Abstract
Context:
Multiple factors are likely associated with an adolescent athlete's ability to return to play after anterior cruciate ligament (ACL) reconstruction (ACLR).
Objective:
To investigate the relationship between self-reported and functional outcome measures on return-to-play timing in an adolescent population, in athletes who returned and those who did not return to sport, and to identify a cutoff value for isometric quadriceps strength that could serve as a clinical target for maximizing the odds of returning to play after ACLR.
Design:
Cross-sectional study.
Setting:
Outpatient clinic.
Patients or Other Participants:
Adolescent athletes who underwent ACLR and completed clinical measures at their 3- and 6-month follow-up appointments were included.
Main Outcome Measure(s):
Clinical measures included functional outcomes of isometric and isokinetic strength tests and the Anterior Cruciate Ligament Return to Sport After Injury scale and the pediatric version of the International Knee Documentation Committee subjective form. Physician clearance dates for return to play were obtained from patient records.
Results:
Higher strength measures were associated with better scores on the Anterior Cruciate Ligament Return to Sport After Injury and the pediatric version of the International Knee Documentation Committee instruments at each follow-up. Differences were found in isometric extension strength (P = .001) and isokinetic extension strength at 180°/s (P = .03) and 300°/s (P = .002) between patients who returned to sports and those who did not. A 6-month isometric extension deficit (mean Limb Symmetry Index = 85.48 ± 23.15) displayed high accuracy (area under the curve = 0.82, 95% confidence interval = 0.68, 0.95) for identifying patients who returned to play after ACLR.
Conclusions:
Higher strength measures at both 3 and 6 months after ACLR were associated with greater self-reported knee function and greater readiness to return to functional activities at 6 months and ultimately earlier return to sport in adolescent athletes. These results provide evidence that self-reported outcome scores should be used as an additional screening tool in conjunction with quadriceps strength testing to help provide realistic recovery timeframes for adolescent patients.
Key Words: knee, strength, International Knee Documentation Committee form, ACL Return to Sport After Injury scale
Key Points
Improved functional strength measures at 3 and 6 months postoperatively were associated with improved self-reported knee function and greater readiness to return to functional activities after anterior cruciate ligament reconstruction.
Self-reported outcome scores should be used as additional screening tools in conjunction with quadriceps strength testing to help promote improved recovery and resumption of functional activities in adolescent athletes.
Anterior cruciate ligament (ACL) injuries are extremely prevalent within the athletic population, with more than 300 000 injuries occurring annually in the United States.1 Until recently, it was believed that ACL injuries in pediatric and adolescent athletes were predominantly avulsion fractures of the tibial spine.2 Further examination of the condition has demonstrated a higher incidence of midsubstance ACL tears than previously believed. Researchers3−5 have reported that the ACL injuries in skeletally immature athletes accounted for 0.5% to 3% of all ACL injuries. Authors of other epidemiologic studies6,7 have observed that, in children with traumatic acute knee hemarthosis and effusion, 29% and 47%, respectively, were diagnosed with an ACL injury. The percentage of these pediatric and adolescent athletes undergoing ACL reconstruction (ACLR) is on the rise.8,9 As surgical techniques for skeletally immature athletes advance and surgical interventions become more prevalent in this population, examining the requirements needed for a safe return to play is pertinent.
A successful ACLR has traditionally been defined as a return to normal symmetric function based on multiple clinical measures, including muscular power and endurance, functional movement, and proprioception of the involved extremity.10 Objective measures, such as isokinetic and isometric strength testing, as well as additional functional testing that analyzes a series of double- and single-limb hop tasks, are often used to determine an athlete's readiness to return to sport after ACLR.11,12 These functional tests are frequently conducted at specific postoperative time points to assess progress throughout rehabilitation. Clearance for return to play normally requires a Limb Symmetry Index (LSI), or quadriceps strength, of >80%−90% of the contralateral side.12,13 Adult athletes are typically expected to return to functional or sport-related activities between 6 and 12 months after ACLR; most individuals will successfully return to sport by 1 year after surgery.14 However, limited evidence suggests that these time points are appropriate for adolescent athletes.
As previously noted, physical impairments and return to function are well studied and represented within the literature and clinical practice. Psychological aspects of injury, especially in younger adolescents, may be less apparent and subsequently may not be fully addressed in typical clinical settings. Numerous psychosocial and environmental factors have been identified as potential barriers to return to sport. These factors include a general loss of interest in sport, changes in level of play, and fear of reinjury.6,10,14−18 Other factors, such as lifestyle changes, loss of motivation, and perceived self-efficacy, may also contribute to whether athletes return to sport.10,19 Self-reported outcome scales can be used to gain a better understanding of how an athlete feels about his or her knee function and readiness to return to sport after an injury. However, self-reported outcome measures have not been used routinely in adolescent patients, thereby limiting our understanding of this population's satisfaction after surgical intervention.20 In addition, little evidence addresses how clinical outcome measures of subjective function, psychological readiness, and strength may be associated with an adolescent patient's recovery of function and ability to obtain clearance to return to play and resume an active lifestyle. Therefore, the primary purpose of our study was to investigate the association between functional strength measurements and self-reported outcomes and how they related to return-to-play timing in adolescent athletes who underwent ACLR. We hypothesized that higher strength measures would correlate with better self-reported outcome scores and earlier return-to-play timing. Additionally, we proposed that athletes who returned to play within a year of surgery (RTP) would have better self-reported outcome scores and strength measures compared with those athletes who did not return to play within a year of surgery (NRTP). A secondary aim of this study was to identify a cutoff value for isometric quadriceps strength that could serve as a clinical target for maximizing the odds of returning to play after ACLR.
METHODS
Study Design
This study was a retrospective review that employed a cross-sectional design. Institutional review board approval was obtained before data collection.
