Abstract
Context:
Return-to-sport criteria after anterior cruciate ligament (ACL) injury are often based on “satisfactory” functional and patient-reported outcomes. However, an individual's decision to return to sport is likely multifactorial; psychological and physical readiness to return may not be synonymous.
Objective:
To determine the psychosocial factors that influence the decision to return to sport in athletes 1 year post–ACL reconstruction (ACLR).
Design:
Qualitative study.
Setting:
Academic medical center.
Patients or Other Participants:
Twelve participants (6 males, 6 females) were purposefully chosen from a large cohort. Participants were a minimum of 1-year postsurgery and had been active in competitive athletics preinjury.
Data Collection and Analysis:
Data were collected via semistructured interviews. Qualitative analysis using a descriptive phenomenologic process, horizontalization, was used to derive categories and themes that represented the data. The dynamic-biopsychosocial model was used as a theoretical framework to guide this study.
Results:
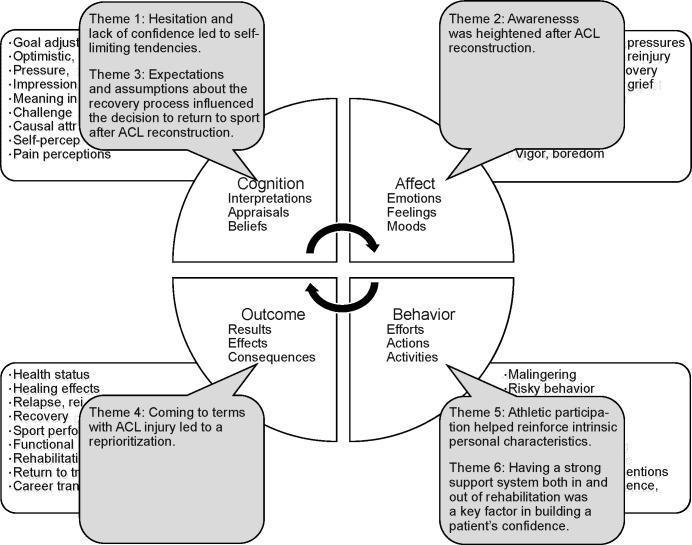
Six predominant themes emerged that described the participants' experiences after ACLR: (1) hesitation and lack of confidence led to self-limiting tendencies, (2) awareness was heightened after ACLR, (3) expectations and assumptions about the recovery process influenced the decision to return to sport after ACLR, (4) coming to terms with ACL injury led to a reprioritization, (5) athletic participation helped reinforce intrinsic personal characteristics, and (6) having a strong support system both in and out of rehabilitation was a key factor in building a patient's confidence. We placed themes into components of the dynamic-biopsychosocial model to better understand how they influenced the return to sport.
Conclusions:
After ACLR, the decision to return to sport was largely influenced by psychosocial factors. Factors including hesitancy, lack of confidence, and fear of reinjury are directly related to knee function and have the potential to be addressed in the rehabilitation setting. Other factors, such as changes in priorities or expectations, may be independent of physical function but remain relevant to the patient-clinician relationship and should be considered during postoperative rehabilitation.
Key Words: psychology, athletes, knee
Key Points
The decision to return to sport after anterior cruciate ligament reconstruction was largely based on psychosocial factors, such as hesitancy, lack of self-confidence, fear of reinjury, and changes in priorities or personal expectations, which may be independent of physical function.
Many of these factors, including hesitancy, lack of confidence, and fear of reinjury, have the potential to be addressed in the rehabilitation setting.
By using a multidisciplinary approach to address both physical and psychosocial factors during the recovery process, clinicians may be able to better assist individuals in their transition back to sport or life after sport.
Anterior cruciate ligament (ACL) injuries are among the most common traumatic ligamentous injuries sustained in an athletic population.1–3 Within the United States alone, more than 250 000 ACL injuries occur annually, and with increased participation in organized athletics, this number is expected to rise.1,4,5 Injury to the ACL occurs via a noncontact or contact mechanism and may result in either complete or partial disruption of the ligament. Often after ACL injury, loss of function at the knee joint is immediate. Surgical intervention is typically recommended for athletes who desire to return to a level of functional activity that involves cutting or pivoting.1,4,6–9
Although ACL reconstruction (ACLR) is considered the most reliable method for regaining full function and returning an athlete to the preinjury activity level, the number of athletes returning to sport participation documented in recent studies has been lower than previously thought. In a systematic review, Ardern et al10 demonstrated that 81% of individuals who underwent ACLR returned to some form of sport after surgery. When the level of sport participation was taken into account, only 65% returned to their preinjury level of sport and 55% returned to competitive sport, despite achieving successful surgical outcomes.9–13 Readiness to return to sport after ACLR is commonly based on a multitude of functional measures, such as strength, power, and proprioception of the involved extremity.4,6 Successful functional outcomes and satisfactory patient-reported outcomes are often the main criteria for clearance in returning an athlete to sport and the preinjury level of activity after ACLR. However, an individual's decision to return to sport is most likely multifactorial and may depend not only on physical factors but on environmental and psychological influences as well. Given the discrepancy between successful functional outcomes and the percentage of athletes who return to sport, it is important to address underlying factors, aside from function, that may contribute to these lower numbers.
Individuals who sustain physical trauma or injury frequently experience psychological responses and effects in addition to functional impairment.14 After injury, the rehabilitation is often focused on treating the physical problem while the psychological aspects are neglected.14–16 It should be noted that physical and psychological readiness might not necessarily be synchronous.16–18 Numerous psychosocial factors unrelated to functional impairment have been identified and may influence a person's decision to return to sport.19 These factors range from a general loss of interest in sport or change in level of play (eg, high school to college) to the fear of reinjuring the involved extremity. Other factors, such as lifestyle changes, occupational demands, and loss of motivation, as well as perceived self-efficacy, may contribute to whether or not individuals return to play at any given level.10,20,21 Little is known, however, about how these factors affect a person's decision or ability to return to sport.
Identifying the psychosocial factors that influence a person's likelihood of returning to sport will allow health care providers to better understand readiness to return to sport from a psychological perspective rather than from just a functional standpoint. This ability to determine readiness to return, in conjunction with knowledge of how to create a positive and successful rehabilitation environment, may help to increase return-to-sport rates while aiding in the transition to life after competitive sport participation in patients who undergo ACLR. Therefore, the purpose of our qualitative study was to examine the various psychosocial factors that influenced the decision to return to sport in athletes a minimum of 1 year after ACLR.
