Abstract
Aim
The objective of this prospective non-randomized study was to establish the role of biodegradable sub-acromial spacer (InSpace™) insertion in the management of patients with massive irreparable rotator cuff tear by reporting beneficial effects on the pain relief and functional outcomes in these patients.
Methods
This is a prospective non-randomized study of patients treated for irreparable cuff tears during a period between January 2014 and November 2016.14 patients with symptomatic massive irreparable rotator cuff tears were managed with arthroscopic debridement and implantation of a biodegradable subacromial spacer and were followed up for a mean 12.6 months (8–16 m). Inclusion criteria were patients with irreparable rotator cuff tears that failed the conservative management, with muscle retraction (Patte > stage 2), muscle atrophy, and fatty infiltration (Goutalier type 3). Patients with osteoarthritis grade 3 in the Hamada classification and/or without preserved passive motion were excluded from our study. Outcome measures included pre and postoperative, the range of motion, Constant and Oxford shoulder scores. The decision to perform surgery was made after failure of nonoperative treatment and rehabilitation (massive rotator cuff tear protocol, reading shoulder unit)for at least six months.
Results
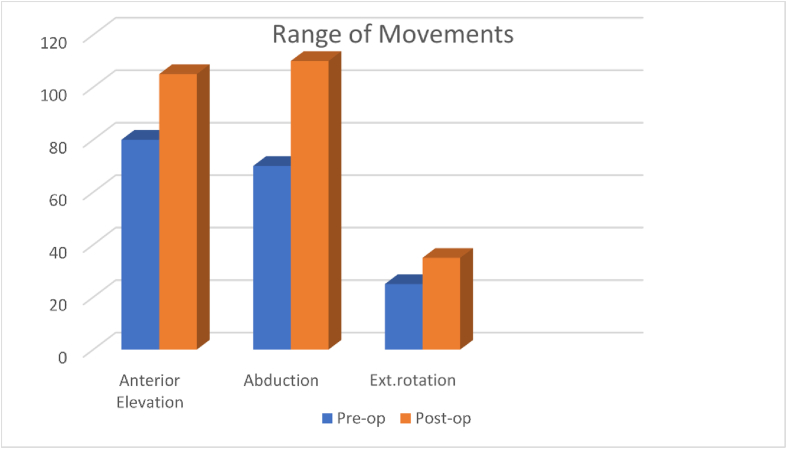
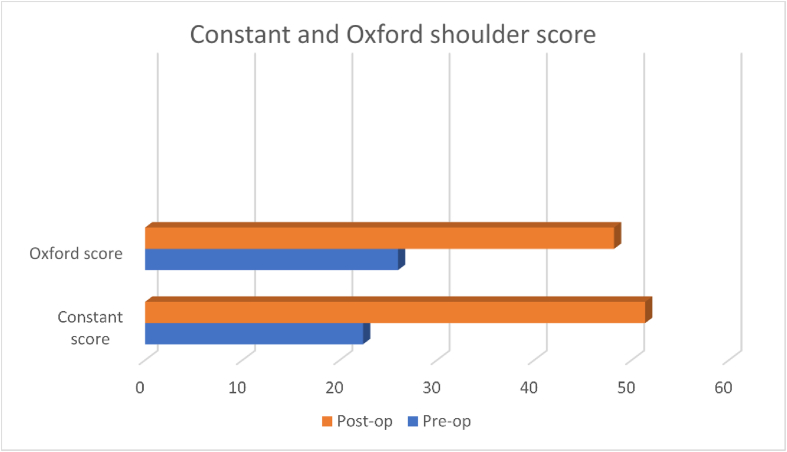
Fourteen shoulders (14 patients, ten male four female) met the inclusion criteria. The mean age of patients was 76.2 (70–85) years. During the last follow-up (8–16 months mean 12.6 months), the range of motion was significantly increased in all patients with anterior elevation (from 80 to 105°), abduction (from 70 to 110°), and external rotation (from 25 to 35°). The mean Constant score was also significantly (P < 0.001) improved from 22.5 (13–33) preoperatively to 51.4 (30–64) at the last follow-up. The Oxford shoulder score improved from 26 preoperatively (21–28) to 48.2 postoperatively (34–56). No night pain following surgery and ADL increased by 40%, which is significant in these patients. No significant perioperative complications were found except for one patient who had a spacer migration. However, no action was required in that case.
Conclusions
Arthroscopic implantation of a subacromial spacer for irreparable rotator cuff tear resulted in a noticeable improvement in pain relief and shoulder function at a mean 12.6 months follow up. It is a quick, safe and a minimally invasive procedure that is suitable for elderly patients with irreparable cuff tears and medical co-morbidities.
Keywords: Subacromial space, Irreparable cuff tear, Shoulder arthroscopy, Inspace, Balloon
1. Introduction
Therapeutic options for the treatment of irreparable rotator cuff tears are dependent on the patients' symptoms, demands and on the grade of the ongoing cuff tear arthropathy. Massive tears [Fig. 5, Fig. 6] have been described as > 5 cm1,2 and tears involving two or more tendons.3 An IRCT (irreparable rotator cuff tear) is any cuff tear which cannot be repaired back to the footprint, despite intra and extra-articular release of the remaining tissue or any repair that is successful but will almost certainly be associated with structural failure.4 The incidence may vary from 6.5% to 30%.5, 6, 7, 8 Static anterosuperior subluxation with AHD (acromiohumeral distance) [Fig. 4] less than 6 mm46 and pseudoparalysis on anterior elevation and dynamic anterosuperior subluxation of the humerus upon resisted abduction4 also suggests that the repair is not going to be successful. Other poor prognostic signs include a lag sign and a positive Horn blowers sign [9,10] for infraspinatus and teres minor function respectively. Grade 3 and 4 fatty infiltration commonly considered irreparable,4,11 although Burkhart has disputed this.12 The cuff tears are generally categorised into posterosuperior (supraspinatus, infraspinatus and teres minor), anterosuperior (supraspinatus and subscapularis) and global tears that include both anterosuperior and posterosuperior tears. Mulieri et al.13 reported reverse shoulder arthroplasty in patients with at least two-tendon tear without glenohumeral arthritis who failed to respond to conservative management for at least six months. In his study with a minimum of two years of follow-up, 58 patients out of 60 shoulders had shown improvement in pain and shoulder joint range of movement. Nevertheless, this procedure is associated with a high complication rate (∼20%) and considered as a salvage option.