Participants
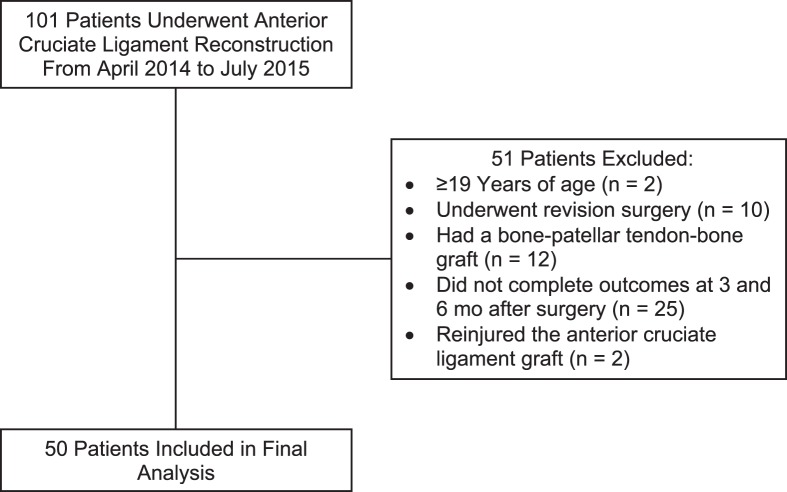
All participants were patients of 2 fellowship-trained orthopaedic surgeons at an outpatient pediatric and adolescent sports medicine clinic. Patients were identified by the Current Procedural Terminology code 29888 as having an ACL tear. A search of the medical records revealed a total of 101 patients who underwent ACLR using a hamstrings autograft between April 2014 and July 2015. Patients who had concomitant meniscal involvement requiring meniscectomy or meniscal repair were included in this study. Patients were excluded if they were 19 years of age or older at the time of surgery, failed to follow up at 3 and 6 months after surgery, had a previous surgery on the contralateral knee, had reconstructive surgery with a bone-patellar tendon-bone graft, underwent a revision surgery, or sustained a multiligamentous injury (Figure 1). All included patients were referred for rehabilitative therapy postoperatively, and a standard ACLR postoperative rehabilitation protocol was provided to both the patient and treating therapist. Physician clearance to resume unrestricted athletics was determined by a combination of criteria: full, pain-free range of motion; resolution of joint effusion; an LSI of >80% for quadriceps isometric and isokinetic testing at 180°/s; and a satisfactory score on the Noyes hop test. Patients were categorized based on clearance status: RTP or NRTP.
Figure 1.
Patient flow chart.
Measures
Clinical data (age, sex, date of surgery, and physician clearance date for return to play, when applicable) were obtained from the patients' medical records. During the 3- and 6-month clinic appointments, as part of the surgeon's standard postoperative care, patients completed 2 self-reported outcome forms, as well as a functional strength test. Return-to-play timing was determined from clinical notes as the date the surgeon released all physical restrictions after a review of the functional performance testing results when appropriate and calculated as the number of months between surgery and return to play.
Self-Reported Outcomes
The ACL Return to Sport After Injury (ACL-RSI) scale was used to assess the patient's readiness to return to functional activity. The ACL-RSI is a 12-item, valid, and reliable questionnaire designed to incorporate specific elements, such as patient confidence and risk appraisal, and is associated with an athlete's readiness to return to functional activity.21 The ACL-RSI scores range from 0 to 100, with higher scores representing patients who are more ready to return to sport. An ACL-RSI score of 56 or less has correctly identified adult athletes who may fail to return to their sport after surgery due to psychological factors.22 Self-reported knee function was measured using the pediatric version of the International Knee Documentation Committee (Pedi-IKDC) subjective evaluation form. The Pedi-IKDC is a 13-item, valid, and reliable knee-specific outcome measure.23,24 Pediatric IKDC scores range from 0 to 100, with higher scores indicating healthier knee function.
Objective Outcomes
Strength measurements were collected using a Humac isokinetic dynamometer (CSMi Solutions, Stoughton, MA) for both the surgical and contralateral limbs. For all testing procedures, the uninvolved extremity was tested first, followed by the involved extremity, and patients were allowed a practice trial before data collection. Isometric strength tests of the quadriceps and hamstrings muscle groups were completed at both 3 and 6 months postoperatively. Isometric strength was measured as the average torque across the 3 trials and reported as the deficit ratio between the surgical and contralateral limbs, also known as the LSI.25 Patients completed 3 trials with each knee in 60° of flexion and were allowed a 10-second rest period between trials. Isokinetic concentric strength testing of the quadriceps and hamstrings muscle groups was conducted at the patient's 6-month clinic visit. Isokinetic testing was similarly measured as the average torque across the 3 trials and was reported as an LSI percentage. Patients completed 3 trials through a full range of knee motion at 60°/s, 180°/s, and 300°/s and were allowed a 30-second rest period between trials.
Statistical Analysis
Initial bivariate Pearson product moment correlations were performed between LSI outcome predictor variables (isometric flexion and extension and isokinetic flexion and extension at 60°/s, 180°/s, and 300°/s) and self-reported outcomes (ACL-RSI, Pedi-IKDC) for all patients at both the 3- and 6-month time points. Correlation coefficients (r) were classified as weak (0.4), moderate (0.4−0.7), or strong (0.7−1.0).26 Pearson product moment correlations were also performed between all predictor variables. Spearman ρ correlations were performed in the case of any non-normally distributed variables.
Follow-up hierarchal multiple linear regression analyses were then calculated to examine the variance in the ACL-RSI and Pedi-IKDC scores at 6 months that could be explained by the variance in each outcome variable at both the 3- and 6-month testing sessions. The order in which the predictor variables were entered into the regression model was determined by the magnitude of the respective Pearson product moment correlations. Only predictor variables that demonstrated significant Pearson product moment correlations were entered into the regression models. The R2 value of the model was reported along with the change in R2 after the addition of each subsequent variable into the model.
Additional bivariate Pearson product moment correlations and hierarchal multiple linear regression analyses were also performed on only the group of patients (n = 34) who returned to play, in the same manner as described earlier, using the independent functional variable predictors (LSI isometric flexion, LSI isometric extension, LSI isokinetic flexion, and LSI isokinetic extension at 60°/s, 180°/s, and 300°/s) and self-reported outcome variable predictors (ACL-RSI, Pedi-IKDC) to determine how these affected return-to-play timing.
To further identify outcomes that help explain those who go on to return to play, separate independent-samples t tests were conducted to examine the differences in functional strength measures and self-reported outcomes at 3 and 6 months between patients in the RTP and NRTP groups. Lastly, a separate receiver operating characteristic (ROC) curve was constructed to determine the ability of 6-month LSI isometric extension strength to predict the dichotomous variable of return to play. Limb Symmetry Index isometric extension is a common, clinically relevant measure used to assess quadriceps strength after ACLR.27 In this case, return to play was categorized as either yes, RTP, or no, NRTP. Results of the ROC curve were reported as the area under the curve (AUC) and corresponding 95% confidence intervals (CIs). The strength of the AUC represented a perfect test (0.9−1), highly accurate test (0.7−0.89), moderately accurate test (0.69−0.5), or noninformative test (<0.5).28 A cutoff score for LSI isometric extension values that maximized the sensitivity and specificity for return to play was determined by identifying the LSI values on the ROC curve positioned closest to the upper left corner of the graph (Figure 2). Odds ratios and corresponding 95% CIs for return to play based on the cutoff scores for LSI isometric extension were calculated. Additional odds ratios were calculated as previously described for both males and females. The level of statistical significance was established a priori at α ≤ .05. All statistical analyses were performed using SPSS (version 24; IBM Corp, Armonk, NY).
