Abstract
Background
Although satisfactory mid- to long-term results of rotational acetabular osteotomy for early osteoarthritis secondary to acetabular dysplasia have been reported, there is still controversy about the long-term effects of this surgery in more advanced osteoarthritis. The purpose of this study was to investigate the radiographic progression of osteoarthritic changes after rotational acetabular osteotomy in acetabular dysplasia according to the preoperative Tönnis grade and evaluate its effects after minimum 10-year follow-up.
Methods
We performed 71 consecutive rotational acetabular osteotomies in 64 patients with symptomatic acetabular dysplasia between November 1984 and April 2005. Of these, 46 hips (four hips with Tönnis grade 0, 30 with grade 1, and 12 with grade 2) whose clinical and radiographic findings were available after minimum 10-year follow-up were evaluated in this study. The mean age at the time of surgery was 39.0 years (range, 18 to 62 years) and the average follow-up duration was 17.3 years (range, 10.0 to 27.7 years). Clinical and radiographic evaluations were performed according to the preoperative Tönnis grade.
Results
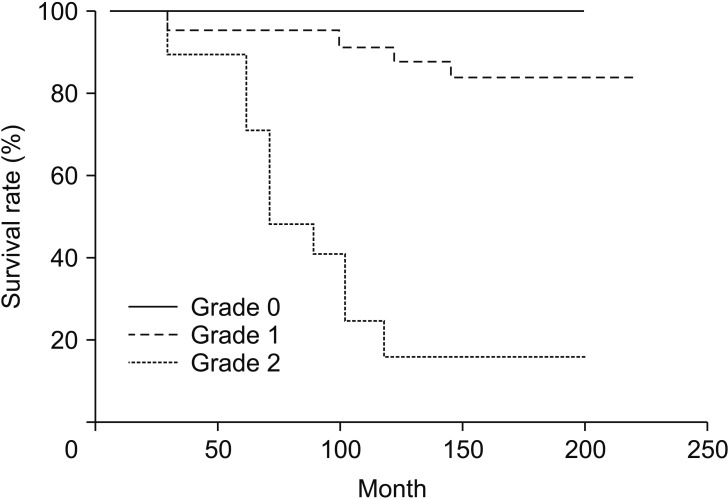
The average Harris hip score improved from 71.8 (range, 58 to 89) to 85.1 (range, 62 to 98). The radiographic parameters also improved in all Tönnis grades after the index surgery. Although the improvement of radiographic parameters was not different between preoperative Tönnis grades, the incidence of osteoarthritic progression was significantly different between grades (zero in Tönnis grade 0, four in Tönnis grade 1, and 10 in Tönnis grade 2; p < 0.001). The mean age at the time of surgery was also significantly older in osteoarthritic progression patients (p < 0.002). Kaplan-Meier survivorship analysis, with radiographic progression of osteoarthritis as the endpoint, predicted a 10-year survival rate of 100% in Tönnis grade 0, 85.7% in Tönnis grade 1, and 14.3% in Tönnis grade 2 (p < 0.001).
Conclusions
The outcome of rotational acetabular osteotomy in most hips with Tönnis grade 0 and 1 was satisfactory after an average of 17 years of follow-up. The incidence of osteoarthritic progression was higher in Tönnis grade 2 and older age. Our results support that early joint preserving procedure is essential in the case of symptomatic dysplastic hips.
Keywords: Hip, Acetabular dysplasia, Osteoarthritis, Rotational acetabular osteotomy
Acetabular dysplasia is characterized by insufficient coverage of the acetabulum (shallow and oblique acetabular weight bearing zone) to the femoral head and generally considered the most common cause of secondary osteoarthritis.1,2) According to Hasegawa et al.,3) osteoarthritis naturally develops in patients with untreated acetabular dysplasia. Although total hip arthroplasty is an effective method for the treatment of advanced osteoarthritis of the hip joint, there is still controversy because of concerns regarding the longevity of total hip arthroplasty in young and active patients.1,4)
For this reason, several pelvic osteotomies such as Steel's triple osteotomy,5) Eppright's dial osteotomy,6) Wagner's spherical acetabular osteotomy,7) Ninomiya and Tagawa's rotational acetabular osteotomy (RAO),8) and Ganz's periacetabular osteotomy9) have been utilized as joint preserving procedures to prevent the early onset of osteoarthritis by redistribution of the loads across the hip joint. These joint preserving surgeries are aimed at relieving pain, normalizing function, and improving the longevity of the native hip10) and have been shown with satisfactory mid- and long-term results in patients with early-stage osteoarthritis secondary to dysplasia of the hip.10,11,12,13) Although some authors reported successful results of RAO in more advanced osteoarthritis after mid-term follow-up, there is still controversy about the long-term effects of RAO in these patients.12,14,15,16) The purpose of this study was to investigate the radiographic progression of osteoarthritic changes after RAO in patients with acetabular dysplasia according to the preoperative Tönnis grade and evaluate its effects after minimum 10-year follow-up.