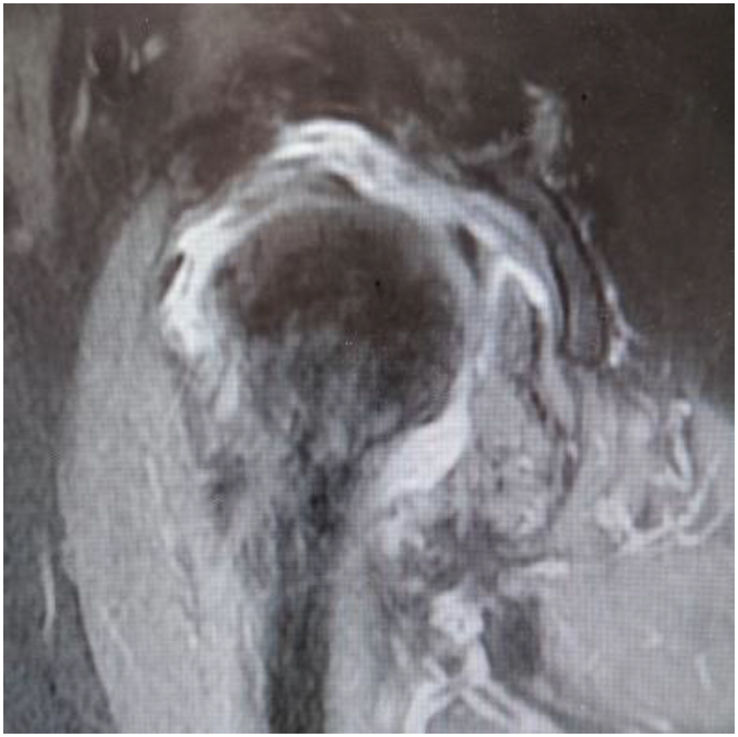
Fig. 5.
MRI shoulder depicting massive cuff tear on coronal section.
Fig. 6.
MRI shoulder depicting massive cuff tear on sagittal section.
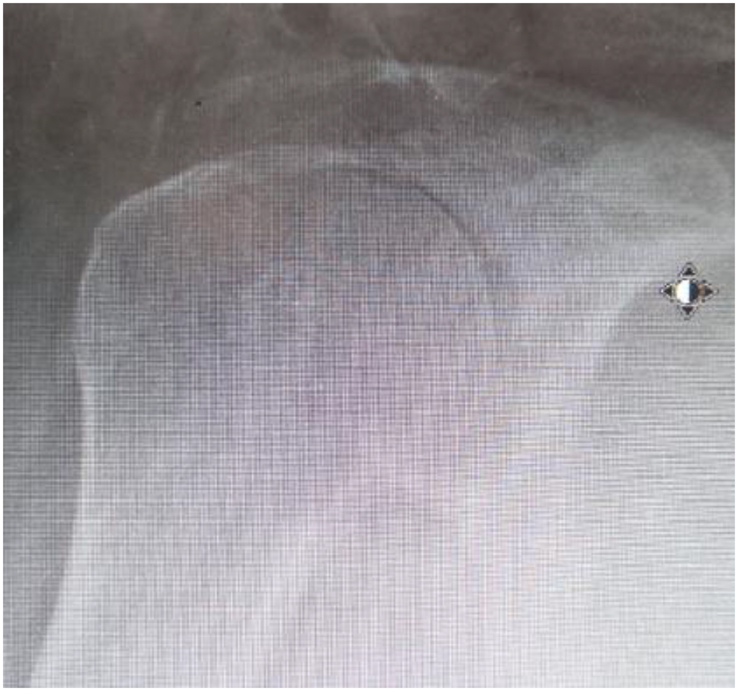
Fig. 4.
X-ray AP Shoulder showing proximal migration in cuff deficient shoulder with no significant arthritis.
Recently, several innovative studies used a biodegradable inspace balloon insertion in the subacromial space to restore shoulder biomechanics, by replicating the lowering effect of humeral head by rotator cuff tendons and reducing the subacromial friction. These studies with short follow up periods reported successful re-establishment of acromiohumeral distance (AHD) to improve the deltoid muscle lever arm to facilitate its function.
The Ortho-Space InSpace TM system is a biodegradable balloon-shaped spacer made of a copolymer Poly (l-lactide-co-ε-caprolactone) which biodegrades over 12 months, during which stage the force coupling should return and allow for long-term improvement in the glenohumeral joint movement. The spacer is available in three sizes to accommodate anatomic variation. The spacer size (small, medium or large) is selected based upon the surgeon's discretion after determining the extent of the tear and following measurement of the distance from the lateral border of the greater tuberosity to approximately 1 cm medial to the glenoid apex.
1.1. Surgical technique
The insertion method is reported to be simple, safe and reproducible. Standard shoulder arthroscopy for evaluation of the shoulder and tendon's condition to determine the presence of an irreparable rotator cuff tear [Fig. 1]. Perform debridement and bursectomy. We have not performed any concomitant acromioplasty or tuberoplasty. Selection of the correct balloon size by measuring the subacromial space using an arthroscopic probe. Three balloon sizes are available (S/M/L). After selection of appropriate size, Insert the rolled-up spacer introducer into the subacromial space through a lateral portal [Fig. 2]. Inflate the balloon by using saline to fill the subacromial space [Fig. 3]. The balloon was secured into position by circumferential hoop forces like in press-fit implantation between the acromion and humeral head. The shoulder is then taken through a full range of movement to ensure stability. After sealing Balloon, retract deployer. Inspace balloon can be used in patients with tears of Supraspinatus, Infraspinatus. It is advised in patients with intact or repaired Subscapularis for anterior stabilisation that helps in restoring biomechanics. It is contraindicated in pre-existing glenohumeral arthritis, active infection and allergies to the material of device components. Possible complications of this procedure apart from general complications include local inflammation, necrosis of the surrounding tissue and balloon displacement.