METHODS
In this study, we used the qualitative method of phenomenology because it attempts to describe participants' perceptions and perspectives regarding a phenomenon of interest: in this case, the decision to return to sport after ACLR. This method allows rich information to be gathered via qualitative methods such as semistructured interviews and participants' observations. By examining participants' actions, values, and motivations, phenomenology ultimately aims to reduce individual experiences and perspectives into broad general themes relevant to all participants in the study.22
Recruitment
Participants were recruited from a larger cohort study that evaluated function after ACLR. Participants must have been a minimum of 1 year post–primary ACLR. Inclusion criteria for this study were as follows: (1) age between 12 and 60 years; (2) ACLR a minimum of 1 year before enrollment; (3) willingness to complete a series of hops and functional testing, including isokinetic strength testing, before the interview; and (4) the ability to speak and understand English in order to participate in the interview process. In addition, participants must have had a Tegner Activity Scale score of at least 5, or before undergoing ACLR, have had a self-reported preinjury sports activity level of “well trained, frequently participating in high-level competitive sports.” The Tegner Activity Scale is an 11-item instrument that rates activity level from 0 (sick leave, disability) to 10 (competitive sports). A score of 5 indicates participation in sport-related activities at the lowest recreational level.4 Recruits who participated in the functional testing were asked if they would be willing to be interviewed. We continuously enrolled participants who matched our eligibility requirements into our study until data saturation was achieved. Data saturation occurs when the researcher is no longer hearing or seeing new information.22
Participants
A total of 12 patients (6 males, 6 females; age = 24 ± 8 years, range = 16–44 years) were recruited and agreed to participate in the study. We purposefully selected participants to represent athletes who returned to sport (RTS; n = 6) as well as those who did not return to sport (NRTS; n = 6) after ACLR. For the purposes of this study, return to sport was defined as having returned to at least 1 of the cutting and landing sports the patient was participating in before the ACL injury. If the participant changed to a noncutting sport such as running after injury, he or she was classified in the no-return-to-sport group. The mean time from surgery to the interview session was 4 years (Table 1). All participants had been active in organized athletics before ACLR. We provided both verbal and written information regarding the interview process, and involvement was voluntary. The study was approved by the Institutional Review Board at the University of Kentucky, and informed consent was obtained before data collection. We assured participants of confidentiality, and pseudonyms were used to protect anonymity.
Table 1.
Participant Demographics
| Pseudonym |
Age, y |
Return to Sport? |
Sport Played |
Time From Surgery to Interview, y |
| Betty | 23 | Yes | Volleyball | 9 |
| Brandon | 21 | Yes | Lacrosse | 5 |
| Claire | 27 | No | Gymnastics | 4 |
| Conner | 16 | Yes | Soccer | 1 |
| Elizabeth | 18 | No | Gymnastics | 2 |
| George | 21 | Yes | Baseball | 7 |
| John | 37 | Yes | Soccer | 1 |
| Kelley | 22 | No | Basketball/softball | 4 |
| Mark | 17 | No | Soccer | 2 |
| Mike | 17 | No | Football | 1 |
| Patty | 28 | No | Soccer | 10 |
| Sally | 44 | Yes | Mountain biking/skiing | 4 |
Data Collection
Data were collected via semistructured interviews conducted by the primary author (J.P.B.). The interviewer was a certified athletic trainer who was not involved in the treatment or rehabilitation of the participants. Each interview lasted approximately 25 to 50 minutes and took place in a quiet classroom or conference room. All interviews were recorded and transcribed verbatim by the primary author (J.P.B.). An interview guide was developed (Appendix) and was based on current literature23,24 relating to the psychosocial aspects of returning to sport after serious injury. This semistructured interview guide was used to maintain the consistency of questions asked of all participants during the interview process.
As part of a larger cohort study, patient-reported outcome measures (International Knee Documentation Committee Subjective Knee Form,25 Tegner Activity Scale,26 Marx Activity Scale, and Knee Injury and Osteoarthritis Outcome Score27) were available to the primary author for review before the interview process. Patient-reported outcome measures that demonstrated significant disability or dysfunction were reviewed to further individualize questions during the interview process. All interviews occurred after participants' completion of a functional test battery designed to assess strength, balance, power, and endurance.28
Data Analysis
Data were analyzed using the Colaizzi descriptive phenomenologic method to develop an essential structure of the phenomenon.22 This approach to data analysis was a multistep process that was used to better understand the experiences of participants after ACLR. Each transcribed interview was read several times by the primary investigator to acquire an understanding of the participants' experiences and values and their responses regarding their experience after ACLR. Significant statements that were relevant to the investigated phenomenon of interest were extracted from each transcript and duplications were removed from the analysis (Table 2). Horizontalization was used to help us organize the remaining significant statements. Horizontalization is the process in which statements from interviews are each given an equal weight.22 Formulated meanings were developed for the remaining significant statements and reflected the original statements made by participants.22 The formulated meanings were grouped into a collection of themes, which were then used to provide a full description of the participants' experiences.
Table 2.
Selected Examples of Participants' Important Statements and Corresponding Formulated Meanings
| Important Statement |
Formulated Meaning |
| “I guess when you first go back to it, if you're, if you're still just going to be able to do it. For me, I knew it, physically I could, but could you get past the mental stuff.” | Physical and psychological confidence are not always synonymous after anterior cruciate ligament reconstruction. |
| “You have something to think about before you do physical activity now instead of just going and doing it.” | Sustaining an anterior cruciate ligament injury causes participants to be more aware and conscious of their knee when returning to sport and activity. |
| “I don't know exactly what I did to tear it, that's the thing that [kind of] scares me.” | Participants are scared on first returning to sport after anterior cruciate ligament reconstruction because they are afraid of reinjuring their knee. |
| “I'm not [going to] make a career out of volleyball, and I probably should focus on studies in college, so I ended up playing the rest of my senior year so that I could, so that I wouldn't regret it.” | Often, the decision to return to sport is replaced by other life priorities. |
Rigor
We used several methods to establish credibility and scientific rigor during this investigation. Themes generated from the data analysis were circulated via e-mail to each participant for member checking. The purpose of member checking was to allow each participant the opportunity to read the exhaustive description of themes to ensure that it accurately represented his or her experience. Member checks were used to validate the research findings.29 All participants verified that the generated themes accurately depicted their experiences; no changes or modifications to the themes were suggested. Additionally, throughout the data analysis, a researcher with significant qualitative research experience reviewed and challenged the emerging categories and themes to ensure credibility and to minimize bias in the interpretation of results. Finally, we used phenomenologic bracketing to set aside our own feelings and experiences regarding ACL injury and recovery, which allowed for a better understanding of the participants' experiences.29
RESULTS
A total of 12 participants completed the semistructured interviews. After data analysis, 234 significant statements, 24 formulated meanings, and 6 overarching themes emerged (Table 3). Each theme is defined below (in no particular order) and accompanied by quotations from participants who best represented the data.
Table 3.