METHODS
Study Population
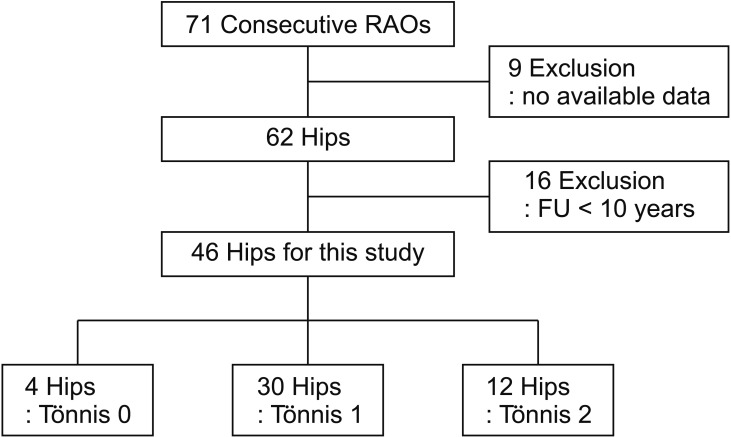
Between November 1984 and April 2005, we performed 71 consecutive RAO in 64 patients with symptomatic acetabular dysplasia. Of those, nine patients (nine hips) whose clinical and radiographic findings were not available, two patients (two hips) who died from causes unrelated to surgery, and 13 patients (14 hips) who were lost to follow up before the end of the minimum 10 years were excluded. After obtaining Institutional Review Board approval (IRB No. 2016-11-056), remaining 40 patients (46 hips) were retrospectively evaluated in this study. There were eight males and 38 females with a mean age of 39.0 years (range, 18 to 62 years) at the time of RAO. The average follow-up duration was 17.3 years (range, 10.0 to 27.7 years). The anteroposterior radiograph of the pelvis was used for the classification of preoperative osteoarthritis of the hip according to the criteria of Tönnis:17) grade 0 indicates no sign of degenerative changes, although there is acetabular dysplasia of the hip (four hips); grade 1 indicates increased sclerosis of the femoral head and acetabulum, slight narrowing of the joint space, and slight lipping at the joint margin (30 hips); grade 2 indicates small cysts in the femoral head and acetabulum, moderate narrowing of joint space, and moderate loss of sphericity of the femoral head (12 hips); and grade 3 indicates large cysts with gross narrowing or obliteration of the joint space, and severe deformity of the femoral head (zero hip) (Fig. 1). There were no significant differences in the patients' age, sex, side of operation, weight, height, body mass index (BMI), or follow-up duration between grades although the mean age at the time of surgery was getting older as per preoperative Tönnis grade (Table 1).
Fig. 1. The flow diagram shows how the final study cohort was determined based on inclusion and exclusion criteria. RAO: rotational acetabular osteotomy, FU: follow-up.
Table 1. Demographics of Patients Treated with Rotational Acetabular Osteotomy According to the Tönnis Grade of Preoperative Osteoarthritis.
| Demographics | Grade 0 (n = 4) | Grade 1 (n = 30) | Grade 2 (n = 12) | p-value |
|---|---|---|---|---|
| Age (yr) | 30.5 (21–39) | 38.8 (18–62) | 42.4 (23–60) | 0.20 |
| Sex (male:female) | 1:3 | 5:25 | 2:10 | 0.79 |
| Side of operation | 0.61 | |||
| Right | 1 | 16 | 6 | |
| Left | 3 | 14 | 6 | |
| Weight (kg) | 59.5 (50–75) | 58.8 (43–70) | 59.1 (43–75) | 0.86 |
| Height (cm) | 162.0 (155–170) | 159.9 (150–176) | 161.8 (150–170) | 0.23 |
| Body mass index (kg/m2) | 22.6 (19.5–26.0) | 22.9 (19.1–25.8) | 22.6 (20.2–25.8) | 0.87 |
| Follow-up duration (yr) | 15.3 (10.0–26.0) | 17.6 (10.0–27.7) | 17.9 (13.8–23.7) | 0.09 |
Values are presented as mean (range).