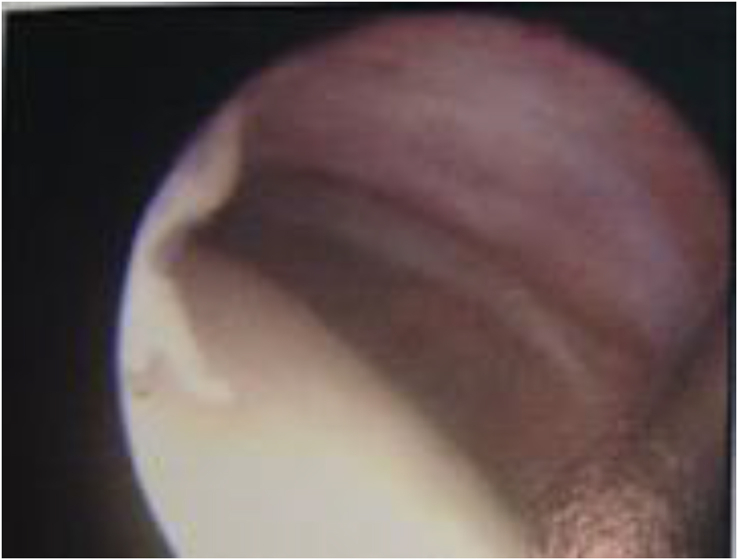
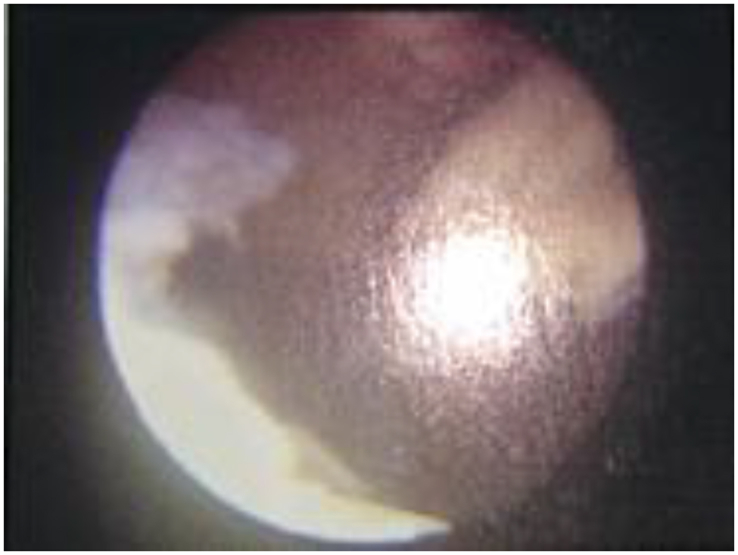
Fig. 1.
Intraoperative finding of massive cuff tear, and stages of balloon insertion.
Fig. 2.
Intraoperative insertion and inflation of balloon.
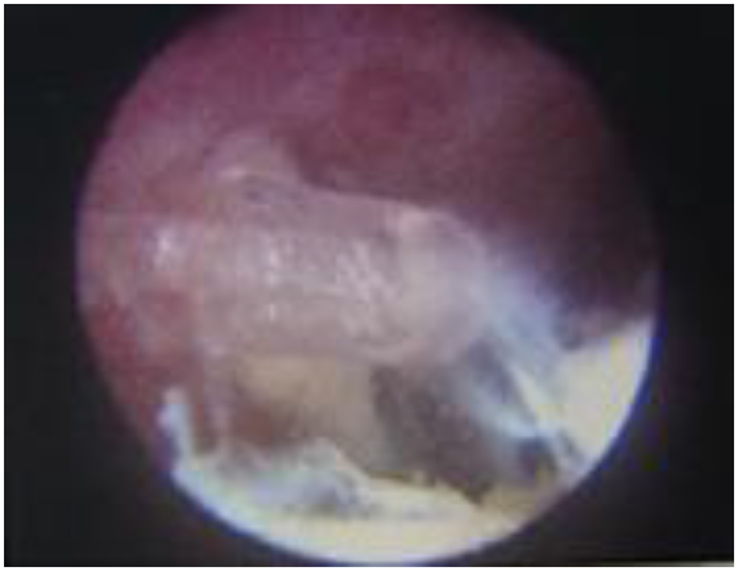
Fig. 3.
Intraoperative finding of massive cuff tear, and full inflation of balloon.
2. Materials and methods
2.1. Methods
A Prospective non-randomized study of patients treated for irreparable cuff tear, between January 2014 and November 2016 in our Orthopaedic department at East Surrey Hospital. 14 patients with symptomatic massive irreparable rotator cuff tears were managed with arthroscopic debridement and implantation of a biodegradable subacromial spacer and were followed up for at least one year (8–16 m). Inclusion criteria were patients with irreparable rotator cuff tears that failed the conservative management, with muscle retraction (Patte > stage 2), muscle atrophy, and fatty infiltration (Goutalier type 3). Patients with osteoarthritis grade 3 in the Hamada classification and/or without preserved passive motion were excluded from our study. In addition to bursal decompression nine patients underwent biceps tenotomy for pain relief. Outcome measures included pre and postoperative, the range of motion, Constant and Oxford shoulder scores. The decision to perform surgery was made after failure of nonoperative treatment and rehabilitation (massive rotator cuff tear protocol, reading shoulder unit) for at least six months.