Figure 2.
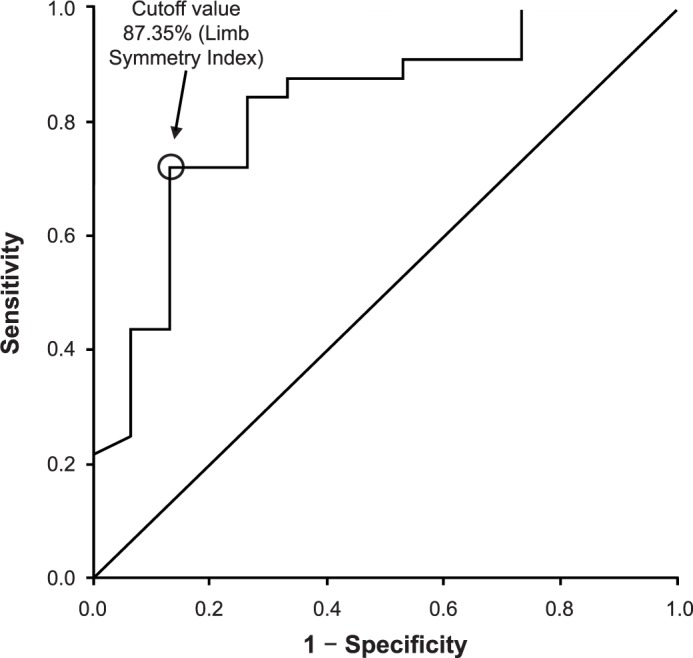
Receiver operating characteristic curve for 6-month Limb Symmetry Index isometric extension predicting return to play.
RESULTS
A total of 50 adolescent patients (27 males/23 females; average age = 15.9 ± 1.82 years, range = 11.4–18.8 years) were included in the final analysis. See Figure 1 for the delineation of excluded patients. Additional demographic data are shown in Table 1, and means and standard deviations for all main outcome variables and group differences can be found in Table 2.
Table 1.
Demographic Characteristics
| Characteristic |
Group |
|
| Returned to Play (n = 34) |
Did Not Return to Play (n = 16) |
|
| Sex | ||
| Male | 21 | 6 |
| Female | 13 | 10 |
| Average age, y (mean ± SD [range]) | 15.9 ± 1.8 (11.4−18.5) | 15.6 ± 1.9 (12.2−18.8) |
| Additional surgical procedures | ||
| Meniscal pathologic condition, % | 44 | 62 |
| Meniscal repair, No. | 12 | 8 |
| Meniscectomy, No. | 3 | 2 |
| Surgical modifications | ||
| Physeal sparing, No. | 3 | 1 |
| Average time to return to play, mo (mean ± SD [range]) | 7.4 ± 1.9 (4.1−12.2) | NA |
Abbreviation: NA, not applicable.
Table 2.
Main Outcome Variables (Mean ± SD)
| Variable |
3-Month Visit |
6-Month Visit |
| Limb Symmetry Index | ||
| Isometric extension | 74.42 ± 20.37 | 85.48 ± 23.15 |
| Isometric flexion | 66.27 ± 20.30 | 79.44 ± 15.08 |
| Isokinetic extension at 60°/s | a | 85.37 ± 23.15 |
| Isokinetic extension at 180°/s | a | 86.03 ± 15.18 |
| Isokinetic extension at 300°/s | a | 87.16 ± 20.28 |
| Isokinetic flexion at 60°/s | a | 90.95 ± 13.42 |
| Isokinetic flexion at 180°/s | a | 94.21 ± 15.53 |
| Isokinetic flexion at 300°/s | a | 96.61 ± 21.52 |
| Anterior Cruciate Ligament Return to Sport After Injury scale | 64.23 ± 20.48 | 74.12 ± 19.29 |
| Pediatric International Knee Documentation Committee self-reported questionnaire | 69.17 ± 13.79 | 83.49 ± 14.48 |
The relationship was not measured at 3 months.
Functional Strength Measures on Self-Reported Outcomes at 3 and 6 Months
Correlation analyses for the 3-month postoperative variables identified several associations (Table 3). A greater LSI for isometric extension was moderately associated with higher Pedi-IKDC scores at 3 months and weakly associated with higher ACL-RSI scores at 6 months. Higher ACL-RSI scores were moderately associated with higher Pedi-IKDC scores at 3 months. In addition, higher Pedi-IKDC scores at 3 months were weakly associated with higher Pedi-IKDC scores at 6 months.
Table 3.
Pearson Product Moment Correlationsa for Subjective Outcomes
| 3-Month Outcome Variable |
Months After Anterior Cruciate Ligament Reconstruction |
|||||||
| 3 |
6 |
|||||||
| ACL-RSI |
Pedi-IKDC |
ACL-RSI |
Pedi-IKDC |
|||||
|
r Value |
P Value |
r Value |
P Value |
r Value |
P Value |
r Value |
P Value |
|
| Limb Symmetry Index: isometric extension | 0.25 | .11 | 0.47 | .002b | 0.38 | .009b | 0.28 | .06 |
| Limb Symmetry Index: isometric flexion | 0.28 | .97 | 0.23 | .14 | 0.20 | .30 | 0.06 | .69 |
| ACL-RSI score | c | c | 0.55 | <.001b | 0.23 | .15 | 0.17 | .27 |
| Pedi-IKDC score | c | c | c | c | 0.31 | .05 | 0.37 | .01d |
Abbreviations: ACL-RSI, Anterior Cruciate Ligament Return to Sport after Injury; Pedi-IKDC, Pediatric International Knee Documentation Committee.
Correlation coefficients were classified as weak (0–0.4), moderate (0.4–0.7), or strong (0.7–1.0).
Indicates relationship (P ≤ .01).
The relationship was redundant and, therefore, was omitted.
Indicates relationship (P ≤ .05).
Correlation analyses for the 6-month postoperative variables also identified several associations (Table 4). Greater LSIs for isometric extension were associated with higher ACL-RSI and Pedi-IKDC scores. Higher LSI values for isometric flexion were associated with higher Pedi-IKDC scores. Higher ACL-RSI scores were associated with higher LSIs for isokinetic extension at all 3 testing speeds. Additionally, higher ACL-RSI scores were associated with higher Pedi-IKDC scores.