Surgical Procedure
The indications for RAO were as follows: increasing hip pain, center-edge angle of Wiberg18) less than 20°, and improved joint congruity of hips in abduction before surgery on anteroposterior radiographs. We performed a valgus femoral osteotomy in combination with RAO for better joint congruency in one hip. RAO was performed as described by Ninomiya and Tagawa.8) An anterior curved incision was made from just below the iliac crest towards the distal aspect of the greater trochanter and the hip was exposed anteriorly and posteriorly. The osteotomy line was marked about 1.5 cm from the acetabular rim, and a straight osteotome was inserted into the bone to a depth of about 1.5 cm without penetrating the joint. Then a curved osteotome was used to complete the osteotomy through the inner wall of the ilium. After complete osteotomy was done, the acetabular fragment was rotated anterolaterally, and an autogenous bone graft from the iliac crest was placed in the gap. Finally, two or three Kirschner wires were inserted to fix the acetabular fragment and the grafted bone. These Kirschner wires were removed through a small skin incision after 6–8 weeks of the index surgery. Active range of motion exercises were permitted after 1 week after surgery. Gradual partial weight-bearing with two crutches was allowed at 2 weeks, and full weight-bearing was initiated 6 to 8 weeks after surgery when radiographic bony union was achieved.
Assessment
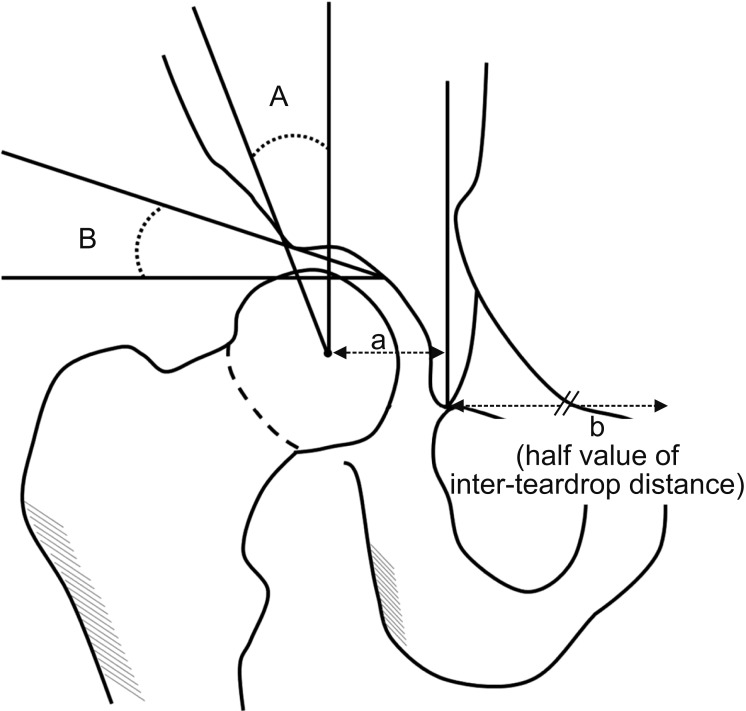
All clinical and radiographic data were collected retrospectively from the patient records. The clinical assessment with the Harris hip score was performed before the index surgery and at each follow-up visit. The radiographic parameters that were analyzed were the center-edge angle of Wiberg,18) the acetabular roof angle,19) and the head lateralization index20) based on the anteroposterior radiographs obtained preoperatively and 3 months postoperatively. All radiographic parameters were assessed by two orthopedic surgeons (BWM and KJL) and the mean values were calculated (Fig. 2). Radiographic progression of osteoarthritis according to the Tönnis grade was compared in the most recent radiographs with radiographs taken 3 months after surgery. We also evaluated intra- and postoperative complications based on the patient records.
Fig. 2. Radiographic parameters for evaluation of the hip. A: Center-edge angle. B: Acetabular roof angle. The head lateralization index is calculated using the distance between the teardrop and the center of the femoral head (a) divided by the half value of the inter-teardrop distance (b).
Statistical analysis was performed with SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). The differences in continuous variables such as age, BMI, Harris hip score, and radiographic parameters between each grade were compared using the Wilcoxon signed-rank test and Kruskal-Wallis test. The linear by linear test was used for analyses of categorical data such as sex, side of operation, and progression of osteoarthritis according to the Tönnis grade. We also evaluated the differences between osteoarthritic progression patients and nonprogression patients by using independent t-test and chi-square test. The p-values of < 0.05 were considered as significant. We performed Kaplan-Meier survivorship analysis for all hips with the progression of osteoarthritis as an endpoint.