Themes and Formulated Meanings Generated From Participants' Interviews
| Theme |
Formulated Meanings |
Important Statements, No. (%) |
| Hesitation and lack of confidence led to self-limiting tendencies. | • Patients experienced hesitation when performing certain activities after ACLR. | 67 (29) |
| • Some patients perceived their knee as unstable when returning to sport or activity. | ||
| • Physical and psychological confidence were not always synonymous after ACLR. | ||
| • Patients relied on a knee brace during activity. | ||
| • To avoid reinjury, patients were self-limiting in the activities in which they participated. | ||
| • Regaining confidence in one's knee after ACLR was an important step toward recovery and return to sport. | ||
| Awareness was heightened after ACLR. | • Patients were scared on first returning to sport after ACLR because they were afraid of reinjuring their knee. | 28 (12) |
| • Many patients disliked the restrictive and cumbersome nature of a knee brace, as well as the attention it brought them. | ||
| • Sustaining an ACL injury caused participants to be more aware and conscious of their knee when returning to sport or activity. | ||
| • Returning to sport after ACLR coincided with anxious feelings in regard to a patient's ability to perform at the same level as before ACL injury. | ||
| Expectations and assumptions about the recovery process influenced the decision to return to sport after ACLR. | • Patients were excited to return to sport after ACLR. | 30 (13) |
| • Limitations in everyday life were frustrating to patients after ACLR. | ||
| • Lengthy rehabilitation programs were frustrating for patients undergoing and recovering from ACLR. | ||
| • Patients often assumed that they would certainly return to sport at either the same or a higher level after ACLR. | ||
| • Expectations regarding outcomes after ACLR dictated a person's decision to return to sport. | ||
| Coming to terms with ACL injury led to a reprioritization. | • The timing of when a patient sustained an ACL injury influenced how he or she coped with and responded to the injury. | 52 (22) |
| • The decision to return to sport was influenced by the quality of life patients desired after ACLR. | ||
| • Often, the decision to return to sport was replaced by other life priorities. | ||
| • Some patients had difficulty discerning whether their decision not to return to sport was based on fear of reinjury or just a loss of interest. | ||
| • Patients who had never experienced a major injury were in shock after ACL injury. | ||
| Athletic participation helped reinforce intrinsic personal characteristics. | • Intrinsic characteristics reinforced through athletic participation influenced the decision to return to sport after ACLR. | 45 (19) |
| • Motivation to return to sport was influenced by a competitive rehabilitation environment and patient self-motivation. | ||
| • Patients who participated in sports their entire lives had a strong sense of athletic identity and connection with their sport. | ||
| • It was beneficial for patients to maintain a healthy lifestyle after ACLR, regardless of their return-to-sport status. | ||
| Having a strong support system both in and out of rehabilitation was a key factor in building a patient's confidence. | • Confidence after ACLR was important in feeling successful and stemmed from external support. | 12 (5) |
Abbreviations: ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction.
Theme 1: Hesitation and Lack of Confidence Led to Self-Limiting Tendencies
Hesitation and lack of confidence with regard to completing a task or sport-related activity was a theme that seemed to influence participants' decisions to return to sport. Regardless of return-to-sport status, those who felt hesitant or lacked confidence in their knee described limiting their involvement in sport or activity. Participants who were self-limiting opted for a lower intensity of play, relied on or were instructed to use a knee brace for support, and were skeptical about performing certain tasks. Some avoided certain activities and sports altogether. In regard to her decision to perform challenging tasks in sport, Sally stated: “Like I said, there's lots of times where I think to myself, ‘I could do that,' and then I think, ‘Do I want to be on crutches for 2 months, not really, no, not going to do that.'” In order to continue participation in sport after ACLR, John thought he would need to decrease his level of intensity: “I guess instead of hanging up the cleats, I hang up the intensity, I just have to go slower.” Interestingly, all individuals seemed to experience the same hesitation and lack of confidence with respect to sport involvement after ACLR, regardless of their return-to-sport status. Each person appeared to weigh the consequences associated with returning to sport or completing a task. Some felt that it was normal to have initial reservations regarding knee function but that their confidence would increase throughout the rehabilitation process. Kelley commented, “I got to where I was doing things without a brace on, I was getting more confident, but there was still some stuff that I was hesitant on.” This theme consisting of hesitation, lack of confidence, and self-limiting tendencies was apparent both in participants who RTS and in those who did not. However, for those who did return, the hesitation and self-limitations were transient, and they eventually became more comfortable and confident in the ability and the strength of their injured knees, as Brandon remarked: “I was like real skeptical about like jumping on it, like real conservative, I didn't want to pivot at first and then like towards the end of physical therapy, I was over that.”
Theme 2: Heightened Awareness After ACLR
Hyperawareness of knee function and the ability to perform competitively in sport after ACLR was another emerging theme. Some participants expressed initial reservations regarding physical activity and the potential consequences of involvement in sport. Others were not as aware of their knee on returning but were more aware of and nervous about their ability to perform the skill set necessary for sport.
Upon return to sport, participants were anxious about performing competitively since being out of competition after ACLR. Patty observed, “Subconsciously, maybe knowing that my skills were rusty, I was like, you know, maybe this isn't worth it.” Whereas some individuals were nervous about their ability to perform after ACLR, George felt that wearing a knee brace caused him to think about the injury more during activity: “When you're wearing a big brace and yeah, it's still fresh in your mind.” In addition to awareness of their injury with brace use, some people who returned felt more aware of their surroundings, and revisiting the location where they tore their ACL brought up intense feelings, as it did for Sally: “I went back there and it smelled the same and it looked the same, I started like, I started having like a little panic attack.”
Participants who NRTS experienced similar emotions as those who did return. Some were conscious of their knee during activity. They felt that they couldn't be active in sport without worrying whether their knee would hold up or if they would injure it again. Mike explained, “You have something to think about before you do physical activity now instead of just going and doing it.” Those who experienced this conscious awareness of their knee withstanding the stresses of sport had a tendency to not return to participation. Others, rather than being cautious of their knee, were self-conscious about wearing a brace during play. Patty stated, “I wore a brace, but even then, I didn't want to wear a brace, so I was hesitant about that. I felt like it made me stand out more and people are brutal when you're playing against them, they'll go for the injured part.” Regardless of whether a participant RTS, all experienced some level of heightened awareness after ACLR. Certain athletes were cognizant of their ability to perform competitively at the same preinjury level, whereas others were mindful of whether or not their physical knee function was reliable. Feelings of self-consciousness while wearing a brace and anxiety upon returning to the location of injury also seemed to affect a person's decision. Overall, both physical and psychological forms of hyperawareness were experienced and described by participants after ACLR.
Theme 3: Expectations and Assumptions About the Recovery Process Influenced the Decision to Return to Sport After ACLR
After ACL injury, participants expressed expectations regarding the next step in the recovery process. Some were uncertain of what the recovery and rehabilitation process entailed and so their assumptions of what would happen were not clear. John, who had previously been exposed to ACL injury and the recovery process, stated that he had set low expectations of what he hoped to accomplish after injury based on someone else's experience with ACLR. Each participant, depending on his or her outlook on injury and loss, had different assumptions regarding the ability to return to sport after ACLR. Some had no doubt in their minds that after their reconstruction, they would return to sport. Kelley commented, “I didn't want sports to end just like that, so I knew I was going to play either in college or I was going to finish off in high school.” In addition to returning to sport, all assumed that they would return to sport at the same level as before the injury. Brandon confirmed, “I definitely wasn't going lower, I did want to go higher as far as college, but I wasn't stepping down to like a lower level.” Other individuals lacked confidence in their ability to return to sport after the ACL injury. “My second feeling was there goes my soccer ever again, and I told the doctor that, well, that's probably it, I have to hang up the cleats because you know, I'm growing older,” John remarked. Even though they expected before surgery to return to some level of sport, other athletes ended up refocusing their goals during the recovery process. Mark said, “I probably would have returned to a high level. I would have continued high-level soccer if I hadn't injured it, but the injury kind of made me refocus my goals.” It was clear that expectations after ACLR often changed in the course of recovery. Some participants had set expectations of ultimately returning to sport after ACLR, whereas others initially had expectations of never resuming sport participation that changed when they returned to some level of activity.