3. Results
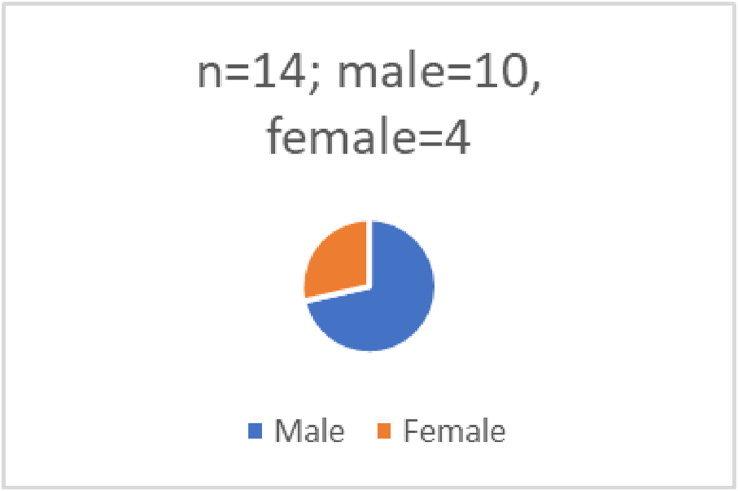
Fourteen shoulders (14 patients, ten male four female) [Fig. 9] met the inclusion criteria. The mean age of patients was 76.2 (70–85) years. During the last follow-up (8–16 months mean 12.6 months), the range of motion [Fig. 7] was significantly increased in all patients with anterior elevation (from 80 to 105°)[Table 1], abduction (from 70 to 110°), and external rotation (from 25 to 35°). There is an improvement in shoulder scores by more than 50%. The mean Constant score was also significantly (P < 0.001) improved from 22.5 (13–33) preoperatively to 51.4 (30–64.5) at the last follow-up. The Oxford shoulder score improved from 26 preoperatively (21–28) to 48.2 postoperatively (34–56) [Fig. 8]. Night pain improved from most nights to 1 or 2 nights in most of the patients as per Oxford score, and ADL increased by 40%, which is significant in these patients. We didn't routinely image the patients postoperatively to check whether they remained inflated or not. But in one case where patient complained of some discomfort in the anterior aspects of the shoulder with swelling underwent USS which has picked up anterior subluxation of the spacer balloon which didn't need any further intervention as the discomfort was not interfering with her day to day activities. No intra or postoperative complications were found except for one patient who had a spacer migration. No second surgical procedure such as reverse shoulder replacement was performed in any of these patients during this follow up period.
Fig. 9.
Graphical representation of demographics.
Fig. 7.
Graphical representation of range of movements pre and post op.
Table 1.
Anterior elevation (from 80 to 105 degrees).
| Ser.no | F/u months | Age | AE (80–105 deg)Pre/post op | ABD (70–110 deg) Pre/post op 70/110 | ER (from 25 to 35 deg) Pre/post op 25/35 | CS Pre/post op 22.5 (13–33) to 51.4 (30–64) | OSS Pre/post op 26 (21–28) to 48.2 (34–56) | Size | Sex |
|---|---|---|---|---|---|---|---|---|---|
| Pt 1 | 12 | 73 | 80/110 | 70/125 | 10/25 | 16/45 | 26/34 | M | M |
| Pt 2 | 10 | 77 | 70/105 | 90/135 | 30/35 | 24/64 | 28/56 | M | M |
| Pt 3 | 9 | 75 | 80/100 | 60/105 | 20/35 | 23/30 | 24//50 | M | M |
| Pt 4 | 10 | 72 | 85/105 | 45/95 | 15/30 | 27/49 | 27/49 | S | F |
| Pt 5 | 8 | 73 | 80/100 | 85/125 | 30/35 | 22/51 | 26/56 | M | M |
| Pt 6 | 9 | 72 | 100/105 | 80/110 | 35/35 | 23/53 | 28/51 | S | F |
| Pt 7 | 13 | 85 | 85/110 | 65/100 | 10/30 | 18/57 | 26/48 | S | M |
| Pt 8 | 11 | 80 | 60/90 | 95/130 | 45/45 | 27/59 | 26/45 | S | F |
| Pt 9 | 16 | 77 | 90/110 | 75/115 | 15/30 | 33/53 | 27/49 | M | M |
| Pt 10 | 12 | 82 | 85/120 | 45/90 | 10/30 | 28/51 | 25/52 | M | M |
| Pt 11 | 11 | 78 | 65/85 | 50/95 | 30/35 | 26/50 | 26/41 | L | M |
| Pt 12 | 12 | 81 | 85/120 | 110/120 | 45/45 | 27/57 | 25/45 | M | M |
| Pt 13 | 10 | 73 | 65/100 | 45/85 | 25/35 | 25/51 | 21/49 | S | F |
| Pt 14 | 10 | 70 | 80/105 | 60/95 | 30/35 | 13/50 | 27/51 | S | M |
SN = serial number; FU = follow up; AE = anterior elevation; ABD = abduction; ER = external rotation; CS = constant score; OSS = oxford shoulder score; Size = Size of balloon.
Fig. 8.
Graphical representation of pre and post op constant and oxford scores.