RESULTS
Overall Results
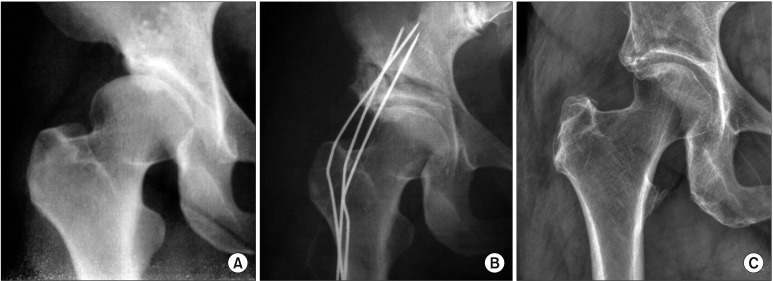
The average Harris hip score was improved from 71.8 (range, 58 to 89) preoperatively to 85.1 (range, 62 to 98) at the latest follow-up (p < 0.001). The center-edge angle improved from an average of 9.4° (range, −20° to 20°) preoperatively to an average of 38.7° (range, 14° to 60°) postoperatively (p < 0.001), and the mean acetabular roof angle improved from 29.5° (range, 20° to 56°) to 19.1° (range, 5° to 42°) (p < 0.001). Although the mean head lateralization index also improved from 0.66 (range, 0.5 to 0.9) to 0.63 (range, 0.4 to 0.9), the statistical difference was not significant (p = 0.09) (Fig. 3).
Fig. 3. Anteroposterior radiographs of the right hip joint in a 47-year-old male. (A) The preoperative radiograph shows mild acetabular dysplasia with no sign of degenerative change (Tönnis grade 0). (B) The postoperative radiograph shows improvement of acetabular coverage over the femoral head. Note that the osteotomized fragment and grafted bone were fixed with three Kirschner wires. (C) The Radiograph obtained 26 years after rotational acetabular osteotomy shows maintenance of good coverage and no progression of osteoarthritis.
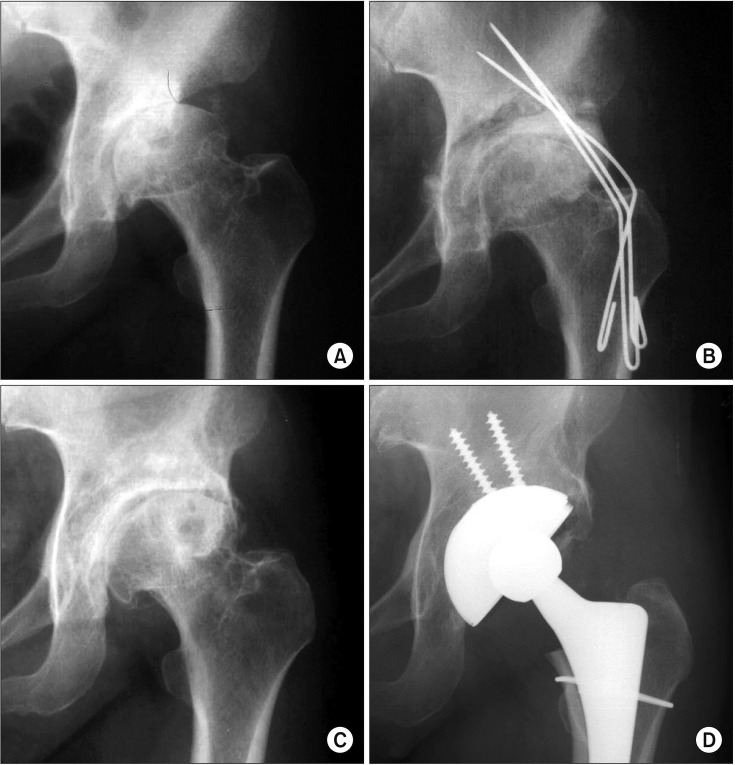
Based on the Tönnis grade, 14 hips had radiographic progression of osteoarthritis (zero in Tönnis grade 0, four in Tönnis grade 1, and 10 in Tönnis grade 2). The incidence of osteoarthritic progression was significantly different between grades (p < 0.001). Although there were no differences between osteoarthritic progression patients and nonprogression patients in terms of sex, height, weight, BMI, and pre- and postoperative radiographic parameters, the mean age at the time of surgery was significantly older in osteoarthritic progression patients (46.8 years; range, 23 to 62 years in progression patients vs. 35.6 years; range, 18 to 56 years in nonprogression patients; p < 0.002). At the final follow-up, eight hips (three in Tönnis grade 1 and five in Tönnis grade 2) were converted to total hip arthroplasty (Fig. 4), and the mean duration from the index surgery to total hip arthroplasty was 9.7 years (range, 1.2 to 23.5 years).