Table 4.
Pearson Product Moment Correlationsa of Main Outcome Variables at 6 Months
| Outcome Variable |
Anterior Cruciate Ligament Return to Sport After Injury Score |
Pediatric International Knee Documentation Committee Self-Reported Questionnaire Score |
||
|
r Value |
P Value |
r Value |
P Value |
|
| Limb Symmetry Index | ||||
| Isometric extension | 0.36 | .01b | 0.34 | .01b |
| Isometric flexion | 0.23 | .13 | 0.31 | .03b |
| Isokinetic extension at 60°/s | 0.54 | .001c | 0.32 | .05 |
| Isokinetic extension at 180°/s | 0.43 | .009c | 0.28 | .09 |
| Isokinetic extension at 300°/s | 0.34 | .04b | 0.18 | .27 |
| Isokinetic flexion at 60°/s | 0.02 | .91 | 0.06 | .74 |
| Isokinetic flexion at 180°/s | 0.24 | .15 | 0.16 | .35 |
| Isokinetic flexion at 300°/s | 0.03 | .87 | −0.01 | .94 |
| Anterior Cruciate Ligament Return to Sport After Injury scale | d | d | 0.51 | <.001c |
| Pediatric International Knee Documentation Committee self-reported questionnaire | d | d | d | d |
Correlation coefficients were classified as weak (0–0.4), moderate (0.4–0.7), or strong (0.7–1.0).
Indicates relationship (P ≤ .05).
Indicates relationship (P ≤ .01).
The relationship was redundant and, therefore, was omitted.
The multiple hierarchical regression model (Table 5) examining 3-month Pedi-IKDC scores, 6-month ACL-RSI scores, and 6-month LSIs for isometric extension and flexion predicted 47% of the variance in 6-month Pedi-IKDC scores; however, 6-month ACL-RSI scores significantly predicted 44% of the total variance, with the remaining variables demonstrating nonsignificant R2 change values and providing only 3% to the model. In the second model examining 6-month ACL-RSI scores, the 6-month LSI for isokinetic extension at 60°/s was the largest predictor at 28% of the variance in the 6-month ACL-RSI scores. The other variables contributed 27% of the variance and wholly explained 55% of the variance in the 6-month ACL-RSI scores. However, the second largest single predictor of the variance was the 6-month Pedi-IKDC score, which contributed an R2 change of 13% to the model and, when combined with the 6-month LSI for isokinetic extension at 60°/s, drove 41% of the total variance.
Table 5.
Regression Analyses Performed Using Predictor Variables to Explain the Variance in the 6-Month Pediatric International Knee Documentation Committee (Pedi-IKDC) Self-Reported Questionnaire and Anterior Cruciate Ligament Return to Sport After Injury Scale
| Model |
Variable |
R2 Value |
P Value |
ΔR2 Value |
P Value |
| Pedi-IKDC score | |||||
| 1 | 6-mo Anterior Cruciate Ligament Return to Sport After Injury score | 0.440a | <.001 | 0.440a | <.001 |
| 2 | 3-mo Pedi-IKDC score | 0.448a | <.001 | 0.008 | .50 |
| 3 | 6-mo LSI: isometric extension | 0.450a | <.001 | 0.002 | .71 |
| 4 | 6-mo LSI: isometric flexion | 0.471a | <.001 | 0.021 | .27 |
| Anterior Cruciate Ligament Return to Sport After Injury scale | |||||
| 1 | 6-mo LSI: isokinetic extension at 60°/s | 0.279a | .002 | 0.279a | .002 |
| 2 | 6-mo Pedi-IKDC score | 0.410a | .001 | 0.131a | .02 |
| 3 | 6-mo LSI: isokinetic extension at 180°/s | 0.411a | .002 | 0.002 | .79 |
| 4 | 3-mo LSI: isometric extension | 0.435a | .004 | 0.024 | .30 |
| 5 | 6-mo LSI: isometric extension | 0.524a | .002 | 0.088a | .04 |
| 6 | 6-mo LSI: isokinetic extension at 300°/s | 0.550a | .002 | 0.026 | .25 |
Abbreviation: LSI, Limb Symmetry Index.
Indicates difference (P ≤ .05).
Functional Strength and Self-Reported Outcomes on Return-to-Play Timing
Further Pearson correlation analyses examining the relationship between functional strength and self-reported outcome measures at 3 and 6 months indicated that, at 3 months post-ACLR, the LSIs for both isometric extension (r = −0.45, P = .01) and flexion (r = −0.44, P = .01) were moderately associated with return-to-play timing, demonstrating that greater strength was associated with quicker timing. The 6-month ACL-RSI and Pedi-IKDC scores and LSI for isokinetic extension at 60°/s were moderately associated with earlier return to play, whereas the LSI for isometric extension was weakly associated with earlier return to play (Table 6). The multiple regression model using the 3-month LSIs for isometric extension and flexion predicted 25% of the variance in return-to-play timing. The LSI values for isometric extension and flexion were both significant to the model; however, the LSI for isometric extension predicted 20% of the total variance, whereas the LSI for isometric flexion had a nonsignificant R2 change of 5% (P = .19). A second model using 6-month self-reported outcome scores and the LSIs for isometric and isokinetic extension significantly predicted 55% of the overall variance in return-to-play timing. The largest predictor of return-to-play timing was the Pedi-IKDC score at 6 months (29%). The other 3 variables added an additional 25% to the model, but the values for the corresponding R2 change were insignificant contributors (Table 7).
Table 6.
Pearson Product Moment Correlationsa of Return-to-Play Timing
| Outcome Variable |
Return-to-Play Timing |
|
|
r Value |
P Value |
|
| 3 mo | ||
| Anterior Cruciate Ligament Return to Sport After Injury score | −0.04 | .86 |
| Pediatric International Knee Documentation Committee self-reported questionnaire score | −0.26 | .19 |
| Limb Symmetry Index | ||
| Isometric extension | −0.45 | .01b |
| Isometric flexion | −0.44 | .01b |
| 6 mo | ||
| Anterior Cruciate Ligament Return to Sport After Injury score | −0.40 | .02b |
| Pediatric International Knee Documentation Committee self-reported questionnaire score | −0.43 | .01c |
| Limb Symmetry Index | ||
| Isometric extension | −0.39 | .02b |
| Isometric flexion | −0.21 | .25 |
| Isokinetic extension at 60°/s | −0.43 | .02b |
| Isokinetic extension at 180°/s | −0.28 | .13 |
| Isokinetic extension at 300°/s | −0.05 | .81 |
| Isokinetic flexion at 60°/s | −0.29 | .12 |
| Isokinetic flexion at 180°/s | −0.22 | .26 |
| Isokinetic flexion at 300°/s | 0.11 | .57 |
Correlation coefficients were classified as weak (0–0.4), moderate (0.4–0.7), or strong (0.7–1.0).