Theme 4: Coming to Terms With ACL Injury Led to a Reprioritization
Changes in life priorities and career paths and an emphasis on education influenced the participants' decisions to return to sport after ACLR. Five of the 6 who chose to not return to sport did so because of some other life event or higher priority. These priorities ranged from career requirements to focusing on education and spending time with family. Others who RTS initially ended up leaving their sport for reasons such as graduation from high school or college, loss of interest, or lack of time. Those who initially returned to play after ACLR but left the sport upon graduation from high school were not upset about the decision. “I also just didn't have the talent level to play volleyball at a big Division I school, um, so that was just something that I sort of already coped with and my knee didn't really play any type of factor in that,” noted Betty. Among the participants who did not return, many cited the need to focus on studies in college to prepare for their careers: Kelley explained, “I'm not [going to] make a career out of volleyball, and I probably should focus on studies in college, so I ended up playing the rest of my senior year so that I could, so that I wouldn't regret it.” Other individuals felt they would not be able to juggle academics and athletics: “It was kinda a hard decision but not just 'cause of my knee, again it was 'cause of my schedule, so it's more of would I have time to really do this kinda thing,” Mark said. Priorities in life were a large contributor to the decision to return to sport after ACLR. Although certain people felt their priority after ACLR was to resume some level of physical activity in order to promote fitness and quality of life, most expressed the desire to focus on their education, career, or family.
Theme 5: Athletic Participation Helped Reinforce Intrinsic Personal Characteristics
A sense of athletic identity, competitive personality, and self-motivation were all factors that motivated participants through the rehabilitation and recovery process after ACLR. Many felt that their sport made them who they were, and not being able to play because of injury was a motivator to return to sport. Betty observed, “Like volleyball has always been a part of who I am, and so why would you not get back to that or find a way to keep that going for as long as you can?” Having a strong sense of athletic identity after ACLR was important for individuals who desired to return to sport because it helped them stay motivated throughout the long recovery process: “I've been playing soccer since I was 5, every year for spring, summer, and fall, so, you know, just kinda something I've been doing my whole life,” Conner described. Those who did not return to competitive sport, including Elizabeth, felt a loss of athletic identity: “I miss the sport, I miss being able to do it.” In addition to their strong sense of athletic identity, participants felt they thrived in a competitive rehabilitation environment. Even for those who NRTS, being challenged daily in rehabilitation was exciting and kept them on track with their recovery goals: “I think it helped me push myself more and be able to kind of gauge where my rehab was going, especially with him [friend] beside me,” Kelley expressed. Intrinsically motivated people were determined to push themselves throughout the rehabilitation process without external influences. This theme was particularly pronounced in those individuals who successfully RTS. They depicted a competitive nature and a positive relationship with physical activity as helping to facilitate improved rehabilitation outcomes and ultimately to ensure a good quality of life after reconstruction.
Theme 6: Having a Strong Support System Both In and Out of Rehabilitation was a Key Factor in Building a Patient's Confidence
Encouragement and external support systems were important in facilitating a positive recovery environment and making participants feel more confident in their steps toward returning to sport. Both those who returned and those who NRTS after their ACLR stated that having, or wishing they had, a good support system was helpful in instilling confidence and a positive outlook on injury. Elizabeth highlighted the importance of having a support system as a source of empathy during the recovery process: “My teammates and my former coaches and my family were all very supportive and they encouraged me to try and get back as much as I could.” Being able to relate to others who had undergone similar injuries helped participants cope with and overcome hardships, as Claire shared: “You see a lot of people who have like similar injuries and stuff so it made me more relatable.” Several participants felt that aside from a strong support system outside of rehabilitation, creating a good rapport with their physical therapist or athletic trainer was paramount in their recovery: “If you don't have a relationship with them, I don't think you'd actually put in the work, and they wouldn't put in the work with you,” Mike remarked. Those individuals who NRTS agreed that having a support system both before and after surgery was comforting. As Patty stated, “Not to have your family and support system there when something like that happens can be even more emotional than the situation already is.” All but 1 participant felt that they had great support systems after ACLR. However, this person felt abandoned by her coach after her injury and initially resented the apathy she perceived as coming from her coaching staff. In conclusion, both those who returned and those who NRTS after reconstruction described support systems as important for their recovery.
DISCUSSION
The purpose of our study was to examine various psychosocial factors that influenced the decision to return to sport in athletes a minimum of 1 year post-ACLR. We identified 6 overarching themes that influenced participants' decisions to return to sport: (1) hesitation and lack of confidence led to self-limiting tendencies, (2) heightened awareness after ACLR, (3) expectations and assumptions about the recovery process influenced the decision to return to sport after ACLR, (4) coming to terms with ACL injury led to a reprioritization, (5) athletic participation helped reinforce intrinsic personal characteristics, and (6) having a strong support system both in and out of rehabilitation was a key factor in building a patient's confidence.
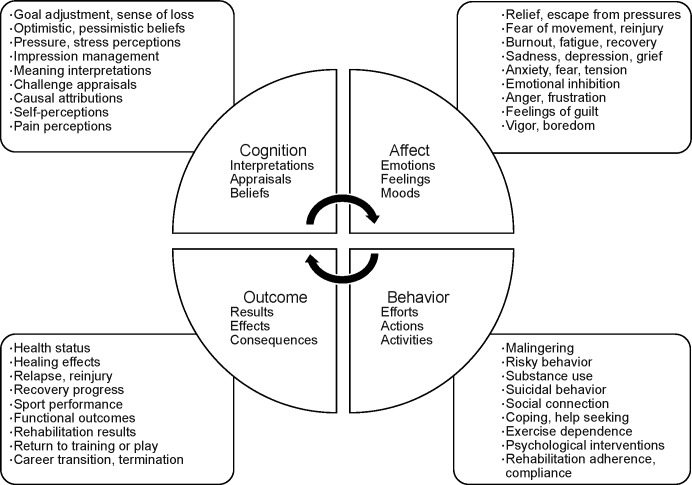
Psychological factors relative to injury, although complicated, are prominent components of the rehabilitation process.13,30–33 These factors are thought to influence the outcome of rehabilitation after injury.30,34,35 Although psychological readiness to return to sport has been identified as a possible hindrance in returning to sport after injury,4,14,15 few qualitative researchers have assessed the underlying psychological factors that may affect those considering a return to sport after ACLR. We aimed to explore the psychosocial factors that are often not considered possible hindrances or barriers to returning to sport. Throughout the literature, numerous psychological models have been identified and associated with the process of coping after injury.13,17,35 We compared our findings from this investigation with the dynamic biopsychosocial model (Figures 1 and 2).35 The dynamic biopsychosocial model encompasses 4 main components (cognition, affect, behavior, and outcome) that are interrelated, modifiable, and dynamic in regard to a patient's response to injury and recovery process postinjury.33
Figure 1.
