Current Information on the Scope and Nature of Child Sexual Abuse. The Future of Children. 1994;4(2):31–53. doi: 10.2307/1602522. [DOI] [PubMed] [Google Scholar]
- Guadamuz TE, McCarthy K, Wimonsate W, Thienkrua W, Varangrat A, Chaikummao S, … van Griensven F. Psychosocial Health Conditions and HIV Prevalence and Incidence in a Cohort of Men Who have Sex with Men in Bangkok, Thailand: Evidence of a Syndemic Effect. AIDS and Behavior. 2014;18(11):2089–2096. doi: 10.1007/s10461-014-0826-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirshfield S, Schrimshaw EW, Stall RD, Margolis AD, Downing MJ, Jr, Chiasson MA. Drug use, sexual risk, and syndemic production among men who have sex with men who engage in group sexual encounters. Journal Information. 2015;105(9) doi: 10.2105/AJPH.2014.302346. Retrieved from https://ajph.aphapublications.org/doi/full/10.2105/AJPH.2014.302346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Johnson JR, Adair V, Rompa D, Multhauf K, Kelly JA. Sexual sensation seeking: Scale development and predicting AIDS-risk behavior among homosexually active men. Journal of Personality Assessment. 1994;62(3):385–397. doi: 10.1207/s15327752jpa6203_1. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Knowlton R, McCusker J, Stoddard A, Zapka J, Mayer K. The use of the CAGE questionnaire in a cohort of homosexually active men. Journal of Studies on Alcohol. 1994;55(6):692–694. doi: 10.15288/jsa.1994.55.692. [DOI] [PubMed] [Google Scholar]
- Koblin B, Chesney M, Coates T the EXPLORE Study Team. Effects of a behavioural intervention to reduce acquisition of HIV infection among men who have sex with men: the EXPLORE randomised controlled study. Lancet. 2004;364:41–50. doi: 10.1016/S0140-6736(04)16588-4. [DOI] [PubMed] [Google Scholar]
- Lenderking WR, Wold C, Mayer KH, Goldstein R, Losina E, Seage GR. Childhood Sexual Abuse Among Homosexual Men. Journal of General Internal Medicine. 1997;12(4):250–253. doi: 10.1046/j.1525-1497.1997.012004250.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayfield D, McLeod G, Hall P. The CAGE questionnaire: validation of a new alcoholism screening instrument. American Journal of Psychiatry. 1974;131(10):1121–1123. doi: 10.1176/ajp.131.10.1121. [DOI] [PubMed] [Google Scholar]
- Millar BM, Starks TJ, Grov C, Parsons JT. Sexual risk-taking in HIV-negative gay and bisexual men increases with depression: Results from a US national study. AIDS and Behavior. 2017;21(6):1665–1675. doi: 10.1007/s10461-016-1507-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mimiaga MJ, Biello KB, Robertson AM, Oldenburg CE, Rosenberger JG, O’Cleirigh C, … Safren SA. High Prevalence of Multiple Syndemic Conditions Associated with Sexual Risk Behavior and HIV Infection Among a Large Sample of Spanish- and Portuguese-Speaking Men Who Have Sex with Men in Latin America. Archives of Sexual Behavior. 2015;44(7):1869–1878. doi: 10.1007/s10508-015-0488-2. [DOI] [PubMed] [Google Scholar]
- Mimiaga MJ, O’Cleirigh C, Biello KB, Robertson AM, Safren SA, Coates TJ, … Mayer KH. The Effect of Psychosocial Syndemic Production on 4-Year HIV Incidence and Risk Behavior in a Large Cohort of Sexually Active Men Who Have Sex With Men. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2015;68(3):329–336. doi: 10.1097/QAI.0000000000000475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mimiaga MJ, Reisner SL, Reilly LC, Soroudi N, Safren SA. Individual interventions. In: Mayer KH, Pizer HF, editors. HIV Prevention: A Comprehensive Approach. Amsterdam, Netherlands: Academic Press; 2009. pp. 203–239. [Google Scholar]