Indicates relationship (P ≤ .05).
Indicates relationship (P ≤ .01).
Table 7.
Regression Analyses Performed Using Predictor Variables to Explain the Variance in Return-to-Play Timing
| Model |
Variable |
R2 Value |
P Value |
ΔR2 Value |
P Value |
| Return to play 3-mo variable | |||||
| 1 | LSI: isometric extension | 0.203a | .01 | 0.203a | .01 |
| 2 | LSI: isometric flexion | 0.249a | .02 | 0.047 | .19 |
| Return to play 6-mo variable | |||||
| 1 | Pediatric International Knee Documentation Committee self-reported questionnaire score | 0.292a | .004 | 0.292a | .004 |
| 2 | LSI: isokinetic extension at 60°/s | 0.394a | .003 | 0.102 | .06 |
| 3 | Anterior Cruciate Ligament Return to Sport After Injury score | 0.429a | .006 | 0.036 | .25 |
| 4 | LSI: isometric extension | 0.546a | .002 | 0.117a | .03 |
Abbreviation: LSI, Limb Symmetry Index.
Indicates difference (P ≤ .05).
Comparisons of Functional Strength and Self-Reported Outcomes Between Return-to-Play Groups
We performed an independent-samples t test to determine if there were differences in functional strength and self-reported outcomes between patient groups (RTP versus NRTP). No differences for 3-month functional and self-reported outcomes were identified between groups. At the 6-month time point, the RTP group was stronger than the NRTP group in the LSIs for isometric flexion (P = .049), isometric extension (P = .001), and isokinetic extension at 180°/s (P = .03) and 300°/s (P = .002; Table 8).
Table 8.
Main Outcome Variables Between Returned-to-Play and Did-Not-Return-to-Play Groups and Independent t Test Results (P Value, 95% Confidence Interval)
| Outcome Variable |
Group (Mean ± SD) |
P Value |
t Value |
95% Confidence Interval |
|
| Returned to Play |
Did Not Return to Play |
||||
| 3 mo | |||||
| Anterior Cruciate Ligament Return to Sport After Injury score | 66.38 ± 19.05 | 60.47 ± 22.94 | .36 | 0.92 | −7.1, 18.8 |
| Pediatric International Knee Documentation Committee self-reported questionnaire score | 68.11 ± 14.41 | 70.99 ± 12.91 | .53 | −0.64 | −11.9, 6.2 |
| Limb Symmetry Index | |||||
| Isometric extension | 77.36 ± 18.07 | 68.13 ± 24.05 | .15 | 1.47 | −3.4, 21.9 |
| Isometric flexion | 69.50 ± 19.88 | 59.38 ± 20.10 | .11 | 1.62 | −2.5, 22.6 |
| 6 mo | |||||
| Anterior Cruciate Ligament Return to Sport After Injury score | 76.72 ± 16.49 | 68.41 ± 24.02 | .17 | 1.37 | −3.6, 20.3 |
| Pediatric International Knee Documentation Committee self-reported questionnaire score | 85.22 ± 14.45 | 79.93 ± 14.34 | .23 | 1.25 | −3.5, 14.1 |
| Limb Symmetry Index | |||||
| Isometric extension | 93.37 ± 19.82 | 68.62 ± 21.08 | .001a | 3.91 | 12.0, 37.5 |
| Isometric flexion | 82.37 ± 13.88 | 73.15 ± 16.07 | .049a | 2.02 | 0.0, 18.3 |
| Isokinetic extension at 60°/s | 86.48 ± 13.66 | 81.78 ± 14.51 | .38 | 0.89 | −6.0, 15.4 |
| Isokinetic extension at 180°/s | 89.03 ± 14.04 | 76.33 ± 15.41 | .03a | 2.32 | 1.6, 23.8 |
| Isokinetic extension at 300°/s | 92.69 ± 17.40 | 69.33 ± 19.34 | .002a | 3.43 | 9.5, 37.2 |
| Isokinetic flexion at 60°/s | 91.79 ± 13.76 | 88.22 ± 12.63 | .49 | 0.69 | −6.9, 14.0 |
| Isokinetic flexion at 180°/s | 95.62 ± 17.01 | 89.67 ± 8.54 | .32 | 1.01 | −6.1, 17.9 |
| Isokinetic flexion at 300°/s | 98.28 ± 20.06 | 91.22 ± 26.27 | .40 | 0.86 | −9.6, 23.7 |
Indicates difference between group means (P ≤ .05).
Predictive Capacity of the 6-Month LSI Isometric Extension Strength for Return to Play
The 6-month LSI for isometric extension (mean = 85.48 ± 23.15) displayed high accuracy (AUC = 0.82; 95% CI = 0.68, 0.95) for identifying patients who returned to play after ACLR (Figure 2). An LSI isometric extension value of 87.35% maximized the sensitivity (0.72) and specificity (0.87) for predicting return to play. Patients with a 6-month LSI isometric extension value ≥87.35% demonstrated 8.33 (95% CI = 2.13, 32.60) times the odds of returning to play compared with patients who exhibited LSI isometric extension values of <87.35% (Table 9). Males (n = 27) and females (n = 23) with an LSI isometric extension value of ≥87.35% demonstrated 9.00 (95% CI = 1.28, 63.02) and 6.40 (95% CI = 0.89, 45.99) times higher odds, respectively, of returning to play after ACLR.
Table 9.