Fig. 4. Anteroposterior radiographs of the left hip joint in a 47-year-old female. (A) The preoperative radiograph shows moderate joint space narrowing with subchondral cyst in the femoral head (Tönnis grade 2). (B) The postoperative radiograph shows improvement of acetabular coverage over the femoral head. (C) The postoperative radiograph obtained 7 years after rotational acetabular osteotomy shows progression of osteoarthritis. (D) Total hip arthroplasty was performed 7.5 years after the index surgery due to progressive osteoarthritis.
Comparative Results According to the Tönnis Grade
The average Harris hip score was improved in all three groups: Tönnis grade 0, from 79.8 to 95.8 (p = 0.01); Tönnis grade 1, from 73.1 to 88.0 (p < 0.001); and Tönnis grade 2, from 65.8 to 74.4 (p = 0.03). The improvement of radiographic parameters according to the Tönnis grade is presented in Table 2. The incidence of osteoarthritic progression was significantly different according to the preoperative Tönnis grade. There was no progression case in Tönnis grade 0, four cases (13.3%) in Tönnis grade 1, and ten cases (83.3%) in Tönnis grade 2 (p < 0.001). The mean duration from the index surgery to osteoarthritic progression was 6.9 years (range, 1.3 to 10 years) in Tönnis grade 1 and 5.2 years (range, 1.2 to 9 years) in Tönnis grade 2 (p = 0.30).
Table 2. Improvement of Radiographic Parameters after Rotational Acetabular Osteotomy According to the Tönnis Grade of Preoperative Osteoarthritis.
| Parameter | Preoperative | Postoperative | p-value |
|---|---|---|---|
| Center-edge angle | |||
| Grade 0 | 4.9 ± 6.8 | 35.3 ± 4.8 | 0.01 |
| Grade 1 | 8.9 ± 9.9 | 37.4 ± 9.6 | < 0.001 |
| Grade 2 | 12.2 ± 5.1 | 43.0 ± 12.3 | < 0.001 |
| Acetabular roof angle | |||
| Grade 0 | 31.0 ± 2.7 | 18.7 ± 6.8 | 0.04 |
| Grade 1 | 28.8 ± 5.5 | 18.1 ± 8.1 | < 0.001 |
| Grade 2 | 30.7 ± 9.1 | 21.8 ± 9.8 | 0.01 |
| Head lateralization index | |||
| Grade 0 | 0.68 ± 0.09 | 0.55 ± 0.13 | 0.14 |
| Grade 1 | 0.67 ± 0.09 | 0.64 ± 0.12 | 0.12 |
| Grade 2 | 0.67 ± 0.08 | 0.70 ± 0.09 | 0.31 |
Values are presented as mean ± standard deviation.
Kaplan-Meier survivorship analysis, with radiographic progression of osteoarthritis as the endpoint, predicted a 10-year survival rate of 100 % in Tönnis grade 0, 85.7 % in Tönnis grade 1, and 14.3 % in Tönnis grade 2 (Fig. 5).
Fig. 5. The Kaplan-Meier survivorship analysis demonstrates the cumulative probability of osteoarthritic progression according to the Tönnis grade.
Complications
There were two cases of medial joint perforation intraoperatively which all healed without any complications at the latest follow-up. There were no other intra- or postoperative complications, including infection, avascular necrosis of the rotated acetabulum, delayed union of the osteotomy site, or heterotopic ossification.
DISCUSSION
In this study, we have shown that the clinical and radiographic parameters were improved after RAO in patients with acetabular dysplasia at the mean 17-year follow-up. Thirty-two out of 46 patients maintained their preoperative Tönnis grade after minimum 10-year follow-up and only eight patients received total hip arthroplasty at the final follow-up. However, the incidence of osteoarthritic progression and Kapan-Meier survivorship with radiographic progression of osteoarthritis as the endpoint were statistically different according to the preoperative Tönnis grade.