- Mustanski B, Feinstein BA, Madkins K, Sullivan P, Swann G. Prevalence and Risk Factors for Rectal and Urethral Sexually Transmitted Infections From Self-Collected Samples Among Young Men Who Have Sex With Men Participating in the Keep It Up! 2.0 Randomized Controlled Trial. Sexually Transmitted Diseases. 2017;44(8):483–488. doi: 10.1097/OLQ.0000000000000636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Garofalo R, Herrick A, Donenberg G. Psychosocial health problems increase risk for HIV among urban young men who have sex with men: preliminary evidence of a syndemic in need of attention. Annals of Behavioral Medicine. 2007;34(1):37–45. doi: 10.1080/08836610701495268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Grov C, Golub SA. Sexual compulsivity, co-occurring psychosocial health problems, and HIV risk among gay and bisexual men: further evidence of a syndemic. American Journal of Public Health. 2012;102(1):156–162. doi: 10.2105/AJPH.2011.300284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safren SA, Blashill AJ, O’Cleirigh CM. Promoting the Sexual Health of MSM in the Context of Comorbid Mental Health Problems. AIDS and Behavior. 2011;15(S1):30–34. doi: 10.1007/s10461-011-9898-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safren SA, Reisner SL, Herrick A, Mimiaga MJ, Stall R. Mental health and HIV risk in men who have sex with men. Journal of Acquired Immune Deficiency Syndromes. 2010;55(Suppl 2):S74. doi: 10.1097/QAI.0b013e3181fbc939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selig JP, Preacher KJ. Mediation Models for Longitudinal Data in Developmental Research. Research in Human Development. 2009;6(2–3):144–164. doi: 10.1080/15427600902911247. [DOI] [Google Scholar]
- Shadaker S, Magee M, Paz-Bailey G, Hoots BE NHBS Study Group. Characteristics and Risk Behaviors of Men Who Have Sex With Men and Women Compared With Men Who Have Sex With Men—20 US Cities, 2011 and 2014. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2017;75:S281–S287. doi: 10.1097/QAI.0000000000001403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan D, Lecrubier Y. The Mini International Neuropsychiatric Interview Version 6.0 (MINI 6.0) Medical Outcomes System Inc; Jacksonville, FL: 2010. [Google Scholar]
- Singer M. Aids and the health crisis of the U.S. urban poor; the perspective of critical medical anthropology. Social Science & Medicine. 1994;39(7):931–948. doi: 10.1016/0277-9536(94)90205-4. [DOI] [PubMed] [Google Scholar]
- Spitzer R, Kroenke K, Williams J the Patient Health Questionnaire Primary Care Study Group. Validation and utility of a self-report version of prime-md: The phq primary care study. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Stall R, Friedman M, Catania JA. Interacting epidemics and gay men’s health: a theory of syndemic production among urban gay men. In: Wolitski RJ, Stall R, Valdiserri RO, editors. Unequal opportunity: Health disparities affecting gay and bisexual men in the United States. Vol. 1. New York: Oxford University Press; 2008. pp. 251–274. [Google Scholar]
- Stall R, Mills TC, Williamson J, Hart T, Greenwood G, Paul J, … Catania JA. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. American Journal of Public Health. 2003;93(6):939–942. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JK, Wilton L, Magnus M, Wang L, Wang J, Dyer TP, … Cummings V. Relation of Childhood Sexual Abuse, Intimate Partner Violence, and Depression to Risk Factors for HIV Among Black Men Who Have Sex With Men in 6 US Cities. American Journal of Public Health. 2015;105(12):2473–2481. doi: 10.2105/AJPH.2015.302878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wulfert E, Wan CK. Condom Use: A Self-Efficacy Model. Health Psychology. 1993;12(5):346–353. doi: 10.1037//0278-6133.12.5.346. [DOI] [PubMed] [Google Scholar]
- Wulfert E, Wan CK. Safer sex intentions and condom use viewed from a health belief, reasoned action, and social cognitive perspective. Journal of Sex Research. 1995;32(4):299–311. [Google Scholar]
- Wulfert E, Safren SA, Brown I, Wan CK. Cognitive, Behavioral, and Personality Correlates of HIV-Positive Persons’ Unsafe Sexual Behavior1. Journal of Applied Social Psychology. 1999;29(2):223–244. [Google Scholar]
- Wulfert E, Wan CK, Backus CA. Gay men’s safer sex behavior: An integration of three models. Journal of Behavioral Medicine. 1996;19(4):345–349. doi: 10.1007/BF01904761. [DOI] [PubMed] [Google Scholar]