Contingency Table for Limb Symmetry Index (LSI) Cutoff Score of 87.35% and Returned-to-Play Versus Did-Not-Return-to-Play Groups
| No. (%) |
|||
| 6 Months LSI: Isometric Extension, % |
Did Not Return to Play |
Returned to Play |
Total |
| <87.35 | 12 (57.1) | 9 (42.9) | 21 Patients with 6-mo LSI for isometric extension < 87.35 |
| ≥87.35 | 4 (13.8) | 25 (86.2) | 29 Patients with 6-mo LSI for isometric extension ≥ 87.35 |
| Total | 16 | 34 | 50 |
DISCUSSION
We sought to investigate the association between functional strength measures and self-reported outcomes and how they related to return-to-play timing in adolescent athletes who underwent ACLR. The results of this study may provide clinicians with an overview of functional and psychological indicators among adolescent athletes. Additionally, our findings may offer insight into those individuals who trend toward an extended recovery course after ACLR. First, patients who exhibited greater LSIs for isometric extension at 3 months postoperative had improved self-reported knee function and greater readiness to return to play at their 6-month follow-up. Second, a greater LSI for isometric extension at 3 months, along with higher self-reported knee function, readiness to return to functional activities, and a greater LSI for isokinetic extension at 6 months predicted a quicker return to play after ACLR. The RTP patients demonstrated greater LSIs for isometric extension and isokinetic strength at 180°/s and 300°/s than the NRTP patients. Lastly, patients who exhibited an LSI isometric extension value of ≥87.35% at 6 months had approximately 8 times the odds of returning to play compared with patients who exhibited an LSI isometric extension value of <87.35%.
Self-reported outcome questionnaires provide clinicians with valuable information regarding a patient's perception of his or her current knee function, such as symptoms, physical function, and activity level in daily life and sports.19 Numerous self-reported outcome questionnaires are available for use after ACLR to help clinicians further understand their patients' perceptions of their knee function over the course of recovery. However, the routine use of self-reported outcomes in a purely adolescent population has been limited.29 We chose to examine the Pedi-IKDC and ACL-RSI to gauge both an individual's perception of knee function and symptoms as well as his or her psychological feelings and readiness to return to functional activities after ACLR. The Pedi-IKDC differentiates between patients who exhibit greater knee symptoms and lower-level physical function from those with fewer symptoms and better knee function,19 whereas the ACL-RSI22 helps to identify those athletes who may not be psychologically ready to return to activities.
Our findings add clinically relevant information regarding patient-reported outcome measures of adolescent patients at 3 and 6 months after ACLR. Patients who returned to play demonstrated higher overall self-reported outcome scores on the Pedi-IKDC and ACL-RSI; however, the scores were not statistically different between groups. The ranges of our patients' subjective scores on both the 6-month Pedi-IKDC and ACL-RSI agreed with those in a recent review30 of factors affecting return-to-play rates after ACLR that determined patient self-reported function to be less than optimal (≥10% self-reported deficits) at the time of release to activity or sport. A self-reported functional deficit of less than 10% on self-reported outcome questionnaires, such as the Pedi-IKDC, IKDC, or Knee Injury and Osteoarthritis Outcome activity scale, is the current clinically recommended criterion for return to play.31 Both groups of patients in the present study demonstrated >10% deficits on the Pedi-IKDC, suggesting that, although some patients returned to play, they did not meet the clinical cutoff criteria for these self-reported scoring tools. In previous research,22 adult patients who scored 56 or less on the ACL-RSI were identified as those who may fail to return to functional activities after surgery due to psychological factors. The RTP group demonstrated ACL-RSI scores well above the 56 cutoff, whereas the NRTP group still scored above 56. It is important to note that these differences may be a factor of age, as no current normative data exist for adolescent patients on the ACL-RSI questionnaire. The findings of our study demonstrate that the ACL-RSI scale, in addition to the Pedi-IKDC and quadriceps strength, can be used as measures associated with return-to-play timing after ACLR. When examining the relationship between the 2 self-reported measures used in this study, we observed that 6-month ACL-RSI scores predicted almost half of the total variance in 6-month Pedi-IKDC scores, demonstrating the comparability of the 2 measures with regard to self-reported physical and psychological function. Additionally, greater readiness to return to functional activity and greater self-reported knee function were associated with faster return-to-play timing in those patients who returned to play.
Specific functional measures, such as isokinetic and isometric strength testing on a dynamometer, are frequently used to help evaluate limb symmetry in muscle strength and functional performance.25,32−35 These functional strength tests are often used at specific postoperative time points, as designated by the treating physician or therapist, to assess progress throughout the rehabilitation process. Current clearance criteria for return to play normally include lower limb symmetry measures that are >90% of the contralateral side.1,36,37 Greater isometric strength at 3 months postoperatively was associated with improved self-reported outcome measures at both 3 and 6 months and predicted faster return-to-play timing. Additionally, although isokinetic extension strength at 60°/s was moderately associated with return-to-play timing, only isometric extension strength predicted earlier return to play. A difference was found in 6-month LSIs for isometric and isokinetic extension between groups. Adolescent athletes in the RTP group demonstrated adequate strength and limb symmetry (>80%) for isometric extension strength and isokinetic extension strength at 180°/s and 300°/s. Patients in the NRTP group demonstrated LSIs that fell outside the clinically recommended cutoff value for almost all of the functional strength measures performed at the 6-month time point. Among patients in the NRTP group, their 3-month LSI for isometric extension strength values (68.13 ± 24.05) was almost identical to their 6-month LSI value (68.62 ± 21.08), demonstrating their inability to recover appropriate quadriceps function required to successfully return to play.
We further sought to determine a clinical cutoff tool for isometric extension strength that could be used as a clinically meaningful criterion for predicting return to play in adolescent athletes. We examined 6-month LSI percentage values for isometric extension strength to help identify patients who returned to play after ACLR. Patients in our study with a 6-month LSI for isometric extension >87.35% demonstrated 8 times greater odds of returning to play compared with patients who exhibited an LSI <87.35%. This finding is extremely relevant for clinicians working with adolescent athletes postoperatively as it agrees with previously published literature13,14,31 on appropriate strength criteria and clinically meaningful cutoff values. Earlier authors recommended functional strength measures of 80% to 90%; however, although this is clinically applicable, it does not always identify those individuals who still may fail or decide not to return to play after ACLR. Additional underlying barriers of return to play in adult athletes have been identified and discussed at length; yet the literature on adolescent athletes lacks consistency. An interesting finding of this study was that, when we considered sex in terms of differences in 6-month isometric extension strength, females were at 12-times higher odds of returning to play if they had an LSI for isometric extension strength of >87.35 compared with males, who were at 9 times higher odds. This may be an important clinical factor to note when adolescent females and males pursue rehabilitation programs.