Acetabular dysplasia is a risk factor for hip osteoarthritis, and preservation of the native hip is important in these patients before the onset of moderate to severe arthrosis.1,2,10,21) Several pelvic osteotomies such as RAO have been utilized as joint preserving procedures and generally have been associated with satisfactory intermediate and long-term results in patients with pre- and early-stage osteoarthritis.2,12,14,22,23,24) Okano et al.24) reported the outcomes of RAO in 49 hips with early osteoarthritis after the mean duration of 13-year follow-up. In their study, the stage of osteoarthritis was unchanged in 38 hips and had progressed in 11 hips (including two technical failures). More recently, Yasunaga et al.23) also reported durable results of RAO for pre- and early osteoarthritis at 20 years. Among the 145 hips (27 hips with pre-osteoarthritis and 118 hips with early-stage osteoarthritis), radiographic progression of osteoarthritis occurred in 25 hips. Kaplan-Meier survivorship analysis, with radiographic signs of progression of osteoarthritis as an endpoint, predicted survival of 96% at 10 years and 20 years in the pre-osteoarthritis group and 89% at 10 years and 78% at 20 years in the early-stage group. In our study, Kaplan-Meier survivorship analysis, with radiographic progression of osteoarthritis as an endpoint, predicted a 10-year survival rate of 100% in Tönnis grade 0 and 85.7 % in Tönnis grade 1 at 10 years. This finding is similar to that of Yasunaga et al.23)
In contrast with the pre- and early-stage osteoarthritis, there is still controversy about the effects of RAO in more advanced osteoarthritis secondary to acetabular dysplasia. Yasunaga et al.25) reported the result of RAO for advanced osteoarthritis after a mean follow-up of 8.5 years. In their study, 10 out of 43 hips with preoperative advanced osteoarthritis had radiographic evidence of progression of osteoarthritis at final follow-up and the predicted 10-year survival rate was 72.22% at 10 years. Nozawa et al.14) also reported the results in 50 hips at an average of 11 years after RAO. Among them, there were 11 hips with preoperative Tönnis grade 2 arthritis and only two had progression of arthritis at final follow-up. On the other hand, Kaneuji et al.16) reported long-term outcome of RAO after a minimum of 20 years. In their report, the prevalence of osteoarthritic progression was 37% in advanced osteoarthritis and the hips with advanced osteoarthritis had a significantly higher rate of conversion to total hip arthroplasty than hips in the other stages did (4% with pre-osteoarthritis, 7% with initial osteoarthritis, and 34% with advanced osteoarthritis). In another study, Nozawa el al.15) evaluated the outcome of RAO for 57 hips with advanced osteoarthritis at a mean of 148.6 months (range, 24 to 254 months). Although 50 of the 57 hips were still functioning at final follow-up, progression of osteoarthritis was detected in 26 hips. In our patients, 10 out of 12 hips with Tönnis grade 2 had progression of arthritic changes and five hips (41.7%) had conversion total hip arthroplasty at final follow-up.
Regarding the age at the time of surgery, Yamaguchi et al.26) compared the results of eccentric RAO in patients younger and older than 50 years. In their study, the 15-year survivorship with a Harris hip score less than 80 points as the endpoint was similar in both groups (71% in older patients and 81% in younger patients). In another study, the improvement of clinical score and radiographic parameters after RAO in patients 46 years of age or older was comparable with that of younger patients, and the 10-year survival rate was not significantly different between two groups.27) On the contrary, Tomioka et al.28) reported the results of RAO in 65 hips with adulthood dysplasia after minimum 10 years of follow-up. Although, they reported no progression of osteoarthritis in 76.7% and no requirement of total hip arthroplasty in 92.3% of the patients, older patients had a higher risk for both osteoarthritic progression and requirement of total hip arthroplasty. In addition, Yasunaga et al.29) performed a systemic review of RAO in 18 studies and concluded that clinical score and prevention of progression of radiographic osteoarthritis in patients 50 years or older or with advanced stage were worse than those in patients younger than 50 years or with early stage. In our study, the mean age at the time of surgery in patients with osteoarthritic progression was 46.8 years, whereas that of nonprogression patients was 35.6 years (p < 0.002). Several authors suggested the indication for RAO in older patients should be restricted to those with early stage osteoarthritis,27) with unilateral involvement,26) or with postoperative good joint congruency expected.27)
Limitations of our study include the retrospective study design, which may have introduced selection bias, the small number of patients, which made it difficult to determine prognostic or risk factors, and lack of preoperative or intraoperative evaluation of articular cartilage using magnetic resonance imaging or hip arthroscopy, which may have altered the outcomes of RAO. In addition, a major limitation of our study is the low follow-up rate. The follow-up rate after a least 10 years was 64.8% and this decreased rate may have masked the true incidence of osteoarthritic progression or total hip arthroplasty conversion. However, this was a consecutive series of acetabular dysplasia treated at the same institution using a consistent surgical procedure, and we could follow the patients for up to an average of 17.3 years.