4. Discussion
No consensus regarding the ideal treatment option for patients suffering from pain and disability from massive/irreparable RC tears is available yet. By the force couple theory,14, 15, 16 active motion can be possible despite massive RC tear if force coupling is maintained. Several surgical interventions have been described as ranging from simple arthroscopic debridement to reverse shoulder arthroplasty to manage these symptomatic patients. However, recent studies reported a biodegradable subacromial balloon spacer implanted between the humeral head and acromion could restore the shoulder biomechanics. Senekovic et al.17 published their early results of 20 patients treated with the InSpace system. The average age in this cohort was 70.5 years (range 54–85 years), and the follow-up period was 34.7 months (range 4–95 months). The average total Constant score increased from 33.4 to 65.4 points, with a statistically significant improvement in all aspects of the constant score. Patients reported significant improvement in their daily living activities during the 6th week after surgery. The range of motion also showed significant improvement eight weeks later. Power improved at 18 months, and the improvement in shoulder function was sustained at three years. In a retrospective study reporting the clinical and radiographic results of the biodegradable subacromial spacer implantation, authors corroborate that, irreparable massive cuff tears in worker patients and with recreational activities' demands, the inspace balloon is a viable option to recover the shoulder function with a reduction of the pain.18 In another clinical study, they performed the clinical evaluation (Constant Score and VAS), X-rays and MR imaging preoperatively in all patients and at 3, 6, 12 and 24 months after surgery, dividing patients into different groups according to the time elapsed from surgery. In their study, Constant Score increased from 39.89 to 62.33 points (p 0.0002) in the six months group and from 41.66 to 65.38 points (p < 0.0001) in the 12 months group. ROM (Range of Movement) and ADL (Activity of Daily Living) significantly improved with the contemporary reduction of VAS and pain at 12 months and, furthermore, an increase of functional performance with reduction of pain was registered at 24 months. In a study19 where the clinical outcome of patients treated with conventional arthroscopic techniques (n = 11, group A, partial repair, biceps tenotomy, and debridement) and that of patients treated with a supplementary ISB (n = 12, group B) was retrospectively analysed. In their series, [with a preoperative American Shoulder and Elbow Surgeons (ASES) score: group A, 59.1; group B, 31.5; and the Constant score: group A, 60.7; group B, 36.8] they found improved shoulder function [ASES score: group A, 88.6; p < 0.001; group B, 85.7; p < 0.001, and the Constant score: group A, 77.6; p < 0.001; group B, 69.5; p < 0.001;] in both the groups at a follow-up after a mean of 22 months. Minimal improvement in 2 pts with pseudoparalytic shoulders was noticed. Patients in both groups were happy with their outcome (the preoperative shoulder function was lower in patients treated with an ISB). In rotator cuff repairs, the spacer may mechanically protect the tendon and reduces the downward force needed by the supraspinatus to centre the humeral head during abduction,20 Which may improve the long-term results of rotator cuff repairs, especially in large tears. Avoid overstuffing as there may be a theoretical risk of a decrease in the blood supply to the repaired cuff, though; it was not proved clinically. In a study21 describing the insertion technique using fluoroscopy, believes that it can be performed in a day-care or outpatient setting with patients under local anaesthesia. The previous studies have shown that the spacer may self-dissolve at 12 months which confines to the period of rehabilitation. The spacer begins to degrade approximately 2–3 months post-implantation and fully disintegrates within 12 months,22 though, it is unclear how long the spacer remains inflated. At 6 months, the device was barely detectable in 54.5% of the patients, yet the shoulder function demonstrated continued improvement in the majority of the subjects (US or MRI). At 3 years, 19 patients underwent a follow-up MRI examination that confirmed total biodegradation of the device.23
Although a variety of studies24 have shown that debridement with or without biceps tenotomy remains a viable option in the elderly and low demand patients with a functional but very painful shoulder, it does not slow the progression of osteoarthritis as it doesn't improve the biomechanics. Loss of shoulder flexion strength is often a concern for patients who are a candidate for LHB sacrifice. Boileau et al.25 concluded that pseudoparalysis of the shoulder and severe RC arthropathy are contraindications to this procedure. However, the literature supports arthroscopic biceps tenotomy with or without inspace balloon insertion in the treatment of RC tears in selected patients yields good objective improvement and a high degree of patient satisfaction.15,26,27 However, Klinger et al.28 disputed that additional LHB tenotomy did not significantly influence the outcomes. There was no generalised consensus in the literature about humeral head migration or progression of cuff arthropathy following tenotomy.
Several studies suggest that the partial repair with tenolysis and interval slide provides a longer lasting improvement in pain relief and restoring function when compared to debridement alone.9,10,29, 30, 31, 32 The prerequisites for partial repair to restore AP force couple (margin convergence technique) are well centred joint with less than or equal to grade 3 fatty degeneration.12,24,33,34 It was noted that only 48% were structurally intact when imaged using ultrasound at 24 months.9,35
Lo et al.36 showed statistically significant improvements with interval slide. However, studies comparing the results of partial repair with interval slide found no significant difference in outcomes.37,38 Concerns regarding this technique include devascularisation of the supraspinatus tendon and defunctioning of an already impaired muscle-tendon unit from the interval slide.37,39
4.1. Tendon transfer
Tendon transfers can be indicated in a cooperative patient with the loss of active external rotation but performable active flexion with a higher grade of muscular atrophy, and without degenerative changes > grade II [24 40]. Split pectoralis major transfer for subscapularis tear may give pain relief and stability, but functional improvement is less specific [16 41] as optimal biomechanics can't be achieved. The outcomes with latissimus dorsi tendon transfers in irreparable posterosuperior rotator cuff tear may reliably restore flexion and relieves pain; however, its use is downcasted in patients with preceding failed rotator cuff surgery due to unpredictable results. If the lack of external rotation is isolated with good active forward elevation, the L'Episcopo procedure (transfer of teres major to a lateral position, causing it to be a lateral rotator of the shoulder) is the procedure of choice.
4.2. Tuberoplasty
Lee et al.27,42 presented satisfactory results with good preservation of acromiohumeral interval and continuity in the inferior scapulohumeral line, regardless of preoperative mobility, at least 3 years after arthroscopic tuberoplasty. Scheibel et al.31 in 2004, who described tuberoplasty as the reversed arthroscopic subacromial decompression, has shown significant improvements in pain, the range of motion and activities of daily living following this procedure. In literature, poor outcomes were attributed to increased preoperative pain, patients with pseudoparalysis32 and a disruption of the inferior scapulohumeral line23 where a debridement with or without biceps tenotomy and the inspace balloon has a role in symptomatic improvement.