Used in isolation, individual outcome measures can provide helpful clinical information, but how these measures relate to each other may offer a stronger clinical picture of the patient's actual recovery from surgery. A number of investigators30,38,39 have assessed the association between self-reported outcomes and functional measures after ACLR. Logerstedt et al19 found that lower IKDC scores suggested poor isometric quadriceps strength during functional testing for clearance to return to activity. Christensen et al18 noted an association between higher IKDC scores at 1 and 2 months after ACLR and better isometric extension limb symmetry. However, the average ages of the participants in these studies were 26.9 ± 9.7 and 33.0 ± 12.1 years, respectively. Zwolski et al38 evaluated the relationship between IKDC scores and isometric extension limb symmetry in adolescent athletes (average age = 16.7 ± 2.7 years) at the time of physician clearance after ACLR. They reported that patients with higher IKDC scores demonstrated an increased likelihood of exhibiting greater involved-limb isometric extension strength and better limb symmetry than patients who had lower knee function scores after ACLR. Our results agree with those of Zwolski et al,38 as we determined that improved isometric extension limb symmetry was associated with greater self-reported function and greater readiness to return to functional activities at 6 months after ACLR. In addition, 6-month isometric extension limb symmetry was different between RTP and NRTP patients. These results support the practice of assessing both self-reported and functional outcomes in adolescent athletes during the recovery phase after ACLR. However, to our knowledge, we are the first to examine the relationship between self-reported psychological readiness to return to functional activities and other clinical outcome measures in a strictly adolescent population.
A unique aspect of our study is that we examined both functional and self-reported outcome measures in an adolescent athletic population to better understand the relationship of physical function with self-reported function and readiness to return to functional activities after ACLR. Most previous authors have focused on a wider age range of individuals who sustained ACL injuries and subsequently underwent ACLR. We included only those athletes who had primary hamstrings autografts after ACLR to avoid possible discrepancies in outcome measures of patients with bone-patellar tendon-bone grafts or revision ACL surgeries. A limitation of this study is that we did not include those athletes who had bone-patellar tendon-bone grafts or ACL revisions as these could have confounded our results, thus preventing the results of this study from being generalizable to all patients who undergo surgical intervention for ACL tears. Additionally, we did not examine long-term rehabilitation results, contralateral injuries, or subsequent reinjury rates. Another limitation was the small sample size. A larger sample size might have resulted in significance of those findings that trended toward significance. Future researchers should study these factors with a larger population in long-term follow-up.
CONCLUSIONS
In an adolescent population, improved functional strength measures at 3 and 6 months after ACLR were associated with improved self-reported knee function and greater readiness to return to functional activities. In addition, both strength and self-reported outcomes were moderately associated with and can be used as collective predictors of return-to-play timing in those individuals who return to play. Lastly, continuing to use appropriate clinically recommended criteria for progression through rehabilitation and when making return-to-play decisions is pertinent, especially in young adolescent patient populations. These results provide evidence that self-reported outcome scores should be used as an additional screening tool in conjunction with quadriceps strength testing to help promote improved recovery and resumption of functional activities in adolescent athletes after ACLR.
ACKNOWLEDGMENTS
This study was supported by a grant from the Pediatric Orthopaedic Society of North America for ACLR return-to-play research (Dr Milewski). Financial reimbursement was received for editorial work with Elsevier, Inc (Dr Milewski).
REFERENCES
- 1.Abrams GD, Harris JD, Gupta AK, et al. Functional performance testing after anterior cruciate ligament reconstruction: a systematic review. Orthop J Sports Med. 2014;2(1):2325967113518305. doi: 10.1177/2325967113518305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schachter AK, Rokito AS. ACL injuries in the skeletally immature patient. Orthopedics. 2007;30(5):365–370. doi: 10.3928/01477447-20070501-01. quiz 371−372. [DOI] [PubMed] [Google Scholar]
- 3.Utukuri MM, Somayaji HS, Khanduja V, Dowd GS, Hunt DM. Update on paediatric ACL injuries. Knee. 2006;13(5):345–352. doi: 10.1016/j.knee.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 4.McConkey MO, Bonasia DE, Amendola A. Pediatric anterior cruciate ligament reconstruction. Curr Rev Musculoskelet Med. 2011;4(2):37–44. doi: 10.1007/s12178-011-9076-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alharby SW. Anterior cruciate ligament injuries in growing skeleton. Int J Health Sci (Qassim) 2010;4(1):71–79. [PMC free article] [PubMed] [Google Scholar]
- 6.Luhmann SJ. Acute traumatic knee effusions in children and adolescents. J Pediatr Orthop. 2003;23(2):199–202. [PubMed] [Google Scholar]
- 7.Stanitski CL, Harvell JC, Fu F. Observations on acute knee hemarthrosis in children and adolescents. J Pediatr Orthop. 1993;13(4):506–510. doi: 10.1097/01241398-199307000-00016. [DOI] [PubMed] [Google Scholar]
- 8.Dodwell ER, Lamont LE, Green DW, Pan TJ, Marx RG, Lyman S. 20 years of pediatric anterior cruciate ligament reconstruction in New York State. Am J Sports Med. 2014;42(3):675–680. doi: 10.1177/0363546513518412. [DOI] [PubMed] [Google Scholar]
- 9.Shea KG, Grimm NL, Ewing CK, Aoki SK. Youth sports anterior cruciate ligament and knee injury epidemiology: who is getting injured? In what sports? When? Clin Sports Med. 2011;30(4):691–706. doi: 10.1016/j.csm.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 10.Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45(7):596–606. doi: 10.1136/bjsm.2010.076364. [DOI] [PubMed] [Google Scholar]
- 11.Barber-Westin SD, Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27(12):1697–1705. doi: 10.1016/j.arthro.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 12.Mueller LM, Bloomer BA, Durall CJ. Which outcome measures should be utilized to determine readiness to play after ACL reconstruction? J Sport Rehabil. 2014;23(2):158–164. doi: 10.1123/jsr.2013-0018. [DOI] [PubMed] [Google Scholar]
- 13.Czuppon S, Racette BA, Klein SE, Harris-Hayes M. Variables associated with return to sport following anterior cruciate ligament reconstruction: a systematic review. Br J Sports Med. 2014;48(5):356–364. doi: 10.1136/bjsports-2012-091786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Müller U, Krüger-Franke M, Schmidt M, Rosemeyer B. Predictive parameters for return to pre-injury level of sport 6 months following anterior cruciate ligament reconstruction surgery. Knee Surg Sports Traumatol Arthrosc. 2015;23(12):3623–3631. doi: 10.1007/s00167-014-3261-5. [DOI] [PubMed] [Google Scholar]