In conclusion, the outcome of rotational acetabular osteotomy in most hips with Tönnis grade 0 and 1 was satisfactory after an average of 17 years of follow-up. The incidence of osteoarthritic progression was higher in Tönnis grade 2 and older age. Our results support that early joint preserving procedure is essential in the case of symptomatic dysplastic hips.
ACKNOWLEDGEMENTS
The authors are grateful to Mi-Kyung Kang, Min-Ji Kim, and Kyung-Jin Lee (Department of Orthopaedic Surgery, Keimyung University Dongsan Medical Center, Daegu, Korea) for their dedicated help.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Dorey FJ. Survivorship analysis of surgical treatment of the hip in young patients. Clin Orthop Relat Res. 2004;(418):23–28. doi: 10.1097/00003086-200401000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Yasunaga Y, Fujii J, Tanaka R, et al. Rotational acetabular osteotomy. Clin Orthop Surg. 2017;9(2):129–135. doi: 10.4055/cios.2017.9.2.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hasegawa Y, Iwata H, Mizuno M, Genda E, Sato S, Miura T. The natural course of osteoarthritis of the hip due to subluxation or acetabular dysplasia. Arch Orthop Trauma Surg. 1992;111(4):187–191. doi: 10.1007/BF00571474. [DOI] [PubMed] [Google Scholar]
- 4.Hartofilakidis G, Karachalios T, Zacharakis N. Charnley low friction arthroplasty in young patients with osteoarthritis: a 12- to 24-year clinical and radiographic followup study of 84 cases. Clin Orthop Relat Res. 1997;(341):51–54. [PubMed] [Google Scholar]
- 5.Steel HH. Triple osteotomy of the innominate bone. J Bone Joint Surg Am. 1973;55(2):343–350. [PubMed] [Google Scholar]
- 6.Eppright RH. Dial osteotomy of the acetabulum in the treatment of dysplasia of the hip. J Bone Joint Surg Am. 1975;57(8):1172. [Google Scholar]
- 7.Wagner H. The Hip Society, editors. The hip: Proceedings of the 4th Open Scientific Meeting of the Hip Society. St Louis, MO: C.V. Mosby; 1976. Osteotomies for congenital hip dislocation; pp. 45–66. [Google Scholar]
- 8.Ninomiya S, Tagawa H. Rotational acetabular osteotomy for the dysplastic hip. J Bone Joint Surg Am. 1984;66(3):430–436. [PubMed] [Google Scholar]
- 9.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias: technique and preliminary results. Clin Orthop Relat Res. 1988;(232):26–36. [PubMed] [Google Scholar]
- 10.Lee CB, Millis MB. Patient selection for rotational pelvic osteotomy. Instr Course Lect. 2013;62:265–277. [PubMed] [Google Scholar]
- 11.de Kleuver M, Kooijman MA, Pavlov PW, Veth RP. Triple osteotomy of the pelvis for acetabular dysplasia: results at 8 to 15 years. J Bone Joint Surg Br. 1997;79(2):225–229. doi: 10.1302/0301-620x.79b2.7167. [DOI] [PubMed] [Google Scholar]
- 12.Nakamura S, Ninomiya S, Takatori Y, Morimoto S, Umeyama T. Long-term outcome of rotational acetabular osteotomy: 145 hips followed for 10–23 years. Acta Orthop Scand. 1998;69(3):259–265. doi: 10.3109/17453679809000926. [DOI] [PubMed] [Google Scholar]
- 13.Schramm M, Pitto RP, Rohm E, Hohmann D. Long-term results of spherical acetabular osteotomy. J Bone Joint Surg Br. 1999;81(1):60–66. doi: 10.1302/0301-620x.81b1.8679. [DOI] [PubMed] [Google Scholar]
- 14.Nozawa M, Shitoto K, Matsuda K, Maezawa K, Kurosawa H. Rotational acetabular osteotomy for acetabular dysplasia: a follow-up for more than ten years. J Bone Joint Surg Br. 2002;84(1):59–65. doi: 10.1302/0301-620x.84b1.12299. [DOI] [PubMed] [Google Scholar]