4.3. Graft interposition
The mechanical properties of biological allografts have been shown to be inferior to both autografts and synthetic grafts.2,3 Gupta et al. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3678622/ 2 described a prospective observational study using Dermal tissue allograft, showed a significant improvement in pain, the range of motion, and strength. In their study, the follow up was for 3 yrs on average, and 76% of patients had intact cuff repair, whereas Glanzmann et al.41, had reported only 16.5% and 12.5% survival rates at mid and long-term follow-ups respectively, which were confirmed on Ultrasound scan in both the studies. With regards to host response, xenografts appear to induce the most significant hypersensitivity, thought to be related to the galactose-a (1,3)-galactose (a-Gal) terminal disaccharide.40 In a randomized prospective study42 comparing interposition autograft with tensor fascia lata and partial repair, there were significantly fewer re-tears in the patch graft group (8.3% vs 41.7%) although, significant improvement in clinical outcomes was recorded in both the groups. Also, shoulders with re-tears had significantly inferior clinical outcomes when compared to those without re-tears (P < 0.001). Glanzmann et al.] showed that Cranial migration of the humeral head progressed in all patients with deltoid flap transfers and insignificant functional gains achieved, though, noticed an improvement in pain and patient satisfaction. By these results, Glanzmann et al. suggested not to use this technique in irreparable cuff tears.
4.4. Arthroscopic superior capsular reconstruction
Compared to interposition patch grafting which allowed impingement of interposition, superior capsular reconstruction wholly restored superior stability and thus prevented impingement in a clinical study.43 Radiographically the acromiohumeral distance increased significantly from 4.6 mm to 8.7 mm (P < 0.0001) postoperatively, with no progression of osteoarthritis of the glenohumeral joint. A postoperative MRI scan confirmed that 20 patients (83.3%) had an intact graft, with no progression of muscle atrophy. The authors surmised that the reconstruction of the superior capsule restored the force coupling due to suturing the graft to the infraspinatus posteriorly and the residual supraspinatus or subscapularis anteriorly.
4.5. Suprascapular nerve ablation/neurolysis or neurotomy
The role of the suprascapular nerve, which can probably be constricted by the retracted rotator cuff, and its therapy has not been completely clarified. Its indicated in patients with significant medical co-morbidities with rotator cuff arthropathy44 with distinct symptoms. The efficacy of the Pulsed radiofrequency techniques treatment may wear off in six months in up to 50% of the patients.45 Nizlan et al.46 described an arthroscopic SSN neurectomy technique with good pain control (sensory). However, no assessment or comment was made about outcomes due to loss of residual infraspinatus function (motor distribution).
Non-surgical management such as physical therapy and exercise may, in selected cases, be a treatment alternative to surgical procedures.47, 48, 49 A study11 on anterior deltoid rehabilitation program for patients with an average age of 80 years (range, 70–96 years) and confirmed massive rotator cuff tear, has reported that the Constant score increased from a mean of 26 (range, 8–41) before treatment to a mean of 60 (range, 43–77) at a minimum of 9 months after treatment. The range of motion in forward elevation was improved from a mean of 40° (range, 30°–60°) at presentation to a mean of 160° (range 150°–180°) after the deltoid rehabilitation course. Authors recommend that a structured deltoid rehabilitation program is suitable for elderly patients with massive rotator cuff tears.
5. Conclusion
The ISB is a feasible treatment option for MRCT, providing subjective pain relief and improved shoulder function. It can be considered as part of the treatment algorithm in patients with an irreparable rotator cuff and could be used as either as an interim procedure, delaying the need for more invasive surgery in the physiologically young and active, or as a potential definitive procedure in the medically unfit patients. Careful subacromial debridement combined with biceps tenotomy and a cautious or reversed decompression may reduce the pain temporarily without influencing the active motion until with the loss of active elevation which is an indication for reverse shoulder arthroplasty, in the meantime, absorbable subacromial spacers may improve shoulder biomechanics. Once again, prospective randomized trials with larger patient cohorts and longer follow-ups are required to confirm its' effectiveness.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jor.2018.08.004.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Ricchetti E.T., Aurora A., Iannotti J.P., Derwin K.A., Scaffold Devices for rotator cuff re-pair. J Shoulder Elbow Surg. 2012;21:251–265. doi: 10.1016/j.jse.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 2.Gupta A.K., Hug K., Berkoff D.J. Dermal tissue allograft for the repair of massive irreparable rotator cuff tears. Am J Sports Med. 2012;40(1):141–147. doi: 10.1177/0363546511422795. [DOI] [PubMed] [Google Scholar]
- 3.Scheibel M., Lichtenberg S., Habermeyer P. Reversed arthroscopic subacromial de-compression for massive rotator cuff tears. J Shoulder Elbow Surg. 2004;13(3):272–278. doi: 10.1016/j.jse.2004.01.007. [Internet] [DOI] [PubMed] [Google Scholar]