- 15.Carey JL, Huffman GR, Parekh SG, Sennett BJ. Outcomes of anterior cruciate ligament injuries to running backs and wide receivers in the National Football League. Am J Sports Med. 2006;34(12):1911–1917. doi: 10.1177/0363546506290186. [DOI] [PubMed] [Google Scholar]
- 16.Kvist J. Rehabilitation following anterior cruciate ligament injury: current recommendations for sports participation. Sports Med. 2004;34(4):269–280. doi: 10.2165/00007256-200434040-00006. [DOI] [PubMed] [Google Scholar]
- 17.Thomeé R, Kaplan Y, Kvist J, et al. Muscle strength and hop performance criteria prior to return to sports after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19(11):1798–1805. doi: 10.1007/s00167-011-1669-8. [DOI] [PubMed] [Google Scholar]
- 18.Christensen JC, Goldfine LR, Barker T, Collingridge DS. What can the first 2 months tell us about outcomes after anterior cruciate ligament reconstruction? J Athl Train. 2015;50(5):508–515. doi: 10.4085/1062-6050-49.3.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Logerstedt D, Lynch A, Axe MJ, Snyder-Mackler L. Symmetry restoration and functional recovery before and after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21(4):859–868. doi: 10.1007/s00167-012-1929-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wells L, Dyke JA, Albaugh J, Ganley T. Adolescent anterior cruciate ligament reconstruction: a retrospective analysis of quadriceps strength recovery and return to full activity after surgery. J Pediatr Orthop. 2009;29(5):486–489. doi: 10.1097/BPO.0b013e3181aa2197. [DOI] [PubMed] [Google Scholar]
- 21.Lentz TA, Tillman SM, Indelicato PA, Moser MW, George SZ, Chmielewski TL. Factors associated with function after anterior cruciate ligament reconstruction. Sports Health. 2009;1(1):47–53. doi: 10.1177/1941738108326700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Webster KE, Feller JA, Lambros C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys Ther Sport. 2008;9(1):9–15. doi: 10.1016/j.ptsp.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 23.Kocher MS, Smith JT, Iversen MD, et al. Reliability, validity, and responsiveness of a modified International Knee Documentation Committee Subjective Knee Form (Pedi-IKDC) in children with knee disorders. Am J Sports Med. 2011;39(5):933–939. doi: 10.1177/0363546510383002. [DOI] [PubMed] [Google Scholar]
- 24.Irrgang JJ, Anderson AF. Development and validation of health-related quality of life measures for the knee. Clin Orthop Relat Res. 2002;(402):95–109. doi: 10.1097/00003086-200209000-00009. [DOI] [PubMed] [Google Scholar]
- 25.Knezevic OM, Mirkov DM, Kadija M, Milovanovic D, Jaric S. Evaluation of isokinetic and isometric strength measures for monitoring muscle function recovery after anterior cruciate ligament reconstruction. J Strength Cond Res. 2014;28(6):1722–1731. doi: 10.1519/JSC.0000000000000307. [DOI] [PubMed] [Google Scholar]
- 26.Cohen J, Cohen P, West S, Leona A. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences 3rd ed. Mahwah, NJ: Lawrence Erlbaum Associates;; 2003. [Google Scholar]
- 27.Schmitt LC, Paterno MV, Hewett TE. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2012;42(9):750–759. doi: 10.2519/jospt.2012.4194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Greiner M, Pfeiffer D, Smith RD. Principles and practical application of the receiver-operating characteristic analysis for diagnostic tests. Prev Vet Med. 2000;45(1−2):23–41. doi: 10.1016/s0167-5877(00)00115-x. [DOI] [PubMed] [Google Scholar]
- 29.Furlong W, Barr RD, Feeny D, Yandow S. Patient-focused measures of functional health status and health-related quality of life in pediatric orthopedics: a case study in measurement selection. Health Qual Life Outcomes. 2005;3:3. doi: 10.1186/1477-7525-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lepley LK, Palmieri-Smith RM. Quadriceps strength, muscle activation failure, and patient-reported function at the time of return to activity in patients following anterior cruciate ligament reconstruction: a cross-sectional study. J Orthop Sports Phys Ther. 2015;45(12):1017–1025. doi: 10.2519/jospt.2015.5753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lepley LK. Deficits in quadriceps strength and patient-oriented outcomes at return to activity after ACL reconstruction: a review of the current literature. Sports Health. 2015;7(3):231–238. doi: 10.1177/1941738115578112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Almosnino S, Brandon SC, Day AG, Stevenson JM, Dvir Z, Bardana DD. Principal component modeling of isokinetic moment curves for discriminating between the injured and healthy knees of unilateral ACL deficient patients. J Electromyogr Kinesiol. 2014;24(1):134–143. doi: 10.1016/j.jelekin.2013.10.012. [DOI] [PubMed] [Google Scholar]
- 33.Eitzen I, Holm I, Risberg MA. Preoperative quadriceps strength is a significant predictor of knee function two years after anterior cruciate ligament reconstruction. Br J Sports Med. 2009;43(5):371–376. doi: 10.1136/bjsm.2008.057059. [DOI] [PubMed] [Google Scholar]
- 34.Eitzen I, Moksnes H, Snyder-Mackler L, Engebretsen L, Risberg MA. Functional tests should be accentuated more in the decision for ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18(11):1517–1525. doi: 10.1007/s00167-010-1113-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Greenberg EM, Greenberg ET, Ganley TJ, Lawrence JT. Strength and functional performance recovery after anterior cruciate ligament reconstruction in preadolescent athletes. Sports Health. 2014;6(4):309–312. doi: 10.1177/1941738114537594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eitzen I, Moksnes H, Snyder-Mackler L, Risberg MA. A progressive 5-week exercise therapy program leads to significant improvement in knee function early after anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2010;40(11):705–721. doi: 10.2519/jospt.2010.3345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lautamies R, Harilainen A, Kettunen J, Sandelin J, Kujala UM. Isokinetic quadriceps and hamstring muscle strength and knee function 5 years after anterior cruciate ligament reconstruction: comparison between bone-patellar tendon-bone and hamstring tendon autografts. Knee Surg Sports Traumatol Arthrosc. 2008;16(11):1009–1016. doi: 10.1007/s00167-008-0598-7. [DOI] [PubMed] [Google Scholar]
- 38.Zwolski C, Schmitt LC, Quatman-Yates C, Thomas S, Hewett TE, Paterno MV. The influence of quadriceps strength asymmetry on patient-reported function at time of return to sport after anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(9):2242–2249. doi: 10.1177/0363546515591258. [DOI] [PubMed] [Google Scholar]
- 39.Oak SR, O'Rourke C, Strnad G, et al. Statistical comparison of the pediatric versus adult IKDC subjective knee evaluation form in adolescents. Am J Sports Med. 2015;43(9):2216–2221. doi: 10.1177/0363546515589108. [DOI] [PubMed] [Google Scholar]