- 15.Nozawa M, Maezawa K, Matsuda K, Kim S, Shitoto K, Kurosawa H. Rotational acetabular osteotomy for advanced osteoarthritis of the hip joint with acetabular dysplasia. Int Orthop. 2009;33(6):1549–1553. doi: 10.1007/s00264-008-0657-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kaneuji A, Sugimori T, Ichiseki T, Fukui K, Takahashi E, Matsumoto T. Rotational acetabular osteotomy for osteoarthritis with acetabular dysplasia: conversion rate to total hip arthroplasty within twenty years and osteoarthritis progression after a minimum of twenty years. J Bone Joint Surg Am. 2015;97(9):726–732. doi: 10.2106/JBJS.N.00667. [DOI] [PubMed] [Google Scholar]
- 17.Tonnis D. Congenital dysplasia and dislocation of the hip in children and adults. New York, NY: Springer-Verlag Berlin Heidelberg; 1987. pp. 165–171. [Google Scholar]
- 18.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special reference to the complication of osteoarthritis. Acta Chir Scand. 1939;83(Suppl 58):53–68. [Google Scholar]
- 19.Massie WK, Howorth MB. Congenital dislocation of the hip. Part I: method of grading results. J Bone Joint Surg Am. 1950;32(3):519–531. [PubMed] [Google Scholar]
- 20.Ninomiya S. Rotational acetabular osteotomy for the severely dysplastic hip in the adolescent and adult. Clin Orthop Relat Res. 1989;(247):127–137. [PubMed] [Google Scholar]
- 21.Murphy SB, Kijewski PK, Millis MB, Harless A. Acetabular dysplasia in the adolescent and young adult. Clin Orthop Relat Res. 1990;(261):214–223. [PubMed] [Google Scholar]
- 22.Takatori Y, Ninomiya S, Nakamura S, et al. Long-term results of rotational acetabular osteotomy in patients with slight narrowing of the joint space on preoperative radiographic findings. J Orthop Sci. 2001;6(2):137–140. doi: 10.1007/s007760100061. [DOI] [PubMed] [Google Scholar]
- 23.Yasunaga Y, Ochi M, Yamasaki T, Shoji T, Izumi S. Rotational acetabular osteotomy for pre- and early osteoarthritis secondary to dysplasia provides durable results at 20 years. Clin Orthop Relat Res. 2016;474(10):2145–2153. doi: 10.1007/s11999-016-4854-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Okano K, Enomoto H, Osaki M, Shindo H. Outcome of rotational acetabular osteotomy for early hip osteoarthritis secondary to dysplasia related to femoral head shape: 49 hips followed for 10–17 years. Acta Orthop. 2008;79(1):12–17. doi: 10.1080/17453670710014699. [DOI] [PubMed] [Google Scholar]
- 25.Yasunaga Y, Ochi M, Terayama H, Tanaka R, Yamasaki T, Ishii Y. Rotational acetabular osteotomy for advanced osteoarthritis secondary to dysplasia of the hip. J Bone Joint Surg Am. 2006;88(9):1915–1919. doi: 10.2106/JBJS.E.00715. [DOI] [PubMed] [Google Scholar]
- 26.Yamaguchi J, Hasegawa Y, Kanoh T, Seki T, Kawabe K. Similar survival of eccentric rotational acetabular osteotomy in patients younger and older than 50 years. Clin Orthop Relat Res. 2009;467(10):2630–2637. doi: 10.1007/s11999-009-0866-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yasunaga Y, Takahashi K, Ochi M, et al. Rotational acetabular osteotomy in patients forty-six years of age or older: comparison with younger patients. J Bone Joint Surg Am. 2003;85(2):266–272. doi: 10.2106/00004623-200302000-00013. [DOI] [PubMed] [Google Scholar]
- 28.Tomioka M, Inaba Y, Kobayashi N, et al. Ten-year survival rate after rotational acetabular osteotomy in adulthood hip dysplasia. BMC Musculoskelet Disord. 2017;18(1):191. doi: 10.1186/s12891-017-1556-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yasunaga Y, Yamasaki T, Ochi M. Patient selection criteria for periacetabular osteotomy or rotational acetabular osteotomy. Clin Orthop Relat Res. 2012;470(12):3342–3354. doi: 10.1007/s11999-012-2516-z. [DOI] [PMC free article] [PubMed] [Google Scholar]