- 4.Mori D., Funakoshi N., Yamashita F. Arthroscopic surgery of irreparable large or mas-sive rotator cuff tears with low-grade fatty degeneration of the infraspinatus: patch autograft procedure versus partial repair procedure. Arthrosc J Arthrosc Relat Surg. 2013;29(12):1911–1921. doi: 10.1016/j.arthro.2013.08.032. [DOI] [PubMed] [Google Scholar]
- 5.Mihata T., McGarry M.H., Pirolo J.M., Kinoshita M., Lee T.Q. Superior capsule recon-struction to restore superior stability in irreparable rotator cuff tears: a biomechani-cal cadaveric study. Am J Sports Med. 2012;40(10):2248–2255. doi: 10.1177/0363546512456195. [DOI] [PubMed] [Google Scholar]
- 6.Shah R.V., Racz G.B. Pulsed mode radiofrequency lesioning of the suprascapular nerve for the treatment of chronic shoulder pain. Pain Physician. 2003;6(4):503–506. [PubMed] [Google Scholar]
- 7.Nizlan N.M., Skirving A.P., Campbell P.T. Arthroscopic suprascapular neurectomy for the management of severe shoulder pain. J Shoulder Elbow Surg. 2009;18(2):245–250. doi: 10.1016/j.jse.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 8.Kane T.P.C., Rogers P., Hazelgrove J., Wimsey S., Harper G.D. Pulsed radiofrequency applied to the suprascapular nerve in painful cuff tear arthropathy. J Shoulder Elbow Surg. 2008;17(3):436–440. doi: 10.1016/j.jse.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 9.Ricci M., Vecchini E., Micheloni G.M. A clinical and radiological study of biodegradable subacromial spacer in the treatment of mas-sive irreparable rotator cuff tears. Acta Biomed. 2017;88 doi: 10.23750/abm.v88i4-S.6797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holschen M., Brand F., Agneskirchner J.D. Subacromial spacer implantation for mas-sive rotator cuff tears: clinical outcome of arthroscopically treated patients. Obere Extrem. 2017;12(1):38–45. doi: 10.1007/s11678-016-0386-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Levy O., Mullett H., Roberts S., Copeland S. The role of anterior deltoid reeducation in patients with massive irreparable degenerative rotator cuff tears. J Shoulder Elbow Surg. 2008;17(6):863–870. doi: 10.1016/j.jse.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 12.Cofield R.H., Parvizi J., Hoffmeyer P.J., Lanzer W.L., Ilstrup D.M., Rowland C.M. Surgical repair of chronic rotator cuff tears. A prospective long-term study. J Bone Joint Surg Am. 2001;83-A:71–77. doi: 10.2106/00004623-200101000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Gerber C., Fuchs B., Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82:505–515. doi: 10.2106/00004623-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Moore D.R., Cain E.L., Schwartz M.L., Clancy W.G. Allograft reconstruction for massive, irreparable rotator cuff tears. Am J Sports Med. 2006;34:392–396. doi: 10.1177/0363546505281237. [DOI] [PubMed] [Google Scholar]
- 15.Ozaki J., Fujimoto S., Masuhara K., Tamai S., Yoshimoto S. Reconstruction of chronic massive rotator cuff tears with synthetic materials. Clin Orthop Relat Res. 1986;(202):173–183. [PubMed] [Google Scholar]
- 16.Rosa Donato. Treatment of massive irreparable rotator cuff tears through biodegradable subacromial InSpace balloon. BMC Surg. 2013;13(suppl 1) A43. PMC. Web. 29 Mar. 2018. [Google Scholar]
- 17.Gerber C., Wirth S.H., Farshad M. Treatment options for massive rotator cuff tears. J Shoulder Elbow Surg. 2011;20:S20–S29. doi: 10.1016/j.jse.2010.11.028. [DOI] [PubMed] [Google Scholar]
- 18.Warner J.J. Management of massive irreparable rotator cuff tears: the role of tendon transfer. Instr Course Lect. 2001;50:63–71. [PubMed] [Google Scholar]
- 19.Anley C.M., Chan S.K., Snow M. Arthroscopic treatment options for irreparable rotator cuff tears of the shoulder. World J Orthoped. 2014;5(5):557. doi: 10.5312/wjo.v5.i5.557. [Internet] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Burkhart S., Barth J., Richards D., Zlatkin M., Larsen M. Arthroscopic repair of massive rotator cuff tears with stage 3 and 4 fatty degeneration. Arthroscopy. 2007;23(4):347–354. doi: 10.1016/j.arthro.2006.12.012. [Internet] [DOI] [PubMed] [Google Scholar]
- 21.Mulieri P., Dunning P., Klein S., Pupello D., Frankle M. Reverse shoulder arthroplasty for the treatment of irreparable rotator cuff tear without glenohumeral arthritis. J Bone Joint Surg Am Vol. 2010;92(15):2544–2556. doi: 10.2106/JBJS.I.00912. [Internet] [DOI] [PubMed] [Google Scholar]
- 22.RH C., Parvizi J., PJ H. Surgical repair of chronic rotator cuff tears. A prospective long-term study. J Bone Joint Surg Am Vol. 2001;83(1):71–77. doi: 10.2106/00004623-200101000-00010. [Internet] [DOI] [PubMed] [Google Scholar]
- 23.Verhelst L., Vandekerckhove P.J., Sergeant G., Liekens K., Van Hoonacker P., Berghs B. Reversed arthroscopic subacromial decompression for symptomatic irreparable rota-tor cuff tears: mid-term follow-up results in 34 shoulders. J Shoulder Elbow Surg. 2010;19(4):601–608. doi: 10.1016/j.jse.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 24.Goutallier D., Postel J.M., Gleyze P., Leguilloux P., Van Driessche S. Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg. 2003;12:550–554. doi: 10.1016/s1058-2746(03)00211-8. [DOI] [PubMed] [Google Scholar]
- 25.Boileau P., Baqué F., Valerio L., Ahrens P., Chuinard C., Trojani C. Isolated arthroscopic biceps tenotomy or tenodesis improves symptoms in patients with massive irrepara-ble rotator cuff tears. J Bone Jt Surg - Ser A. 2007;89(4):747–757. doi: 10.2106/JBJS.E.01097. [DOI] [PubMed] [Google Scholar]
- 26.Ellman H., Hanker G., Bayer M. Repair of the rotator cuff. End-result study of factors influencing reconstruction. J Bone Joint Surg Am. 1986;68:1136–1144. [PubMed] [Google Scholar]
- 27.Warner J.J. Management of massive irreparable rotator cuff tears: the role of tendon transfer. Instr Course Lect [Internet] 2001;50 63–7112. [PubMed] [Google Scholar]