The dynamic biopsychosocial model as developed by Wiese-Bjornstal et al.35 Weise-Bjornstal DM, Smith AM, Shaffer SM, Morrey MA. An integrated model of response to sport injury: psychological and sociological dynamics. J Appl Sport Psychol. 1998;10(1):46–69. Copyright © the Association for Applied Sport Psychology, www.appliedsportpsych.org, adapted by permission of Taylor & Francis Ltd, http://www.tandfonline.com on behalf of the Association for Applied Sport Psychology.
Figure 2.
Dynamic biopsychosocial model and corresponding themes, based on the biopsychosocial model developed by Wiese-Bjornstal et al.35 Abbreviation: ACL, anterior cruciate ligament. Weise-Bjornstal DM, Smith AM, Shaffer SM, Morrey MA. An integrated model of response to sport injury: psychological and sociological dynamics. J Appl Sport Psychol. 1998;10(1):46–69. Copyright © the Association for Applied Sport Psychology, www.appliedsportpsych.org, adapted by permission of Taylor & Francis Ltd, http://www.tandfonline.com on behalf of the Association for Applied Sport Psychology.
The term cognition focuses on the conscious appraisals and thoughts that athletes have after injury.13,33 Our study identified several themes related to cognition that contributed to the participants' decisions to return to sport. These included hesitation and lack of confidence, expectations and assumptions during the recovery process, and self-efficacy. An individual's expectations and assumptions regarding ACL injury and the rehabilitation process may influence the decision to return to sport. Participants in our study conveyed that their initial expectations regarding the ACLR process were skewed, and many expressed intense feelings of unpreparedness postreconstruction. Over the course of the rehabilitation process, their expectations regarding recovery and return to sport were modified based on how they felt about their progress. Because these expectations changed throughout recovery, they played a role in the decision-making process. In a similar qualitative study,15 unrealistic expectations regarding the content and time frame of the rehabilitation process were evident among individuals recovering from ACLR. They felt they were not mentally prepared for the rehabilitation process after surgery.15 Few athletes mentally prepare themselves for injury and, therefore, they may lack the necessary psychological intervention strategies to cope with injury. Subsequently, a lack of preparation may lead to depressed mood states and decreases in self-perception and confidence. Individuals who have unrealistic expectations of their recovery process may experience decreased levels of confidence and self-efficacy in regard to their ability to return to sport.36 Participants in our study expressed having either high or low expectations of the recovery process and their ability to return to sport after injury. These expectations were often based on the perceptions and experiences of other individuals who had sustained ACL injuries and were not always realistic, which led to disappointment and decreased confidence in their ability to return to sport.
Self-efficacy can be described as an individual's judgment of his or her ability to carry out a task, regardless of whether the person can or does complete it.13,31,33,37–39 People with higher self-efficacy levels have more positive outcomes after rehabilitation because they have confidence in their ability to complete the tasks that are presented to them; this may, in turn, facilitate greater adherence to rehabilitation.13,38,39 Rehabilitation programs that incorporate techniques such as positive self-talk and goal setting have been associated with increased adherence to home rehabilitation and greater perceived effort.40 Previous researchers40 showed that patients with greater perceived self-efficacy had improved return-to-sport rates at 12 months after ACLR; therefore, it is important to identify those participants who may have lower levels of self-efficacy. Although we did not measure it in our study, self-efficacy can be measured subjectively using validated scales such as the Knee Self-Efficacy Scale (K-SES).41
Not surprisingly, feelings of hesitation and decreased levels of confidence after ACLR were apparent among the participants in our study. Regardless of whether participants RTS, they acknowledged feelings of hesitation that led to a pattern of self-limitation in everyday life and activity, either restricting the intensity of sport or choosing an activity that required less skill. Those who exhibited self-limiting tendencies demonstrated characteristics similar to individuals in previously published literature42 who were known to have lower levels of self-efficacy. Thomeé et al41,42 examined determinants of self-efficacy in patients after ACL injury and described individuals with high and low levels of self-efficacy based on the K-SES subjective outcome score.41 Our findings of hesitation and decreased confidence are consistent with the concept of low self-efficacy and may be a topic of interest for future researchers. Knowing a patient's self-efficacy level can allow for appropriate interventions to be implemented during the recovery process. Cognition-related themes (which included hesitancy, lack of confidence, and expectations of recovery) identified in this study demonstrate the importance of addressing self-efficacy throughout the rehabilitation process.
The second tier of the dynamic biopsychosocial model encompasses affective responses and is made up mainly of emotions, feelings, and moods. For many athletes, fear of reinjury is one of the primary emotional factors in not returning to sport,14,16,31,43 and fear of reinjury was a common theme in our interviews. However, this fear was secondary to the more common theme of hyperawareness that emerged from our participants. Kinesiophobia (the heighted fear of movement and subsequent reinjury),44 as well as increased awareness of the knee joint, is frequent after ACLR and is associated with lower levels of self-reported knee function and lower rates of return to sport.32,45 Participants in this study demonstrated increased physical and mental awareness regarding their knees during activity. Awareness of the knee after ACLR encompassed participants' fear of reinjury and associated knee discomfort or perceived changes in functional performance. Additionally, participants acknowledged that other aspects representing awareness affected the process of returning to sport. For example, some viewed wearing a brace as a physical reminder of their injury, and others reported emotional and physical responses to returning to the place of injury. Interestingly, although some participants expressed fear of reinjury as a contributor to not returning to sport, hyperawareness of the knee was more limiting than the actual fear of reinjury. They may have been fearful of reinjury on initial return to sport; however, this feeling was transient compared with a prolonged sense of heightened awareness of their knee during activity and daily life. This increased awareness both physically and psychologically affected how returners and nonreturners weighed the options regarding return to sport. This demonstrates the need for further interventions throughout the rehabilitation process, to assess and address the affective responses of the biopsychosocial model. Acknowledging these affective responses may help patients make informed and conscientious decisions regarding whether or not to return to play after ACLR.
Behavior, which is greatly influenced by both cognitive and affective responses, is the third component of the biopsychosocial model and incorporates an individual's actions, efforts, and activities after an injury.35 Because of the extensive rehabilitation period after ACLR, rehabilitation adherence is a crucial part of the recovery process and is often influenced by numerous factors, including intrinsic motivation. Intrinsic motivation can be described as “the natural tendency to seek out challenges with the intent of further development/enhancement and mastery of skills.”46 Individuals who have high levels of intrinsic motivation are thought to exhibit more autonomy and self-determination and tend to have better return-to-sport outcomes.18,23 As described by theme 5, participants in our study displayed characteristics of intrinsic motivation toward their recovery and were dedicated to the rehabilitation process. They also demonstrated a competitive nature that drove them to improve and exhibited a willingness to succeed without external influence or encouragement. Although this finding was not quantified in our research, Eastlack et al47 demonstrated that individuals with high levels of intrinsic motivation were more likely to return to sport after ACLR compared with individuals lacking intrinsic motivation. Among our participants, it may be that those who NRTS, even though they demonstrated characteristics of intrinsic motivation, were motivated to achieve a successful rehabilitation outcome but did not have enough incentive or desire to return fully to sport.
Secondary to intrinsic motivation, individuals who had strong support systems seemed to have positive rehabilitation experiences and better return-to-sport outcomes.48 Our participants described their need for some type of social support throughout the recovery process as an important factor in increasing their confidence. The majority felt they had a good support system after injury and during their recovery process. Similarly, Johnston and Carroll48 highlighted the importance of social support systems at different times in the rehabilitation process and described social supports as multidimensional and dynamic. Social support systems, among other coping strategies described by Carson and Polman,24 were used throughout the rehabilitation process to facilitate the development of confidence in rugby athletes after ACLR. Although it is important for instilling confidence after ACLR, social support did not seem to be a factor in whether our participants RTS. Those who returned versus those who did not expressed similar thoughts regarding the importance of a support system and felt their support systems helped them cope with the recovery process. Only 1 person stated she felt that a lack of support from her coach inhibited her ability to return to sport after reconstruction, but her decision was not based solely on that factor.
Outcome, an amalgamation of the 3 previously depicted modifiable components, encompasses smaller components such as functional measures, rehabilitation results, and career transitions or terminations, which together make up the entirety of what it means to return.13 Acknowledgment of the numerous factors that act as facilitators of and barriers to return to sport is essential when providing care to individuals after ACLR. Each patient may have different expectations and life aspirations after surgery, which may or may not include returning to competitive sport. A change in life priorities has been identified as one of the most overlooked reasons why patients do not return to sport after ACLR.49 All of our participants who NRTS after reconstruction indicated that their reason for not returning was a career, education (transitional periods), or family. Those individuals who desired to maintain a healthy lifestyle described the necessity of athletics in their life, not only for the health benefits but also because being athletes was part of who they were. Regardless of an apparent connection with their sport and a sense of athletic identity, a reevaluation of life priorities after ACLR greatly contributed to our participants' decisions to return to sport.
As depicted in the dynamic biopsychosocial model, it is apparent that both the physical and psychosocial aspects of rehabilitation are fundamental components for a successful return to sport after ACLR. It is important to note that not only are physical outcomes modifiable through rehabilitation, but psychological responses to injury are also modifiable and can be influenced throughout the rehabilitation process. Many functional and objective tools are available for clinicians to use on a daily basis after ACLR to better understand the patient's functional ability. However, only a few authors49–51 have examined the relationship between psychological aspects and return to sport after ACLR.4 Having a clearer understanding of an individual's intent and psychological readiness to return to sport can highlight potential barriers that need to be addressed during the recovery process. The implementation of psychological assessment scales such as the Anterior Cruciate Ligament Return to Sport After Injury scale52 and the K-SES39 may be useful in evaluating psychological barriers to ACLR rehabilitation.
Once these barriers are identified, appropriate intervention strategies may be used to facilitate improvements. Psychological interventions such as goal setting, imagery, and positive self-talk can positively influence rehabilitation outcomes after sports injuries.53 Recognizing and evaluating the psychosocial barriers that may influence an individual's rehabilitation outcome or decision to return to sport may help the patient address these barriers and achieve treatment goals.
CLINICAL IMPLICATIONS
The success of a rehabilitation program is often determined by whether an athlete returns to sport or to his or her preinjury level of activity.6,13,53 Although return to sport is often reported as the ideal outcome after ACLR, it is important to consult with patients to learn what they wish to accomplish. Understanding the numerous psychosocial factors that frequently influence an individual's decision to return to sport, as demonstrated by our 6 overarching themes, may help clinicians recognize areas in which individuals may struggle after ACLR. Although our themes identify meaningful areas that should be recognized during the rehabilitation and recovery process, these themes do not necessarily apply to every individual. Our 6 themes should be considered a guideline as to the psychosocial factors that can affect an individual's decision to return to sport and may help clinicians preemptively address any concerns that arise during the recovery process. Having a general idea of which factors may influence the decision to return to sport can help clinicians reassure patients that their responses, thoughts, and emotions after ACLR are normal. Additionally, identifying and allowing individuals to verbalize their expectations and goals before surgery as well as at the beginning of and throughout the rehabilitation process may prove helpful in avoiding loss of confidence and unrealistic expectations. Overall, using a multidisciplinary approach to rehabilitation and recovery is an important component in facilitating a positive (that is, what an individual deems as positive) outcome after ACLR. Being able to address the psychosocial factors that may affect an individual after ACL injury and ACLR may smooth the transition back to sport or life after participation in sports.
LIMITATIONS
This study had several limitations. The participants were purposefully selected and had been previously enrolled in a larger cohort study, which quantitatively evaluated functional measures of the knee after ACLR.28 To be involved in the larger cohort study, participants had to be willing to jump, skip, hop, and partake in an isokinetic strength test. This willingness to participate in some physical activity may have biased our sample to disproportionately include high-functioning individuals and exclude lower-functioning individuals with a history of ACLR. An additional limitation of this study was that the participants were an average of 4 years postsurgery, which may have affected their ability to generate responses to questions regarding emotions and thoughts after injury or throughout rehabilitation. Although this recall bias is a possible limitation of our study, it is also a strength, because participants who were further out from surgery had the ability to fully process and reflect on their experience after ACL injury.
CONCLUSIONS
After ACLR, the decision to return to sport was largely influenced by psychosocial factors. We identified 6 major themes that commonly affected individuals after ACL injury and reconstruction. Some factors, including hesitancy, lack of confidence, and fear of reinjury, were directly related to knee function and have the potential to be addressed in the rehabilitation setting. Other factors, such as changes in priorities or expectations, may be independent of physical function but remain relevant to the patient-clinician relationship and should be considered during postoperative rehabilitation. The findings of this qualitative study highlight important areas that need to be acknowledged and taken into consideration when mapping an individual's rehabilitation program after ACLR. Additionally, using quantitative psychosocial outcome measures, such as the Anterior Cruciate Ligament Return to Sport After Injury Scale and promoting psychological interventions will allow clinicians to create a rehabilitation environment in which patients can thrive. By addressing both physical and psychosocial factors during the recovery process, clinicians may be able to better assist individuals in their transition back to sport or to life after sport.
ACKNOWLEDGMENTS
The study was supported by the National Athletic Trainers' Association District 2 Research Endowment.
Appendix.
Interview Guidea Continued on Next Page
| Date: | Time of Interview: |
| Place: | |
| Interviewer: | |
| Subject ID: | |
| Procedures: | |
| • Set up room and ensure privacy of location. | • Review purpose of the study. |
| • Review and sign informed consent (if not previously completed). | |
| • Test, position, and turn on tape recorder. | • Ask them for alternate name. |
| Interview: | |
| 1. Tell me about your knee injury… | |
| a. How did the injury occur? | |
| b. When did the injury occur? | |
| c. What made you seek medical treatment? | |
| 2. Describe your thoughts and emotions regarding your injury. | |
| 3. Describe for me the kind of feedback and/or encouragement you've had from people in your life regarding your recovery progress up to this point? | |
| a. Did/do you have a good support system while undergoing rehabilitation? | |
| 4. How is it decided that you were ready to make your return to competition? Has anyone influenced you in making this decision? | |
| a. How? Explain… | |
| 5. Describe your thoughts and emotions regarding return to sport | |
| a. If you have not returned, why haven't you? Please elaborate. | |
| 6. What were your expectations regarding your goals/outcomes following ACLR? | |
| a. Return to competition at a higher level, same level, lower level, not at all | |
| i. Explain your reasoning and decisions. | |
| 7. Did you utilize any strategies to help you overcome any fear you may have had during rehabilitation or upon return to play? | |
| 8. Did you have confidence in your ability to pick up where you left off/return to the level of play you once were at? | |
| 9. Is there anything that worries or worried you regarding your return to play? | |
| 10. Do you have physical confidence in your knee? | |
| 11. Is there anything else you would like to share with us about your injury and rehabilitation experience? | |
• Note: Since this will be a semistructured interview, there may be additional questions that arise resulting from responses given by participant.