- 28.Sugaya H., Maeda K., Matsuki K., Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. A prospective outcome study. J Bone Jt Surg Am [Internet] 2007;89(5):953–960. doi: 10.2106/JBJS.F.00512. [DOI] [PubMed] [Google Scholar]
- 29.Walch G., Edwards T.B., Boulahia A., Nové-Josserand L., Neyton L., Szabo I. Arthro-scopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: clinical and radiographic results of 307 cases. J Shoulder Elbow Surg. 2005;14(3):238–246. doi: 10.1016/j.jse.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 30.Senekovic V., Poberaj B., Kovacic L., Mikek M., Adar E., Dekel A. Prospective clinical study of a novel biodegradable sub-acromial spacer in treatment of massive irrepara-ble rotator cuff tears. Eur J Orthop Surg Traumatol [Internet] 2013;23(3):311–316. doi: 10.1007/s00590-012-0981-4. [DOI] [PubMed] [Google Scholar]
- 31.Patzer T., Hufeland M., Krauspe R. [Irreparable rotator cuff tears. Debridement, partial reconstruction, tendon transfer or reversed shoulder arthroplasty] Orthopä. 2016;45(2):149–158. doi: 10.1007/s00132-015-3204-y. [In-ternet] [DOI] [PubMed] [Google Scholar]
- 32.Omid R., Lee B. Tendon transfers for irreparable rotator cuff tears. J Am Acad Orthop Surg. 2013;21(8):492–501. doi: 10.5435/JAAOS-21-08-492. [Internet] [DOI] [PubMed] [Google Scholar]
- 33.Burkhart S.S. Arthroscopic debridement and decompression for selected rotator cuff tears. Clinical results, pathomechanics, and patient selection based on biome-chanical parameters. Orthop Clin N Am. 1993;24(1):111–123. [PubMed] [Google Scholar]
- 34.Kim S.J., Kim S.H., Lee S.K., Seo J.W., Chun Y.M. Arthroscopic repair of massive con-tracted rotator cuff tears: aggressive release with anterior and posterior interval slides do not improve cuff healing and integrity. J Bone Jt Surg - Ser A. 2013;95(16):1482–1488. doi: 10.2106/JBJS.L.01193. [DOI] [PubMed] [Google Scholar]
- 35.Maman E., Safran O., Beyth S. Biceps tenotomy does not affect the functional outcomes of patients treated with spacer implanta-tion due to massive irreparable rotator cuff tears. Open Orthop J [Internet] 2017;11(1):1577–1584. doi: 10.2174/1874325001711011577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Szöllösy G., Rosso C., Fogerty S., Petkin K., Lafosse L. Subacromial spacer placement for protection of rotator cuff repair. Arthrosc Tech. 2014;3(5):e605–e609. doi: 10.1016/j.eats.2014.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gervasi E., Cautero E., Dekel A. Fluoroscopy-guided implantation of subacromial “Biodegradable Spacer” using local anesthesia in patients with irreparable rotator cuff tear. Arthrosc Tech. 2014;3(4):e455–e458. doi: 10.1016/j.eats.2014.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Savarese E., Romeo R. New solution for massive, irreparable rotator cuff tears: the subacromial “biodegradable spacer”. Arthrosc Tech. 2012;1(1) doi: 10.1016/j.eats.2012.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Klinger H.M., Spahn G., Baums M.H., Steckel H. Arthroscopic debridement of irrepara-ble massive rotator cuff tears - a comparison of debridement alone and combined procedure with biceps tenotomy. Acta Chir Belg. 2005;105(3):297–301. doi: 10.1080/00015458.2005.11679720. [DOI] [PubMed] [Google Scholar]
- 40.Iagulli N.D., Field L.D., Hobgood E.R., Ramsey J.R., Savoie F.H. Comparison of partial versus complete arthroscopic repair of massive rotator cuff tears. Am J Sports Med [Internet] 2012;40(5):1022–1026. doi: 10.1177/0363546512438763. [DOI] [PubMed] [Google Scholar]
- 41.Glanzmann M.C., Goldhahn J., Flury M., Schwyzer H.-K., Simmen B.R. Deltoid flap reconstruction for massive rotator cuff tears: mid- and long-term functional and structural results. J Shoulder Elbow Surg. 2010;19(3) doi: 10.1016/j.jse.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 42.Hirooka A., Yoneda M., Wakaitani S. Augmentation with a Gore-Tex patch for repair of large rotator cuff tears that cannot be sutured. J Orthop Sci. 2002;7:451–456. doi: 10.1007/s007760200078. [DOI] [PubMed] [Google Scholar]
- 43.Lee B.G., Cho N.S., Rhee Y.G. Results of arthroscopic decompression and tuberoplasty for irreparable massive rotator cuff tears. Arthrosc J Arthrosc Relat Surg. 2011;27(10):1341–1350. doi: 10.1016/j.arthro.2011.06.016. [DOI] [PubMed] [Google Scholar]
- 44.Nasca R.J. The use of freeze-dried allografts in the management of global rotator cuff tears. Clin Orthop Relat Res. 1988;228:218–226. [PubMed] [Google Scholar]
- 45.Edwards P., Ebert J., Joss B., Bhabra G., Ackland T., Wang A. Exercise rehabilitation in the non-operative management of rotator cuff tears: a review of the literature. Int J Sport Phys Ther [Internet] 2016;11(2):279–301. [PMC free article] [PubMed] [Google Scholar]
- 46.Melillo A.S., Savoie F.H.I., Field L.D. Massive rotator cuff tears: debridement versus repair. Orthop Clin N Am. 1997;28(1):117–124. doi: 10.1016/s0030-5898(05)70269-8. [DOI] [PubMed] [Google Scholar]
- 47.Valenti P. Joint-preserving treatment options for irreparable rotator cuff tears. Orthopä. 2018;47(2):103–112. doi: 10.1007/s00132-017-3516-1. [Internet] [DOI] [PubMed] [Google Scholar]
- 48.Lo I.K.Y., Burkhart S.S. Arthroscopic repair of massive, contracted, immobile rotator cuff tears using single and double interval slides: technique and preliminary Re-sults. Arthrosc J Arthrosc Relat Surg. 2004;20(1):22–33. doi: 10.1016/j.arthro.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 49.Omid R., Lee B. Tendon transfers for irreparable rotator cuff tears. J Am Acad Orthop Surg. 2013;21:492–501. doi: 10.5435/JAAOS-21-08-492. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.