Abbreviations: ACLR, anterior cruciate ligament reconstruction; ID, identification.
Guide is presented in its original form.
REFERENCES
- 1.Beynnon BD, Johnson RJ, Abate JA, Fleming BC, Nichols CE. Treatment of anterior cruciate ligament injuries, part I. Am J Sports Med. 2005;33(10):1579–1602. doi: 10.1177/0363546505279913. [DOI] [PubMed] [Google Scholar]
- 2.Dragoo JL, Braun HJ, Durham JL, Chen MR, Harris AH. Incidence and risk factors for injuries to the anterior cruciate ligament in National Collegiate Athletic Association football: data from the 2004–2005 through 2008–2009 National Collegiate Athletic Association Injury Surveillance System. Am J Sports Med. 2012;40(5):990–995. doi: 10.1177/0363546512442336. [DOI] [PubMed] [Google Scholar]
- 3.McCullough KA, Phelps KD, Spindler KP, Matava MJ, Dunn WR, Parker RD. Return to high school- and college-level football after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) cohort study. Am J Sports Med. 2012;40(11):2523–2529. doi: 10.1177/0363546512456836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lentz TA, Zeppieri G, Jr, Tillman SM, et al. Return to preinjury sports participation following anterior cruciate ligament reconstruction: contributions of demographic, knee impairment, and self-report measures. J Orthop Sports Phys Ther. 2012;42(11):893–901. doi: 10.2519/jospt.2012.4077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sanders TL, Maradit Kremers H, Bryan AJ, et al. Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med. 2016;44(6):1502–1507. doi: 10.1177/0363546516629944. [DOI] [PubMed] [Google Scholar]
- 6.Ardern CL, Webster KE, Taylor NF, Feller JA. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery: two-thirds of patients have not returned by 12 months after surgery. Am J Sports Med. 2011;39(3):538–543. doi: 10.1177/0363546510384798. [DOI] [PubMed] [Google Scholar]
- 7.Lyman S, Koulouvaris P, Sherman S, Do H, Mandl LA, Marx RG. Epidemiology of anterior cruciate ligament reconstruction: trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am. 2009;91(10):2321–2328. doi: 10.2106/JBJS.H.00539. [DOI] [PubMed] [Google Scholar]
- 8.Spindler KP, Wright RW. Clinical practice. Anterior cruciate ligament tear. N Engl J Med. 2008;359(20):2135–2142. doi: 10.1056/NEJMcp0804745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tripp DA, Stanish W, Ebel-Lam A, Brewer BW, Birchard J. Fear of reinjury, negative affect, and catastrophizing predicting return to sport in recreational athletes with anterior cruciate ligament injuries at 1 year postsurgery. Rehabil Psychol. 2007;52(1):74–81. [Google Scholar]
- 10.Ardern CL, Taylor NF, Feller JA, Webster KE. Return-to-sport outcomes at 2 to 7 years after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2012;40(1):41–48. doi: 10.1177/0363546511422999. [DOI] [PubMed] [Google Scholar]
- 11.Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48(21):1543–1552. doi: 10.1136/bjsports-2013-093398. [DOI] [PubMed] [Google Scholar]
- 12.Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. Sports participation 2 years after anterior cruciate ligament reconstruction in athletes who had not returned to sport at 1 year: a prospective follow-up of physical function and psychological factors in 122 athletes. Am J Sports Med. 2015;43(4):848–856. doi: 10.1177/0363546514563282. [DOI] [PubMed] [Google Scholar]
- 13.te Wierike SC, van der Sluis A, van den Akker-Scheek I, Elferink-Gemser MT, Visscher C. Psychosocial factors influencing the recovery of athletes with anterior cruciate ligament injury: a systematic review. Scand J Med Sci Sports. 2013;23(5):527–540. doi: 10.1111/sms.12010. [DOI] [PubMed] [Google Scholar]
- 14.Kvist J, Ek A, Sporrstedt K, Good L. Fear of re-injury: a hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2005;13(5):393–397. doi: 10.1007/s00167-004-0591-8. [DOI] [PubMed] [Google Scholar]
- 15.Heijne A, Axelsson K, Werner S, Biguet G. Rehabilitation and recovery after anterior cruciate ligament reconstruction: patients' experiences. Scand J Med Sci Sports. 2008;18(3):325–335. doi: 10.1111/j.1600-0838.2007.00700.x. [DOI] [PubMed] [Google Scholar]
- 16.Langford JL, Webster KE, Feller JA. A prospective longitudinal study to assess psychological changes following anterior cruciate ligament reconstruction surgery. Br J Sports Med. 2009;43(5):377–381. doi: 10.1136/bjsm.2007.044818. [DOI] [PubMed] [Google Scholar]
- 17.Podlog L, Eklund RC. The psychosocial aspects of a return to sport following serious injury: a review of the literature from a self-determination perspective. Psychol Sport Exerc. 2007;8(4):535–566. [Google Scholar]
- 18.Podlog L, Eklund RC. Returning to competition after a serious injury: the role of self-determination. J Sports Sci. 2010;28(8):819–831. doi: 10.1080/02640411003792729. [DOI] [PubMed] [Google Scholar]
- 19.Smith FW, Rosenlund EA, Aune AK, MacLean JA, Hillis SW. Subjective functional assessments and the return to competitive sport after anterior cruciate ligament reconstruction. Br J Sports Med. 2004;38(3):279–284. doi: 10.1136/bjsm.2002.001982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dunn WR, Spindler KP. Predictors of activity level 2 years after anterior cruciate ligament reconstruction (ACLR): a Multicenter Orthopaedic Outcomes Network (MOON) ACLR cohort study. Am J Sports Med. 2010;38(10):2040–2050. doi: 10.1177/0363546510370280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Feller J, Webster KE. Return to sport following anterior cruciate ligament reconstruction. Int Orthop. 2013;37(2):285–290. doi: 10.1007/s00264-012-1690-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Creswell JW. Qualitative Inquiry & Research Design: Choosing Among Five Approaches 2nd ed. Thousand Oaks, CA: SAGE Publications;; 2007. [Google Scholar]
- 23.Podlog L, Eklund RC. A longitudinal investigation of competitive athletes' return to sport following serious injury. J Appl Sport Psychol. 2006;18(1):44–68. [Google Scholar]
- 24.Carson F, Polman R. Experiences of professional rugby union players returning to competition following anterior cruciate ligament reconstruction. Phys Ther Sport. 2012;13(1):35–40. doi: 10.1016/j.ptsp.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 25.Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS) Arthritis Care Res (Hoboken) 2011;63(suppl 11):S208–S228. doi: 10.1002/acr.20632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29(2):213–218. doi: 10.1177/03635465010290021601. [DOI] [PubMed] [Google Scholar]
- 27.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee injury and osteoarthritis outcome score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- 28.Werner JL, Burland JP, Mattacola CG, Toonstra J, English RA, Howard JS Decision to return to sport participation after anterior cruciate ligament reconstruction, part II: self-reported and functional performance outcomes. J Athl Train. 2018;53(5):464–474. doi: 10.4085/1062-6050-328-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Petty NJ, Thomson OP, Stew G. Ready for a paradigm shift? Part 2: introducing qualitative research methodologies and methods. Man Ther. 2012;17(5):378–384. doi: 10.1016/j.math.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 30.Brewer BW, Van Raalte JL, Cornelius AE, et al. Psychological factors, rehabilitation adherence, and rehabilitation outcome after anterior cruciate ligament reconstruction. Rehabil Psychol. 2000;45(1):20–37. doi: 10.1037/a0031297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chmielewski TL, Zeppieri G, Jr, Lentz TA, et al. Longitudinal changes in psychosocial factors and their association with knee pain and function after anterior cruciate ligament reconstruction. Phys Ther. 2011;91(9):1355–1366. doi: 10.2522/ptj.20100277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Christino MA, Fantry AJ, Vopat BG. Psychological aspects of recovery following anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2015;23(8):501–509. doi: 10.5435/JAAOS-D-14-00173. [DOI] [PubMed] [Google Scholar]
- 33.Wiese-Bjornstal DM. Psychology and socioculture affect injury risk, response, and recovery in high-intensity athletes: a consensus statement. Scand J Med Sci Sports. 2010;20(suppl 2):103–111. doi: 10.1111/j.1600-0838.2010.01195.x. [DOI] [PubMed] [Google Scholar]
- 34.Podlog L, Eklund RC. Return to sport after serious injury: a retrospective examination of motivation and psychological outcomes. J Sport Rehabil. 2005;14(1):20–34. [Google Scholar]
- 35.Wiese-Bjornstal DM, Smith AM, Shaffer SM, Morrey MA. An integrated model of response to sport injury: psychological and sociological dynamics. J Appl Sport Psychol. 1998;10(1):46–69. [Google Scholar]
- 36.Podlog L, Eklund RC. High-level athletes' perceptions of success in returning to sport following injury. Psychol Sport Exerc. 2009;10(5):535–544. [Google Scholar]
- 37.Brand E, Nyland J. Patient outcomes following anterior cruciate ligament reconstruction: the influence of psychological factors. Orthopedics. 2009;32(5):335. doi: 10.3928/01477447-20090502-01. [DOI] [PubMed] [Google Scholar]
- 38.Thomeé P, Währborg P, Börjesson M, Thomeé R, Eriksson BI, Karlsson J. Self-efficacy, symptoms and physical activity in patients with an anterior cruciate ligament injury: a prospective study. Scand J Med Sci Sports. 2007;17(3):238–245. doi: 10.1111/j.1600-0838.2006.00557.x. [DOI] [PubMed] [Google Scholar]
- 39.Thomeé P, Währborg P, Börjesson M, Thomeé R, Eriksson BI, Karlsson J. Self-efficacy of knee function as a pre-operative predictor of outcome 1 year after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2008;16(2):118–127. doi: 10.1007/s00167-007-0433-6. [DOI] [PubMed] [Google Scholar]
- 40.Everhart JS, Best TM, Flanigan DC. Psychological predictors of anterior cruciate ligament reconstruction outcomes: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23(3):752–762. doi: 10.1007/s00167-013-2699-1. [DOI] [PubMed] [Google Scholar]
- 41.Thomeé P, Währborg P, Börjesson M, Thomeé R, Eriksson BI, Karlsson J. A new instrument for measuring self-efficacy in patients with an anterior cruciate ligament injury. Scand J Med Sci Sports. 2006;16(3):181–187. doi: 10.1111/j.1600-0838.2005.00472.x. [DOI] [PubMed] [Google Scholar]
- 42.Thomeé P, Währborg P, Börjesson M, Thomeé R, Eriksson BI, Karlsson J. Determinants of self-efficacy in the rehabilitation of patients with anterior cruciate ligament injury. J Rehabil Med. 2007;39(6):486–492. doi: 10.2340/16501977-0079. [DOI] [PubMed] [Google Scholar]
- 43.Chmielewski TL, Jones D, Day T, Tillman SM, Lentz TA, George SZ. The association of pain and fear of movement/reinjury with function during anterior cruciate ligament reconstruction rehabilitation. J Orthop Sports Phys Ther. 2008;38(12):746–753. doi: 10.2519/jospt.2008.2887. [DOI] [PubMed] [Google Scholar]
- 44.Hartigan EH, Lynch AD, Logerstedt DS, Chmielewski TL, Snyder-Mackler L. Kinesiophobia after anterior cruciate ligament rupture and reconstruction: noncopers versus potential copers. J Orthop Sports Phys Ther. 2013;43(11):821–832. doi: 10.2519/jospt.2013.4514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lentz TA, Zeppieri G, Jr, George SZ, et al. Comparison of physical impairment, functional, and psychosocial measures based on fear of reinjury/lack of confidence and return-to-sport status after ACL reconstruction. Am J Sports Med. 2015;43(2):345–353. doi: 10.1177/0363546514559707. [DOI] [PubMed] [Google Scholar]
- 46.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55(1):68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- 47.Eastlack ME, Axe MJ, Snyder-Mackler L. Laxity, instability, and functional outcome after ACL injury: copers versus noncopers. Med Sci Sports Exerc. 1999;31(2):210–215. doi: 10.1097/00005768-199902000-00002. [DOI] [PubMed] [Google Scholar]
- 48.Johnston LH, Carroll D. The provision of social support to injured athletes: a qualitative analysis. J Sport Rehabil. 1998;7(4):267–284. [Google Scholar]
- 49.Tjong VK, Murnaghan ML, Nyhof-Young JM, Ogilvie-Harris DJ. A qualitative investigation of the decision to return to sport after anterior cruciate ligament reconstruction: to play or not to play. Am J Sports Med. 2014;42(2):336–342. doi: 10.1177/0363546513508762. [DOI] [PubMed] [Google Scholar]
- 50.Ardern CL, Osterberg A, Tagesson S, Gauffin H, Webster KE, Kvist J. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br J Sports Med. 2014;48(22):1613–1619. doi: 10.1136/bjsports-2014-093842. [DOI] [PubMed] [Google Scholar]
- 51.Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2013;41(7):1549–1558. doi: 10.1177/0363546513489284. [DOI] [PubMed] [Google Scholar]
- 52.Webster KE, Feller JA, Lambros C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys Ther Sport. 2008;9(1):9–15. doi: 10.1016/j.ptsp.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 53.Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45(7):596–606. doi: 10.1136/bjsm.2010.076364. [DOI] [PubMed] [Google Scholar]